Supplemental Digital Content is Available in the Text.
Evidence-informed guidance to better leverage, implement, and select virtual care platforms for pediatric chronic pain, and identified knowledge gaps are in need of additional research.
Keywords: Virtual care, Digital health, Chronic pain, Youth, Best practices, Guidelines, Systematic review
Abstract
The COVID-19 pandemic has acutely challenged health systems and catalyzed the need for widescale virtual care and digital solutions across all areas of health, including pediatric chronic pain. The objective of this rapid systematic review was to identify recommendations, guidelines, and/or best practices for using virtual care to support youth with chronic pain and their families (CRD42020184498). MEDLINE, CINAHL, Embase, APA PsychINFO, and Web of Science were searched the week of May 25, 2020, for English language peer-reviewed articles published since 2010 that (1) discussed children and adolescents aged <18 years reporting any type of chronic pain (ie, pain lasting >3 months); (2) focused on any type of virtual care (eg, telephone, telehealth, telemedicine, mHealth, eHealth, online, or digital); and (3) reported on guidelines, best practices, considerations, or recommendations for virtual care. Abstract and full text screening and data extraction were performed in duplicate. Meta-ethnography was used to synthesize concepts across articles. Of 4161 unique records screened, 16 were included addressing diverse virtual care and pediatric chronic pain conditions. Four key themes were identified: (1) opportunities to better leverage virtual care, (2) direct effective implementation of virtual care, (3) selection of virtual care platforms, and (4) gaps in need of further consideration when using virtual care to support youth with chronic pain and their families. No existing guidelines for virtual care for pediatric chronic pain were identified; however, best practices for virtual care were identified and should be used by health professionals, decision makers, and policymakers in implementing virtual care.
1. Introduction
The COVID-19 pandemic has acutely challenged health systems and catalyzed the need for widescale virtual care and digital solutions across all areas of health, including chronic pain,11,27 a common, undertreated, often debilitating disease and expensive public health issue.32,42,55 In response to challenges posed by the COVID-19 pandemic, health professionals and health systems pivoted from in-person to virtual delivery of ambulatory care on a large scale to respond to immediate needs (Killackey et al., under review). Virtual care refers to remote interactions between patients and health professionals using any form of communication or information technologies to facilitate delivery of effective, quality health care (eg, apps, videoconference, and telephone consultation).65 Virtual care is touted for its ability to facilitate rapid access to care for more people at reduced cost while also reducing the financial and time burdens of patients who may otherwise have to travel to hospital and risk virus exposure during the current COVID-19 pandemic.11 A recent report from the Canadian Medical Association revealed that Canadians have a high demand for virtual care that is not currently being met.75
Poor access to care for youth living with chronic pain is a long-standing problem.57 Indeed, before the COVID-19 pandemic, increasing access to pediatric chronic pain care was identified as a top patient-oriented research priority.9,18 The COVID-19 pandemic has significantly exacerbated difficulties accessing pain care because of initial closures of medical clinics and continued limited access to in-person therapies relevant for effective chronic pain management, such as psychological or physical interventions.21,27,64 Pain may also be worsened by exacerbation of other risk factors related to the pandemic such as inactivity, poor sleep, and social isolation.20 These impacts may be long-lasting because the prolonged stress and chronic pain experienced by youth today can influence their mental, physical, social, and occupational functioning well into adulthood.33,41,53,56,78,79 Early, effective, and accessible virtual treatments for pain in youth is critical to prevent the exacerbation of these persistent health issues. Research focused on youth and evidence-based virtual delivery of clinics and resources have identified mental health and chronic pain priorities for the COVID-19 pandemic.19,36 A variety of emerging, evidence-based digital treatments (apps, online modules, and telehealth clinics) exist to improve chronic pain management and mental health in youth and their parents; however, prepandemic implementation and uptake were sparse.25,27,30,43
To date, published guidance for adapting chronic pain management to virtual settings during the COVID-19 pandemic has been based on expert opinion without a systematic evidence review.27,64 Indeed, a systematic review of clinical practice guidelines developed rapidly and early in the COVID-19 pandemic (February–April 27, 2020) across different areas of health identified that most guidelines were of insufficient methodological quality due to a sole reliance on informal expert consensus (83% of 188 guidelines), with only 8 guidelines (4%) built on a systematic literature search and one guideline involving patients (<1%).67 The objective of the current rapid systematic review was to rigorously review the published literature to identify recommendations, guidelines, and/or best practices for using virtual care to support youth with chronic pain and their families. High-quality knowledge syntheses, such as this article, serve to enhance knowledge about a particular topic, thereby enabling evidence-informed decision making to guide implementation and policy across the health system.31,70 Knowledge syntheses form a critical foundation from which to develop clinical practice guidelines and to improve health care by reducing unwanted variability in care delivery,26 as is in pediatric chronic pain care both before18,57 and since the start of the COVID-19 pandemic (Killackey et al., under review). This article represents the first phase of a larger multimethods knowledge synthesis project identifying best practices and virtual care solutions across the stepped care continuum to support children and adolescents living with chronic pain and their families.
2. Materials and methods
This rapid systematic review protocol was registered in PROSPERO (CRD42020184498). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for systematic reviews guided the conduct and reporting of this review.46
2.1. Patient engagement
The team overseeing this rapid systematic review used a patient-oriented and patient-partnered approach,16,17 engaging 3 people with lived experience (patient and parent partners) as collaborators and equal members of the research team.49 The aim of collaborating with people with lived experience was to involve them in this review to ensure knowledge translation was meaningful and responsive to the needs of people for whom the evidence is most immediately relevant. Patient and parent partners were engaged in designing and overseeing the review, refining descriptions and examples of the emerging themes, and codeveloping knowledge translation outputs, including coauthorship of this publication. Specifically, patient and parent partners improved clarity of language of the described themes. Patient and parent partners also provided input to interpretation and presentation of the emerging themes to ensure diversity, equity, and inclusion.
2.2. Eligibility criteria
English language peer-reviewed scientific articles published in the past 10 years were identified for inclusion if they (1) discussed children and adolescents aged <18 years reporting any type of chronic pain (ie, pain lasting >3 months); (2) focused on any type of virtual care (eg, telephone, telehealth, telemedicine, mHealth, eHealth, online, and digital); and (3) reported on guidelines, best practices, considerations, or recommendations for virtual care. All article types were considered eligible (eg, systematic reviews or meta-analyses, clinical practice guidelines, editorials, commentaries, and qualitative studies); however, primary studies with the identified purpose of evaluating the effectiveness of virtual care were excluded (eg, randomized controlled trials and nonrandomized treatment studies) because they are included in a subsequent scoping review mapping all virtual care solutions for pediatric chronic pain.
2.3. Search strategy and conduct
The search strategy was developed in collaboration with a medical research librarian (D.L.L). Database searches were conducted in MEDLINE, CINAHL, Embase, APA PsychINFO, and Web of Science during the week of May 25, 2020. A sample search strategy is available in Supplementary Material 1 (available at http://links.lww.com/PR9/A108).
2.4. Screening and selection
Three research assistants or clinical research coordinators screened all abstracts and subsequent full-text articles for eligibility, in duplicate using Covidence.22 Disagreements were resolved by consultation with 2 other authors (K.A.B. and T.K.) as needed.
2.5. Data extraction and synthesis
Data extraction and synthesis were conducted independently by 2 team members (K.A.B. and T.K.) with disagreements resolved through consensus. Extracted data included the following: author; publication year; article type; and type(s) of virtual care; key concepts, recommendations, or guidelines identified for virtual care. Articles were also coded for their relevance to level(s) of stepped care (steps 1–5).52 Stepped care models enable matching of levels of care to individual need from self-guided resources up to tertiary, specialist care. Stepped care is a patient-oriented model recommended by the Canadian Pain Task Force19 and the Mental Health Commission of Canada,52 is a framework increasingly applied in chronic pain care,2,7,60 and is well-suited for addressing the expected surge of youth mental health needs during and postdisaster.51
Stepped care levels were coded as follows:
(1) Level 1: self-guided (whole population; eg, apps and educational websites).
(2) Level 2: peer-to-peer (low needs; eg, real-time peer support).
(3) Level 3: minimal health professional involvement (moderate needs; eg, real-time psychoeducational workshop, health professional-assisted e-supports [through app or website]).
(4) Level 4: ongoing real-time health professional interaction (high needs; eg, online individual or group programming).
(5) Level 5: real-time specialist health professional(s) (complex needs; eg, tertiary interdisciplinary clinic).
Meta-ethnographic techniques were used to synthesize concepts, recommendations, and guidelines that commonly occurred across articles.5,54 Meta-ethnography is a widely accepted form of qualitative synthesis involving translation of findings from primary studies into one another, in order for overarching themes or concepts to emerge.5,54 Specific steps include the following: determining the research question, determining the scope of the synthesis, reading the articles, determining how the articles are related, identifying themes, synthesizing themes across articles, and reporting the synthesis.5,54 Although various article types were included in this review, for the purposes of data extraction and synthesis, all content included in the published articles was treated as qualitative data. This strategy was used given the authors' expectation of a lack of rigorously developed clinical practice guidelines focused on provision of virtual care for children and adolescents with chronic pain, as well as the pressing pragmatic need in light of the COVID-19 pandemic to offer evidence-informed guidance to health care providers and decision makers supporting this population. Each article was read multiple times and the key concepts identified. A table was created describing concepts from each article and then synthesized across articles. Concepts that were described in only one article were also retained.
Our original systematic review protocol indicated that identified articles would be coded for quality as assessed using AGREE II for guidelines.12,13 This method was not ultimately used because specific guidelines were not identified and the AGREE II tool was not deemed appropriate.
3. Results
3.1. Study selection
Database searches identified 6334 records. Three additional articles known to the study authors published since the start of the COVID-19 pandemic were also included. After duplicates were removed, 4161 unique abstracts remained for review. Of these, 4101 were deemed not eligible. A total of 60 full texts were reviewed, of which 44 were excluded. Sixteen full texts met inclusion criteria. Refer to Figure 1 for the PRISMA review flowchart, including reasons for full-text exclusion.
Figure 1.
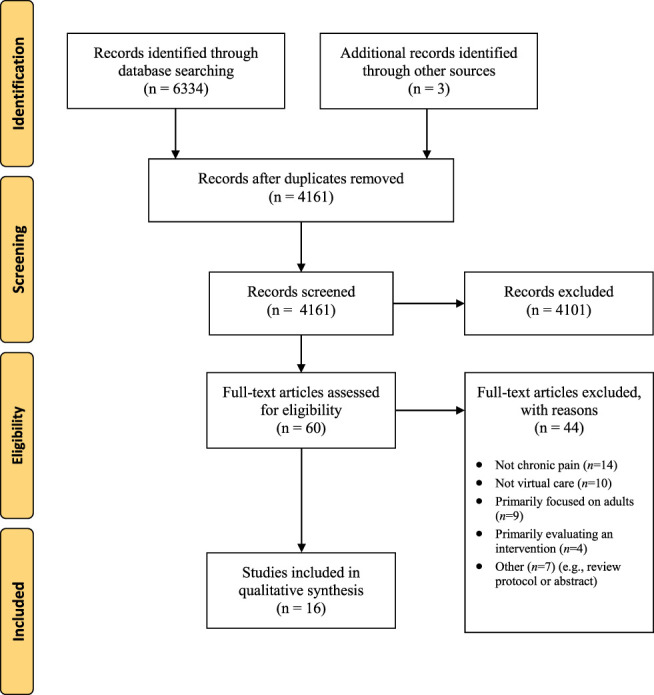
PRISMA flow diagram.
3.2. Study characteristics
Of the 16 articles meeting review inclusion criteria, 10 were scoping or systematic reviews or meta-analyses,14,30,34,62,66,68,69,71,73,74 3 were commentaries or editorials or opinion articles,27,28,38 2 were qualitative studies,37,76 and one was a nonsystematic literature review.44 Refer to Table 1 for a summary of data extracted from each article. Articles were from a variety of countries, including 4 articles each from Canada,28,37,44,69 the United States,34,38,66,68 and the United Kingdom14,27,30,74; 2 articles from Australia62,76 ; one from China71; and one from New Zealand.73 Most of these articles shared comparable health care contexts and focus on publicly funded health systems, although variety is noted. Articles addressed virtual care for a variety of chronic pain conditions, including headaches, migraines, musculoskeletal pain, recurrent abdominal pain, chronic widespread pain or fibromyalgia, and pain associated with arthritis, postconcussion, sickle cell disease, and irritable bowel syndrome. Types of virtual care discussed included apps, telephone support, virtual peer-to-peer, and web-based self-management with or without coach support. Most articles addressed lower levels of the stepped care continuum, such as apps, educational websites, and peer support interventions (Table 1).
Table 1.
Description of included articles.
| Author, year | Article type | Pediatric chronic pain population | Description of virtual care included | Relevance to Level of Stepped Care Continuum | ||||
|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | ||||
| Caes, 201814 | Systematic review (or meta-analysis) | Chronic musculoskeletal pain: JIA and fibromyalgia | Online remote delivery of psychological interventions | Yes | Yes | Yes | No | No |
| Eccleston, 202027 | Commentary or editorial or opinion | Chronic pain: SCD, musculoskeletal, JIA, and headache | Telemedicine, remotely delivered self-management programs, and psychological therapies delivered through the internet or mobile apps | No | Yes | Yes | Yes | Yes |
| Ellis, 201928 | Commentary or editorial or opinion | Migraine headache | Telemedicine | No | No | No | Yes | Yes |
| Fisher, 201930 | Systematic review (or meta-analysis) | Headache, JIA, SCD, IBS, recurrent abdominal pain, and musculoskeletal pain | Remote delivery of psychological interventions (eg, internet, smartphone applications, or CD-ROMs) | Yes | Yes | Yes | No | No |
| Harrison, 201934 | Systematic review (and/or meta-analysis) | Functional abdominal pain (FAP) and chronic pain | Online remote delivery of psychological interventions | Yes | Yes | Yes | No | No |
| Huguet, 201437 | Qualitative study (survey or interviews) | Headache | Online remote delivery of psychological interventions (smartphone pain diary, internet-based self-management treatment, and social support) | Yes | Yes | Yes | No | No |
| Hunter, 201838 | Commentary or editorial or opinion | Acute and chronic pain | Apps and websites | Yes | Yes | Yes | Yes | Yes |
| Lalloo, 201444 | Book chapter | JIA | Pain assessment apps and electronic pain diaries | Yes | No | No | No | No |
| Schults, 201962 | Scoping review | JIA, SCD, fibromyalgia, headache, and persistent pain | Apps | Yes | Yes | No | No | No |
| Smith, 201566 | Systematic review (or meta-analysis) | Chronic pain | Apps | Yes | Yes | No | No | No |
| Stiles Shields, 201968 | Systematic review (or meta-analysis) | Chronic pain (n = 5 articles), chronic fatigue syndrome (n = 1), JIA (n = 1), and cerebral palsy (n = 2) | Web-based or app-based self-management programs (75% included real-time professional support) | Yes | Yes | Yes | Yes | No |
| Stinson, 201369 | Systematic review (or meta-analysis) | Recurrent headache, JIA, and SCD | E-diaries on a handheld device | Yes | No | No | No | No |
| Tang, 201871 | Systematic review (or meta-analysis) | Chronic pain and headache | Online remote delivery of psychological interventions | Yes | Yes | Yes | No | No |
| Thabrew, 201873 | Systematic review (or meta-analysis) | Chronic idiopathic pain, abdomen pain, MSK pain, multiple pain areas, headache, and chronic respiratory illness (cystic fibrosis, asthma, and others) | Remote delivery of psychological interventions (eg, static or interactive websites, automated emails, or web-based applications, automated phone calls or short text messages, or mobile websites or smartphone applications). | Yes | Yes | Yes | No | No |
| Velleman, 201074 | Systematic review (or meta-analysis) | Headache, recurrent abdominal pain, and MSK pain | Online remote delivery of psychological interventions | Yes | Yes | Yes | Yes | No |
| Waite Jones, 201876 | Qualitative study (survey or interviews) | JIA | Apps (self-management, symptom tracking, and social support) | Yes | Yes | No | No | No |
IBS, irritable bowel syndrome; JIA, juvenile idiopathic arthritis; MSK, musculoskeletal; SCD, sickle cell disease.
3.3. Synthesis of results
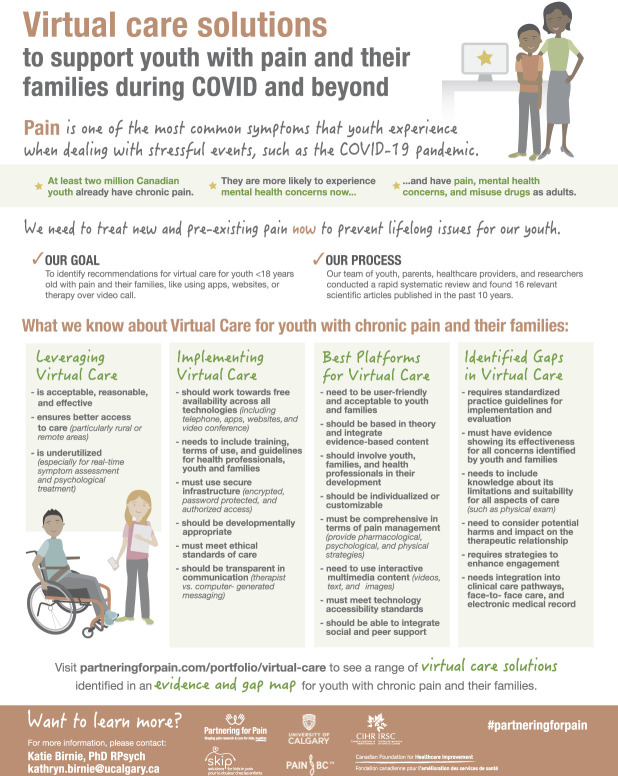
Meta-ethnography across the 16 articles identified 4 key themes: (1) opportunities to better leverage virtual care (theme 1), (2) direct effective implementation of virtual care (theme 2), (3) selection of virtual care platforms (theme 3), and (4) gaps in need of further consideration when using virtual care (theme 4) to support youth with chronic pain and their families. Key points related to each theme are synthesized in Figure 2 (available for download: www.partneringforpain.com/portfolio/virtual-care).
Figure 2.
Best practices for virtual care to support children and adolescents with chronic pain and their families.
3.3.1. Theme 1: leveraging virtual care
Virtual care for youth with chronic pain and their families has been described as acceptable,71 reasonable,73 and effective.14,34,71,73 Various studies included in this review reported that virtual care interventions resulted in significant reductions in pain,34,38 anxiety, and depressive symptoms,71 as well as improvements in sleep.71 Although according to Fisher et al.30 there is insufficient evidence to determine that virtual psychological therapies can reduce pain severity or other symptoms associated with chronic pain, there are encouraging outcomes resulting from some studies included in this review. Specifically, interventions such as internet-delivered cognitive behavioural therapy71 or computer-delivered cognitive behavioural therapy74 both demonstrated clinically significant improvements in pain and mental health symptoms (eg, anxiety). Overall, the quality of evidence is low due to the small samples and fairly heterogeneous group of studies available, and therefore there is a need for more randomized controlled trials to increase understanding of the efficacy of these treatments.30,73,74
The use of virtual care can ensure better access to care, particularly in rural or remote areas.34,38 Multidisciplinary and multimodal pain treatments are not always available to pediatric patients, and therefore innovative virtual care solutions may be especially useful in this population.38 However, virtual care remains underutilized, especially for real-time symptom assessment and psychological treatment. Many existing technologies or applications have not been widely disseminated or are unable to sustain prolonged engagement with users, which signals low uptake.38 Overall, there are significant opportunities to better leverage virtual care in the pediatric population with chronic pain going forward.
3.3.2. Theme 2: implementing virtual care
This review identified key considerations for the implementation of virtual care in the pediatric population with chronic pain. Virtual care for youth with chronic pain and their families should work towards being freely available across all technologies, including but not limited to telephone, apps, websites, and videoconference.27 Virtual care implementation should include training, terms of use, and guidelines for health professionals, youth, and families.27,37 As Eccleston et al.27 noted that understanding who struggles to engage and use virtual care solutions is crucial to ensure effectiveness, along with supporting training needs of staff who are accustomed to providing face-to-face pain care.27,37 Huguet et al.37 outlined that guidelines for the use of the virtual care solution should be created, clearly understood by participants and also enforced by a system administrator (ie, users should be taught not to post identifying information). In their qualitative study exploring what users want in virtual health technology, one of the main concerns articulated by potential users was the risk of breaching privacy issues,37 and therefore platforms should use secure infrastructure (ie, encrypted, password protected, and authorized access).37 In addition to privacy and training considerations, virtual care solutions should be developmentally appropriate, meet ethical standards of care, and be transparent in communication (ie, clearly indicate whether content is being shared by a therapist vs computer-generated messaging).27 Privacy was repeatedly raised as a critical ethical issue requiring greater consideration in virtual care, in addition to liability and monitoring of peer-to-peer discussions for incorrect information.27,37,76 Overall, implementation of virtual care requires careful consideration of many aspects related to accessibility, training, privacy, and security to ensure that users feel confident and safe to use this technology.
3.3.3. Theme 3: selecting virtual care platforms
Multiple sources noted that platforms used to provide virtual care for youth with chronic pain and their families should be user-friendly and acceptable to youth and families. Youth, families, and health professionals should be involved in the development and testing process of various virtual care platforms, such as user-centered design37,38,62,69; codesigning virtual care interventions with participants allows for improved acceptability and engagement with target audiences.73 Importantly, platforms should be theoretically sound and integrate evidence-based content shown to be effective when delivered through that platform66; as mentioned, more high-quality trials testing the effectiveness of virtual care interventions are needed.62,71 When selecting a platform, the opportunity to individualize or customize the technology to the youth and family's needs is beneficial,37,38 as is the use of interactive multimedia content (eg, videos, text, and images) to enhance engagement. For example, in the study by Huguet et al.,37 participants described wanting the ability to decide the content and format of a pain reporting diary, flexibility for entering information in the diary, and the ability to create personalized profiles and set notifications for specific activities (eg, medication reminders). Furthermore, youth have stressed the importance of app ownership, and the ability to choose how and when to use these apps, and control the apps' presentation and its interactivity.76 Overall, virtual care technologies should be comprehensive in pain management offerings (ie, provide pharmacological, psychological, and physical strategies). However, a recent review of existing Apple (iOS) applications for pediatric pain and pain-related stress demonstrated that none of the apps were considered to be sufficiently comprehensive to be an independent alternative to psychological services.66 Finally, it is recommended that platforms be age-, gender-, and developmental stage-appropriate and be able to integrate social and peer support.37,62,76
3.3.4. Theme 4: identified gaps in virtual care
As noted by Smith et al.,66 “there are currently no established guidelines for app-related real-time communications (eg, direct text or video messaging communications between app users or with a health care provider), meaning that providers must think critically about the use of these communication features before integrating them into practice” (p. 105). In addition, there is a need for robust evidence demonstrating the effectiveness of virtual care solutions.14,38 Further investigation is also needed regarding the limitations of virtual care and suitability for all aspects of care (eg, conducting physical examinations virtually).27 Although there are many benefits of harnessing virtual care technologies, there is a need to consider the potential harms and impact (positive or negative) on the therapeutic relationship, as well as strategies to enhance uptake and ongoing engagement with virtual interventions over extended periods.38 Addressing accessibility for people with disabilities is required as few studies have examined, tracked, or reported specifically on this.27,38 Finally, there is a need to ensure virtual care solutions are integrated into existing clinical care pathways, in-person care, and the electronic medical record.14 A thorough list of research priorities for virtual care for individuals with chronic pain during the COVID-19 pandemic was additionally outlined in one of the included articles.27
4. Discussion
The objective of this rapid systematic review was to identify recommendations, guidelines, and/or best practices for using virtual care to support youth with chronic pain and their families. Previous practice recommendations were rapidly developed based on expert consensus early during the COVID-19 pandemic21,27,64; this review builds on this work by providing a rigorous and rapid review of the literature. Unfortunately, no pre-existing guidelines were identified to support effective implementation of quality virtual care for youth living with chronic pain and their families. Our review identified an urgent need for the development of such standardized practice guidelines for the implementation and evaluation of virtual care for youth with chronic pain and their families. However, 16 peer-reviewed articles reporting scoping or systematic reviews or meta-analyses,14,30,34,62,66,68,69,71,73,74 commentaries or editorials or opinion articles,27,28,38 qualitative studies,37,76 or nonsystematic literature review44 provided evidence to inform best practice recommendations. Qualitative synthesis across articles identified key themes when using virtual care to support youth with chronic pain and their families, including (1) opportunities to better leverage virtual care, (2) effective implementation of virtual care, (3) selection of best virtual care platforms, and (4) identified knowledge gaps in need of further research. The need for timely decisions on health care and health policy is a key indication for conducting a rapid review.63 The rapid nature of this review and creation of a 1-page infographic was conducted with the goal of stimulating immediate practice change, based on the best available evidence, without delay.63
This article represents the first phase of a larger multimethods knowledge synthesis project identifying best practices and virtual care solutions to support children and adolescents living with chronic pain and their families. The second phase is creation of an interactive Evidence and Gap Map of virtual care solutions across the stepped care continuum for children and adolescents with chronic pain and their families (Birnie et al., under review). The Evidence and Gap Map synthesizes virtual care solutions identified from the scientific literature, apps and websites, and a call for emerging and demonstrated innovations in virtual care for pediatric chronic pain. A full project description and outputs from all project phases are available online: www.partneringforpain.com/portfolio/virtual-care.
In response to the COVID-19 pandemic, researchers, health professionals, and policymakers have called for better access to virtual care to support individuals with chronic pain.19,21,27,58,64 Consensus recommendations from multiple international panels of adult chronic pain health professionals identified the value of telemedicine (virtual care) to manage pain during the COVID-19 pandemic and need to ensure selected technology is easy to use, maintains confidentiality of personal health information, and is ethically delivered as per health professional jurisdictional requirements.21,58,64 Issues related to opioid prescribing, the provision of interventional treatments, and comorbidities for increased risk of adverse COVID-19 outcomes are also discussed,21,27,58,64 albeit generally less relevant to pediatric populations with chronic pain. The most thorough provision of practical recommendations for introducing pain management strategies virtually during the COVID-19 pandemic are provided by Eccleston et al.27 in an article included in the current review. They outline guidance for the best use of technology platforms, navigating technical challenges, scheduling considerations, use of complementary or combined virtual resources (eg, apps or websites in combination with remote sessions with health professional), flexibility in approach, and pain self-management strategies (ie, positive reinforcement, problem solving, experiential learning, and goal setting).27 Findings from the current systematic review of the literature expand on published recommendations for virtual chronic pain care in the time of the COVID-19 pandemic based on expert opinion by providing additional guidance for implementation and selection of virtual care platforms particularly related to cost, accessibility, usability, suitability and developmental appropriateness, and customizability, specifically for the pediatric population.
Some guidance regarding the use of virtual care during the COVID-19 pandemic has been predominantly physician centric.3 Given the evidence-based multimodal approach to pediatric chronic pain care,47 there is a need to ensure virtual chronic pain care comprehensively address pharmacological, psychological, and physical treatments. Currently, much of the discussion surrounding virtual care for chronic pain supports the delivery of psychological interventions (ie, cognitive behavioural therapy).14,30,34,71 This mirrors the proportionally larger evidence base for psychological interventions—as opposed to pharmacological or physical interventions—delivered digitally for pediatric chronic pain,10 as well as the ease of delivering psychological interventions remotely. Furthermore, the added psychological burden of the COVID-19 pandemic is present59 such that virtual psychological treatment of mental health of children and adolescents is also an identified priority.4,36 Notably, the use of a variety of information technologies is covered in this review (eg, email, apps, websites, and videoconference platforms); however, as the evidence develops for virtual or augmented reality for pediatric chronic pain, specific additional considerations may be needed,27,60,81 particularly to address the challenges posed by remote physical therapies. There is also further need to address the challenges related to virtual physical examinations for pain.25,72 This current review identified articles focused predominantly on virtual care at lower levels of the stepped care continuum (eg, apps and websites). This is important to note because best practices for virtual care identified here do not incorporate evidence from virtual care interventions higher in the stepped care continuum (eg, tertiary care interdisciplinary chronic pain clinics) that are rapidly being delivered remotely in response to the COVID-19 pandemic.25 This speaks to the need for iterative refinement of these guidelines for virtual care for pediatric chronic pain as new evidence and learnings emerge.
The long-standing call for increased access to chronic pain care is one of equity, diversity, and inclusion.9,18,19 However, virtual care is not the panacea. Although virtual care offers the potential for better access to care for those living in rural and remote areas as identified by articles in this review, this is not a guarantee. The COVID-19 pandemic has shone a spotlight on social inequities, including in digital health.24 Individuals who live outside of urban centers face slower, less reliable access to the internet, and challenges with affordability of high-speed connectivity.39 Barriers to accessing digital health care include lack of access to technology required, low technical literacy, or poor engagement with digital health.24 Strategies for addressing inequities within the health system include equal access to digital health care and equal outcomes from this care irrespective of social factors, health professional training, consideration of necessary adaptations, integrated measurement and quality improvement, and involvement of people from vulnerable groups in codesign.24 Aligned with this, findings from this review stress the importance of virtual care to include training for health professionals, being accessible to people with disabilities, include empirical evaluation and evidence-based content, and involve youth, families, and health professionals in their development (ie, user-centered design). Although authors of included articles mentioned the importance of accessibility, this concept was not defined beyond emphasizing the importance of enabling access to people with disabilities. Compliance with existing established technology accessibility standards, such as the Web Content Accessibility Guidelines, including for mobile (WCAG 2.0)82 and for web developers may be useful for ensuring virtual platforms and content are perceivable, operable, understandable, and robust to people with a wide range of disabilities, including blindness and low vision, deafness and hearing loss, learning disabilities, cognitive limitations, limited movement, speech disabilities, photosensitivity, and combinations of these. In addition, much of the research contributing to this review may disproportionately represent White populations. To address this, our group is seeking input regarding the best practices for virtual care identified here with specific groups at-risk for inequities in chronic pain care,1,23 including Black youth living with sickle cell disease,40,77 indigenous youth with chronic pain,45,50,83 and youth with medical complexities6 and their families. Stepped care approaches to chronic pain care are increasingly recommended,2,19,60 as are potential hub-and-spoke models,28 to reach rural and remote communities.
Overall, these results highlight that virtual care was underutilized prepandemic for youth with chronic pain, and given the current COVID-19 pandemic and associated restrictions with widespread virtual care implementation, there is an urgent need for evidence-based guidelines to direct virtual care practices. Furthermore, some identified best practices from articles included in this review may be less relevant today given the rapid advancement of technology over the past 10 years; certain aspects of virtual care may be more common today such as standard integration of customizability and/or use of multimedia content. Despite the evaluation of virtual care for pediatric chronic pain before the COVID-19 pandemic, there remain numerous empirical questions for consideration. Health systems decision makers and health professionals require best practice guidelines to select, implement, and evaluate virtual care practices. Specifically, recommendations are needed to ensure virtual care platforms and technologies provide comprehensive and evidence-based pain management, suitable to the patient population, safe, accessible, and use design methodologies, such as human-centered design and design thinking,35,61 that integrate the input from end users to ensure patient-centered care in a post-COVID-19 digital world.11
This review also revealed the need to include routine collection of patient-reported outcomes to evaluate the efficacy of care delivered virtually.8 Implementation science approaches are highly recommended to collect and analyze “real-world” data in the rapidly evolving COVID-19 context.80 Examples include the collection of quality improvement data for implementation of virtual care within clinical programs or use of rapid, iterative research evaluation designs, such as the mHealth agile development and evaluation lifecycle model.60 Specific frameworks also exist to guide evaluation of virtual care.15,29
This review is limited by the quantity and quality of existing evidence to guide virtual care implementation for youth with chronic pain. Because of the rapid nature of the review, the scope of the search strategy was restricted by date range and English language alone. It is possible that studies were also missed that focused on other dimensions or sources of chronic pain that were not included. Unfortunately, there are no existing best practice guidelines or evidence-based recommendations for the use of virtual care in this unique population, and therefore a rigorous assessment of guideline quality (ie, using the AGREE II tool as planned) was not possible. Furthermore, although this review examined youth with existing chronic pain complaints, emerging research indicates the potential for new onset chronic pain among youth.48 As such, it does not adequately address best practices for virtual care for the prevention of new onset chronic pain.
In light of the current COVID-19 pandemic, the chronic pain crisis, and the rapid shift to the use of virtual care,1,2 it is essential that existing evidence-based virtual care recommendations are identified to guide practice. The results of this systematic review should be used to inform ongoing decision making by health professional, decision makers, and policymakers regarding best practices for virtual delivery of chronic pain care for youth and their families.
Disclosures
The authors have no conflicts of interest to declare.
This work was funded by a COVID-19 Rapid Research Funding Opportunity in Mental Health and Substance Use Knowledge Synthesis Grant from the Canadian Institutes of Health Research (CIHR). Project partners include Solutions for Kids in Pain (SKIP), Pain BC, and the Canadian Foundation for Healthcare Improvement (CFHI; now called Healthcare Excellence Canada [HEC]).
Appendix A. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PR9/A108.
Supplementary Material
Acknowledgments
The authors thank Laura Harris, Mallika Makkar, and Brittany Wiles for their research assistance. The authors also thank Kari Tiffin from Bright By Design Inc for the graphic design.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painrpts.com).
Contributor Information
Tieghan Killackey, Email: tieghan.killackey@sickkids.ca.
Jennifer Stinson, Email: jennifer.stinson@sickkids.ca.
Melanie Noel, Email: melanie.noel@ucalgary.ca.
Diane L. Lorenzetti, Email: dllorenz@ucalgary.ca.
Justina Marianayagam, Email: justina.marianayagam@gmail.com.
Isabel Jordan, Email: isabeljordan@me.com.
Evie Jordan, Email: eviejmjordan@icloud.com.
Alexandra Neville, Email: alexandra.neville@ucalgary.ca.
Maria Pavlova, Email: mpavlova@ucalgary.ca.
Fiona Campbell, Email: fiona.campbell@sickkids.ca.
Chitra Lalloo, Email: chitra.lalloo@sickkids.ca.
References
- [1].Anastas TM, Miller MM, Hollingshead NA, Stewart JC, Rand KL, Hirsh AT. The unique and interactive effects of patient race, patient socioeconomic status, and provider attitudes on chronic pain care decisions. Ann Behav Med 2020;54:771–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Anderson DR, Zlateva I, Coman EN, Khatri K, Tian T, Kerns RD. Improving pain care through implementation of the Stepped Care Model at a multisite community health center. J Pain Res 2016;9:1021–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Anthony B, Jr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst 2020;44:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Asmundson GJG, Blackstock C, Bourque MC, Brimacombe G, Crawford A, Deacon SH, McMullen K, McGrath PJ, Mushquash C, Stewart SH, Stinson J, Taylor S, Campbell-Yeo M. Easing the disruption of COVID-19: supporting the mental health of the people of Canada. Canada: Royal Society of Canada, 2020. Available at: https://rsc-src.ca/en/research-and-reports/easing-disruption-covid-19-supporting-mental-health-people. [Google Scholar]
- [5].Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Barney CC, Andersen RD, Defrin R, Genik LM, McGuire BE, Symons FJ. Challenges in pain assessment and management among individuals with intellectual and developmental disabilities. Pain Rep 2020;5:e821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bell L, Cornish P, Gauthier R, Kargus C, Rash J, Robbins R, Ward S, Poulin PA. Implementation of the Ottawa Hospital Pain Clinic stepped care program: a preliminary report. Can J Pain 2020;4:168–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bhandari RP, Feinstein AB, Huestis SE, Krane EJ, Dunn AL, Cohen LL, Kao MC, Darnall BD, Mackey SC. Pediatric-Collaborative Health Outcomes Information Registry (Peds-CHOIR): a learning health system to guide pediatric pain research and treatment. PAIN 2016;157:2033–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Birnie KA, Dib K, Ouellette C, Dib MA, Nelson K, Pahtayken D, Baerg K, Chorney J, Forgeron P, Lamontagne C, Noel M, Poulin P, Stinson J. Partnering for Pain: a Priority Setting Partnership to identify patient-oriented research priorities for pediatric chronic pain in Canada. CMAJ Open 2019;7:E654–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Birnie KA, Ouellette C, Do Amaral T, Stinson JN. Mapping the evidence and gaps of interventions for pediatric chronic pain to inform policy, research, and practice: a systematic review and quality assessment of systematic reviews. Can J Pain 2020;4:129–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Boissy A. Getting to patient-centered care in a post–covid-19 digital world: a proposal for novel surveys, methodology, and patient experience. NEJM Catal Innov Care Deliv 2020. doi: 10.1056/CAT.19.1106. [Google Scholar]
- [12].Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L. For the AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. Can Med Assoc J 2010;182:E839–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Hanna SE, Makarski J, for the AGREE Next Steps Consortium. Development of the AGREE II, part 2: assessment of validity of items and tools to support application. Can Med Assoc J 2010;182:E472–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Caes L, Fisher E, Clinch J, Eccleston C. Current evidence-based interdisciplinary treatment options for pediatric musculoskeletal pain. Curr Treatm Opt Rheumatol 2018;4:223–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Canada Health Infoway. Benefits evaluation indicators. Ottawa: Canada Health Infoway, 2012. Available at: https://www.infoway-inforoute.ca/en/resource-centre/toolkits/benefits-evaluation-toolkit. Accessed April 2, 2021. [Google Scholar]
- [16].Canadian Institutes of Health Research. Patient engagement. 2018. Available at: www.cihr-irsc.gc.ca/e/45851.html. Accessed April 2, 2021. [Google Scholar]
- [17].Canadian Institutes of Health Research. Strategy for patient-oriented research: patient engagement framework. Ottawa: Canadian Institutes of Health Research, 2019. p. 1–19. Available at: http://www.cihr-irsc.gc.ca/e/48413.html. Accessed April 2, 2021. [Google Scholar]
- [18].Canadian Pain Task Force. Chronic pain in Canada: laying a foundation for action. Government of Canada, 2019. Available at: https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2019.html#pre. Accessed April 2, 2021. [Google Scholar]
- [19].Canadian Pain Task Force. Working together to better understand, prevent, and manage chronic pain: what we heard. Ottawa: Health Canada, 2020. p. 75. Available at: https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2020.html. Accessed April 2, 2021. [Google Scholar]
- [20].Clauw DJ, Häuser W, Cohen SP, Fitzcharles M-A. Considering the potential for an increase in chronic pain following the COVID-19 pandemic. PAIN 2020;161:1694–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cohen SP, Baber ZB, Buvanendran A, McLean LTCBC, Chen Y, Hooten WM, Laker SR, Wasan WAD, Kennedy DJ, Sandbrink F, King LTCSA, Fowler CDRIM, Stojanovic MP, Hayek SM, Phillips CDRCR. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Med 2020;21:1331–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Covidence. Australia: Veritas health innovation. 2019. Available at: www.covidence.org. Accessed April 2, 2021. [Google Scholar]
- [23].Craig KD, Holmes C, Hudspith M, Moor G, Moosa-Mitha M, Varcoe C, Wallace B. Pain in persons who are marginalized by social conditions. PAIN 2019;161:261–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Crawford A, Serhal E. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res 2020;22:e19361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].D'Alessandro L, Brown SC, Campbell F, Ruskin D, Mesaroli G, Stinson JN. Rapid mobilization of a virtual pediatric chronic pain clinic in Canada during the COVID-19 pandemic. Can J Pain 2020. 4:162–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Eccles MP, Grimshaw JM, Shekelle P, Schünemann HJ, Woolf S. Developing clinical practice guidelines: target audiences, identifying topics for guidelines, guideline group composition and functioning and conflicts of interest. Implement Sci 2012;7:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, Palermo TM, Reid MC, Williams ACC. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. PAIN 2020;161:889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ellis MJ, Russell K. The potential of telemedicine to improve pediatric concussion care in rural and remote communities in Canada. Front Neurol 2019;10:840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Fatehi F, Smith AC, Maeder A, Wade V, Gray LC. How to formulate research questions and design studies for telehealth assessment and evaluation. J Telemed Telecare 2017;23:759–63. [DOI] [PubMed] [Google Scholar]
- [30].Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2019;4:CD011118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N. Lost in knowledge translation: time for a map? J Contin Edu Health Prof 2006;26:13–24. [DOI] [PubMed] [Google Scholar]
- [32].Groenewald CB, Essner BS, Wright D, Fesinmeyer MD, Palermo TM. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. J Pain 2014;15:925–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Groenewald CB, Law EF, Fisher E, Beals-Erickson SE, Palermo TM. Associations between adolescent chronic pain and prescription opioid misuse in adulthood. J Pain 2019;20:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Harrison LE, Pate JW, Richardson PA, Ickmans K, Wicksell RK, Simons LE. Best-evidence for the rehabilitation of chronic pain part 1: pediatric pain. J Clin Med 2019;8:1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Harte R, Glynn L, Rodríguez-Molinero A, Baker PM, Scharf T, Quinlan LR, ÓLaighin G. A human-centered design methodology to enhance the usability, human factors, and user experience of connected health systems: a three-phase methodology. JMIR Hum Factors 2017;4:e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Worthman CM, Yardley L, Cowan K, Cope C, Hotopf M, Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Huguet A, Stinson J, MacKay B, Watters C, Tougas M, White M, McGrath PJ. Bringing psychosocial support to headache sufferers using information and communication technology: lessons learned from asking potential users what they want. Pain Res Manag 2014;19:E1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Hunter JF, Kain ZN, Fortier MA. Pain relief in the palm of your hand: harnessing mobile health to manage pediatric pain. Paediatr Anaesth 2019;29:120–4. [DOI] [PubMed] [Google Scholar]
- [39].Innovation, Science and Economic Development Canada. High-speed access for all: Canada's connectivity strategy. Ottawa: Government of Canada, 2019. Available at: www.canada.ca/high-speed-access-for-all. Accessed April 2, 2021. [Google Scholar]
- [40].Jenerette CM, Brewer C. Health-related stigma in young adults with sickle cell disease. J Natl Med Assoc 2010;102:1050–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kashikar-Zuck S, Cunningham N, Sil S, Bromberg M, Lynch-Jordan AM, Strotman D, Peugh J, Noll J, Ting TV, Powers SW, Lovell DJ, Arnold LM. Long-Term outcomes of adolescents with juvenile-onset fibromyalgia in early adulthood. Pediatr 2014;133:e592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. PAIN 2011;152:2729–38. [DOI] [PubMed] [Google Scholar]
- [43].Lalloo C, Jibb LA, Rivera J, Agarwal A, Stinson JN. “There's a pain app for that”: review of patient-targeted smartphone applications for pain management. Clin J Pain 2015;31:557–63. [DOI] [PubMed] [Google Scholar]
- [44].Lalloo C, Stinson JN. Assessment and treatment of pain in children and adolescents. Best Pract Res Clin Rheumatol 2014;28:315–30. [DOI] [PubMed] [Google Scholar]
- [45].Latimer M, Rudderham S, Lethbridge L, MacLeod E, Harman K, Sylliboy JR, Filiaggi C, Finley GA. Occurrence of and referral to specialists for pain-related diagnoses in First Nations and non–First Nations children and youth. Can Med Assoc J 2018;190:E1434–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Liossi C, Howard RF. Pediatric chronic pain: biopsychosocial assessment and formulation. Pediatrics 2016;138:e20160331. [DOI] [PubMed] [Google Scholar]
- [48].Liu S, Liu Y, Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res 2020;289:113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Manafò E, Petermann L, Vandall-Walker V, Mason-Lai P. Patient and public engagement in priority setting: a systematic rapid review of the literature. PLoS One 2018;13:e0193579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Matthews R. The cultural erosion of Indigenous people in health care. CMAJ 2017;189:E78–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].McDermott BM, Cobham VE. A stepped-care model of post-disaster child and adolescent mental health service provision. Eur J Psychotraumatol 2014;5:24294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Mental Health Commission of Canada. Newfoundland and Labrador Stepped Care 2.0 e-mental health demonstration project. Ottawa: Health Canada, 2019. [Google Scholar]
- [53].Murray CB, Groenewald CB, de la Vega R, Palermo TM. Long-term impact of adolescent chronic pain on young adult educational, vocational, and social outcomes. PAIN 2020;161:439–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Noblit GW, Hare RD. Meta-ethnography: Synthesizing qualitative studies. London: Sage, 1988. [Google Scholar]
- [55].Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: a critical review of the literature. J Dev Behav Pediatr 2000;21:58–69. [DOI] [PubMed] [Google Scholar]
- [56].Palermo TM. Pain prevention and management must begin in childhood: the key role of psychological interventions. PAIN 2020;161(suppl 1):S114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Peng P, Stinson JN, Choiniere M, Dion D, Intrater H, LeFort S, Lynch M, Ong M, Rashiq S, Tkachuk G, Veillette Y; STOPPAIN Investigators Group. Dedicated multidisciplinary pain management centres for children in Canada: the current status. Can J Anaesth 2007;54:985–91. [DOI] [PubMed] [Google Scholar]
- [58].Puntillo F, Giglio M, Brienza N, Viswanath O, Urits I, Kaye AD, Pergolizzi J, Paladini A, Varrassi G. Impact of COVID-19 pandemic on chronic pain management: looking for the best way to deliver care. Best Pract Res Clin Anaesthesiol 2020;34:529–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Racine N, Cooke JE, Eirich R, Korczak DJ, McArthur B, Madigan S. Child and adolescent mental illness during COVID-19: a rapid review. Psychiatry Res 2020;292:113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Richardson PA, Harrison LE, Heathcote LC, Rush G, Shear D, Lalloo C, Hood K, Wicksell RK, Stinson J, Simons LE. mHealth for pediatric chronic pain: state of the art and future directions. Expert Rev Neurother 2020;20:1177–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Roberts JP, Fisher TR, Trowbridge MJ, Bent C. A design thinking framework for healthcare management and innovation. Healthc (Amst) 2016;4:11–4. [DOI] [PubMed] [Google Scholar]
- [62].Schults J, Cooke M, Richards J, Theodoros J, Andresen E, Paterson R, Alcock M. mHealth applications for children and young people with persistent pain: a scoping review. Clin Nurs Res 2019;28:779–94. [DOI] [PubMed] [Google Scholar]
- [63].Schünemann HJ, Moja L. Reviews: rapid! Rapid! Rapid! … and systematic. Syst Rev 2015;4:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Shanthanna H, Strand NH, Provenzano DA, Lobo CA, Eldabe S, Bhatia A, Wegener J, Curtis K, Cohen SP, Narouze S. Caring for patients with pain during the COVID‐19 pandemic: consensus recommendations from an international expert panel. Anaesthesia 2020;75:935–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Shaw J, Jamieson T, Agarwal P, Griffin B, Wong I, Bhatia RS. Virtual care policy recommendations for patient-centred primary care: findings of a consensus policy dialogue using a nominal group technique. J Telemed Telecare 2018;24:608–15. [DOI] [PubMed] [Google Scholar]
- [66].Smith K, Iversen C, Kossowsky J, O'Dell S, Gambhir R, Coakley R. Apple apps for the management of pediatric pain and pain-related stress. Clin Pract Pediatr Psychol 2015;3:93–107. [Google Scholar]
- [67].Stamm TA, Andrews MR, Mosor E, Ritschl V, Li LC, Ma JK, Campo-Arias A, Baker S, Burton NW, Eghbali M, Fernandez N, Ferreira RJO, Gäbler G, Makri S, Mintz S, Moe RH, Morasso E, Murphy SL, Ntuli S, Omara M, Simancas-Pallares MA, Horonieff J, Gartlehner G. The methodological quality is insufficient in clinical practice guidelines in the context of COVID-19: systematic review. J Clin Epidemiol 2021;135:125–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Stiles-Shields C, Crowe AN, Driscoll CFB, Ohanian DM, Stern A, Wartman E, Winning AM, Wafford QE, Lattie EG, Holmbeck GN. A systematic review of behavioral intervention technologies for youth with chronic health conditions and physical and intellectual disabilities: implications for adolescents and young adults with spina bifida. J Pediatr Psychol 2019;44:349–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Stinson JN, Huguet A, McGrath P, Rosenbloom B, Soobiah C, White M, Coburn G. A qualitative review of the psychometric properties and feasibility of electronic headache diaries for children and adults: where we are and where we need to go. Pain Res Manag 2013;18:142–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Straus SE, Kastner M, Soobiah C, Antony J, Tricco AC. Introduction: engaging researchers on developing, using, and improving knowledge synthesis methods: a series of articles describing the results of a scoping review on emerging knowledge synthesis methods. J Clin Epidemiol 2016;73:15–8. [DOI] [PubMed] [Google Scholar]
- [71].Tang WX, Zhang LF, Ai YQ, Li ZS. Efficacy of Internet-delivered cognitive-behavioral therapy for the management of chronic pain in children and adolescents: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Tauben DJ, Langford DJ, Sturgeon JA, Rundell SD, Towle C, Bockman C, Nicholas M. Optimizing telehealth pain care after COVID-19. PAIN 2020;161:2437–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Thabrew H, Stasiak K, Hetrick SE, Wong S, Huss JH, Merry SN. E-Health interventions for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst Rev 2018;8:CD012489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Velleman S, Stallard P, Richardson T. A review and meta-analysis of computerized cognitive behaviour therapy for the treatment of pain in children and adolescents: cCBT for pain in children. Child Care Health Development 2010;36:465–72. [DOI] [PubMed] [Google Scholar]
- [75].Virtual Care Task Force. Recommendations for scaling up virtual medical services. Canadian Medical Association; College of Family Physicians of Canada; Royal College of Physicians and Surgeons of Canada, 2020. p. 1–50. Available at: https://www.cma.ca/sites/default/files/pdf/virtual-care/ReportoftheVirtualCareTaskForce.pdf. Accessed August 20, 2020. [Google Scholar]
- [76].Waite-Jones JM, Majeed-Ariss R, Smith J, Stones SR, Van Rooyen V, Swallow V. Young people's, parents', and professionals' views on required components of mobile apps to support self-management of juvenile arthritis: qualitative study. JMIR mHealth uHealth 2018;6:e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Wakefield EO, Popp JM, Dale LP, Santanelli JP, Pantaleao A, Zempsky WT. Perceived racial bias and health-related stigma among youth with sickle cell disease. J Dev Behav Pediatr 2017;38:129–34. [DOI] [PubMed] [Google Scholar]
- [78].Walker LS, Dengler-Crish CM, Rippel S, Bruehl S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. PAIN 2010;150:568–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. PAIN 2012;153:1798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Wensing M, Sales A, Armstrong R, Wilson P. Implementation science in times of Covid-19. Implement Sci 2020;15:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Won AS, Bailey J, Bailenson J, Tataru C, Yoon IA, Golianu B. Immersive virtual reality for pediatric pain. Children (Basel) 2017;4:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].World Wide Web Consortium (W3C). Web content accessibility guidelines (WCAG) 2.0. 2008. Available at: https://www.w3.org/TR/WCAG20/. Accessed April 2, 2021. [Google Scholar]
- [83].Wylie L, McConkey S. Insiders' insight: discrimination against indigenous peoples through the eyes of health care professionals. J Racial Ethn Health Disparities 2019;6:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content associated with this article can be found online at http://links.lww.com/PR9/A108.