Abstract
Objective:
To determine the reliability, responsiveness, and convergent validity of the Four-Meter Walk Test (4mWT) compared to the Six-Minute Walk Test (6MWT) surrounding total knee arthroplasty (TKA).
Design:
Secondary analysis of a randomized controlled trial.
Setting:
Research laboratory
Participants:
One hundred sixty-two patients (aged 63.5 ± 7.4 (mean ± sd) years; 89 females) undergoing TKA participated.
Main Outcome Measures:
4mWT (usual and fastest) and 6MWT were measured 1–2 weeks preoperatively, and 1, 2, 3, 6 and 12 months post-operatively.
Results:
4mWT demonstrated excellent test-retest reliability with Interclass Correlation Coefficients (ICC’s) ranging from 0.80s to 0.93. 4mWT also demonstrated small measurement error with Standard Error of Measurement (SEM) ranging from 0.15s to 0.35s. 4mWT (fastest) demonstrated similar responsiveness to 6mWT in the first 2 months after surgery and better responsiveness from 2 to 3 months after surgery. Convergent validity between 6MWT and 4mWT (fastest) was high, with Pearson correlation coefficients ranging from 0.73 to 0.81.
Conclusions:
The 4mWT (fastest) has excellent test-retest reliability, shows high responsiveness sufficient for clinical outcomes in the immediate postoperative time periods, and exhibits high convergent validity with 6MWT. Given space and time requirements to conduct each test, 4mWT may be preferred for routine clinical assessment.
Keywords: Prognosis, Gait, Outcome Measure, Osteoarthritis, Rehabilitation
INTRODUCTION
Over 700,000 total knee arthroplasties (TKAs) are performed annually in the United States and this number is expected to rise to over 3.5 million by the year 2030 due to the aging of the population, obesity, and increasing utilization of the surgery.[1,2] Walking is a major activity limitation following TKA with reductions of walking distance of 39% compared to preoperative levels in the first month following surgery.[3] Walking recovery plateaus in the first 3–6 months after TKA; however, walking ability in the long-term remains decreased by 28% compared to age matched healthy adults.[3,4] Additionally, walking ability, measured with walking speed, has been shown to be related to discharge location, rehabilitation needs, fall risk, loss of independence, future hospitalizations, and mortality.[5–12]
Clinically, improving walking ability is a major focus of the overall plan of care for patients presenting to physical therapy after TKA.[13] Additionally, the need to capture physical performance data from the perspective of payers is becoming increasingly important given the emphasis on demonstrating patient improvement and quality of care. While self-reported outcomes are commonly utilized after TKA, they may not accurately reflect physical performance and are highly correlated with pain recovery.[14–19] Therefore, accurate outcome tracking of walking ability is important from the patient perspective, the physical therapist perspective, as well as from a payer perspective. Reliability, validity, and responsiveness to change are major factors to consider when selecting an outcome measure. Additionally, potential floor and ceiling effects as well as clinical utility are other major factors to consider when selecting an outcome measure. Two potential outcome measures to quantify walking ability after TKA are the Six-minute Walk Test (6MWT) and a short walking speed test such as the 4-Meter Walk Test (4mWT).[20,21]
The 6MWT has been studied extensively in patients after TKA as well as is in a recommended core battery of physical performance tests for individuals with knee osteoarthritis (OA).[4,14,22,23] The 6MWT has been shown to be a reliable and valid outcome measure demonstrating excellent intra-rater reliability[4] as well as a strong relationship to longer walking distances[24] and recovery prognosis.[25] The 6MWT has also been shown to be a responsive measure at 7 weeks after TKA.[4] From a clinical utility perspective, this is a challenging outcome measure for many clinicians to utilize given it requires a walking track or large corridor (typically 30m or greater), and it takes up to 10 minutes to conduct.[26]
Given the limited clinical utility of the 6MWT, an important clinical question is: Can a short walking speed test such as the 4m-walk test (4mWT) test be utilized in place of the 6MWT? The clinical utility of the 4mWT is much higher because it requires only an eight-meter walkway and takes less time to administer.[21] It is clear that the 6MWT is a longer test and therefore potentially a better measure of walking endurance; however, if the rationale in selecting a walking test as an outcome is based on capturing walking ability in general as well as assessing progress during rehabilitation, the 4mWT may be a sound choice. Moreover, walking speed has been advocated as a sixth vital sign and recommended as a routine outcome measure for clinical practice.[27] Before recommending utilization of the 4mWT, it is important to establish its reliability, responsiveness and validity compared to the 6MWT during common clinical time points after TKA. Only one study to date has examined the reliability of the 4mWT (fastest) after TKA, however this study only examined individuals in the immediate postoperative period during inpatient rehabilitation.[28] No studies to date have examined the responsiveness or construct validity of the 4mWT compared to the 6MWT.
Therefore, the purpose of this study was to determine the reliability, responsiveness, and construct validity of the 4mWT compared to the 6MWT surrounding TKA. We hypothesized that the 4mWT would demonstrate almost perfect test-retest reliability, large responsiveness similar to the 6MWT, and high levels of construct validity with the 6MWT.
METHODS
Study Design
This was a secondary analysis of a randomized controlled trial that examined the difference between a high-intensity rehabilitation program compared to a low-intensity rehabilitation program. Full details of this clinical trial have been published elsewhere.29
Subjects
Patients were consecutively recruited by nine participating orthopedic surgeons at four institutions from August 2011 to November 2014. Patients aged 50 to 85 years were included if they were awaiting a primary, unilateral TKA secondary to knee OA. Exclusion criteria were: 1) current smoker; 2) current cancer treatment; 3) uncontrolled diabetes (hemoglobin A1c level >7.0); 4) body mass index (BMI) greater than 40 kg/m2; 5) neurological, vascular, or cardiac problems that limited function; 6) discharge to location other than home after surgery (e.g., skilled nursing facility); 7) severe contralateral knee OA (>5/10 pain with stair climbing) or other orthopedic conditions that limited function and necessitated alternative concurrent intervention (e.g., severe lumbar spinal stenosis; severe hip or ankle OA). Informed consent was obtained from all participants. The study was approved by the (removed for blinding) Institutional Review Board and registered at ClinicalTrials.gov (removed for blinding).
Interventions
Surgical technique and implant selection were based on surgeon preference. All components were cemented and the operations were performed via a medial parapatellar or mid-vastus approach, using either posterior-stabilized or cruciate-retaining implants with fixed or mobile bearing components. The patella was resurfaced in all instances. Following surgery, all patients received inpatient physical therapy twice daily prior to discharge. The high-intensity and low-intensity interventions were initiated 4.2 ± 1.2 (mean ± sd) days after surgery. All patients were seen 2–3 times per week over 11 weeks in an outpatient physical therapy setting for a total of 26 visits. The high-intensity intervention consisted of a progressive resistance exercise program targeting major lower extremity muscle groups and a rapid progression to weight-bearing exercises targeting key activities in addition to balance and agility training. The low-intensity intervention had an initial focus on isometric exercise and active range of motion exercise with a slower progression to weight-bearing exercises and activities compared to the high-intensity intervention. Both interventions included patient education on pain, swelling, and wound management; training on transfers, gait, and stair climbing; range of motion techniques; and instruction in a home exercise program.
Outcomes
All outcomes were assessed 1–2 weeks preoperatively and at 1, 2, 3, 6 and 12 months postoperatively by a blinded outcome assessor (blinded to group assignment). A total of six testers administered assessments over the course of the study period. Testers were trained by lead researchers on the investigative team according to a manual of operating procedures.
Four-Meter Walk Test
This test measures two walking speeds for each participant: usual speed and fastest speed. For the 4mWT (usual), patients were instructed to walk at their usual, comfortable speed. For the 4mWT (fastest), patients were instructed to walk safely at their fastest speed without running.
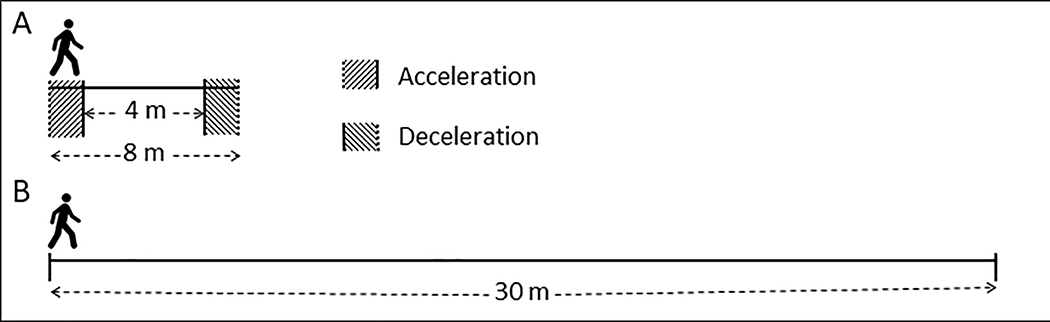
Two trials were measured at each of the two speeds, and the average time was used in reporting. Patients were placed on a path marked at 0, 2, 6, and 8 meters (figure 1). The 0–2 meter interval allowed for acceleration. Four-meter walking speed was measured in the 2–6 meter interval. The final 6–8 meter interval provided for 2 meters of deceleration. For both speeds, patients were instructed to continue walking through the 2–6 meter interval to the 8 meter mark to eliminate the effects of early deceleration. The time started when the participant’s front foot crossed the 2 meter line and stopped when their front foot crossed the 6 meter line. A digital stopwatch was used to measure the time. Two trials were performed with a rest period (usually less than 1 min) between trials. Total time to assess both versions of the 4mWT (usual and fastest) was less than 4 min.
Figure 1.
Space requirements and course setup for A) 4mWT, including 2-meter acceleration/deceleration zones; and B) 6MWT.
Six-Minute Walk Test
This 6MWT measures the distance a patient can walk in 6 minutes and was assessed with a 30.5 meter walkway with a tape marker at each end, and tape marks placed every 3 meters along the walkway.[20] One full lap was 30.5m x 2, or 61 meters. Only one foot was required to cross the tape at the end of the walkway prior to turning to complete the lap. The participant was instructed “to safely cover as much distance as possible in six-minutes.” At the end of six-minutes, the participant was instructed to stop. Total distance was estimated to the nearest 3 meters by using the marks on the walkway. The same rater assessed both 6MWT and the 4mWT (usual and fastest) for a given testing session. Only one trial of the 6MWT was conducted.
Statistical Analysis
Group data from the parent trial were pooled for this analysis as there were no differences in any outcomes between groups over time.[29] Descriptive statistics (e.g., mean +/− standard deviation) were utilized to report participant characteristics as well as the 4mWT and 6MWT results over time. The test-retest reliability of the 4mWT was described by intraclass correlation coefficients (ICCs) (Type 2,1) at all assessment times.[30] Intraclass correlation coefficients were characterized using the following scale[31]: slight (ICC 0.00–0.20), fair (ICC 0.21–0.40), moderate (ICC 0.41–0.60), substantial (ICC 0.61–0.80), almost perfect (ICC 0.81–1.00). The standard error of measurement (SEM) and minimal detectable change at the 95% confidence level (MDC95) in seconds were also calculated for the 4mWT at all assessment time points.[32] Additionally, the 95% confidence intervals for ICC and SEM estimates were calculated.
Responsiveness was assessed by calculating standardized response means (SRMs) between consecutive assessment points for each of the tests. Calculations were arranged so that a decline in function across time points was represented as a negative SRM value. Bootstrapping was utilized to obtain sampling distributions of the SRMs for the purposes of estimating 95% confidence intervals.[33] Standardized response means were characterized using the following scale [34]: trivial (SRM 0–0.19), small (SRM 0.20–0.49), moderate (SRM 0.50–0.79), large (≥0.80).
To determine the construct validity between 4mW and 6MWT results, simple linear regression was performed at each time point separately with 6MWT as the dependent variable and 4mWT (usual or fastest) as the independent variable. Pearson correlation coefficients were characterized using the following scale[35]: negligible( r=0.0–0.3), low (r=0.3–0.5), moderate (r=0.5–0.7), high (r=0.7–0.9), very high (r=0.9–1.0). Additionally, the coefficient of determination was calculated (r2), along with 95% confidence intervals to inform comparisons between usual and fastest speeds for the 4mWT. All analyses were performed in R version 3.4.1 (The R Foundation for Statistical Computing).
RESULTS
Sample Description
One hundred sixty-two individuals (aged 63±7 years; 89 females) were available for this analysis. Baseline characteristics of patient groups are reported in table 1. Participant flow through the trial has been previously published.[29]
Table 1.
Baseline characteristics of study sample. Values are reported as mean ± standard deviation unless otherwise indicated.
| Characteristic | Study Sample (n=162) |
|---|---|
| Age, years | 63.5 ± 7.4 |
| BMI, kg/m 2 | 30.4 ± 4.8 |
| Sex, n (% female) | 89 (55) |
Outcome Measures
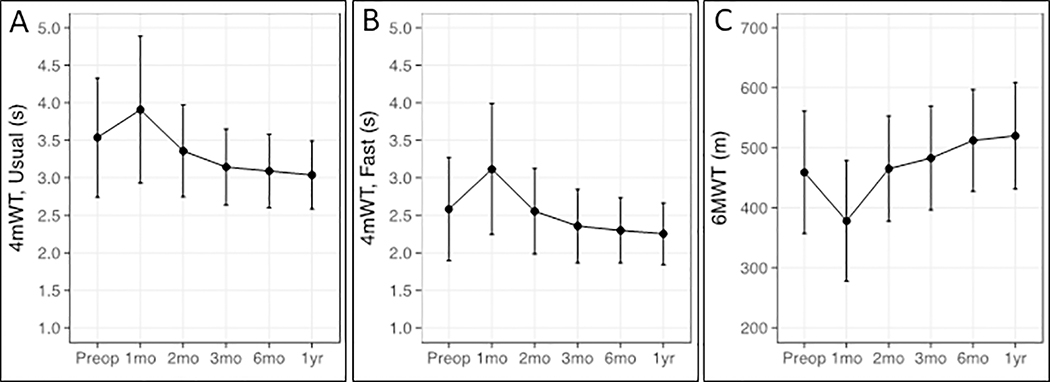
Figure 1 provides the measures of 4mWT (usual), 4mWT (fastest), and 6MWT distances across all time points. The first interval from pre-surgery to 1-month post-surgery showed decline in walking performance across all measures, followed by positive gains from 1 to 12 months.
Reliability
Test-retest reliability coefficients (ICCs), SEM’s, and MDC95’s for the 4mWT for all time points are presented in table 2. The test-retest reliability of 4mWT (usual) was substantial to almost perfect (ICC range: 0.79–0.87). Test-retest reliability for the 4mWT(fastest) was almost perfect at all time points (ICC range: 0.84–0.93). The SEM values for the 4mWT (usual) ranged from 0.20s to 0.35s with higher levels of measurement error found preoperatively and 1 month postoperatively compared to 4mWT (fastest). The SEM values for the 4mWT (fastest) ranged from 0.15s to 0.23s and were stable across all time points. Correspondingly, the MDC95’s for the 4mWT (fastest) were smaller than the 4mWT (usual) and ranged from 0.42s to 0.64s.
Table 2.
Estimates of reliability, Standard Error of the Measurement, and Minimal Detectable Change for 4-meter walk tests at each time point.
| Measure | 4mWT (usual) | 4mWT (fastest) | ||||
|---|---|---|---|---|---|---|
| ICC (95% CI) | SEM (95% CI) | MDC95 | ICC (95% CI) | SEM (95% CI) | MDC95 | |
| Pre-op (n=156) | 0.80 (0.74, 0.85) | 0.35 (0.30, 0.40) | 0.97 | 0.91 (0.88, 0.93) | 0.21 (0.18, 0.24) | 0.58 |
| 1 month (n=152) | 0.87 (0.83, 0.91) | 0.34 (0.30, 0.40) | 0.94 | 0.93 (0.91, 0.95) | 0.23 (0.19, 0.26) | 0.64 |
| 2 months (n=153) | 0.87 (0.83, 0.91) | 0.22 (0.19, 0.25) | 0.61 | 0.92 (0.89, 0.94) | 0.16 (0.14, 0.19) | 0.44 |
| 3 months (n=152) | 0.84 (0.79, 0.88) | 0.20 (0.17, 0.23) | 0.55 | 0.86 (0.82, 0.90) | 0.18 (0.16, 0.21) | 0.5 |
| 6 months (n=139) | 0.80 (0.74, 0.86) | 0.22 (0.19, 0.25) | 0.61 | 0.84 (0.78, 0.88) | 0.17 (0.15, 0.20) | 0.47 |
| 1 year (n=135) | 0.79 (0.72, 0.85) | 0.21 (0.18, 0.24) | 0.58 | 0.87 (0.82, 0.90) | 0.15 (0.13, 0.18) | 0.42 |
Responsiveness
The SRM’s for the 4mWT and 6MWT are presented in table 3. Responsiveness to deterioration in the first month postoperatively (indicated by a negative SRM value) was small for 4mWT (usual) and moderate for 4mWT (fastest) and 6MWT. Responsiveness from 1 to 2 months was moderate for the 4mWT (usual) and large for the 4mWT (fastest) and 6MWT. The 4mWT (usual and fastest) demonstrated better responsiveness than the 6MWT from 2 to 3 months postoperatively and was moderate for all three walking tests. Responsiveness for the 4mWT (usual and fastest) was trivial after 3 months but remained moderate for the 6MWT during the same time period.
Table 3.
Standardized Response Means (95% Confidence Interval) for the 4-meter Walk Tests (usual and fastest speeds) and 6-Minute Walk Test for each testing period.
| Measure | Pre-op to 1 mo | 1 mo to 2 mo | 2 mo to 3 mo | 3 mo to 6 mo | 6 mo to 1 yr |
|---|---|---|---|---|---|
| 4mWTa (usual) | −0.38 (−0.33, −0.44) | 0.76 (0.70, 0.82) | 0.59 (0.52, 0.65) | 0.13 (0.06, 0.20) | 0.14 (0.08, 0.21) |
| 4mWT (fastest) | −0.69 (−0.62, −0.76) | 0.91 (0.84, 0.99) | 0.65 (0.59, 0.70) | 0.12 (0.05, 0.19) | 0.17 (0.10, 0.24) |
| 6MWT b | −0.78 (−0.71, −0.84) | 1.08 (0.98 1.20) | 0.41 (0.34, 0.49) | 0.54 (0.48, 0.61) | 0.26 (0.19, 0.32) |
4mWT: 4-meter Walk Test
6MWT: 6-Minute Walk Test
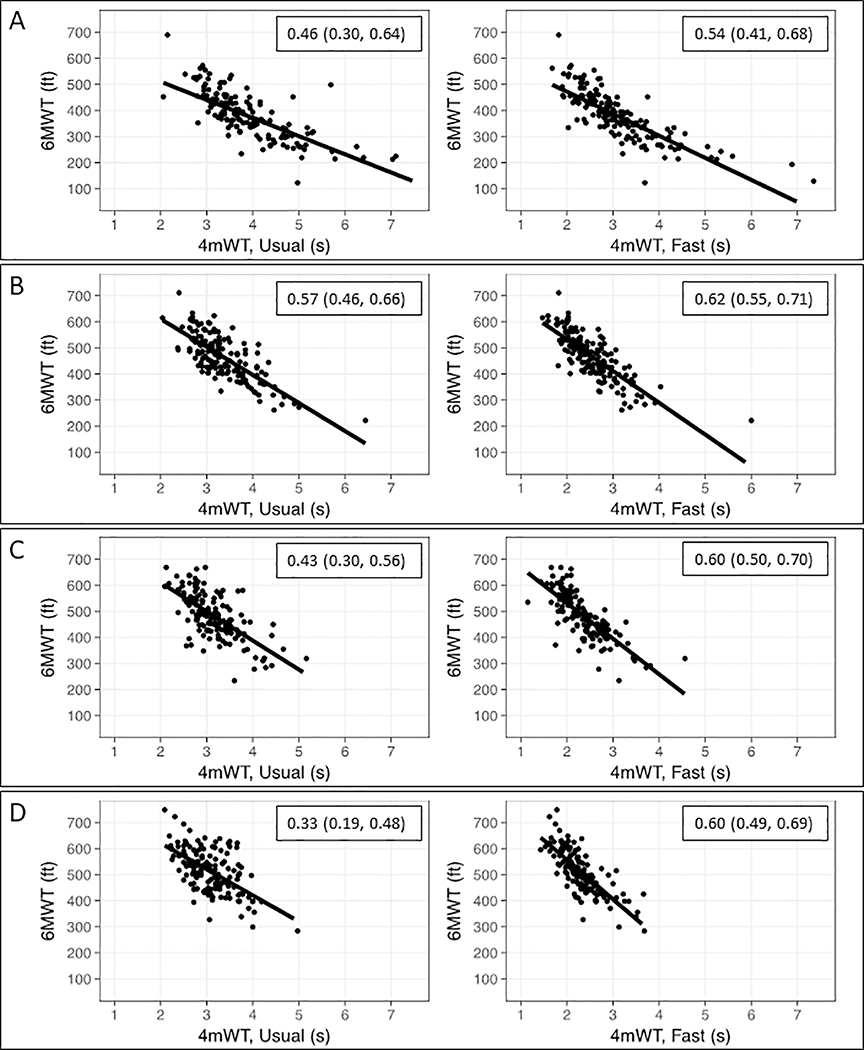
Construct Validity
The relationship between the 4mWT and 6MWT during the first three postoperative time points are displayed in figure 2 and Pearson correlations are reported in table 4 for all time points. The correlation between 4mWT (usual) and 6MWT was moderate and ranged from r=0.57 to r=0.75. The correlation between 4mWT (fastest) and 6MWT was high and ranged from 0.73 to 0.81. For the estimates of coefficient of determination, 95% confidence intervals overlapped at all time points except at six months following surgery, when 4mWT (fastest) explained a higher proportion of the variance observed in 6MWT results (r2 = 0.60, 95% CI: 0.50, 0.70), compared to the 4mWT (usual) (r2 = 0.33, 95% CI = 0.19, 0.48).
Figure 2.
Means (points) and standard deviations (error bars) of walking ability test results at all time points: A) 4mWT (usual speed), B) 4mWT (fast speed), and C) 6MWT distance.
Table 4.
Pearson correlation coefficients for the relationship between 4-meter walk test times and 6-minute walk test distance at each of the time points.
| Measure | Pre-op | 1 month | 2 months | 3 months | 6 months | 1 year |
|---|---|---|---|---|---|---|
| 4mWTa (usual) | 0.74 | 0.68 | 0.75 | 0.66 | 0.57 | 0.62 |
| 4mWT (fastest) | 0.81 | 0.73 | 0.79 | 0.77 | 0.77 | 0.77 |
4mWT: 4-meter Walk Test
DISCUSSION
The purpose of this study was to determine the reliability, responsiveness, and construct validity of the 4mWT compared to the 6MWT after TKA. We found that both versions of the 4mWT demonstrated nearly perfect reliability (ICC >0.80) across almost all time points. Our reliability findings are similar to those of Unver et al [28] which also found nearly perfect test-retest reliability (ICC=0.93) for the 4mWT (fastest) following TKA in an inpatient setting. Test-retest reliability was slightly lower at the preoperative time point for the 4mWT (usual) although still substantial. We also found that the MDC95 for the 4mWT (fastest) was more stable and indicated greater precision over the course of the study compared to 4mWT (usual). With MDC95 values ranging from 0.42 to 0.64 seconds, our results suggest much greater precision to the 4mWT (fastest) than was reported by Unver et al [28] (5.5s). However, Unver et al measured the 4mWT (fastest) immediately following surgery in the inpatient setting and the mean time to complete the 4mWT (fastest) was also much faster in our study (2.5s vs 17.6s). It is likely that precision of the test varies based on level of performance (i.e. very slow patients will demonstrate greater absolute error between assessments compared to very fast patients).
For responsiveness, our study found that the 4mWT (fastest) had superior responsiveness for detecting deterioration in the first postoperative month and recovery in the second postoperative month compared to the 4mWT (usual). Levels of responsiveness for the 4mWT (fastest) were similar to the 6MWT during the first two months. However, the 4mWT (fastest) demonstrated better responsiveness from 2 to 3 months postoperatively compared to the 6MWT, while the 6MWT demonstrated better responsiveness from 3 months to 1 year after surgery. This indicates that patients typically plateau in recovery of their walking speed by 3 months postoperatively and that the 6MWT shows less of a plateau in long-term recovery. Therefore, the 6MWT might be preferred for long-term tracking of walking ability. Conversely, the 4mWT (fastest) may be preferred during the initial postoperative period when many patients are undergoing rehabilitation. Parent and Moffet [22] compared the 10-meter walk test with the 6MWT and found the 6MWT had better responsiveness during the first two months after surgery, although the rehabilitation programs utilized in each study were different as were walking speed assessment methods (laboratory vs clinical) and these factors may have influenced responsiveness.[22] Kennedy et al [4] also examined the responsiveness of the 6MWT and reported higher levels of responsiveness than the current study (SRM=−1.74 for deterioration and 1.90 for improvement) although deterioration was measured at 8 days postoperatively versus the 1 month time point used in this study and improvement was measured from 8 days to 47 days postoperatively.[4] This highlights the need to standardize time points when comparing outcome measures as this may be a primary reason for observed differences between studies.
For construct validity, the 4mWT (fastest) demonstrated a stronger relationship to the 6MWT compared to the 4mWT (usual) and was highly correlated at all time points to the 6MWT. On average, 4mWT (fastest) explained 54–66% of the variability of performance on the 6MWT. These results are similar to prior studies in stroke[36] and spinal cord injury [37] which have found very high correlation (>0.90) between the 10-meter walk test and the 6MWT.
Study Limitations
A primary limitation in this study is the utilization of multiple raters over the course of the study and the lack of blinding of raters to performance on the 4mWT and 6MWT within a given testing session. While all raters underwent a standardized training procedure, this may have introduced potential error or bias into the study. Additionally, subjects in this study were participating in an interventional trial, which may have impacted responsiveness. The study sample likely consists of a more homogenous patient population than typically encountered in clinical practice. Future studies should examine the reliability and responsiveness of the 4mWT in a larger more heterogeneous patient population after TKA.
A further limitation to this study is the potential for familiarization by the participants to the 4mWT. However, test-retest reliability of the 4mWT has been demonstrated in studies that used sequential repetitions with short temporal spacing.[20,21,28] Further, the use of the 4mWT in our study is likely to represent how it will be utilized in clinical practice.
CONCLUSIONS
In conclusion, the 4mWT (fastest) has excellent test-retest reliability, shows high levels of responsiveness sufficient for clinical outcomes in the immediate postoperative time periods, and exhibits high construct validity with the 6MWT. Given the significant difference in space and time requirements to conduct each test, the 4mWT (fastest) may be preferred for routine clinical assessment. Additionally, given the superior reliability, responsiveness, and construct validity of the 4mWT (fastest) versus the 4mWT (usual), the 4mWT (fastest) is recommended over the 4mWT (usual).
Figure 3.
Relationship between 6MWT and 4mWT results at 4 postoperative time points: A) 1 month, B) 2 months, C) 3 months, and D) 6 months. Insets provide coefficients of determination with 95% confidence intervals.
Implications for Rehabilitation:
Walking Ability
Walking is an important functional ability for patients who undergo total knee arthroplasty (TKA).
While the Six-Minute Walk Test is a validated measure of walking ability in the TKA population, its clinical utility is limited by the space and time it takes to perform the test.
The Four-Meter Walk Test (fastest speed) is a valid, reliable, and responsive alternative to the 6MWT and is recommended for routine clinical use after TKA.
Acknowledgments
Funding: NIH R01-HD065900, NIH/NCATS UL1-TR001082, NIH T32 AG00279, and the Foundation for Physical Therapy Promotion of Doctoral Studies (PODS) I and II Scholarships
Footnotes
Author Disclosures
Conflict of interest: None of the authors have any conflicts of interest to report
Clinical Trial Registration: Clinicaltrials.gov NCT01537328
REFERENCES
- [1.].Fingar KR, Stocks C, Weiss AJ, et al. Most frequent operating room procedures performed in U.S. hospitals, 2003–2012. HCUP Statistical Brief. 2014. [cited 1-15 p.]. Goverment statistical brief available at [PubMed] [Google Scholar]
- [2.].Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007. Apr;89(4):780–5. [DOI] [PubMed] [Google Scholar]
- [3.].Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010. Sep;40(9):559–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4.].Kennedy DM, Stratford PW, Wessel J, et al. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC musculoskeletal disorders. 2005;6:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5.].Brach JS, VanSwearingen JM, Newman AB, et al. Identifying early decline of physical function in community-dwelling older women: performance-based and self-report measures. Physical therapy. 2002. Apr;82(4):320–8. [PubMed] [Google Scholar]
- [6.].Montero-Odasso M, Schapira M, Soriano ER, et al. Gait Velocity as a Single Predictor of Adverse Events in Healthy Seniors Aged 75 Years and Older. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2005;60(10):1304–1309. [DOI] [PubMed] [Google Scholar]
- [7.].Rabadi MH. Admission Ambulation Velocity Predicts Length of Stay and Discharge Disposition Following Stroke in an Acute Rehabilitation Hospital. 2005;19(1):20–26. [DOI] [PubMed] [Google Scholar]
- [8.].Hardy SE, Perera S, Roumani YF, et al. Improvement in Usual Gait Speed Predicts Better Survival in Older Adults. Journal of the American Geriatrics Society. 2007;55(11):1727–1734. [DOI] [PubMed] [Google Scholar]
- [9.].Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. 2005;42(4):535. [DOI] [PubMed] [Google Scholar]
- [10.].Maki BE. Gait Changes in Older Adults: Predictors of Falls or Indicators of Fear? Journal of the American Geriatrics Society. 1997;45(3):313–320. [DOI] [PubMed] [Google Scholar]
- [11.].Kuo HK, Liao KC, Leveille SG, et al. Relationship of Homocysteine Levels to Quadriceps Strength, Gait Speed, and Late-Life Disability in Older Adults. 2007;62(4):434–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12.].Penninx BWJH, Ferrucci L, Leveille SG, et al. Lower Extremity Performance in Nondisabled Older Persons as a Predictor of Subsequent Hospitalization. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2000;55(11):M691–M697. [DOI] [PubMed] [Google Scholar]
- [13.].Westby MD, Brittain A, Backman CL. Expert consensus on best practices for post-acute rehabilitation after total hip and knee arthroplasty: a Canada and United States Delphi study. Arthritis care & research. 2014. Mar;66(3):411–23. [DOI] [PubMed] [Google Scholar]
- [14.].Mizner RL, Petterson SC, Clements KE, et al. Measuring Functional Improvement After Total Knee Arthroplasty Requires Both Performance-Based and Patient-Report Assessments. The Journal of arthroplasty. 2011;26(5):728–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15.].Stevens-Lapsley JE, Schenkman ML, Dayton MR. Comparison of Self-Reported Knee Injury and Osteoarthritis Outcome Score to Performance Measures in Patients After Total Knee Arthroplasty. PM&R. 2011;3(6):541–549. [DOI] [PubMed] [Google Scholar]
- [16.].Naili JE, Iversen MD, Esbjornsson AC, et al. Deficits in functional performance and gait one year after total knee arthroplasty despite improved self-reported function. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2017. Nov;25(11):3378–3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17.].Terwee CB, Van Der Slikke RMA, Van Lummel RC, et al. Self-reported physical functioning was more influenced by pain than performance-based physical functioning in knee-osteoarthritis patients. Journal of Clinical Epidemiology. 2006;59(7):724–731. [DOI] [PubMed] [Google Scholar]
- [18.].Stratford PW, Kennedy DM, Woodhouse LJ. Performance measures provide assessments of pain and function in people with advanced osteoarthritis of the hip or knee. Physical therapy. 2006. Nov;86(11):1489–96. [DOI] [PubMed] [Google Scholar]
- [19.].Jacobs CA, Christensen CP. Correlations between knee society function scores and functional force measures. Clin Orthop Relat Res. 2009. Sep;467(9):2414–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20.].Butland RJ, Pang J, Gross ER, et al. Two-, six-, and 12-minute walking tests in respiratory disease. BMJ (Clinical research ed). 1982;284(6329):1607–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21.].Peters DM, Fritz SL, Krotish DE. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. 2013. Jan-Mar;36(1):24–30. [DOI] [PubMed] [Google Scholar]
- [22.].Parent E, Moffet H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Archives of Physical Medicine and Rehabilitation. 2002;83(1):70–80. [DOI] [PubMed] [Google Scholar]
- [23.].Dobson F, Hinman RS, Roos EM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis and cartilage. 2013;21(8):1042–1052. [DOI] [PubMed] [Google Scholar]
- [24.].Ko V, Naylor JM, Harris IA, et al. The six-minute walk test is an excellent predictor of functional ambulation after total knee arthroplasty. BMC Musculoskelet Disord. 2013. Apr 24;14:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25.].Kennedy DM, Stratford PW, Riddle DL, et al. Assessing recovery and establishing prognosis following total knee arthroplasty. Physical therapy. 2008. Jan;88(1):22–32. [DOI] [PubMed] [Google Scholar]
- [26.].Bennell K, Dobson F, Hinman R. Measures of physical performance assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task. Arthritis care & research. 2011;63(S11):S350–S370. [DOI] [PubMed] [Google Scholar]
- [27.].Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign”. J Geriatr Phys Ther. 2009;32(2):46–9. [PubMed] [Google Scholar]
- [28.].Unver B, Baris RH, Yuksel E, et al. Reliability of 4-meter and 10-meter walk tests after lower extremity surgery. Disabil Rehabil. 2017. Dec;39(25):2572–2576. [DOI] [PubMed] [Google Scholar]
- [29.].Bade MJ, Struessel T, Dayton M, et al. Early High-Intensity Versus Low-Intensity Rehabilitation After Total Knee Arthroplasty: A Randomized Controlled Trial. Arthritis care & research. 2017. Sep;69(9):1360–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30.].PE S, JL F. Intraclass correlation: Uses in assessing rater reliability.. Psychol Bull. 1979;86:420–8. [DOI] [PubMed] [Google Scholar]
- [31.].Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33(1):159. [PubMed] [Google Scholar]
- [32.].Stratford PW, Goldsmith CH. Use of the standard error as a reliability index of interest: an applied example using elbow flexor strength data. Physical therapy. 1997. Jul;77(7):745–50. [DOI] [PubMed] [Google Scholar]
- [33.].Efron B, Gong G. A leisurely look at the bootstrap, the jack-knife, and cross-validation. Am Stat. 1983;37:36–48. [Google Scholar]
- [34.].Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed ed. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- [35.].Hinkle D, Wiersma W, Jurs S. Applied Statistics for the Behavioral Sciences. 5th edition ed. Boston: Houghton Mifflin; 2002. 2002. [Google Scholar]
- [36.].Eng JJ, Chu KS, Dawson AS, et al. Functional Walk Tests in Individuals With Stroke: Relation to Perceived Exertion and Myocardial Exertion. 2002;33(3):756–761. [DOI] [PubMed] [Google Scholar]
- [37.].Van Hedel HJ, Wirz M, Dietz V. Assessing walking ability in subjects with spinal cord injury: Validity and reliability of 3 walking tests. Archives of Physical Medicine and Rehabilitation. 2005;86(2):190–196. [DOI] [PubMed] [Google Scholar]