Abstract
We report a 31 year old female with urologic history significant for right ureteropelvic junction obstruction managed with open right pyeloplasty in 1996 with recurrent stricture managed with right ureterocalycostomy in 1997 along with right distal ureteroneocystostomy for iatrogenic distal ureteral stricture. She developed symptomatic stone episodes and recurrent urinary tract infections and elected to proceed with shockwave lithotripsy. Postoperatively she developed a large liver hemorrhage requiring supportive care and endovascular embolization.
Keywords: Shockwave lithotripsy, Hematoma, Angioembolization
Introduction
Shockwave lithotripsy (SWL) was first used in humans in 1980 and approved by the US Food and Drug Administration in 1984 for commercial use.1 Shock wave lithotripsy has the lowest complication rate compared to other stone surgeries, and a majority of the complications are mild. Severe and life-threatening complications are rare. Historically, perinephric hematomas were reported as a rare complication occurring in 0.2–1.5% of cases. However, routine imaging with computerized tomography or magnetic resonance imaging has demonstrated hematoma rate to be as high as 20–25%.2 Hepatic hematomas are an extremely rare but potentially catastrophic complication following SWL. We report a patient with a complex urologic history who developed a large hepatic hematoma requiring endovascular embolization.
Case report
The patient is a 31 year old female with urologic history significant for right ureteropelvic junction obstruction managed with open right pyeloplasty in 1996. She developed recurrent obstruction and underwent a right ureterocalycostomy in 1997 along with right distal ureteroneocystostomy for iatrogenic distal ureteral stricture. She was initially followed with annual renal ultrasounds which revealed stable caliectasis and normal renal function. She was also evaluated by multiple urologists secondary to family relocation for recurrent urinary tract infections. Her first acute stone episode occurred in 2014 during pregnancy and she spontaneously passed a total of three kidney stones. After establishing care she had four documented symptomatic urinary tract infections with four cultures growing E. Coli and one culture growing Enterococcus Faecalis in a 10 month period. She complained of intermittent right sided flank pain that worsened with dehydration. A non-contrast CT scan was performed showing multiple right sided non-obstructing renal stones with the largest stone measuring approximately 6 mm in the upper pole (Fig. 1). She elected to proceed with shockwave lithotripsy. A total of 1250 shocks were delivered to the upper pole and 750 shocks delivered to the lower pole with power settings at 20 kV for the first 400 shocks but decreased to 17 kV for the remaining shocks. The stones appeared well fragmented at conclusion of the procedure and she was discharged home from recovery unit.
Fig. 1.
Axial and coronal views of non-contrast CT scan showing multiple calculi within each calyx.
She returned to the Emergency Department a few hours later with severe right sided abdominal pain and right shoulder pain. Post operative hemoglobin down-trended from 15.0 g/dL to 10.6 g/dL A contrast enhanced CT scan demonstrated a 12.7 × 9.8 × 16.1 cm right hepatic sub-capsular hematoma with compression of the liver and extension of hemorrhage along the right paracolic gutter without any contrast extravasation (Fig. 2). She was admitted to the intensive care unit and initially transfused 2 units of packed red blood cells with post transfusion hemoglobin having down-trended to 9.5 g/dL. Her hemoglobin continued to down-trend over the next three days and she required a total of 7 units of packed red blood cells, 1 unit of fresh frozen plasma, and 1 unit of platelets. Given the continuous down-trend in hemoglobin despite no contrast extravasation on CT scan, she was taken for a visceral arteriogram by interventional radiology on post operative day 4. There was no obvious active contrast extravasation from the hepatic branches. However based on the expertise and discretion of the interventional radiologist, selective gel foam embolization of right hepatic artery branches was performed (Fig. 3). After embolization her hemoglobin remained stable and she did not require anymore blood transfusions. She was ultimately discharged home on post operative day 9. She did well after discharge and follow up imaging 1 month later demonstrated interval decrease in the size of the hematoma which measured 10.9 × 9.7 × 13.1 cm. A CT scan performed approximately 8 months after discharge demonstrated near resolution of the hematoma which then measured 4.2 × 4.5 cm.
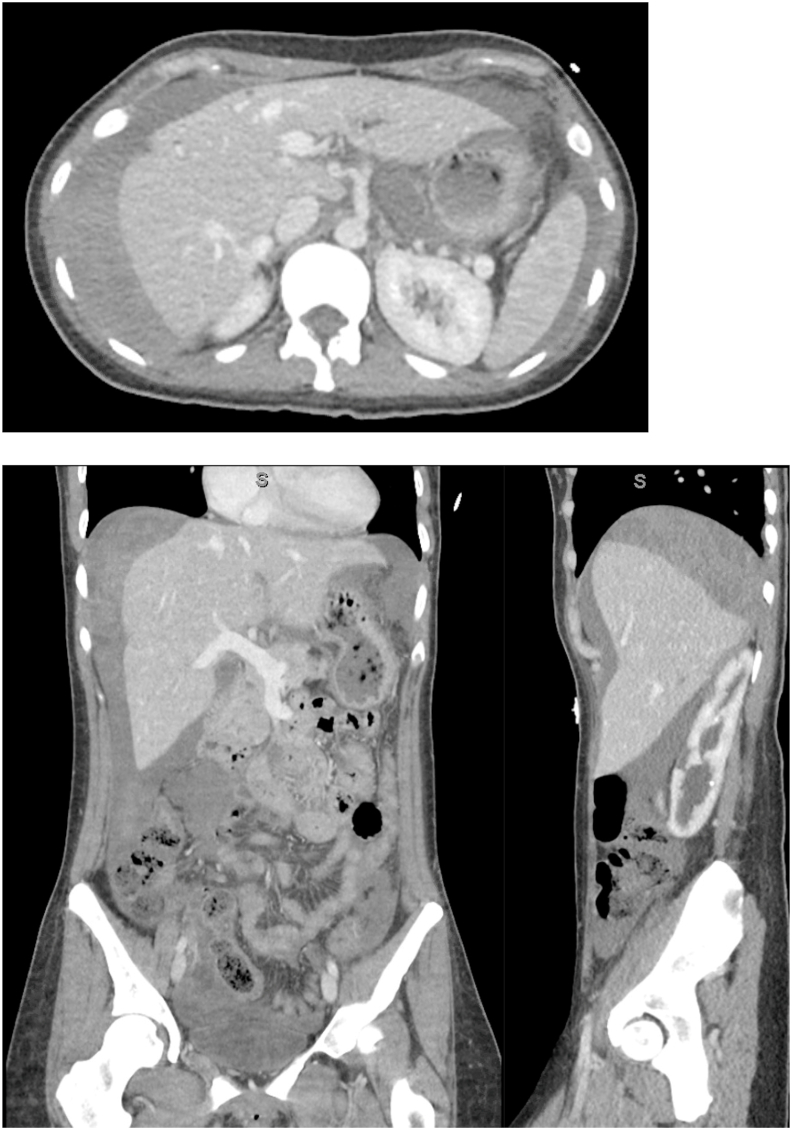
Fig. 2.
Contrast enhanced CT scan with transverse, coronal, and sagittal images demonstrating large hepatic hematoma extending into right paracolic gutter.
Fig. 3.
Visceral arteriogram of right hepatic artery with selective gel foam embolization of branches.
Discussion
The prevalence of nephrolithiasis is estimated to be around 9% of the United States population. Compared to other surgical treatment options for kidney stones, shockwave lithotripsy has the least morbidity and lowest complication rates which have been estimated to be <6%.3,4 The most common complications include transient gross hematuria, flank pain, urinary tract infection, and accumulation of obstructing stone fragments within the ureter (Steinstrasse). Symptomatic subcapsular renal hematomas have been estimated to occur in 1.5% patients post SWL.2 There are multiple risk factors associated with renal subcapsular hematoma formation with uncontrolled hypertension having the strongest association. Other risk factors include diabetes mellitus, coronary artery disease, and obesity all of which have underlying vascular pathology possibly increasing the bleeding risk. Hepatic hematoma is an even rarer complication with limited reported cases in the literature.5
This patient developed severe abdominal pain along with signs of hemorrhagic shock within hours after conclusion of the procedure. Solid organ injury and internal hemorrhage should be considered in these situations, with particular evaluation for renal, splenic, and liver injuries. There should be a low threshold in obtaining abdominal imaging to diagnose and guide management. Hepatic subcapsular hematomas, like renal subcapsular hematomas, can generally be managed with supportive care including serial hemoglobin monitoring, blood transfusions, and analgesics. However, angioembolization should be considered in the setting of a persistently down-trending hemoglobin despite blood transfusions especially if contrast extravasation is seen on imaging. Our patient did not have extravasation of contrast on CT scan or visceral arteriogram but gel foam embolization was selectively performed due to failure of conservative management. Her hemoglobin stabilized after embolization and she was discharged home shortly after this procedure. At one year follow up she has not experienced recurrent urinary tract infection or acute stone episode. This case report demonstrates a patient with a complex urologic surgical history who developed a rare but potentially fatal complication following SWL requiring supportive care and angioembolization.
References
- 1.Chaussy C., Schmiedt E., Schuller J. Extracorporeal shock-wave lithotripsy (ESWL) for treatment of urolithiasis. Urology. 1984;23(5):59–66. doi: 10.1016/0090-4295(84)90243-7. [DOI] [PubMed] [Google Scholar]
- 2.Dhar N.B., Thornton J., Karafa M.T., Streem S.B. A multivariate analysis of risk factors associated with subcapsular hematoma formation following electromagnetic shock wave lithotripsy. J Urol. 2004;172(6 Pt 1):2271–2274. doi: 10.1097/01.ju.0000143459.03836.2d. [DOI] [PubMed] [Google Scholar]
- 3.Tiselius H.G., Chaussy C.G. Arguments for choosing extracorporeal shockwave lithotripsy for removal of urinary tract stones. Urolithiasis. 2015;43:387–396. doi: 10.1007/s00240-015-0818-9. [DOI] [PubMed] [Google Scholar]
- 4.Assimos D., Krambeck A., Miller N.L. Surgical management of stones: American urological association/endourological society guideline, PART I. J Urol. 2016;196(4):1153–1160. doi: 10.1016/j.juro.2016.05.090. [DOI] [PubMed] [Google Scholar]
- 5.Beatrice J., Strebel R.T., Pfammatter T., Röhweder J.H., Sulser T. Life-threatening complication after right renal extracorporeal shock wave lithotripsy: large hepatic haematoma requiring embolisation of the right hepatic artery. Eur Urol. 2007;52(3):909–911. doi: 10.1016/j.eururo.2007.02.011. [DOI] [PubMed] [Google Scholar]