ABSTRACT
Responsive feeding (RF) involves reciprocal nurturing feeding practices between the caregiver and the child that encourage the child to develop preferences for healthy foods and beverages and to eat autonomously. In this commentary, we summarize RF-related findings from a recent US National Academies of Sciences, Engineering, and Medicine (National Academies) consensus study report examining consistency in infant and young child feeding (IYCF) recommendations in guidelines from high-income countries, and we discuss implications for future IYCF guidelines. Although existing guidelines included generally consistent messages about several RF behaviors, such as the importance of encouraging self-feeding and self-regulation in infants and toddlers, they generally did not present the recommendations as part of a cohesive RF interdisciplinary framework. Moving forward, evidence-based RF recommendations should be routinely incorporated and identified in dietary guidance for IYCF based on a consensus definition of RF grounded in sound responsive parenting and feeding frameworks. We recommend replicating the National Academies’ scoping review in low- and middle- income countries and mixed-methods implementation science research to improve our understanding of how best to disseminate and implement RF-related recommendations across settings (e.g., home and early care and education centers), taking the social determinants of health into account.
Keywords: responsive feeding, complementary feeding, dietary guidelines, feeding recommendations, infants and young children, parent-child relationship
Background
Responsive feeding (RF) has been previously defined in different but overlapping ways. RF definitions reflect researcher disciplines (e.g., child development, child nutrition, interdisciplinary teams that include both) and settings with different poverty and food-security contexts (e.g., higher- vs. lower-income countries). In this commentary we define RF from an interdisciplinary perspective as “feeding practices that encourage the child to eat autonomously and in response to physiological and developmental needs, which may encourage self‐regulation in eating and support cognitive, emotional and social development” (1–4). This definition is consistent with the RF conceptual frameworks that guided the recent development of RF scales in Cambodia (5) and Sri Lanka (6) by 2 independent research groups.
At the core of RF is the concept of active feeding (5). Based on RF descriptions by Bentley et al. (7) and Black and Aboud (8), active feeding involves reciprocal nurturing feeding practices between the caregiver and the child that encourage the child to develop preferences for healthy foods and beverages and to eat autonomously. By contrast, non-RF is characterized by a lack of active feeding or reciprocity between the caregiver and child and can include the following caregiver behaviors: 1) dominating the feeding situation through controlling and pressuring behaviors (e.g., forcing a child to finish all of the food on his or her plate before leaving the table), 2) failing to redirect child behaviors that interfere with the establishment of healthy food preferences and eating routines (e.g., allowing a child to carry around a bottle of milk and drink from it all day long), or 3) being uninvolved and ignoring the child (e.g., being preoccupied with a television or smartphone during meal times) (1, 2). When caregivers over-control the feeding, not only do they potentially override the child's internal hunger and satiety regulatory cues they may also interfere with the child's emerging autonomy and striving for competence (8). At the same time, an under- or uninvolved caregiver does not provide the child with the scaffolding and structure he or she needs to develop healthy habits and routines as part of his or her emerging autonomy.
Ultimately, RF can contribute to optimal growth and psycho-emotional, social, and cognitive development as one of the key components of nurturing care (1–4, 9–11).
RF has been recognized as a necessary component of strategies to prevent all forms of malnutrition, including stunting and childhood obesity, because it encourages self‐regulation of children's intake of healthy foods and beverages in response to hunger and satiety (1–3, 5). Hence, it has recently been argued that robust, evidence-based RF recommendations should routinely be included as part of dietary guidelines for infant and young children (3). An important first step towards this goal is to understand whether and how RF recommendations are currently being included in existing dietary guidelines for infants and young children.
In this commentary, we summarize the RF-related findings from a recent US National Academies of Sciences, Engineering, and Medicine (National Academies) consensus study report examining consistency in infant and young child feeding (IYCF) recommendations in guidelines from high-income countries (12) and discuss implications for future IYCF guidelines. This commentary complements 2 previous ones detailing the implications of the consensus study to registered dietitian nutritionists (13) and researchers (14).
Synthesis of RF-Related Recommendations from Guidelines Included in the National Academies Report
Table 1 summarizes the consistency in recommendations related to “how to feed” infants and young children across IYCF guidelines. Guidelines that explicitly included RF recommendations were generally consistent in recommending that the feeding environment be pleasant and that caregivers demonstrate nurturing behaviors, such as verbalizing, making eye contact, and not pressuring the child to eat. They were consistent in recommending repeated exposure to new foods to facilitate acceptance by the infant or young child. Furthermore, they were generally consistent in recommending that self-feeding and self-regulation be encouraged in infants and toddlers. Interestingly, although guidelines were generally consistent in emphasizing the importance of using hunger and satiety cues to guide infant and child feeding, they did not always label these recommendations as RF. Guidelines were generally consistent with regard to recommending that food consistency and texture be adapted to the developmental stage of the child, and that feeding routines should be established, although we note that these practices were also not always specifically identified as being part of RF.
TABLE 1.
Summary of the consistency of recommendations on how to feed infants and young children, by topic area1
| Topic area | Summary of consistency across recommendations |
|---|---|
| Safety of foods and feeding practices | • Consistent in recommending that milk, milk products, and juice given to children should be pasteurized |
| • Consistent in recommending against giving honey to children under 1 y of age due to risk of botulism | |
| • Generally consistent in recommending against consumption of raw or undercooked eggs | |
| • Consistent in advising about choking hazards, although examples provided varied across guideline documents | |
| • Consistent in recommending that infants and young children be supervised while eating | |
| Introduction of complementary foods | • Generally consistent in recommending that complementary foods not be introduced before 4 mo of age or delayed to after 6 mo of age |
| • Not consistent in whether the recommended age of introduction is an age range (4–6 mo) or is focused on introduction at ∼6 mo | |
| • Consistent in recommending that the first foods offered to infants be iron rich or iron fortified | |
| • Consistent in recommending gradual introduction of new foods | |
| Food consistency and texture | • Consistent in recommending that food consistency and texture be tailored to the developmental needs of the child |
| • Consistent in recommending that consistencies and textures of foods offered should change as the child gets older | |
| Meal frequency | • Generally consistent in recommending that a consistent meal schedule be established |
| • Generally consistent in recommending that young children need several eating occasions, both meals and snacks, over the course of the day | |
| Hunger and satiety cues | • Generally consistent in emphasizing the importance of using hunger and satiety cues to guide infant and child feeding |
| Responsive feeding | • Generally consistent in recommending that the feeding environment be pleasant and include nurturing behaviors (e.g., verbalization, eye-to-eye contact, not forcing the child to eat) |
| • Consistent in recommending that repeated exposure is needed for children to accept new foods | |
| • Generally consistent in recommending that self-feeding and self-regulation be encouraged in infants and toddlers |
Adapted with permission from the National Academies of Sciences, Engineering, and Medicine (12). Note: The committee used the following phrases to describe consistency of recommendations: Consistent indicates alignment across the recommendations; Generally consistent indicates that the recommendations tended to provide similar guidance, although there were some differences in details or wording; indicates mixed recommendations, some of which align; Not consistent indicates recommendations provided different guidance on a topic. Food safety recommendations are not discussed in this commentary.
Overall, many guidelines addressed at least some aspects of RF. However, it is our observation that they generally did not group all of the aspects of RF together in 1 section of the guideline or present the recommendations as part of a cohesive RF framework. Only 1 guideline reviewed in the National Academies report used a comprehensive RF framework, using the context of responsive parenting (RP) to guide RF recommendations (1, 2).
To improve the incorporation and presentation of RF recommendations in future guidelines, a consensus framework for RF is necessary. Some RP and RF frameworks that have been used in the development of IYCF RF recommendations are presented in the following section.
Conceptual Framework
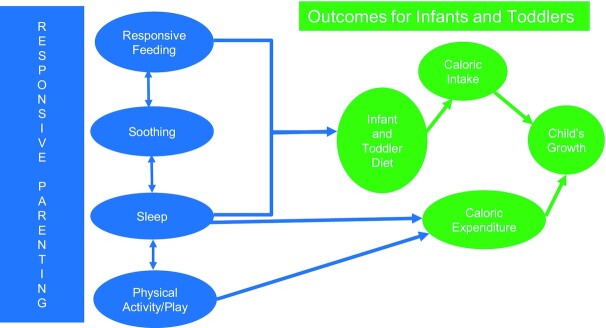
RF falls under the umbrella of the RP framework, which acknowledges that soothing, sleep, and play routines are intimately intertwined with feeding routines (1, 2, 8) (Figure 1).
FIGURE 1.
Responsive parenting framework guiding the development of the Robert Wood Johnson Foundation Healthy Eating Research infant and toddler feeding guidelines (2). Adapted with permission from reference 2.
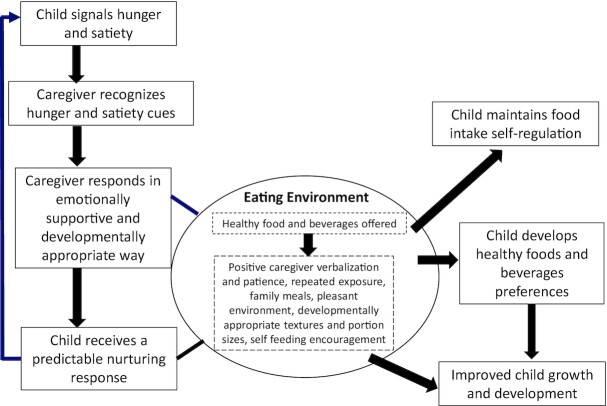
The central active feeding component of the RF framework is grounded in the following steps (Figure 2): 1) the child signals hunger and satiety through motor actions, facial expressions, or vocalizations; 2) the caregiver recognizes the cues and responds promptly in a manner that is emotionally supportive, contingent on the signal, and developmentally appropriate; and 3) the child exhibits a predictable response to these signals (7, 8).
FIGURE 2.
Responsive feeding framework. Original framework supported with evidence from Bentley et al. (7); Black and Aboud (8); National Academies of Sciences, Engineering, and Medicine (15); Pérez-Escamilla et al. (2); Redsell et al. (16); and Pérez-Escamilla et al.(1, 2)
The RP and RF frameworks are strongly supported by empirical research, including randomized controlled trials (1, 2, 9) that included interventions to promote a number of RP/RF-consistent behaviors (Text Box 1).
Text Box 1: Components of effective responsive parenting/responsive feeding interventions (1, 2, 9, 15, 16)
Hunger and satiety cues: Caregiver identifies and responds in an emotionally supportive and predictable way to hunger and satiety cues, recognizing changing cues as the child develops, and differentiating hunger from other issues that may cause an infant or young child to fuss or cry
Soothing: Caregiver does not use food to calm child when s/he is not hungry
Introduction of complementary foods: Caregiver introduces complementary foods in a timely way, taking into account child developmental readiness
Flavor preferences: Caregiver offers a diverse diet with repeated exposures to healthy foods/beverages, and avoids offering ultra-processed foods and sugar-sweetened beverages
Food consistency: Caregiver offers foods with appropriately evolving consistency as the child develops
Portion sizes: Caregiver offers foods and beverages in the child's own plate or bowl and with other eating utensils (e.g., spoon) appropriate for the developmental stage and nutritional needs of child
Caregiver feeding styles: Caregiver is patient and does not pressure the child to eat or finish food or limit food intake (e.g., to prevent weight gain in child)
Nurturing feeding environment: Caregiver provides loving and stimulating verbalizations to the child
Eat as a family: Infant or child can actively observe caregivers and other family members preparing and consuming healthy foods/beverages in a clean and pleasant nurturing environment
Avoid distractions during feeding: Caregiver does not use screens or cell phones (e.g., texting) during feeding
Daily routines/structure: Caregiver establishes well-structured daily routines for eating, sleeping, playing, and bathing
Randomized controlled trials have demonstrated that intervention packages based on comprehensive RF recommendations delivered to caregivers at clinics and/or at home by doctors or home visiting nurses can improve RF behaviors and lead children to develop healthier food preferences, to increase their intake of healthier foods, to reduce their intake of ultra-processed foods and sugar-sweetened beverages, and to have improved weight outcomes. A limitation of this body of evidence is that the randomized controlled trials that have used a comprehensive RP/RF “bundle” or “package” approach to deliver RP/RF interventions have all been conducted among well-to-do families in high-income countries (1, 2).
Next Steps and Research Recommendations
Moving forward, evidence-based RF recommendations should be routinely incorporated and clearly identified in dietary guidance for infants and young children based on a consensus framework for RF (3). The best RF framework to use to develop practical and effective recommendations should be identified through an evidence-based interdisciplinary consensus process (13). Because feeding cues and RF approaches evolve as the child develops, RF recommendations should ideally be broken down in guideline documents by age groups (e.g., 0 to <6, 6 to <12, 12–24 mo). In addition, dissemination documents for IYCF guidelines should consider providing specific guidance on how to implement RF recommendations in settings outside the home, such as early care and education centers. For dissemination documents to be effective, they will need to be written by interdisciplinary teams with strong expertise in implementation and dissemination science.
Because implementing RF recommendations requires family stability and continuous access to healthy foods, equity should be considered when translating RF recommendations into policy and practice (17). It is important to address how social-protection policies can help low-income families implement RF recommendations under conditions of poverty and food, housing, and health insecurity in the complex context of nurturing care (3, 17).
We identified 3 research priorities in the area of RF and feeding recommendations for infants and young children. First, it would be useful to replicate the scoping review conducted by the National Academies (12) in low- and middle-income countries. Several countries have now developed feeding guidelines for children under 2 y (18, 19) and there is global interest in RF (11). Second, we recommend conducting mixed-methods implementation science research to improve our understanding of how best to disseminate and implement RF-related recommendations across settings (e.g., home and early care and education centers), countries, and households with different income levels (13). Third, to estimate the impact of RF recommendations on feeding behaviors, it is key to develop pragmatic RF measurement scales that can be applied at the population level and are valid and reliable across countries (1, 2). The RF measurement scale studies conducted by Sall et al. (5) in Cambodia and Pallewaththa et al. (6) in Sri Lanka are an important step, but there is a need to examine performance across additional low-, middle-, and high-income countries.
Given the globalized unhealthy first-food systems (i.e., food systems surrounding pregnant and lactating women, infants, and young children) (20) and the resources required to develop evidence-based guidelines (11, 13, 21), it is prudent to encourage across-borders collaborations to harmonize RF aspects of dietary guidelines for infants and young children. For example, there have been attempts to develop trilateral partnerships between Canada, the United States, and Mexico (22). There is also a current across-borders childhood obesity initiative led by the NIH's Fogarty Center to share learning and establish collaborations between Latin American countries and the United States, as well as among Latin American countries (23). Moving forward, it will be important to fully embrace the development of a comprehensive interdisciplinary RF framework and IYCF recommendations. Such a framework should go beyond food recommendations, and also include other domains strongly linked to the feeding process, such as infant sleep routines. It is encouraging to see that the 2020–2025 Dietary Guidelines for Americans have begun to address RF as part of the IYCF recommendations (19).
ACKNOWLEDGEMENTS
The authors thank Meghan Harrison, PhD, and Alice Vorosmarti, MSPH, for their technical assistance. The authors’ responsibilities were as follows—RPE: wrote the initial draft of the article, which was subsequently reviewed and revised by EYJ and KGD; and all authors: contributed substantively and read and approved the final manuscript.
Notes
The authors reported no funding received for this work.
Author disclosures: The authors report no conflicts of interest. RPE is currently funded with grants from the Centers for Disease Control and Prevention, The National Institutes of Health, The World Health Organization, and the Family Larsson-Rosenquist Foundation. He is also a consultant to the Robert Wood Johnson Foundation Healthy Eating Research Initiative based at Duke University. None of this funding was related to this project or the writing of this commentary. All authors were members of the National Academies of Sciences, Engineering, and Medicine committee that generated the Feeding Infants and Children from Birth to 24 Months: Summarizing Existing Guidance report. The views presented in this commentary reflect those of the individual authors and do not represent those of the National Academies or the committee that authored the consensus report.
Abbreviations used: IYCF, infant and young child feeding; RF, responsive feeding; RP; responsive parenting.
Contributor Information
Rafael Pérez-Escamilla, Email: rafael.perez-escamilla@yale.edu, Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, CT, USA.
Elizabeth Yakes Jimenez, Departments of Pediatrics and Internal Medicine and College of Population Health, University of New Mexico Health Sciences Center, NM, USA.
Kathryn G Dewey, Department of Nutrition and Institute for Global Nutrition, University of California at Davis, Davis, CA, USA.
References
- 1. Pérez-Escamilla R, Segura-Pérez S, Lott M. Feeding guidelines for infants and young toddlers: a responsive parenting approach. Nutr Today. 2017;52(5):223–31. [Google Scholar]
- 2. Pérez-Escamilla R, Segura-Pérez S, Lott M; RWJF HER (Robert Wood Johnson Foundation Healthy Eating Research) Expert Panel on Best Practices for Promoting Healthy Nutrition, Feeding Patterns, and Weight Status for Infants and Toddlers from Birth to 24 Months . Feeding guidelines for infants and young toddlers: a responsive parenting approach. Guidelines for health professionals. Durham (NC): Healthy Eating Research; 2017; [Internet]. Available from: https://healthyeatingresearch.org/wp-content/uploads/2017/02/her_feeding_guidelines_report_021416-1.pdf. [Google Scholar]
- 3. Pérez-Escamilla R, Segura-Pérez S, Hall Moran V. Dietary guidelines for children under 2 years of age in the context of nurturing care. Matern Child Nutr. 2019;15:e12855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pérez-Escamilla R, Segura-Pérez S. Can a pragmatic responsive feeding scale be developed and applied globally?. Matern Child Nutr. 2020;16(3):e13004. doi: 10.1111/mcn.13004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sall NS, Bégin F, Dupuis JB, Bourque J, Menasria L, Main B, Vong L, Hun V, Raminashvili D, Chea C, Chiasson L, Blaney S. A measurement scale to assess responsive feeding among Cambodian young children. Matern Child Nutr. 2020;16(3):e12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pallewaththa P, Agampodi TC, Agampodi SB, Pérez-Escamilla R, Siribaddana S. Measuring responsive feeding in Sri Lanka: development of the Responsive Feeding Practices Assessment Tool. J Nutr Educ Behav. 2021, epub date: March 25, 2021. doi: S1499-4046(21)00051-8.T [DOI] [PubMed] [Google Scholar]
- 7. Bentley ME, Wasser HM, Creed-Kanashiro HM. Responsive feeding and child undernutrition in low- and middle-income countries. J Nutr. 2011;141(3):502–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Black MM, Aboud FE. Responsive feeding is embedded in a theoretical framework of responsive parenting. J Nutr. 2011;141(3):490–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Black MM, Trude ACB, Lutter CK. All children thrive: integration of nutrition and early childhood development. Annu Rev Nutr. 2020;40(1):375–406. [DOI] [PubMed] [Google Scholar]
- 10. Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, Perez-Escamilla R, Rao N, Ip P, Fernald LCHet al. ; Early Childhood Development Interventions Review Group, for the Lancet Early Childhood Development Series Steering Committee. Nurturing care: promoting early childhood development. Lancet North Am Ed. 2017;389(10064):91–102. [DOI] [PubMed] [Google Scholar]
- 11. United Nations Children's Fund (UNICEF) . Improving young children's diets during the complementary feeding period. UNICEF programming guidance. New York: UNICEF; 2020; [Internet]. Available from: https://mcusercontent.com/fb1d9aabd6c823bef179830e9/files/12900ea7-e695-4822-9cf9-857f99d82b6a/UNICEF_Programming_Guidance_Complementary_Feeding_2020_Portrait_FINAL.pdf. [Google Scholar]
- 12. National Academies of Sciences, Engineering, and Medicine . Feeding infants and children from birth to 24 months: summarizing existing guidance. Washington (DC): National Academies Press; 2020. Available from: 10.17226/25747. [DOI] [PubMed] [Google Scholar]
- 13. Jimenez EY, Pérez-Escamilla R, Atkinson SA. Existing guidance on feeding infants and children from birth to 24 months: implications and next steps for registered dietitian nutritionists. J Acad Nutr Diet. 2021;121(4):647–54. [DOI] [PubMed] [Google Scholar]
- 14. Atkinson SA, Jimenez EY, Pérez-Escamilla R. Evidence gaps and research needs in current guidance on feeding children from birth to 24 months. Appl Physiol Nutr Metab. 2021;46(3):294–7. [DOI] [PubMed] [Google Scholar]
- 15. National Academies of Sciences, Engineering, and Medicine (NASEM). Obesity in the early childhood years: state of the science and implementation of promising solutions: Workshop summary. Washington (DC): National Academies Press; 2016. doi: 10.17226/23445. [PubMed] [Google Scholar]
- 16. Redsell SA, Slater V, Rose J, Olander EK, Matvienko-Sikar K. Barriers and enablers to caregivers' responsive feeding behaviour: A systematic review to inform childhood obesity prevention. Obes Rev. 2021;e13228. doi: 10.1111/obr.13228. [DOI] [PubMed] [Google Scholar]
- 17. Skouteris H, Bergmeier HJ, Berns SD, Betancourt J, Boynton-Jarrett R, Davis MB, Gibbons K, Pérez-Escamilla R, Story M. Reframing the early childhood obesity prevention narrative through an equitable nurturing approach. Matern Child Nutr. 2021;17(1):e13094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. FAO . El estado de las guías alimentarias basadas en alimentos en América Latina y El Caribe. Rome (Italy): FAO; 2014; [Internet]. Available from: http://www.fao.org/3/i3677s/i3677s.pdf (accessed 11 November 2020). [Google Scholar]
- 19. US Department of Agriculture ; US Department of Health and Human Services. Dietary guidelines for Americans, 2020–2025. 9th ed. December 2020; [Internet]. Available from: DietaryGuidelines.gov. [Google Scholar]
- 20. Baker P, Melo T, Augusto Neves P, Machado P, Smith J, Piwoz E, Barros AJD, Victora CG, McCoy D. First-food systems transformations and the ultra-processing of infant and young child diets: the determinants, dynamics and consequences of the global rise in commercial milk formula consumption. Matern Child Nutr. 2020:e13097, epub: November 3, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Institute of Medicine . Clinical practice guidelines we can trust. Washington (DC): National Academies Press; 2011; [Internet]. Available from: 10.17226/13058. [DOI] [Google Scholar]
- 22. Rabadán-Diehl C, Safdie M, Rodin R; Trilateral Working Group on Childhood Obesity . Canada-United States-Mexico Trilateral Cooperation on Childhood Obesity Initiative. Rev Panam Salud Publica. 2016;40(2):80–4. [PubMed] [Google Scholar]
- 23. King A, Pérez-Escamilla R, Rivera J. Childhood obesity prevention across borders: the promise of US-Latin American research collaboration. Obes Rev., 2021 May 5:e13238. doi: 10.1111/obr.13238.. [DOI] [PMC free article] [PubMed] [Google Scholar]