Abstract
Inflammatory fibrous hyperplasia, pyogenic granuloma, peripheral ossifying fibroma, irritational fibroma (IF), peripheral giant cell granuloma, etc., are the different types of reactive gingival lesions that may occur in response to mild chronic irritation associated with subgingival factors, root remnant, iatrogenic factors, and trauma. Gingival IF is one of the most common reactive lesions and is usually sessile in nature, and its size is usually not more than 1.5 cm. Complete surgical excision along with the elimination of precipitating/aggravating factors is the treatment of choice generally adopted by a general dentist without giving due consideration to its size, location, and postoperative sequel. The present rare case describes the simple, easy to perform, and effective periodontal plastic treatment for the management of expected residual soft tissue defect, following surgical excision of large recurrent IF in the posterior maxillary teeth at 9 months postoperatively, in addition to its conceivable etiology and diagnosis.
Keywords: Coronally repositioned flap, irritational fibroma, osteoplasty, reactive gingival lesions, surgical excision
INTRODUCTION
Different types of lesions (developmental, benign, inflammatory, reactive, and neoplastic) are observed in the oral cavity. Irritational fibroma (IF) is among one of the most common types of reactive gingival lesion encountered in routine dental practice. It usually occurs in response to different low-grade intrinsic and extrinsic irritational factors.[1] Comprehensive surgical excision of reactive gingival lesion, followed by thorough eradication of infuriating factors, is the principle handling protocol to prevent the recurrence of such lesions; however, sometimes, if the excised lesion is large, it may create a residual soft tissue defect, which may further precipitate functional and esthetic discrepancies if not managed immediately. The present rare case not only describes the method of assessment, plausible etiology, and diagnosis of recurrent IF but also harmonizes the repair of residual gingival defect by coronally repositioned flap (CRF) technique in the posterior maxillary teeth.
CASE REPORT
A 50-year-old otherwise healthy female patient was reported to the institutional outpatient department of periodontology with chief complaints of swelling of gums in the left upper back teeth and difficulty in brushing for the past 1.5 years and 3 months, respectively. History disclosed that the lesion was excised approximately 2 years back but recurred. Initially, the lesion was small, and gradually, it gained the present size.On clinical examination, generalized mild papillary inflammation with bleeding on probing and generalized normal gingival sulcus depth on periodontal probing were observed.
Buccal gingival sulcus depth with respect to #26, 27 was not probable due to gingival overgrowth.Thegrowth was sessile in nature, the size was approximately ≥20 mm × 15 mm and without any color differentiation from the adjacent gingival tissue [Figure 1a]. The basal attachment of the growth on exploration from all aspects (mesial, distal, apical and coronal direction) with 4-0 black silk suturesuggested that the lesion involvedmarginal gingiva andpart of the attached gingiva with respect to #26, 27. Intraoral periapical radiographic evaluation with respect to #25, 26, 27 was normal [Figure 1b]. Provisional diagnosis of pyogenic granuloma (PG)/peripheral ossifying fibroma (POF)/IF with respect to #26, 27 with generalized chronic mild papillary gingivitis was made. Phase-1 periodontal therapy was performed. All routine hematological (hemoglobin, bleeding time, clotting time, total leukocyte count, differential leukocyte count, and random blood sugar) investigations were within normal limits. Punch incision biopsy was taken [Figure 1c] after administration of 2% lignocaine hydrochloride and 1:80,000 adrenaline bitartrate containing local anesthetic (LA) solution (XICAINE™, ICPA Health Products, Mumbai, India). Biopsy specimen was sent for histopathological evaluation in 10% formalin solution. An oral analgesic (ibuprofen 400 mg) was prescribed as and when required for pain relief. The patient was instructed to rinse twice daily with 0.2% chlorhexidine gluconate mouth rinse for 2 weeks postoperatively and not to brush the treated area during the first 2 weeks. Surgical treatment protocol with concurrent restoration of anticipated residual gingival defect by means of CRF was discussed. The patient was recalled after 2 weeks. On recall visit, the patient agreed to the surgical treatment protocol as advice at the time of the first visit and submitted the signed written consent.
Figure 1.

Preoperative picture showing (a) isolated gingival growth of 2 cm with respect to tooth no 25–27; (b) no lesion observed on intraoral periapical X-ray evaluation; (c) an punch incisional biopsy was under process, (d) photomicrograph (×10) showing atrophic epithelium, connective tissue stroma, and focal areas of inflammation
Hematoxylin and eosin-stained histological section under ×10 showed thin parakeratinized stratified squamous epithelium with loss of rete ridges. The epithelium was atrophic. Underlying connective tissue stroma was moderately collagenous interspersed with fibroblasts. Mild chronic inflammatory cell infiltration was seen chiefly consisting of lymphocytes and plasma cells which suggestive of IF [Figure 1d].
On the 14th day recall visit, lesion was slightly reduced in size [Figure 2a]. Basal attachment of the IF was reassessed with the help of suturing thread [Figure 2b]. Under aseptic condition, left posterior superior alveolar and infraorbital nerve block was given utilizing 2% LA solution. Surgical excision of IF growth close to the facial gingival surface of #26, 27 was carried out with the help of 15 number surgical blade to observe its basal and peripheral extensions [Figure 2c]. Internal bevel incision was given 1.5–2 mm away the lesion's peripheral extensions [Figure 2d] to prevent recurrence. Crevicular incision was given in the 1–1.5 mm of remaining attached gingiva apical to the internal bevel incision with respect to #26, 27 followed by two vertical releasing incisions mesial and distal line angle of #26, 27, respectively. Full-thickness flap was reflected. Comprehensive elimination of the lesion was carried out with the help of Gracey's and surgical curettes, and anticipated area of residual soft tissue defect was observed.Thediseased granulation tissue and irregular marginal bone contour with respect to buccal aspect of #26, 27 were observed after growth excision [Figure 2e], were thoroughly debrided and root surfaces were planned followed by osteoplasty with surgical carbide bur [Figure 2f] under copious irrigation, respectively. Split thickness incision was given in the vestibule [Figure 2g] for tension-free advancement of CRF which was achieved [Figure 2h], and CRF was secured at the surgical site with 4-0 silk sutures [Figure 2i]. Coe-Pak was applied at the surgical site. Oral tablet ibuprofen 400 mg 8 hourly for 3 days and 0.2% chlorhexidine gluconate rinsing after 24 h were advised for 10 days postsurgically as per the previous oral hygiene protocol. The patient was recalled for suture removal on the 10th day postoperatively. Surgical site healed uneventfully, and sutures were removed on the 14th day postoperatively [Figure 3a]. Maintenance therapy was performed. Surgical site healed pleasingly without any residual soft tissue defect and its associated complications at 1 and 3 months postoperatively which will remain unaltered till 9-month postoperative follow-up [Figures 3b-3d].
Figure 2.
(a) Reduction in growth size observed; (b) the exploration of basal attachments of the growth; (c) peripheral extensions of the lesion observed after growth head excision; (d) internal bevel incision 1.5–2 mm away from the growth extensions, (e) surgical site showed granulation tissue and bony deformities; (f) after thorough debridement, the osteoplasty was proceeded; (g) vestibular partial-thickness incision; (h) tension-free coronal displacement of the flap; and (i) flap secured at the surgical site with 4-0 silk suture
Figure 3.
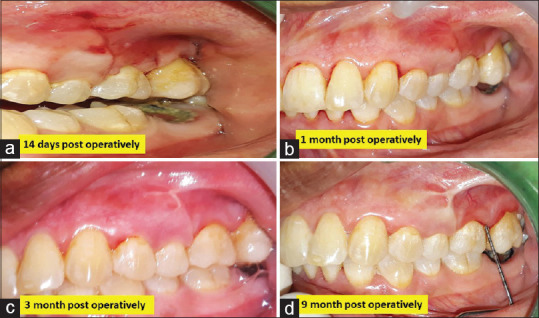
(a-d) Postoperative evaluation at 14 days showed that healing was uneventful, flap margin was well adapted to the underlying alveolar bone at 1 month, gingival margin showed a scalloped pattern with slight scar formation at the mesial vertical incision line at 3 months, and rest is same as 3 months healing except thick fibrosis at mesial releasing incision site at 9 months, respectively, without any recurrence
DISCUSSION
IF is observed and perceived usually as a fibrous polyp that may occur in the submucosal tissue in response to dental trauma or prosthesis.[1,2] It may be observed anywhere in the oral cavity. IF is a smooth surface lesion, usually 1.5 cm or less, sessile in nature without any color discrimination from the adjacent gingival tissue, observed commonly on the buccal mucosa along the bite line, and routinely reported in the fourth to sixth decade of life.[2] Somewhat similar clinical findings were observed in the present case of IF which was confirmed histologically. The present case was rare because (i) the size of the growth was ≥2 cm as it is generally reported to be ≤1.5 cm[1] and only few authors had reported its size from 4 to 6 cm,[3] (ii) it was observed in the posterior maxillary teeth,[4] whereas usually, it appears in the anterior maxilla, (iii) recurrence is rare, and (iv) extremely limited number of cases reported the simultaneous repair of residual soft tissue defect following excision of IF.[5,6]
IF was differentially diagnosed from POF which clinically looked similar but is usually <1.5 cm at its greatest dimensions, whereas histologically matured bone ossification in the connective tissue with plumb fibroblast is observed.[5] PG is routinely observedclinically on marginal and/or attached gingiva. The nature of the lesion is soft in consistency. On histologicalevaluationthe lesion in its early phase reveals diffuse endothelial cells with few budding capillaries; in lobular capillary hemangioma phase- numerous blood vessels organized into lobular aggregates whereas in involuntary phase showed healing of the lesion characterized by extensive fibrosis in the connective tissue. Although the clinical features of all the above reactive lesions overlap with IF, none of the characteristic histological findings of POF and PG was observed in the present case.[7]
Although the rate of recurrence of IF is low, it was reported in the present case. The reason for the same may be (a) local infuriating factors were not taken care following surgical management and (b) incomplete surgical excision.[2,5,6] The conceivable etiology in the existing reactive lesion may be because of the chronic interaction of local factors and/or toothbrush-associated insult.[6]
It is always a prodigious task for a periodontist while treating a recurrent large gingival reactive lesion, as extensive surgical excision might induce large residual soft tissue defect, which may provoke postoperative discomfort, sensitivity, difficulty in maintaining oral hygiene, etc.[5,6] Laterally, a displaced flap is difficult to execute in such location, whereas subepithelial connective tissue graft harvesting for the management of residual soft tissue defect is technique sensitive procedure too. Therefore, looking after the same, concurrent repair of anticipated residual soft tissue by CRF was planned and implemented in this case. CRF was planned on the basis of its primary requisite of the band of attached gingiva apical to the soft tissue defect and deep vestibule, which was well observed in the present case too, secondly, CRF isis less time-consuming, simple to learn and execute as well as because of its excellent outcome when coronally advance flap (CAF) was used alone[8,9] or in combination with platelet-rich fibrin (PRF)[4,6] or other materials.[10] Complete residual soft tissue defect coverage was obtained without any ill effects in the present case, which is consistent with the report of Salaria et al., but they utilized modified laterally displaced flap[6] and PRF in conjunction with CAF in the management of residual soft tissue defect.[7]
CONCLUSION
CRF was an effective treatment modality for preventing the functional difficulties that might be associated with residual soft tissue defect, following thorough surgical removal of recurrent IF.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors express special thanks to the Management of Surendera Dental College and Research Institute, for providing all kind of instruments, equipment, and technical expertise support needed for the case. Special thanks to Dr. Kathikeyan Ramalingam, Professor and Head, and Dr. Gurveen, Senior Lecture, Department of Oral and Maxillofacial Pathology, Surendera Dental College and Research Institute, for their kind support and timely help.
REFERENCES
- 1.Halim DS, Pohchi A, Pang EE. The prevalence of fibroma in oral mucosa among patient attending USM dental clinic year 2006-2010. Indonesian J Dent Res. 2010;1:61–6. [Google Scholar]
- 2.Babu B, Hallikeri K. Reactive lesions of oral cavity: A retrospective study of 659 cases. J Indian Soc Periodontol. 2017;21:258–63. doi: 10.4103/jisp.jisp_103_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kendrick F, Waggoner WF. Managing a peripheral ossifying fibroma. ASDC J Dent Child. 1996;63:135–8. [PubMed] [Google Scholar]
- 4.Das UM, Azher U. Peripheral ossifying fibroma. J Indian Soc Pedod Prev Dent. 2009;27:49–51. doi: 10.4103/0970-4388.50818. [DOI] [PubMed] [Google Scholar]
- 5.Salaria SK, Gupta N, Bhatia V, Nayar A. Management of residual mucogingival defect resulting from the excision of recurrent peripheral ossifying fibroma by periodontal plastic surgical procedure. Contemp Clin Dent. 2015;6:S274–7. doi: 10.4103/0976-237X.166832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salaria SK, Kaur S, Sharma I, Ramalingam K. Coronally advanced flap in conjunction with platelet-rich fibrin-assisted immediate management of residual gingival defect following surgical excision of recurrent pyogenic granuloma in the maxillary esthetic segment. J Indian Soc Periodontol. 2018;22:273–6. doi: 10.4103/jisp.jisp_94_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marla V, Shrestha A, Goel K, Shrestha S. The histological spectrum of pyogenic granuloma: A case series? Case Rep Dent. 2016;2016:1323798. doi: 10.1155/2016/1323798. doi: 10.1155/2016/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldstein M, Brayer L, Schwartz Z. A critical evaluation of methods for root coverage. Crit Rev Oral Biol Med. 1996;7:87–98. doi: 10.1177/10454411960070010601. [DOI] [PubMed] [Google Scholar]
- 9.Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian Soc Periodontol. 2015;19:66–71. doi: 10.4103/0972-124X.145790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chopra P, Kassal J, Masamatti SS, Grover HS. Comparative evaluation of clinical efficacy of coronally advanced flap alone and in combination with placental membrane and demineralized freeze-dried bone allograft in the treatment of gingival recession. J Indian Soc Periodontol. 2019;23:137–44. doi: 10.4103/jisp.jisp_308_18. [DOI] [PMC free article] [PubMed] [Google Scholar]



