Abstract
Background
Increasing the vertical dimension of occlusion (VDO) is a common procedure in complicated prosthodontic treatment. The swallowing technique had been verified as a functional method to determine the VDO. The purpose of this study was to investigate the association between increasing VDO and mandibular movement during swallowing.
Methods
26 females and 14 males were enrolled (age range: 21 to 30 year-old). Under different increased VDO (3, 5, and 8 mm), the mandibular trajectory during swallowing was measured by K7 Evaluation System (Myotronics®). When the subjects were instructed to salivary swallowing, the range of mandibular movement in vertical, anteroposterior and lateral directions were recorded.
Results
Increasing VDO significantly impacted the range of mandibular movement in lateral direction during swallowing (p < 0.0001, F value = 40.09). The average variance of the mandibular movement distance in lateral direction during swallowing raise 1.58 (p = 0.001); 3.59 (p = 0.0001) and 2.01 (p = 0.001) when th VDO was raised from 3 mm to 5 mm; from 3 mm to 8 mm and from 5 to 8 mm respectively. The range of mandibular movement was significantly correlated to the increasing VDO (p ≤ 0.05) under the analysis of the Post Hoc test.
Conclusions
VDO was closely correlated to the trajectory of mandibular motion during swallowing. The increase in VDO could change the extent of mandibular trajectory during swallowing if the increase was more than 3 mm. The range of mandibular motion when swallowing had positive correlative tendency as the VDO was increased.
Keywords: Vertical dimension of occlusion, Swallowing, Mandibular movement
Vertical dimension of occlusion (VDO) is defined as the distance between two selected anatomic points when the occluding members are in contact [1]. It is a controversial issue to determine the proper VDO for prosthodontic rehabilitation in dental clinic. Physiological VDO occurs at a range rather than a specific constant position. Some studies confirmed that the VDO is a highly adaptable position and the patients have ability to adapt after increasing the VDO without adverse consequences [2]. A variety of clinical methods had been developed to determine the acceptable VDO, including the use of vertical dimension of rest and freeway space [3], closest speaking space method [4], cephalometric radiographs [5], swallowing [6], pre-extraction records [7], facial analysis [8], and electromyography [9]. None of them has been shown to be scientifically more accurate than any other and each method has its own limitations [10]. Among these methods, the vertical dimension of rest is frequently used to determine the VDO in dental clinic. This method is derived from mandibular manipulation, a central-bearing-point device or graphic evaluation [11]. However, the age-related and facial changes usually interfere the measurements of VDO and physiologic factors also play influence on the valid of the result [12]. Although there is no exact perfect technique to ensure the accuracy of VDO, how to determine the VDO according to physiologic pattern to reduce the adapting time in clinic is an important issue.
Swallowing is one of the most important of biological functions. At the beginning of the swallowing cycle, mandible moves to the centric occlusion position, and the teeth come together with light contact [13]. According to previous study, the maxillomandibular relationship of VDO and centric relation can be determined based on repeated swallowing [6]. Other researches agreed the swallowing technique is a functional method of recording the VDO [14]. Therefore, the swallowing technique is recommended as a reliable method for establishing the VDO of edentulous patients [15]. The position of the mandible during swallowing does not seem to be a single position but rather an occlusal zone [14]. Gay et al. observed that the extent of mandibular trajectory in swallowing seems “float” within a relatively small vertical range [16].
Increasing the VDO is most common procedure in patients who need receive complicated prosthodontic treatment. Understanding the effects after increasing the VDO are prerequisites for many clinical situations. Although the swallowing technique had been verified as a functional method to determine the VDO, little information is related to the impact of increasing VDO on the mandibular trajectory during swallowing. The purpose of this study was to evaluate the impact of increasing the VDO on the swallowing pattern and we hope this study can provide clinician some physical viewpoints to increase the VDO.
Material and methods
Study subject
A total of 40 subjects, including 26 female and 14 male patients, was enrolled in this study. This study was approved by the Ethical Committee and Institutional Review Board of Chang Gung Memorial Hospital, Linkou, Taiwan (101–4900B), and all of the participants had signed the consent. The range of age was from 21 to 30 years (average, 26.3 year-old). The dental occlusion of this population invited in this study was restricted to Angle Class I. They did not have temporomandibular disorders, oral facial pain history and para-habitual functional problems such as clenching, bruxism, etc. All the subjects had full dentition, had no teeth attrition and no chewing or neuromuscular problems.
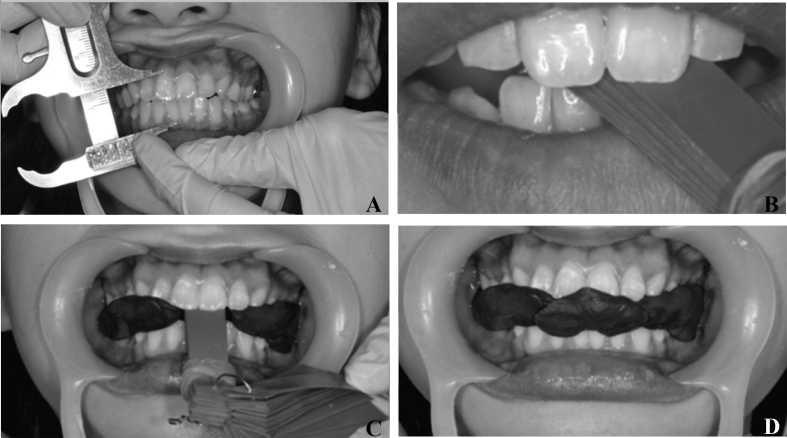
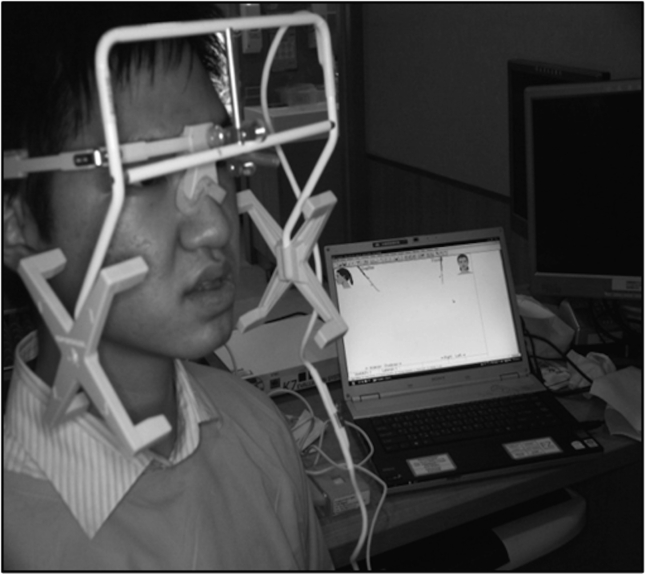
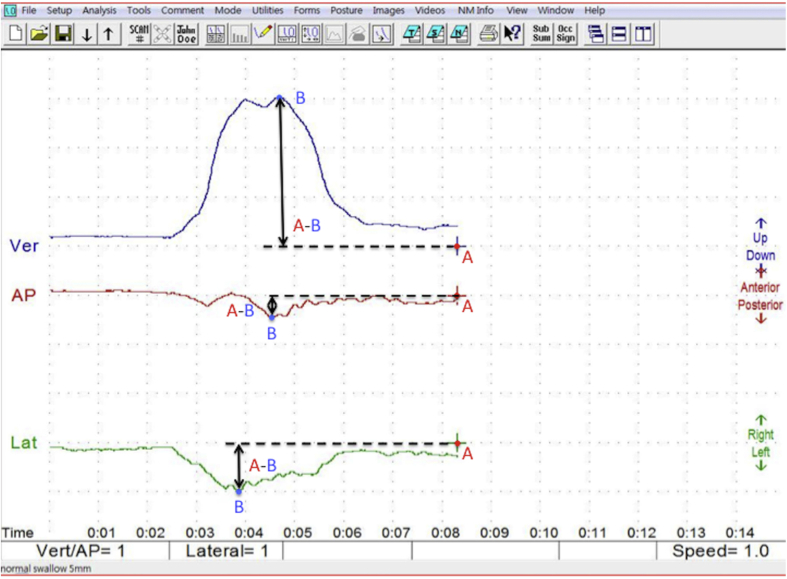
Before we started this study, all subjects must be ensured their VDO was not loss. This population was required that the distance from the center of the pupil of the eye to a line projected laterally from the lips median line was equal to the length from glabella to the subnasion in centric occlusion [17]. Those who suffered from VDO loss were excluded in this study. The distance between the zenith of the gingival contour of upper right central incisor and lower right central incisor was measured with millimeter in maximal intercuspation. The height of normal VDO was defined as the baseline (0 mm) in this study (Fig. 1A). The acrylic leaf gauge was put in the interocclusal space continuously to increase the VDO until the height was increased to 3 mm, 5 mm and 8 mm compared to baseline (Fig. 1B), then the dental impression brown compound (KERR@) was used to record the maxillao-mandibular relationship when the VDO was increased (Fig. 1C and D). Avoiding the compound was too big to interfere the normal swallowing pattern, it must be adjusted before the evaluation is started. We had ensured the deglutition function when the subjects worn the compound could not be affected. Multiple previous studies utilized the reliable K7 Evaluation System (Myotronics®) to monitor the jaw motion [[18], [19], [20]]. This equipment could accurately trace the mandibular trajectory in swallowing pattern. Initially, the magnet was attached on the lower incisal gingiva and the trajectory of mandibular motion was traced through the multiple sensor of this equipment. The measured mandibular trajectory was defined as the dynamic change of mandibular position in swallowing. It represented the range of jaw motion from static mandibular position. The subjects were instructed to voluntary swallow with saliva (Fig. 2) then recorded the range of mandibular movement in lateral, anteroposterior and vertical directions measured by the instrument in different VDO (Fig. 3). The cross mark indicated the mandibular position in centric relation and which was defined as the reference point (Fig. 3). To compare the farthest distance of mandibular movement in swallowing from the reference point was defined the variance in different vertical dimension of occlusion. The 0 mm VDO increased was regarded as comparison then placed the brown compound in the posterior interarch space to increase VDO 3 mm, 5 mm and 8 mm gradually.
Fig. 1.
Vertical dimension of occlusion (VDO) measurement. (A) The VDO was measured the distance between the zenith of the gingival contour of upper right central incisor and lower right central incisor in maximal intercuspation (B) Put the acrylic leaf gauge in the interocclusal space continuously to increase the VDO to 3 mm, 5 mm, and 8 mm (C) The dental impression brown compound was used to record the maxillao-mandibular relationship in the increasing VDO status (D) Fill the space of the acrylic leaf gauge with dental impression brown compound in the increasing VDO status.
Fig. 2.
K7 Evaluation System (Myotronics®). The instrument was applied to trace the trajectory of mandibular movement while a participant was instructed to salivary swallow in different increasing vertical dimension of occlusion.
Fig. 3.
Mandibular trajectory during swallowing. The range of mandibular movement in lateral, anteroposterior and vertical view were measured in different VDO with the K7 Evaluation System (Myotronics®). The cross mark indicated the mandibular position in centric relation and which was defined as the reference point (A). To compare the farthest distance of mandibular movement in swallowing (B) from the reference point was defined the variance (A–B) in different vertical dimension of occlusion.
Statistical analysis
The statistical power (G* Power) helps study design to decide the numbers of subjects. The variance analysis (ANOVA) was used as statistical analysis for repeated measures. Mean and standard deviation (SD) were shown in the range of mandibular movement in lateral direction, anteroposterior direction and vertical direction when swallowing. Post Hoc test was performed to compare two different VDO increased group in lateral direction. SPSS for Windows statistical software package version 19.0 was operated for these aforementioned analyses. Statistical significance was defined as p < 0.05.
Results
The results revealed increasing VDO significantly impacted the range of mandibular movement in lateral direction during swallowing (p < 0.0001, F value = 40.09) (Table 1). However, there was no significant difference in anteroposterior direction and vertical direction (p = 0.193 and 0.073). The lateral direction data were aimed to be further analyzed. To compare the change of mandibular trajectory in deglutition under difference between the baseline 0 mm and the three groups as increasing 3 mm, 5 mm, and 8 mm VDO by Post Hoc test (Table 2), the results showed that the average variance of the mandibular movement distance in lateral direction during swallowing raise 1.58 (p = 0.001) when the VDO was raised from 3 mm to 5 mm. The average variance of mandibular movement range during swallowing was significantly increased 3.59 (p < 0.0001) with the VDO raised from 3 mm to 8 mm. Compared to the 5 mm VDO condition, once the distance was increased to 8 mm the average variance changed 2.01 (p < 0.0001). There was no significant difference between the VDO in baseline 0 mm and in increasing of 3, 5, and 8 mm, the average variance changed 0.591 (p > 0.05), 0.397 (p > 0.05) and 0.351 (p > 0.05) respectively. There was significant difference between the lateral direction of mandibular movement range in swallowing pattern and the increasing VDO.
Table 1.
ANOVA for the different increasing vertical dimension to the range of mandibular movement in lateral direction during swallowing (n = 40).
| VDO | mean | SD | p-value |
|---|---|---|---|
| Lateral direction | 0.0001 | ||
| 0 mm | 1.03 | 0.45 | |
| 3 mm | 3.56 | 1.44 | |
| 5 mm | 5.14 | 1.82 | |
| 8 mm | 7.15 | 2.36 | |
| Anteroposterior direction | 0.193 | ||
| 0 mm | 0.29 | 0.15 | |
| 3 mm | 4.98 | 1.59 | |
| 5 mm | 4.32 | 1.47 | |
| 8 mm | 2.86 | 1.09 | |
| Vertical direction | 0.073 | ||
| 0 mm | 2.62 | 0.75 | |
| 3 mm | 7.31 | 2.38 | |
| 5 mm | 4.08 | 1.43 | |
| 8 mm | 4.05 | 1.34 |
Abbreviation: SD: standard deviation; VDO: vertical dimension of occlusion.
Table 2.
Post Hoc test was performed to compare the range of mandibular movement in lateral direction between two different VDO increased groups (n = 40).
| (I) VDO | (J) VDO | average variance (I-J) | p-value | 95% confidence interval |
|
|---|---|---|---|---|---|
| Lower | Upper | ||||
| 3 mm | 0 mm | 0.591 | 0.566 | −0.63 | 1.812 |
| 5 mm | −1.58* | 0.001 | −2.578 | −0.586 | |
| 8 mm | −3.59* | 0.0001 | −4.589 | −2.597 | |
| 5 mm | 0 mm | 0.397 | 0.818 | −0.824 | 1.617 |
| 3 mm | 1.58* | 0.001 | 0.586 | 2.578 | |
| 8 mm | −2.01* | 0.0001 | −3.007 | −1.015 | |
| 8 mm | 0 mm | 0.351 | 0.865 | −0.87 | 1.572 |
| 3 mm | 3.59* | 0.0001 | 2.597 | 4.589 | |
| 5 mm | 2.01* | 0.0001 | 1.015 | 3.00 | |
*p < 0.05.; Abbreviation: VDO: vertical dimension of occlusion.
Discussion
The increasing VDO is a frequent modality to facilitate dental treatment, but the technique is still considerable debate. Although the implication of increasing VDO is still a controversial issue based on evidence, it is meaningful in rehabilitative procedure. More consistent and reliable determination to increase VDO is worthy to be investigated. This was the precursor research to investigate VDO change from physical perspective. The freeway space in neutral dentition is 2–4 mm [3], so the increase of 3 mm VDO was considered to be physiological compatible. In 2012, Abduo and Lyons indicated the 5 mm maximum increase in VDO is safe and acceptable due to the predictable patient adaptation [21]. Hence, in this study the 5 mm increased VDO was defined as physiological limit. In this study we tried to investigate whether the VDO increased over physical adaptation significantly impact on the swallowing pattern so we designed the 8 mm increased VDO.
The mean frequency of spontaneous swallowing is 1.32 cycle/minute [22], so deglutition is the most frequent physical action every day. However, less literature investigated the jaw motion in deglutition. The reason might be contributed to the narrow range of mandibular movement is hard to be detected during swallowing. Moreover, Gross et al. reported that there was no significant extraoral improvement of facial tissues appearance after increase of the VDO by 2–6 mm for dentate individuals [23] and the extent of mandibular movements were within a very small vertical range [16]. Hence, the study utilized the changed distance of gingival zenith of upper and central incisor to define the increased VDO. The K7 Evaluation System (Morita®) utilized in this study supplies useful supports in the diagnosis of body dysfunctions and are now being applied to dental clinical practice [24]. That allows dynamic investigation of mandibular movements in three dimensions during different physiologic activities such as swallowing. The magnetic induction of this equipment could more precisely detect the jaw motion and we had also increased the sensitivity of the instrument to enlarge the difference of trajectory. Based on the viewpoint verified in the previous research [16], we calculate the distance of jaw motion in the lateral direction because the difference is more obvious even if the mandibular trajectory in lateral, anteroposterior and vertical directions all had been measured. The study design might overcome many errors derived from subjective measurement in previous research and increased the realism and validity.
Some investigations indicated increasing VDO may disturb the dental physiology and masticatory mechanisms [25]. However, the result revealed the swallowing pattern could not be significantly violated if increasing VDO less than 3 mm and it was coincident to the previous study [26]. But when the VDO increased over 3 mm, the mandibular movement in deglutition revealed significant differences. This result was coincident to the consensus proposed in 1994 [16]. They put a 12 mm plastic bite block between the molars to increase VDO then found the movement trajectories of the oral structures were highly variable, both within and among different individuals, during swallowing. In our study the compound filling the interdental space derived from the increasing VDO could simulate the real swallowing status and that design also reduced the interference the tongue thrusting in deglutition pattern. One of the preliminary finding in this research indicated the close association with increasing VDO and the range of mandibular movement during swallowing in lateral direction (Table 1).
Clinically, an increase in VDO should consider the remaining tooth structure, the space available for the restoration, occlusal variables and aesthetics. Many articles approved the feasibility of increasing VDO [21], but the modality used to increase the VDO in clinic lack consistency and reliability until now [25]. Generally, the magnitude of increasing the VDO for dentate individuals is limited to 5 mm inter-incisally [26]. In the physical aspect, the study indicated the significant difference of mandibular movement range during swallowing once the VDO had been increased over 3 mm. This result was coincident to the statement proposed in 1984, the increasing VDO might interfere the masticatory function or oral physiology [27]. Based on this result the impact of VDO change on the pattern of jaw motion in deglutition should be worthy of attention if the increasing VDO is considered in clinic. In addition, this result also showed to sum up the variance about the range of mandibular movement derived from the VDO increased from 3 mm to 5 mm and 5 mm–8 mm was equal to the result of VDO from 3 mm to 8 mm. The clinical significance provided from this outcome was the increase of VDO and the mandibular trajectory during swallowing seemed had positive correlative tendency. The physical impact in deglutition caused by direct change VDO from 3 mm to 5 mm might be similar to result of the gradual increasing VDO as the VDO was raised from 3 mm to 5 mm first then increased from 5 mm to 8 mm later. This consensus was similar to some author advocated the gradual increasing the VDO in clinic is recommended because the minimal change of VDO can be justified by physical adaptation [28]. Furthermore, to find the physical tolerance of maximal VDO might be further explored in another study.
Although this result provided multiple precursor findings, there was still some limitation in the present study. From the available studies, most of the negative consequences of symptoms and signs followed on increasing VDO resolved within two weeks [21]. The increasing VDO from 3 to 5, 5 to 8 and 3–8 mm resulted in significant changes in the trajectory of the mandibular movement during swallowing. However, the control group (0 mm increased in VDO) had no significant different from 3, 5, and 8 mm increase in VDO (Table 2). This reason we inferred that the study increased the VDO of each subject in a short time then measured the data continuously and the influence of physical adaptation was not considered in this study. Whether the physical adaption makes the no significance of increment compared to baseline is worthy to further investigate. Hence, all subjects should be measured the mandibular trajectory during swallowing again after the data of the VDO increment had been recorded based on physical adaptation consideration. It might affect the result compared between 0 mm and 3 mm, 0 mm and 5 mm, 0 mm and 8 mm. Hope the limitation of this research can be overcome in the future. It is necessary to provide more understanding of the long-term effect on mandibular movement of changing the VDO in the future. Besides, the age of samples ranged from 20 to 30 years might not represent the typical patients who need receive prosthodontics rehabilitation and their neuromuscular function is healthy to adapt the VDO change easily. All participants in this study were absence of any VDO loss, and patients who suffered from extensive loss of tooth structure may behave differently. Furthermore, the increased VDO defined as the change of gingival zenith between upper and lower central incisor. The mandibular midline shift might interfere the VDO measurement but the interference had not been considered in the study design. Hope these aforementioned limitations can be resolved in future investigations. How to increase the realism of modality to change the VDO is a valuable issue in dental clinic. To investigate the topic from other physiological perspective is the direction in further research.
Conclusions
The increased VDO plays a significant role on the mandibular movement in deglutition. The increase in VDO could change the extent of mandibular trajectory during swallowing if the increase is more than 3 mm. The range of mandibular motion while swallowing has positive correlative tendency as the VDO increased.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgement
This study is supported by Chang Gung Memorial Hospital, Linkou (CMRPG3C1791 and CMRPG3H0371).
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.The glossary of prosthodontic terms. J Prosthet Dent. 2005;94:10–92. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Ormianer Z., Gross M. A 2-year follow-up of mandibular posture following an increase in occlusal vertical dimension beyond the clinical rest position with fixed restorations. J Oral Rehabil. 1998;25:877–883. doi: 10.1046/j.1365-2842.1998.00326.x. [DOI] [PubMed] [Google Scholar]
- 3.Pleasure M.A. Correct vertical dimension and freeway space. J Am Dent Assoc. 1951;43:160–163. doi: 10.14219/jada.archive.1951.0188. [DOI] [PubMed] [Google Scholar]
- 4.Silverman M.M. The speaking method in measuring vertical dimension. J Prosthet Dent. 1952;85:427–431. doi: 10.1067/mpr.2001.116139. [DOI] [PubMed] [Google Scholar]
- 5.Pyott J.E., Schaeffer A. Centric relation and vertical dimension by cephalometric roentgenograms. J Prosthet Dent. 1954;4:35–41. [Google Scholar]
- 6.Shanahan T.E. Physiologic jaw relations and occlusion of complete dentures. J Prosthet Dent. 1955;91:203–205. doi: 10.1016/j.prosdent.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Turner L.C. The profile tracer: method for obtaining accurate pre-extraction records. J Prosthet Dent. 1969;21:364–370. doi: 10.1016/0022-3913(69)90044-4. [DOI] [PubMed] [Google Scholar]
- 8.Fayz F., Eslami A. Determination of occlusal vertical dimension: a literature review. J Prosthet Dent. 1988;59:321–323. doi: 10.1016/0022-3913(88)90182-5. [DOI] [PubMed] [Google Scholar]
- 9.Shpuntoff H., Shpuntoff W. A study of physiologic rest position and centric position by electromyography. J Prosthet Dent. 1956;6:621–628. [Google Scholar]
- 10.Rivera-Morales W.C., Mohl N.D. Relationship of occlusal vertical dimension to the health of the masticatory system. J Prosthet Dent. 1991;65:547–553. doi: 10.1016/0022-3913(91)90298-b. [DOI] [PubMed] [Google Scholar]
- 11.Myers M., Dziejma R., Goldberg J., Ross R., Sharry J. Relation of Gothic arch apex to dentist-assisted centric relation. J Prosthet Dent. 1980;44:78–81. doi: 10.1016/0022-3913(80)90052-9. [DOI] [PubMed] [Google Scholar]
- 12.Koller M.M., Merlini L., Spandre G., Palla S. A comparative study of two methods for the orientation of the occlusal plane and the determination of the vertical dimension of occlusion in edentulous patients. J Oral Rehabil. 1992;19:413–425. doi: 10.1111/j.1365-2842.1992.tb01583.x. [DOI] [PubMed] [Google Scholar]
- 13.Thexton A.J. Mastication and swallowing: an overview. Br Dent J. 1992;173:197–206. doi: 10.1038/sj.bdj.4808002. [DOI] [PubMed] [Google Scholar]
- 14.Millet C., Jeannin C., Vincent B., Malquarti G. Report on the determination of occlusal vertical dimension and centric relation using swallowing in edentulous patients. J Oral Rehabil. 2003;30:1118–1122. doi: 10.1046/j.1365-2842.2003.01201.x. [DOI] [PubMed] [Google Scholar]
- 15.Ismail Y.H., George W.A. The consistency of the swallowing technique in determining occlusal vertical relation in edentulous patients. J Prosthet Dent. 1968;19:230–236. doi: 10.1016/0022-3913(68)90083-8. [DOI] [PubMed] [Google Scholar]
- 16.Gay T., Rendell J.K., Spiro J., Mosier K., Lurie A.G. Coordination of oral cavity and laryngeal movements during swallowing. J Appl Physiol. 1994;77:357–365. doi: 10.1152/jappl.1994.77.1.357. [DOI] [PubMed] [Google Scholar]
- 17.Mc G.G. Use of facial measurements in determining vertical dimension. J Am Dent Assoc. 1947;35:342–350. doi: 10.14219/jada.archive.1947.0361. [DOI] [PubMed] [Google Scholar]
- 18.Ferrario V.F., Sforza C., Miani A., Serrao G. Kinesiographic three-dimensional evaluation of mandibular border movements: a statistical study in a normal young nonpatient group. J Prosthet Dent. 1992;68:672–676. doi: 10.1016/0022-3913(92)90385-n. [DOI] [PubMed] [Google Scholar]
- 19.Ferrario V.F., Sforza C., Sigurta D., Dalloca L.L. Temporomandibular joint dysfunction and flat lateral guidances: a clinical association. J Prosthet Dent. 1996;75:534–539. doi: 10.1016/s0022-3913(96)90459-x. [DOI] [PubMed] [Google Scholar]
- 20.Lopez-Cedrun J., Santana-Mora U., Pombo M., Perez Del Palomar A., Alonso De la Pena V., Mora M.J. Jaw biodynamic data for 24 patients with chronic unilateral temporomandibular disorder. Scientific data. 2017;4:170168. doi: 10.1038/sdata.2017.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abduo J., Lyons K. Clinical considerations for increasing occlusal vertical dimension: a review. Aust Dent J. 2012;57:2–10. doi: 10.1111/j.1834-7819.2011.01640.x. [DOI] [PubMed] [Google Scholar]
- 22.Afkari S. Measuring frequency of spontaneous swallowing. Australas Phys Eng Sci Med. 2007;30:313–317. [PubMed] [Google Scholar]
- 23.Gross M.D., Nissan J., Ormianer Z., Dvori S., Shifman A. The effect of increasing occlusal vertical dimension on face height. Int J Prosthodont (IJP) 2002;15:353–357. [PubMed] [Google Scholar]
- 24.Ferrario V.F., Sforza C., Miani A., D'Addona A., Tartaglia G. Statistical evaluation of some mandibular reference positions in normal young people. Int J Prosthodont (IJP) 1992;5:158–165. [PubMed] [Google Scholar]
- 25.Tench R.W. Dangers in dental reconstruction in-volving increase of the vertical dimension of the lower third of the human face. The Journal of the American Dental Association and The Dental Cosmos. 1938;25:566–570. [Google Scholar]
- 26.Dahl B.L., Krogstad O. Long-term observations of an increased occlusal face height obtained by a combined orthodontic/prosthetic approach. J Oral Rehabil. 1985;12:173–176. doi: 10.1111/j.1365-2842.1985.tb00632.x. [DOI] [PubMed] [Google Scholar]
- 27.Turner K.A., Missirlian D.M. Restoration of the extremely worn dentition. J Prosthet Dent. 1984;52:467–474. doi: 10.1016/0022-3913(84)90326-3. [DOI] [PubMed] [Google Scholar]
- 28.Schuyler C.H. Problems associated with opening the bite which would contraindicate it as a common procedure. J Am Dent Assoc. 1939;26:734–740. [Google Scholar]