Abstract
Introduction and importance
Acute scrotum is considered a urological emergency requiring early intervention depending on the cause. There are multiple causes of acute scrotum with testicular torsion being the most feared as delayed treatment leads to testicular loss. However, differentiating between epididymo-orchitis and torsion can be very difficult.
Case presentation
We present a case of an 18-year old male patient with 2 separate episodes of acute scrotum. He had epididymo-orchitis as the first presentation followed by testicular torsion 5 days later. To our knowledge this is the first case of testicular torsion secondary to epididymo-orchitis.
Clinical discussion
Differentiating between epididymo-orchitis and torsion is challenging but important due to risk of loss of testis with a wrong diagnosis. Once you establish epididymo-orchitis the suspicion for subsequent torsion should be high with close follow up and adequate counselling.
Conclusion
He ultimately had orchiectomy, although a rare presentation, enlarged testis due to epididymo-orchitis can predispose an individual to developing testicular torsion thus adequate counselling on warning signs to patients with epididymo-orchitis is of particular importance so as to intervene early and ultimately save the testis.
Keywords: Acute scrotum, Epididymo-orchitis, Testicular torsion, Testicular infarction
Highlights
-
•
18-year old male presenting with 2 separate episodes of acute scrotum.
-
•
Initially diagnosed to have epididymo-orchitis with confirmation of color doppler ultrasound
-
•
Second acute scrotum 5 days after and diagnosed to have torsion
-
•
Unsalvageable testis due to delay in second presentation
-
•
Epididymo-orchitis as a preceding risk factor to develop torsion
1. Introduction and importance
Acute scrotum is considered a urological emergency requiring prompt surgical or medical intervention depending on the underlying etiology [1]. Causes of acute scrotum include testicular torsion, torsion of appendage, epididymo-orchitis (EO), scrotal trauma, hernia, infected hydroceles and vasculitis such as Henoch-Schönlein purpura [2]. Among the causes of acute scrotum testicular torsion is the one that must be ruled out first, as delay in the treatment leads to irreversible testicular necrosis thus the need for early identification and surgical intervention is important [3]. It is suggested that onset of irreversible ischemia sets in at around 6 h therefore early surgical intervention is of paramount importance [4]. However, it can be extremely difficult to differentiate between causes of acute scrotum on clinical examination alone, especially between testicular torsion and EO, thus the need of a Doppler ultrasound study as a supplement to a scrotal examination when diagnosis of EO is equivocal as toll to rule out torsion [5]. We report a case on 2 separate episodes acute scrotum within a 1-week period of time, to our knowledge this is the first case of EO predisposing to testicular torsion. This paper has been reported in line with the SCARE 2020 criteria [6]. This article has been registered with the Research Registry with identification number research registry 6835 and can be found through the following hyperlink Browse the Registry - Research Registry.
2. Case presentation
An 18-year old male patient with no comorbid, not on medications, no drug allergies, no prior surgical history, no significant family history of disease and does not smoke or drinks alcohol. Presented with a 4-h history of right testicular pain of gradual onset, non-radiating, aggravated on movement, relieved with oral analgesia and associated with right scrotal swelling. He had a history of prior pain on micturition with no urethral discharge, also denied any chills, fever, nausea, trauma or similar past pain attacks. Had a history of unprotected multiple sexual contacts in the last 3 months otherwise his medical and surgical history are unremarkable.
On examination he was alert, oriented and afebrile with stable vitals. His scrotal examination revealed an obvious right scrotal swelling with normal overlying skin. The right epididymis and testicle were enlarged, tender, not high riding testis, with a positive Prehn's test and intact cremasteric reflex. The left testis had normal findings and the rest of the systemic examination was essentially normal.
The initial workup of the patient revealed a leukocytosis with predominance neutrophilia, raised inflammatory marker and mid-stream urinalysis showed 2+ leucocytes and pus cells 5–10/HPF. Emergency Doppler ultrasound of the scrotum performed and interpreted by a senior radiologist showed an enlarged right testis and epididymis accompanied with fluid collection around epididymis which was suggestive of EO with normal Doppler flow, however high vascularity and hyperemia (inferno sign) increased the sensitivity of ultrasound to diagnose EO around 91%, still 9% showed normal flow [7] (Fig. 1).
Fig. 1.
Doppler ultrasound of scrotum. A – Enlarged right testes with normal doppler flow. B – Enlarged right epididymis. C – Fluid collection around epididymis suggestive of inflammatory in origin. D – Left testes with normal doppler flow.
In view of the EO, the patient was reviewed by a senior urologist and admitted for intravenous (IV) cefepime 1 g 12 hourly, pain management of IV paracetamol 1 g 8 hourly with oral ibuprofen 400 mg 8 hourly, scrotal support and observation. During his admission, pain was well controlled throughout his stay, no spikes in fever and vitals were stable. On day of discharge, 3 days later, he had no complaints and on examination scrotal swelling had subsided significantly with a non-tender right testis. He was discharged on oral antibiotic (cefixime 200 mg 12 hourly) with analgesia (oral paracetamol 1 g 8hourly and oral ibuprofen 400 mg 8 hourly) and counselled on warning signs.
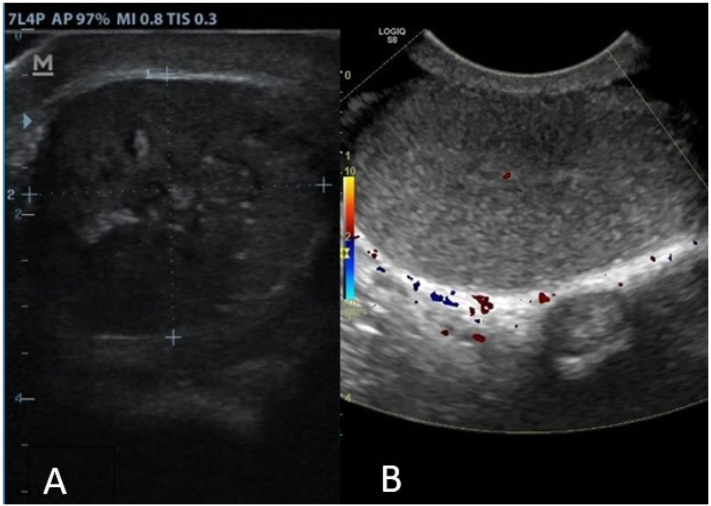
Patient came for follow up and seen by the urologist 3 days later complaining of severe right testicular pain for more than 48 h which he had developed after discharge at home however he did not seek medical attention as he attributed it to the ongoing infection. On examination, he was alert, in pain, afebrile with stable vitals and scrotal examination revealed right scrotal swelling with normal overlying scrotal skin. Right testicle was enlarged, tender, high riding testis, in a transverse lie, and absent cremasteric reflex. Doppler scrotal ultrasound carried out by the same radiologist revealed an enlarged right testicle with areas of diffuse low echotexture and no Doppler tracing of testicular artery suggestive of right testicular infarction secondary to torsion. Left testicle appeared with normal size and echotexture with normal color Doppler flow (Fig. 2).
Fig. 2.
A – Right testes with diffuse low echotexture and no vascularity on color doppler suggestive of testicular infarction. B – Compared to same testes from previous scan.
Patient was booked for emergency scrotal exploration performed by the senior urologist and intra-operative findings of spermatic cord twisted 360o around its axis and a gangrenous right testis (Fig. 3). Thus, right orchidectomy and left orchidopexy was performed and post operatively patient put on antibiotic (IV cefepime 1 g 12 hourly), pain management (IV paracetamol 1 g 8 hourly and intramuscular pethidine 100 mg as per need basis) and counselled on preventive measures and warning signs on living with one testicle explained. Patient on discharge understood the need for emergent surgical intervention however was still feeling sad with regards to a lost testis. On follow up at outpatient clinic he was progressing well with minimal tenderness and a clean surgical scar and was coming to terms with losing one testis with his last follow up at 6 months post-operative.
Fig. 3.
Intra-operative gangrenous right testicle with spermatic cord twisted 360o.
3. Discussion
Acute scrotum is responsible for around 1% of all visits to the emergency department with most common causes being EO, testicular torsion and torsion of testicular appendices [8]. Testicular torsion more often presents in the post pubescent period from 12 to 18 where as EO is the most common cause of acute scrotum in adults [9,10]. Classically a high riding testis with absent cremasteric reflex, negative Prehn's sign and associated nausea or vomiting is suggestive of testicular torsion [11]. However, it has been seen that symptoms and signs of testicular torsion and EO overlap [10]. As with our case the patient during the first presentation was consistent with EO and later presented with the above features after developing testicular torsion at home.
Since clinical presentation of testicular torsion and EO tend to mimic one another reaching a diagnosis on clinical examination alone becomes difficult. Hence Color Doppler ultrasound is now the imaging modality of choice particularly to rule out a testicular torsion and to evaluate scrotal contents for features of inflammation [12]. Findings of Color Doppler sonography when compared to surgical exploration findings revealed the sensitivity, specificity, positive and negative predictive values of Color Doppler sonography for detecting testicular torsion were 100%, 75.2%, 80.4% and 100%, respectively [13]. Our case is a reflection of the above findings with our ultrasound findings having the ability to suggest EO during the first presentation and to identify testicular torsion at the second presentation.
Causes of EO are most commonly of infectious origin while non-infectious causes include trauma, autoimmune and vasculitis [14]. Infectious causes below the age of 35 are N. gonorrhoeae and C. trachomatis and E. coli in the older age group specifically in those with obstructive uropathies [15,16]. On the other hand, the exact cause of torsion is unknown however predisposing factors include bell clapper deformity, increase in testicular volume, testicular tumor, horizontal lie testicle, trauma, long spermatic cords [17]. Therefore, increase in testicular volume in EO as seen in our case due to inflammatory reactions can predispose an individual to develop testicular torsion. According to Campbell-Walsh-Wein Urology textbook, the exact provoking cause of torsion is still unknown however activating the cremasteric reflex, which is exaggerated in an inflammatory setting, as well as rapid testicular growth are factors that may lead to torsion [18].
There are few case reports on testicular infarction following an event of EO. Previous case reports stating abscess formation, compression of testicular vasculature due to swelling, bacterial toxins causing thrombus formations as possible causes of infarction following an episode of EO [[19], [20], [21]]. However, no case report on testicular infarction due to the development of a testicular torsion following EO has been previously reported on, which was the underlying cause of infarction in our case.
4. Conclusion
Acute scrotum is a surgical emergency with a high suspicion for testicular torsion until ruled out otherwise. This is because early identification and intervention is paramount towards salvage of the testicle. As seen in our case an enlarged testis due to EO can predispose an individual to developing testicular torsion thus a patient with EO requires adequate counselling on warning signs with post discharge observation and follow up as it may lead to torsion of which early diagnosis is of paramount importance.
Abbreviations
Patient perspectives
I thought I was on the road to recovery and then developed an intense pain which I attributed to the same infection. However, I lost a testicle in the process hence am now very vigilant and aware of what to look out for.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
A.I: study conception, production of initial manuscript, collection of data.
A.Z: Study conception, revision of the manuscript, proofreading.
P. A: Reviewed the manuscript.
A.A: Reviewed the manuscript.
Declaration of competing interest
None.
Contributor Information
Ali Akbar Zehri, Email: draazehri@gmail.com, aliakbar.zehri@akhst.org.
Allyzain Ismail, Email: allyzain.ismail@akhst.org.
Athar Ali, Email: athar.ali@akhst.org.
Refrences
- 1.Liguori G., Bucci S., Zordani A., Benvenuto S., Ollandini G., Mazzon G. Role of US in acute scrotal pain. World J. Urol. 2011;29(5):639–643. doi: 10.1007/s00345-011-0698-8. [DOI] [PubMed] [Google Scholar]
- 2.Kass E.J., Lundak B. The acute scrotum. Pediatr. Clin. N. Am. 1997;44(5):1251–1266. doi: 10.1016/s0031-3955(05)70556-3. [DOI] [PubMed] [Google Scholar]
- 3.Bertolotto M., Campo I., Derchi L.E. Springer; Pain Imaging: 2019. Imaging of Acute Scrotum; pp. 487–498. [Google Scholar]
- 4.Kapoor S. Testicular torsion: a race against time. Int. J. Clin. Pract. 2008;62(5):821–827. doi: 10.1111/j.1742-1241.2008.01727.x. [DOI] [PubMed] [Google Scholar]
- 5.Beni-Israel T., Goldman M., Chaim S.B., Kozer E. Clinical predictors for testicular torsion as seen in the pediatric ED. Am. J. Emerg. Med. 2010;28(7):786–789. doi: 10.1016/j.ajem.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Ralls P.W., Jensen M.C., Lee K.P., Mayekawa D.S., Johnson M.B., Halls J.M. Color Doppler sonography in acute epididymitis and orchitis. J. Clin. Ultrasound. 1990;18(5):383–386. doi: 10.1002/jcu.1870180503. [DOI] [PubMed] [Google Scholar]
- 8.Davis J.E., Silverman M. Scrotal emergencies. Emerg. Med. Clin. 2011;29(3):469–484. doi: 10.1016/j.emc.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Sathler E.S., Viera R. Atypical case report of testicular torsion intravaginal in preschool. Braz. J. Surg. Clin. Res. 2017;18:49–51. [Google Scholar]
- 10.Boniface M., Mohseni M. StatPearls Publishing LLC; Treasure Island, FL: 2019. Acute scrotum pain. [PubMed] [Google Scholar]
- 11.Ringdahl E.N., torsion Teague L. Testicular. American family physician. 2006;74(10):1739–1743. [PubMed] [Google Scholar]
- 12.Herbener T.E. Ultrasound in the assessment of the acute scrotum. J. Clin. Ultrasound. 1996;24(8):405–421. doi: 10.1002/(SICI)1097-0096(199610)24:8<405::AID-JCU2>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 13.Altinkilic B., Pilatz A., Weidner W. Detection of normal intratesticular perfusion using color coded duplex sonography obviates need for scrotal exploration in patients with suspected testicular torsion. J. Urol. 2013;189(5):1853–1858. doi: 10.1016/j.juro.2012.11.166. [DOI] [PubMed] [Google Scholar]
- 14.Tracy C.R., Steers W.D., Costabile R. vol. 35(1) Urologic Clinics of North America; 2008. Diagnosis and Management of Epididymitis; pp. 101–108. [DOI] [PubMed] [Google Scholar]
- 15.Doble A., Taylor-Robinson D., Thomas B., Jalil N., Harris J., Witherow R.O.N. Acute epididymitis: a microbiological and ultrasonographic study. Br. J. Urol. 1989;63(1):90–94. doi: 10.1111/j.1464-410x.1989.tb05132.x. [DOI] [PubMed] [Google Scholar]
- 16.Hawkins D., Taylor-Robinson D., Thomas B., Harris J. Microbiological survey of acute epididymitis. Sex. Transm. Infect. 1986;62(5):342–344. doi: 10.1136/sti.62.5.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wampler S.M., Llanes M. Common scrotal and testicular problems. Prim. Care. 2010;37(3):613–626. doi: 10.1016/j.pop.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Partin A.W., Wein A.J., Kavoussi L.R., Peters C.A., Dmochowski R.R. Elsevier Health Sciences; E-Book: 2020. Campbell Walsh Wein Urology. [Google Scholar]
- 19.Chia D, Penkoff P, Stanowski M, Beattie K, Wang AC. Testicular infarction and rupture: an uncommon complication of epididymo-orchitis. J. Surg. Case Rep. 2016;2016(5). [DOI] [PMC free article] [PubMed]
- 20.Rhudd A, Moghul M, Reid G. Epididymo-orchitis causing testicular infarction: a serious complication of a common disorder. J. Surg. case Rep. 2017;2017(10). [DOI] [PMC free article] [PubMed]
- 21.Alharbi B., Rajih E., Adeoye A., Allatiefe B.A., Abdullah M.H. Testicular ischemia secondary to epididymo-orchitis: a case report. Urol. Case Rep. 2019;27:100893. doi: 10.1016/j.eucr.2019.100893. [DOI] [PMC free article] [PubMed] [Google Scholar]