Abstract
This study investigated the relationship between redeeming a voucher at hospital-based Medical Food Pantry (MFP) and hospital readmissions in Greenville, NC. Admitted patients at Vidant Medical Center identified as food insecure were given a voucher to the MFP. A retrospective chart review identified demographic information, type of insurance, voucher provision, and redemption dates, food bag type and number of subsequent hospital readmissions for all patients issued a voucher (n = 542) between June 21, 2018 and July 1, 2019. Negative binomial regression analysis assessed the relationship between readmissions and voucher redemption. Sixty percent of patients receiving a voucher were minority (African American) with an average age of 55. Nearly half (48 percent) had Medicare. Thirty-eight percent of those vouchers that were issued were redeemed, usually within five days. Regression results indicate that the number of readmissions was higher among women and non-whites in the sample relative to men and whites. Those patients who redeemed a food voucher had a seven percent lower likelihood of being readmitted (CI, 0.05–0.27). Food insecure patients who redeemed MFP vouchers had a comparatively lower likelihood of subsequent readmissions. These findings suggest that programs targeting modifiable social determinants of health like food insecurity could improve health outcomes and reduce utilization of the healthcare system.
Keywords: Food pantry, Readmissions, Food security
1. Introduction
Healthcare costs in the US are primarily driven by the treatment and management of chronic diseases. Annual health care expenditures total $3.5 trillion and chronic disease treatment comprises 90 percent of that total (Buttorff et al., 2017, Center for Medicare Medicaid Services. National Health Expenditures, 2017). For example, a three-day hospitalization of a patient with type II diabetes averages $30,000 (Protection from High Medical Costs, 2020). While symptomatically different, all chronic diseases are associated with four primary lifestyle risk factors—poor nutrition, lack of physical activity, smoking, and excessive alcohol consumption (Diseases and Center, 2020) – making management of these conditions difficult without social and environmental intervention.
Poor nutrition can be approximated by an individual’s level of food insecurity (Leung and Tester, 2019 Oct, Puddephatt et al., 2020). Defined as limited access to healthful, quality food, food insecure individuals “… [lack] enough food for an active, healthy life.” (Security, 2020) Food insecurity has been associated with poor health outcomes, higher health care costs, and frequent use of the healthcare system (Rabaut, 2019). These frequent users, known as “super users,” are particularly expensive for the healthcare system due to their unmet social needs and costly treatment of health conditions (Phipps et al., 2016).
Due to its association with high medical costs and frequent medical service usage, food insecurity has become the focus of many public, social, and research programs. In order to address food insecurity and improve health outcomes, intervention programs must not only address quantity, but also quality of food. Medically tailored meals (MTMs), meal delivery services, and food pantries with medically tailored options have been developed as mechanisms through which to provide high quality food to support chronic disease management, improve health outcomes, and reduce healthcare expenditures (Center for Medicare Medicaid Services. National Health Expenditures, 2017, Clements et al., 2020).
Evidence suggests that MTMs improve diet, strengthen medical treatment adherence, increase quality of life, and reduce healthcare costs for both diabetic and HIV positive patient populations (Rabaut, 2019, Palar et al., 2017, Berkowitz et al., 2018). The use of pre-prepared meals reduces the burden of food preparation as well as transportation. However, MTMs are often expensive and require staff to prepare and deliver the meals. Food pantries offer an alternative to MTMs at lower cost and without the need for staff to prepare and deliver meals. A food pantry is defined as any food organization that provides unprepared food to individuals in need (Long et al., 2019). Medical food pantries (MFPs), focus on providing food packages or bags tailored to support chronic disease management and promote health rather than addressing hunger alone. While there are millions of food banks operating in the US, there is currently no estimate of how many are located on medical campuses or within hospital settings.
Few studies have evaluated MFPs, particularly those associated with hospitals. Gany et al. (2015) examined the utilization of MFPs by urban cancer patients but lacked data on patient health outcomes to correlate with MFP usage (Greenthal et al., 2019). The first hospital-based food pantry study, published in 2019, focused on patient’s utilization of a 20-year-old pantry and highlighted the potential for reduced stigma (Musicus et al., 2019). The belief that hospital-based MFPs address health rather than need has a positive effect on patient perception (Musicus et al., 2019). In addition to MFPs, a recent study outlined the development and implementation of a hospital-based roof-top farm that focused on reducing food cost by providing fresh produce for patients and employees (Berkowitz et al., 2019).
The absence of studies focusing on patient outcomes associated with hospital-based MFPs leaves many gaps in the literature. Continued evaluation of programs which address food insecurity – a modifiable social determinant of health—and its association with poor chronic disease management, increased healthcare utilization, and higher healthcare costs are needed. While previous studies have demonstrated lower readmissions, reduced healthcare utilization, and lower costs are associated with MTMs, research regarding lower cost programs like hospital-based MFPs is lacking but warranted (Berkowitz et al., 2019, Buys et al., 2017, Brody School of Medicine: Center for Health Disparities, 2020). Therefore, this study investigates the impact of redeeming a hospital-based MFP medically tailored food voucher on patient readmissions.
2. Methods
2.1. Study design
Vidant Medical Center distributes vouchers to their hospital-based MFP to all admitted patients identified as food insecure. A retrospective chart review was conducted for all patients who were issued a voucher between June 21, 2018 and July 1, 2019.
3. Data collection
Electronic Health Records (EHR) data was collected for patients who received a MFP voucher upon discharge and included: voucher status, household size, language, age, county of residence, race, gender, insurance provider, and, if patients were readmitted to the hospital, the admitting department, problem, and diagnosis were collected. Subsequent readmissions were tracked. The total number of readmissions ranged from zero to nine, with an average of one. While the exact duration between each readmission is not known, the total number of readmissions within the observation window is provided.
4. Site and program description
Vidant Medical Center (VMC), one of four academic medical centers in North Carolina, is the flagship hospital for Vidant Health and serves as the teaching hospital for the Brody School of Medicine at East Carolina University (ECU). VMC, located in Greenville, NC, serves as a regional resource for all levels of health services and information. The hospital is a tertiary referral center with 974 licensed beds. It provides acute, intermediate, rehabilitation, and outpatient health services to more than 1.4 million people in 29 counties. Residents in the rural counties served by this regional hospital experience elevated rates of food insecurity, poverty, and chronic disease related health disparities in comparison with the rest of the state. (Du et al., 2012) The MFP was developed in response to acknowledgement by clinicians and administrators at VMC and Brody School of Medicine, of the correlation between food insecurity and poor health outcomes. Every patient admitted to VMC is screened for food insecurity using two questions from the Hunger Vital Signs questionnaire. Previous studies have used the Vital Hunger Signs, a two-question food insecurity screening, and demonstrated validity and sensitivity within clinical settings. (Rabaut, 2019)
Hunger Vital Signs Questions:
(1) “Within the past 12 months we worried whether our food would run out before we got money to buy more?”
Responses included never, sometimes true, or always true.
(2) “Within the past 12 months the food we bought just didn’t last and we didn’t have money to get more?”
Responses included never, sometimes true, or always true.
Patients were identified as food insecure if they answered “sometimes true” or “always true” to at least one question on the Vital Hunger Signs screener. Patients identified as food insecure, were given nutrition education, instructions from a clinical registered dietitian nutritionist, and a voucher for a medically tailored food bag. The registered dietitian nutritionist also determined the type of medically tailored food bag based on their clinical assessment of the patient’s medical conditions, and nutritional needs, and the patient’s current hospital diet order. The voucher provided patients with one of three types of food bags containing approximately 20 lb of donated, non-perishable foods designed by a registered dietitian nutritionist. The three types of bags included balanced diet (general, healthy), carbohydrate control or low sodium. Patients with type II diabetes were most commonly provided a carbohydrate-controlled bag, and patients with a cardiovascular related diagnosis (e.g. hypertension) received a low sodium bag, and patients without a nutrition related chronic disease received a general/healthy bag. Food bags were intended to support the patient’s immediate nutrition needs until connections could be made with resources in the patient’s home community. All bags consisted of various meat, starchy/non-starchy vegetables, fruits, grains, cereals, beans, and dairy. Quantities, types, and proportions of these items were adjusted based on the dietary prescription of the respective bag.
Following discharge, patients were encouraged to redeem vouchers within 72 h at the MFP. The MFP was located on the VMC campus. The MFP assembled, stored, and distributed the medically tailored food bags to patients based on the guidance of a registered nutritionist/dietician. Those patients who redeemed their voucher also received a follow up phone call from the Vidant Health MFP coordinator. Patients who redeemed vouchers were asked a set of questions to ensure coordination of longer-term community-based social support, reinforce dietary requirements, and receive feedback on the items in their bags. Individuals who did not redeem vouchers were asked a different set of questions to understand what resources may or may not be available to the individual. They were asked if they received a voucher to verify distribution which had been documented. Patients were also asked if they had a conversation with the dietitian regarding the purpose of the food bag. They were also invited to redeem their voucher as well as asked about their utilization of any local community-based food resources. If patients responded “no” they were asked if they would like to be connected to any local community-based food resources.
4.1. Data analysis
Data analysis utilized SAS 9.4 (Cary, NC) and included descriptive and regression analysis. Analysis focused on hospital readmissions. While use of a binary independent variable indicating whether or not the patient had any readmissions was possible, this type of specification would have treated patients with one readmission to be the same as those who had multiple readmissions. Therefore, a count of the total number of readmissions was used as the dependent variable to exploit heterogeneity between patients. Use of this type of count data is increasingly common in clinical research, but significant results can be obscured if models are not specified correctly. (Poretsky, 2017) One important characteristic of counts is that the variance tends to increase with the average size of the counts. In studies of repeated events, such as this one where durations are not known, counts are generally higher than the number of patients in the sample. These attributes preclude the use of Poisson estimation—the most popular count data model—since Poisson models assume that the expected value of the random variable is equal to its variance. Since this data presents significant overdispersion—a disproportionately large number of patients had zero readmissions—a derivative of the Poisson mode, the negative binomial (NB), was estimated. The NB is appropriate when the mean parameter is not identical for all members of the population, but itself is distributed with a gamma distribution. The NB distribution accounts for population heterogeneity and overdispersion providing greater flexibility in modeling the relationship between the expected value and the variance of the dependent variable. The count of total readmissions was estimated using SAS 9.4 (Cary, NC) command Proc Genmod for repeated measures data and statistical significance was set at P < 0.05. All research and analysis was done under the supervision of the East Carolina University IRB.
5. Results
The final patient sample (n = 542) was 60 percent Africa American, 57 percent male, and had an average age of 55 (sd = 14.7). Nearly half (48 percent) of patients were on Medicare and 15 percent on Medicaid. The remainder of patients had private insurance. Prior to the end of the observation window, 14 percent of patients were identified as deceased with cause of death unknown. Thirty-eight percent of patients redeemed vouchers for their medically tailored food bag within an average of five days (sd = 13.2). Food vouchers were roughly equal among balanced diet, low sodium, and carbohydrate control with a slightly higher percentage (36 percent) of patients receiving a carbohydrate-controlled diet food bag. Household size ranged from one to eight, but patients, on average lived in a two-person household. Patients were residents of eight different counties and less than two percent were Spanish speaking (Table 1).
Table 1.
Descriptive Statistics for VMC MFP Patients June 21, 2018 to July 1, 2019.
| N | Mean | Std Dev | Min | Max | |
|---|---|---|---|---|---|
| Total Readmissions | 542 | 0.723 | 1.2 | 0 | 9 |
| Days until Redemption | 204 | 5.0e | 12.13 | 0 | 87 |
| Age | 541 | 55.49 | 14.75 | 30 | 99 |
| HH Size | 473 | 1.99 | 1.14 | 1 | 8 |
| Redeemed | 542 | 0.38 | 0.49 | 0 | 1 |
| Repeat Redemption | 542 | 0.07 | 0.25 | 0 | 1 |
| N | Percent | ||||
| Food Bag Type | |||||
| Carb Control | 189 | 35 | |||
| Low Sodium Diet | 155 | 30 | |||
| Balanced Diet | 198 | 35 | |||
| Insurance | |||||
| Private | 135 | 27.14 | |||
| Medicaid | 119 | 23.94 | |||
| Medicare | 243 | 48.89 | |||
| Language | |||||
| English | 533 | 98.34 | |||
| Spanish | 9 | 1.66 | |||
| Gender | |||||
| Male | 315 | 58.12 | |||
| Female | 227 | 41.88 | |||
| Race | |||||
| Black | 320 | 59.04 | |||
| Hispanic | 17 | 3.14 | |||
| Other | 2 | 0.37 | |||
| Unknown | 1 | 0.18 | |||
| White | 202 | 37.27 | |||
| Mortality | |||||
| Living | 468 | 86.35 | |||
| Deceased | 74 | 13.65 | |||
| Redeemed | Did Not Redeem | ||||
| Insurance | |||||
| Other | 68 | 25.81 | 112 | 27.97 | |
| Medicaid | 49 | 26.34 | 70 | 22.51 | |
| Medicare | 89 | 47.85 | 154 | 49.52 | |
| Language | |||||
| English | 203 | 98.54 | 330 | 98.21 | |
| Spanish | 3 | 1.46 | 6 | 1.79 | |
| Gender | |||||
| Male | 122 | 59.22 | 193 | 57.44 | |
| Female | 84 | 40.78 | 143 | 42.56 | |
| Race | |||||
| Black | 126 | 61.17 | 194 | 57.74 | |
| Hispanic | 5 | 2.43 | 12 | 3.57 | |
| Other | 0 | 0 | 2 | 0.6 | |
| Unknown | 1 | 0.49 | 0 | 0 | |
| White | 74 | 35.92 | 128 | 38.1 | |
| Mortality | |||||
| Living | 176 | 85.44 | 292 | 86.9 | |
| Deceased | 30 | 14.56 | 44 | 13.1 | |
The lower panel of Table I allows for comparison of patients who redeemed and did not redeem vouchers. Both groups have similar racial, gender, and linguistic distributions and have equal proportions of privately insured patients. These statistics suggest that patients who did and did not redeem vouchers display similar observable characteristics.
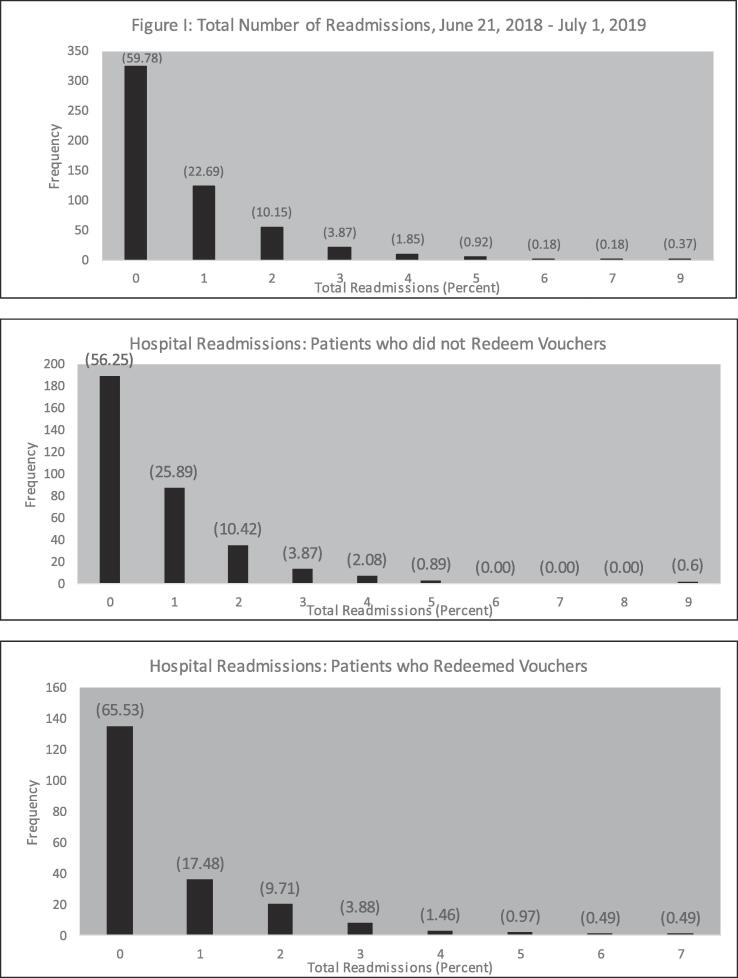
Most patients had either zero or one readmission to the hospital, however, the highest number observed was nine. Fig. 1 and Table 1 show the frequency of readmissions for the full sample, both those who redeemed vouchers and those who did not redeem vouchers. Sixty percent of patients were not readmitted to the hospital and 23 percent were readmitted only once. A small number of patients had two, three, or four readmissions, 10 percent, four percent, and two percent respectively. Less than one percent of the sample was readmitted more frequently. The average number of readmissions was seven percent lower for those who redeemed vouchers than those who did not.
Fig. 1.
Total Number of Readmissions, June 21, 2018 - July 1, 2019.
Results from the negative binomial model regression are presented in Table 2. Regression coefficients indicate that for a one-unit change in the predictor variable, the difference in the logs of expected readmissions changed by the amount of the respective regression coefficient, given the other predictor variables in the model are held constant. For a more intuitive interpretation, results are also presented in the form of marginal effects. Marginal effects measured changes in readmission corresponding to a unit change in the independent variable. Estimates indicated a negative relationship between readmissions and redemption of a food voucher. Redemption was associated with seven percent lower average number of readmissions. Females had 23 percent higher average readmissions while whites have 11 percent lower readmissions all other variables constant. Those at older ages had lower average readmissions, but only slightly (ME = -0.03 CI = -0.04, −0.02). One probable interpretation of this association is that elderly individuals could reside in long-term care or assisted living facilities with nursing staff nearby, therefore only requiring hospitalization in the direst circumstance. Those who died during the panel had a higher average number of readmissions (ME = 0.47 CI = 0.08, 0.86), consistent with declining health.
Table 2.
Negative Binomial Regression of Total Patient Readmissions June 21, 2018 to July 1, 2019.
| Chi-Square = 4916.6* |
AIC = 13998.7 |
||
|---|---|---|---|
| Parameter | Estimate** (Std. Dev) | Chi-Square | Marginal Effect*** (Confidence Interval) |
| Intercept | 0.70* (0.09) | 56.29 | |
| Redeemed | −0.07* (0.04) | 2.85 | −0.07 (−0.28,0.14) |
| Carb Control | 0.73* (0.06) | 227.71 | 0.79 (0.36,1.22) |
| Low Sodium Diet | 0.43* (0.05) | 65.19 | 0.47 (0.03, 0.90) |
| Medicaid | 0.04 (0.06) | 0.53 | 0.05 (−0.55, 0.65) |
| Medicare | 0.32* (0.045) | 52.46 | 0.35 (0.00, 0.70) |
| Female | 0.21* (0.04) | 29.30 | 0.23 (−0.18, 0.64) |
| Age | −0.03* (0.00) | 285.39 | −0.03 (−0.04, −0.02) |
| White | −0.10* (0.042) | 6.03 | −0.11 (−0.58, 0.35) |
| Deceased | 0.44* (0.05) | 69.14 | 0.47 (0.08, 0.86) |
| Dispersion | 0.82 (0.04) | ||
| N = 542 | |||
| *=Denotes statistical significance, α = 0.05 | |||
| **Estimate = percent change in readmissions over the study period associated with voucher redemption. | |||
| ***Marginal Effects = absolute change in readmissions over the study period associated with a one-unit change in the explanatory variable | |||
| Dependent variable: total readmissions. | |||
| Patients were issued one of three food vouchers: Carb Control, Low Sodium or Balanced Diet. For regression analysis, Balanced Diet was the omitted category. | |||
Individuals receiving the carbohydrate control and low sodium food bags had higher average readmissions, compared to the reference group. Medicaid did not show any significant association with the number of readmissions; however, receipt of Medicare Health Insurance was correlated with higher average readmissions compared to those with private insurance.
6. Discussion
This study examined the relationship between medically tailored food voucher redemption and hospital readmissions. It suggested that lower-cost programs (like MFPs) targeting modifiable social determinants of health (food insecurity) had the potential to improve patient health outcomes and reduce costly hospitalizations. To the authors’ knowledge, it was the first empirical study to analyze the association between patient outcomes and use of an MFP. It differed from existing MTM studies, which mostly involved urban populations, by examining a rural, under-served patient population.
While a lower number of readmissions were associated with redemption of a food voucher, readmissions varied by the type of food bag provided. For example, the carbohydrate-controlled bag was provided to patients suffering from poor diet quality, glycemic control, and management of diabetes. These individuals showed a higher number of readmissions, likely a result of the confounding effects of diet on their condition (Heather, 2020, Berkowitz et al., 2013, Hess et al., 2017 Feb 7). Their chronic disease management was likely impeded post-discharge by poor access to healthy food in their higher readmission rates.
In addition to food bag type, individuals who were female, African American, and older had higher, on average, readmissions than males, non-African Americans, and younger recipients, respectively. This is consistent with other studies showing that African Americans experience an elevated burden of chronic diseases, comorbidities, and social risk factors such as low income and food insecurity (Nastars et al., 2019 Aug, Hasson et al., 2015 Jun, Clements et al., 2020, Hernandez et al., 2017 Oct, Courtney et al., 2009). Age was negatively associated with readmissions. This result has two possible explanations. First, older patients may have been receiving long term or other unobserved source of care which contributed to their lower readmission rates (Takahashi et al., 2012, Strom et al., 2017). Second, coupled with the positive association between death and readmissions, the negative age relationship could indicate that elderly patients who survived throughout the observation window, were comparatively healthier than those who did not survive. While Buys et al. showed no significant impact from provision of food and nutrition education in patients over 65, their study only included a short-term provision and noted that Medicare patients were generally more vulnerable and experienced poorer health outcomes than those with private insurance (Brody School of Medicine: Center for Health Disparities, 2020, Baldwin et al., 2017, Tumin et al., 2016 Sep, Smith et al., 2017).
Despite differences in observed readmission rates, results demonstrated that addressing food security was associated with improved health outcomes. Studies showing similar results from other nutrition and MTM programs relied on staff to make and deliver meals – resources that are not always attainable or affordable (Berkowitz et al., 2018, Buys et al., 2017). Hospital-based MFPs, in contrast, rely on donated food – a low cost and sustainable option. However, MFPs do require patients to prepare food or follow nutritional guidelines established by providers. While this does present a potential barrier, results showed significantly lower readmissions among those who redeemed food vouchers compared to those who did not. Future support efforts might consider supplementing with nutrition education or culinary support to facilitate simple, fast, healthful food preparation at home. However, authors of this study cannot exclude the possibility that the relationship between readmissions and voucher redemption was due, in part, to selection bias—unobserved differences between patients who redeemed and did not redeem vouchers.
In addition to screening for and addressing food insecurity, VMC MFP clinicians made efforts to connect patients with community-based resources and follow-up regarding the utilization of these resources. However, the status of these connections is currently unknown. The authors of this study acknowledge that utilization of community-based resources is a core component of the intervention and this information is critical to understanding the long-term impact of the program. While community-based resources may offer a long-range solution, the best mode of community outreach is not always clear, and patients vary in their willingness to utilize various support mechanisms. For example, food insecure patients at a student-run ambulatory clinic were connected with local off-site food resources after their discharge but showed low rates of utilization.35 These lower rates of utilization were likely due to short windows of availability, challenges accessing continuous supply of volunteers, and difficulty informing patients of operating hours (Greenthal et al., 2019). Low utilization rates could also result from the negative social stigma associated with certain community organization and patients reportedly perceived MFPs differently than other community resources suggesting that partnerships between pantries and healthcare organizations may improve use (Musicus et al., 2019).
While this study showed that efforts by the VMC-MFP to address food security were correlated with reduced healthcare utilization, it faced several limitations. First, it was not possible to account for situational confounders such as household income, alternative nutritional resources, or other community resource utilization. Second, after redeeming vouchers, patients received follow-up calls from MFP staff connecting them with community resources. However, no information was available on the utilization of these community resources which may have impacted outcomes. Third, individual clinical data on patients was not available for this study and the severity of disease and comorbidities may have impacted readmission rates. Fourth, some patients may have had limited accessibility to the MFP due to geographic distance and temporary closure of the MFP. Additionally, the total number of readmissions does not include admissions to other hospitals or outpatient centers (urgent care, etc.); in other words, estimates likely reflect the lower bound of readmission rates since individuals could have received treatment elsewhere. Finally, this study was conducted with patients in a rural, under-served community making results difficult to generalize to other geographic areas or urban communities.
7. Conclusion
Results indicate that redemption of a voucher for a medically tailored food bag was associated with reduced healthcare utilization rates in the form of fewer hospital admissions. By screening for and addressing food insecurity, use of the VMC MFP was correlated with improved patient outcomes. Therefore, addressing modifiable social determinants of health could potentially improve patient health and reduce overall medical costs. This work contributes to the growing body of literature examining the intersectionality of social circumstances and health. Given that social circumstances, health outcomes, and health services utilization cannot be disentangled, they should be treated as confounding issues and addressed simultaneously.
Receipt of a medically tailored food bag was significantly correlated with lower hospital readmissions and could potentially correspond to improved patient outcomes. This study, coupled with evidence from similar MTM programs, suggests that food could be used as a preventative treatment. It also suggests that hospitals could be used to connect food insecure patients with resources such as the VMC MFP. MFPs offer a lower-cost, potentially impactful mode of addressing modifiable social determinant of health. Additional research surrounding community-based programs like MFPs, particularly those targeting a high priority patient population, is warranted. Studies exploring the cost-effectiveness of such programs and their long-term sustainability would provide important insight. Additionally, a detailed examination of health outcomes among patients who did not redeem vouchers would inform program design to best reach a diverse group of patients.
CRediT authorship contribution statement
Lauren Sastre: Writing - review & editing. Desiree Wynn: Conceptualization. Melissa Roupe: Conceptualization. Molly Jacobs: Software, Formal analysis, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank several supporters of the Medical Food Pantry (MFP), for without their support this vital community resource would not be possible. We would like to thank Gideon Adams and George Young with the Food Bank of Central & Eastern NC for their leadership and support to establish the MFP. We would also like to thank several individuals at Vidant and ECU Physicians including; Debra Thompson, Jeff Dial and Dr. Jason A Foltz. We would like to thank Njeri Njuguna for her role in developing the inpatient referral process and her team’s role in issuing food vouchers for the medical food pantry as well as Kay Craven- and Dr. Kathy Kolasa for their work to develop the medically tailored food bags, patient education materials, and questions/script for follow-up patient phone calls. Lastly, we would like to thank all of the donors and community volunteers, without which we would not have been able to maintain the MFP.
References
- Baldwin M.R., Sell J.L., Heyden N., Javaid A., Berlin D.A., Gonzalez W.C., Bach P.B., Maurer M.S., Lovasi G.S., Lederer D.J. Race, ethnicity, health insurance, and mortality in older survivors of critical illness. Crit. Care Med. 2017;45(6):e583–e591. doi: 10.1097/CCM.0000000000002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013 Oct;36(10):3093-9. doi: 10.2337/dc13-0570. Epub 2013 Jun 11. [DOI] [PMC free article] [PubMed]
- Berkowitz S.A., Terranova J., Hill C., Ajayi T., Linsky T., Tishler L.W., DeWalt D.A. Meal delivery programs reduce the use of costly health care in dually eligible medicare and medicaid beneficiaries. Health Aff (Project Hope) 2018;37(4):535–542. doi: 10.1377/hlthaff.2017.0999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz S.A., Delahanty L.M., Terranova J., Steiner B., Ruazol M.P., Singh R., Shahid N.N., Wexler D.J. Medically tailored meal delivery for diabetes patients with food insecurity: A Randomized Cross-over Trial. J. Gen. Intern. Med. 2019;34(3):396–404. doi: 10.1007/s11606-018-4716-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz S.A., Terranova J., Randall L., Cranston K., Waters D.B., Hsu J. Association between receipt of a medically tailored meal program and health care use. JAMA Inten. Med. 2019;179(6):786. doi: 10.1001/jamainternmed.2019.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody School of Medicine: Center for Health Disparities. https://www.ecu.edu/cs-dhs/healthdisparities/ Accessed March 31, 2020.
- Buttorff C., Ruder T., Bauman M. Rand Corp; Santa Monica, CA: 2017. Multiple Chronic Conditions in the United States pdf icon[PDF – 392 KB]external icon. [Google Scholar]
- Buys D.R., PhD M.S.P.H., Campbell A.D., Godfryd A. Meals enhancing nutrition after discharge: Findings from a Pilot Randomized Controlled Trial. J. Acad. Nutr. Diet. 2017;117:599–608. doi: 10.1016/j.jand.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Medicare & Medicaid Services. National Health Expenditures 2017 Highlights pdf icon[PDF – 74 KB]external icon.
- Clements J.M., West B.T., Yaker Z., Lauinger B., McCullers D., Haubert J., Tahboub M.A., Everett G.J. Disparities in diabetes-related multiple chronic conditions and mortality: The influence of race. Diabetes Res. Clin. Pract. 2020;159:107984. doi: 10.1016/j.diabres.2019.107984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mary Courtney Helen Edwards Anne Chang Anthony Parker Kathleen Finlayson Kyra Hamilton Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: A randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program 57 3 2009 395 402. [DOI] [PubMed]
- About Chronic Diseases, National Center for Chronic Disease Prevention and Health Promotion, The Centers for Disease Control and Prevention. https://www.cdc.gov/chronicdisease/about/prevent/index.htm Accessed February 12, 2020, Page last reviewed: October 23, 2019.
- Du J., Park Y.-T., Theera-Ampornpunt N., McCullough J.S., Speedie S.M. The use of count data models in biomedical informatics evaluation research. J. Am. Med. Inform. Assoc. 2012;19(1):39–44. doi: 10.1136/amiajnl-2011-000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gany F., Lee T., Loeb R., Ramirez J., Moran A., Crist M., McNish T., Leng J.C.F. Use of hospital-based food pantries among low-income urban cancer patients. J. Community Health. 2015;40(6):1193–1200. doi: 10.1007/s10900-015-0048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenthal E., Jia J., Poblacion A., James T. Patient experiences and provider perspectives on a hospital-based food pantry: a mixed methods evaluation study. Public Health Nutr. 2019;22(17):3261–3269. doi: 10.1017/S1368980019002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasson B.R., Apovian C., Istfan N. Racial/Ethnic differences in insulin resistance and beta cell function: Relationship to racial disparities in Type 2 Diabetes among African Americans versus Caucasians. Curr. Obes. Rep. 2015;4(2):241–249. doi: 10.1007/s13679-015-0150-2. [DOI] [PubMed] [Google Scholar]
- Eicher-Miller HA. A review of the food security, diet and health outcomes of food pantry clients and the potential for their improvement through food pantry interventions in the United States. Physiol Behav. 2020 Mar 13:112871. doi: 10.1016/j.physbeh.2020.112871. [Epub ahead of print]. [DOI] [PubMed]
- Hernandez D.C., Reesor L.M., Murillo R. Food insecurity and adult overweight/obesity: Gender and race/ethnic disparities. Appetite. 2017;1(117):373–378. doi: 10.1016/j.appet.2017.07.010. Epub 2017 Jul 22. [DOI] [PubMed] [Google Scholar]
- Hess C.N., Kaltenbach L.A., Doll J.A., Cohen D.J., Peterson E.D., Wang T.Y. Race and Sex Differences in Post-Myocardial Infarction Angina Frequency and Risk of 1-Year Unplanned Rehospitalization. Circulation. 2017;135(6):532–543. doi: 10.1161/CIRCULATIONAHA.116.024406. [DOI] [PubMed] [Google Scholar]
- Leung C.W., Tester J.M. The association between food insecurity and diet quality varies by race/ethnicity: An Analysis of National Health and Nutrition Examination Survey 2011–2014 Results. J Acad Nutr Diet. 2019 Oct;119(10):1676–1686. doi: 10.1016/j.jand.2018.10.011. Epub 2018 Dec 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long C.R., Rowland B., Steelman S.C., McElfish P.A. Outcomes of disease prevention and management interventions in food pantries and food banks: a scoping review. BMJ Open. 2019;9(8):e029236. doi: 10.1136/bmjopen-2019-029236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musicus A.A., Vercammen K.A., Fulay A.P., Moran A.J., Burg T., Allen L., Maffeo D., Berger A., Rimm E.B. Implementation of a rooftop farm integrated with a teaching kitchen and preventive food pantry in a hospital setting. Am J Public Health. 2019;109(8):1119–1121. doi: 10.2105/AJPH.2019.305116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nastars D.R., Rojas J.D., Ottenbacher K.J., Graham J.E. Race/Ethnicity and 30-day readmission rates in medicare beneficiaries With COPD. Respir Care. 2019;64(8):931–936. doi: 10.4187/respcare.06475. Epub 2019 Mar 26. [DOI] [PubMed] [Google Scholar]
- Palar K., Napoles T., Hufstedler L.L., Seligman H., Hecht F.M., Madsen K., Ryle M., Pitchford S., Frongillo E.A., Weiser S.D. Comprehensive and medically appropriate food support is associated with improved HIV and Diabetes Health. J Urban Health. 2017;94(1):87–99. doi: 10.1007/s11524-016-0129-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps E.J., Singletary S.B., Cooblall C.A., Hares H.D., Braitman L.E. Food Insecurity in Patients with High Hospital Utilization. Popul Health Manag. 2016;19(6):414–420. doi: 10.1089/pop.2015.0127. [DOI] [PubMed] [Google Scholar]
- Sonmez H, Kambo V, Avtanski D, Lutsky L, Poretsky L.The readmission rates in patients with versus those without diabetes mellitus at an urban teaching hospital.J Diabetes Complications. 2017 Dec;31(12):1681-1685. doi: 10.1016/j.jdiacomp.2017.07.006. Epub 2017 Jul 19. [DOI] [PubMed]
- Protection from High Medical Costs. https://www.healthcare.gov/why-coverage-is-important/protection-from-high-medical-costs/ Accessed February 12, 2020.
- J.-A. Puddephatt G.S. Keenan A. Fielden D.L. Reaves J.C.G. Halford C.A. Hardman 147 2020 104547 10.1016/j.appet.2019.104547. [DOI] [PubMed]
- Rabaut L.J. Medically tailored meals as a prescription for treatment of food-insecure Type 2 Diabetics. J. Patient Cent. Res. Rev. 2019;6(2):179–183. doi: 10.17294/2330-0698.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food Security in the U.S., Overview. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/ Accessed February 12, 2020, Last updated: Wednesday, September 04, 2019.
- Smith S., Malinak D., Chang J., Perez M., Perez S., Settlecowski E., Rodriggs T., Hsu M., Abrew A., Aedo S. Implementation of a food insecurity screening and referral program in student-run free clinics in San Diego, California. Prev. Med. Rep. 2017;5:134–139. doi: 10.1016/j.pmedr.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strom J.B., Kramer D.B., Wang Y., Shen C., Wasfy J.H., Landon B.E., Wilker E.H., Yeh R.W., Jia Z. Short-term rehospitalization across the spectrum of age and insurance types in the United States. PLoS One. 2017;12(7):e0180767. doi: 10.1371/journal.pone.0180767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi P.Y., Pecina J.L., Upatising B., Chaudhry R., Shah N.D., Van Houten H., Cha S., Croghan I., Naessens J.M., Hanson G.J. A randomized controlled trial of telemonitoring in older adults with multiple health issues to prevent hospitalizations and emergency department visits. Arch. Inter. Med. 2012;172(10) doi: 10.1001/archinternmed.2012.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumin D., Foraker R.E., Smith S., Tobias J.D., Hayes D., Jr. Health insurance trajectories and long-term survival after heart transplantation. Circ. Cardiovasc Qual. Outcomes. 2016;9(5):576–584. doi: 10.1161/CIRCOUTCOMES.116.003067. Epub 2016 Sep 13. [DOI] [PubMed] [Google Scholar]