Abstract
Background
The outcomes and complication rates of patients with isolated greater tuberosity fractures are not well documented. The present study aimed to evaluate the reoperation rates, types of reoperations, and complications for patients undergoing open reduction internal fixation and those undergoing initial nonoperative treatment of isolated greater tuberosity fractures.
Methods
An administrative claims database was queried from 2010 to 2018 for adult patients treated with open reduction internal fixation or initial nonoperative treatment within 6 weeks of sustaining a closed isolated greater tuberosity fracture. Reoperation rates, types of reoperations, local/surgical complications, and systemic complications for two cohorts were collected, and statistical analysis was performed using R statistical software for patients initially treated operatively and nonoperatively. Complication rates were compared using multivariate logistic regression, while demographic data were compared using chi-square analysis.
Results
Of the 8509 patients who were documented to have sustained a closed isolated greater tuberosity fracture, 333 patients underwent operative treatment and 8176 patients received initial nonoperative treatment within the first 6 weeks of diagnosis. The operative cohort had a reoperation rate of 2.7% at 90 days, 5.7% at 6 months, and 7.8% at 1 year, with the majority of reoperations being rotator cuff repair (40.6%). Within the initial nonoperative cohort, 7.3% had an operation within a year, with the majority of operations being open reduction internal fixation (41.3%). The subsequent reoperation rate for those patients was 3.5% at 2 years with the majority of reoperations being rotator cuff repair (32.4%). In the operative cohort, the 90-day infection rate was 3.0%. Nonunion was demonstrated in the operative cohort at a rate of 1.8% at 6 months and 2.7% at 1 year.
Conclusion
When surgical care was provided to patients sustaining isolated greater tuberosity fractures in the first 6 weeks, there was a 7.8% rate of reoperation within the first year. Patients initially treated nonoperatively had a future operation rate of 7.3% within the first year and a 3.5% reoperation rate within the second year. The most common reoperation regardless of initial treatment was rotator cuff repair. With an elevated rate of subsequent operations, education is paramount to provide patients with expectations for the sequelae of this injury especially when presenting with concomitant injuries.
Keywords: Isolated greater tuberosity fracture, Reoperation rates, Reoperation types, Operative treatment, Nonoperative treatment, Local complications, Systemic complications
With its superior aspect located 6-8 mm inferior to the most superior aspect of the humeral head articular surface, the greater tuberosity provides structural integrity to the shoulder as an attachment point for the rotator cuff.6,11 As a consequence of impaction, shearing, or avulsion forces, even slight anatomic aberrations to the greater tuberosity from fractures can alter shoulder dynamics and stability.7,9 Greater tuberosity fractures can occur as an isolated entity and may present with concomitant injuries such as anterior shoulder dislocation, rotator cuff injury, shoulder instability, and/or with complex fracture patterns.12,16,18,20 Isolated greater tuberosity fractures account for 2%-20% of all proximal humerus fractures with varying surgical treatments available.14,22,24
Current surgical options for isolated greater tuberosity fractures include fragment excision, open reduction and internal fixation (ORIF), closed reduction and percutaneous fixation, and arthroscopically assisted reduction with fixation.6,12 When indicated, fixation is achieved with the aforementioned techniques using a combination of screws with or without washers, pins, plates, heavy sutures, or suture anchors.6 Although outcomes are variable with satisfactory results for arthroscopic fixation as well as ORIF, there is still a potential for complications resulting in reoperations.9,13 When comparing arthroscopic double-row suture anchor fixation to ORIF with plate fixation for displaced isolated greater tuberosity fractures, Liao et al13 noted 3 of 23 patients, all from the ORIF cohort, underwent a reoperation owing to secondary subacromial impingement and postoperative stiffness. Although studying more complex and comminuted isolated greater tuberosity fractures, Bhatia et al4 documented 3 of 21 patients, all of whom received ORIF with double-row suture anchors, required a reoperation for bicipital tendonitis from fracture fragment impingement on the biceps tendon or osteonecrosis of the greater tuberosity. Finally, in a systematic review comparing nonoperative with operative management of isolated greater tuberosity fractures, Levy et al12 reported 8 of 429 patients, all of whom were treated operatively, received a reoperation most commonly for postoperative stiffness, followed by heterotopic ossification, transient neurapraxias, and superficial infection.
The threshold for surgical intervention of isolated greater tuberosity fractures is currently debated as surgery is performed on this fracture at variable displacement lengths. While the decision for surgery of this fracture is dependent on patient factors such as age, activity level, and comorbidities, several studies recommend surgical treatment for superior fracture displacement greater than 5 mm in the general active population or in patients with impingement.6,9,21 Other studies suggest that fracture displacement as low as 3 mm should be treated surgically for optimal outcomes especially in athletes or overhead workers.12 When initially treated nonoperatively for greater tuberosity fractures with a primary displacement greater than 3 mm, Schliemann et al22 demonstrated all patient eventually required revision surgery owing to secondary displacement of the fracture fragment.
There is a paucity of literature in the comprehensive assessment of subsequent operations and outcomes of patients sustaining an isolated greater tuberosity fracture. The present study aimed to evaluate the reoperation rates, types of reoperations, and complications for patients undergoing open reduction internal fixation and those undergoing initial nonoperative treatment of isolated greater tuberosity fractures. To determine this difference with an adequately powered study, a large national database was used to detect significant changes.
Materials and methods
A retrospective review of deidentified patient records was conducted using the PearlDiver database (PearlDiver, Inc, Fort Wayne, IN, USA), a large nationwide administrative claims database. This study used the Mariner data set, which contains approximately 122 million patients from various provider groups in the United States. Patient cohorts, procedures, demographic information, prescription information, comorbidities, and other clinical data are available in the database and can be obtained using Current Procedural Technology (CPT) and International Classification of Diseases (ICD), ninth revision and tenth revision (ICD-9/ICD-10) codes. Institutional review board exemption was granted for this study as the provided data were deidentified and compliant with the Health Insurance Portability and Accountability Act.
Patients identified with a closed isolated greater tuberosity fractures were included in the analysis. Patients with a prior history of autoimmune disease, fractures related to a neoplastic process, osteoporosis secondary to cancer, vitamin abnormalities, malignancy, or open fractures during the time of injury were excluded from the analysis. Patients older than the age of 18 years with a greater tuberosity fracture diagnosis required a minimum of 1-year follow-up from 2010 to 2018 Q2 to be included in this study.
Patients with isolated greater tuberosity fractures were subdivided into two groups: patients who received ORIF during the first 6 weeks after fracture diagnosis (CPT 23630) or no operative intervention in the first 6 weeks after fracture diagnosis to best represent the initial operative and nonoperative fracture treatment cohorts. The full list of criteria used to define each cohort and all inclusion/exclusion criteria can be found in Supplementary Table S1.
Demographic data and preexisting clinical characteristics were queried directly from the database and included age, gender, body mass index, geographic region, Charlson comorbidity index (CCI), and major comorbidities (tobacco use, liver disease, cardiac history, alcohol use, preexisting anemia, chronic obstructive pulmonary disease, chronic kidney disease, congestive heart failure, immunodeficiency, depression).
Incidence of local/surgical complications was evaluated for both cohorts at 90 days, 6 months, and 1 year postoperatively. These complications included a subsequent operation, nerve injury, nonunion, adhesive capsulitis, avascular necrosis, and infection. The types of initial operations for the nonoperative cohort after 6 weeks of nonoperative treatment in addition to the types of reoperations for both cohorts were obtained using a combination of ICD and CPT procedural codes to examine the most common surgical interventions performed. For example, CPT codes 23410, 23412, 29827, ICD9-P-8363, ICD10-P-0LQ10ZZ, ICD10-P-0LQ14ZZ, ICD10-P-0LQ20ZZ, and ICD10-P-0LQ24ZZ were used to query for rotator cuff repair (RCR). In a similar manner, ICD codes were used to query for nerve injuries of the upper arm and shoulder. Infection was defined by a combination of diagnosis and procedural codes that indicated surgical intervention for a deep infection and excluded superficial wound complications that would not necessitate surgical intervention. Incidences of systemic complications were evaluated in the acute 90-day postfracture period. Systemic complications queried included cerebrovascular accidents, pneumonia, pulmonary embolism, myocardial infarction, acute renal failure, deep venous thrombosis, anemia, respiratory failure, urinary tract infection, and altered mental status. The codes used to define local/surgical complications are available in Supplementary Table S2 and systemic complications are available in Supplementary Table S3.
Statistical analysis was performed using R statistical software (R Project for Statistical Computing, Vienna, Austria) integrated with the PearlDiver software with an α level set to 0.05. Demographic and clinical characteristics of both cohorts were compared using chi-square analysis with Yate's correction for categorical variables and Welch's t-test for continuous variables. Multivariate logistic regression was used to calculate odds ratios and statistical significance for local and systemic complications after adjusting for demographics such as patient age, sex, CCI, body mass index, diabetes status, and tobacco use.
Results
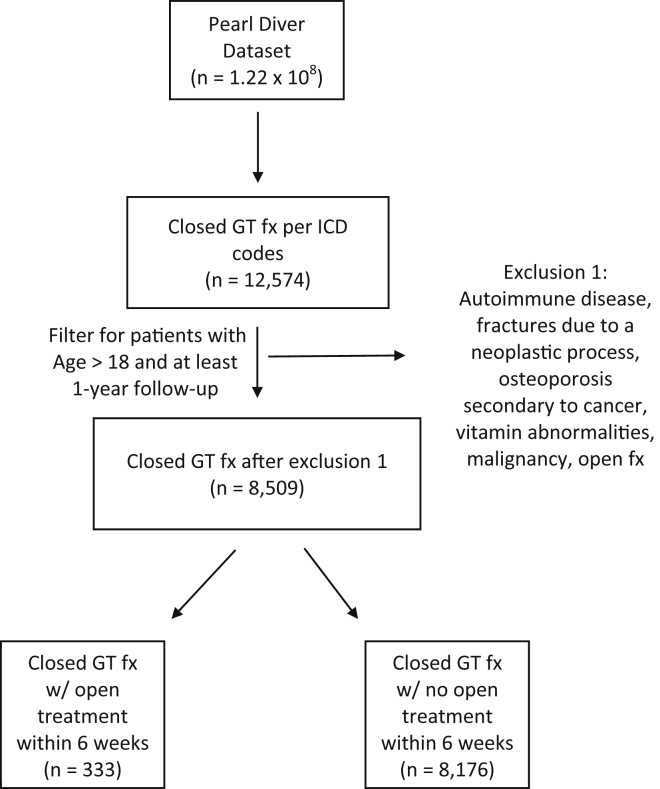
A total of 12,574 patients sustaining an isolated greater tuberosity fracture were queried from the PearlDiver database using ICD-9 and ICD-10 codes. After adjusting for exclusion criteria, filtering for patients with a 1-year follow-up, and removing duplicates, this number decreased to 8509. Of this total, 333 (3.9%) patients had ORIF and 8176 (96.1%) patients had nonoperative treatment within 6 weeks of diagnosis (Fig. 1).
Figure 1.
Flow diagram of patients included in study. Fx, fracture; GT, greater tuberosity.
A significantly greater proportion of patients treated with initial operative fixation for an isolated greater tuberosity fracture were men (men: 33.0% vs. 23.0%, P = .002) and had a preexisting history of alcohol use (alcohol use: 9.9% vs. 6.7%, P = .048). The operative group also had a significantly lower CCI (CCI: 1.11 vs. 1.44, P < .001). The nonoperative group had significantly older patients (mean age: 62.1 vs. 58.2, P < .001) and included more patients with a preexisting history of congestive heart failure (congestive heart failure: 8.2% vs. 3.9%, P = .011). All other demographic data between the operative and nonoperative cohorts were statistically insignificant and comparable (Table I).
Table I.
Demographic and clinical characteristics of patients with operative fixation vs. nonoperative care within 6 weeks of sustaining a closed isolated greater tuberosity fracture.
| Comparison of demographic and clinical characteristics | |||
|---|---|---|---|
| Operative (n = 333) | Nonoperative (n = 8176) | P value | |
| Age (%) | |||
| 19-64 | 200 (60.1) | 4112 (50.3) | .058 |
| 64-79 | 133 (39.9) | 4064 (49.7) | .040 |
| 80+ | 0 | 0 | N/A |
| Mean ± SD | 58.2 ± 14.1 | 62.1 ± 13.0 | <.001 |
| Gender (%) | |||
| Male | 110 (33.0) | 1883 (23.0) | .002 |
| Female | 223 (67.0) | 6293 (77.0) | .124 |
| BMI (%)∗ | |||
| Less than 30 | 0 (0) | 18 (0.2) | N/A |
| 30-40 | 2 (0.6) | 29 (0.4) | .796 |
| Greater than 40 | 5 (1.5) | 43 (0.5) | .735 |
| Region of the United States (%) | |||
| South | 129 (38.7) | 3198 (39.1) | .956 |
| Midwest | 93 (27.9) | 1932 (23.6) | .188 |
| Northeast | 57 (17.1) | 1806 (22.1) | .089 |
| West | 54 (16.2) | 1226 (15.0) | .664 |
| CCI ± SD | 1.11 ± 1.81 | 1.44 ± 2.23 | <.001 |
| Major comorbidities (%) | |||
| Tobacco | 65 (19.5) | 1586 (19.4) | .981 |
| Liver disease | 29 (8.7) | 675 (8.3) | .866 |
| Cardiac | 44 (13.2) | 1492 (18.2) | .055 |
| ETOH | 33 (9.9) | 549 (6.7) | .048 |
| Anemia | 55 (16.5) | 1684 (20.6) | .154 |
| COPD | 78 (23.4) | 1977 (24.2) | .854 |
| CKD | 24 (7.2) | 731 (8.9) | .365 |
| CHF | 13 (3.9) | 671 (8.2) | .011 |
| Immunodeficiency | 7 (2.1) | 229 (2.8) | .567 |
| Depression | 85 (25.5) | 1946 (23.8) | .617 |
BMI, body mass index; CCI, Charlson comorbidity index; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; ETOH, alcohol use; RA, rheumatoid arthritis; SD, standard deviation.
BMI was only able to be calculated on 2.1% of operative group and 1.1% of nonoperative group
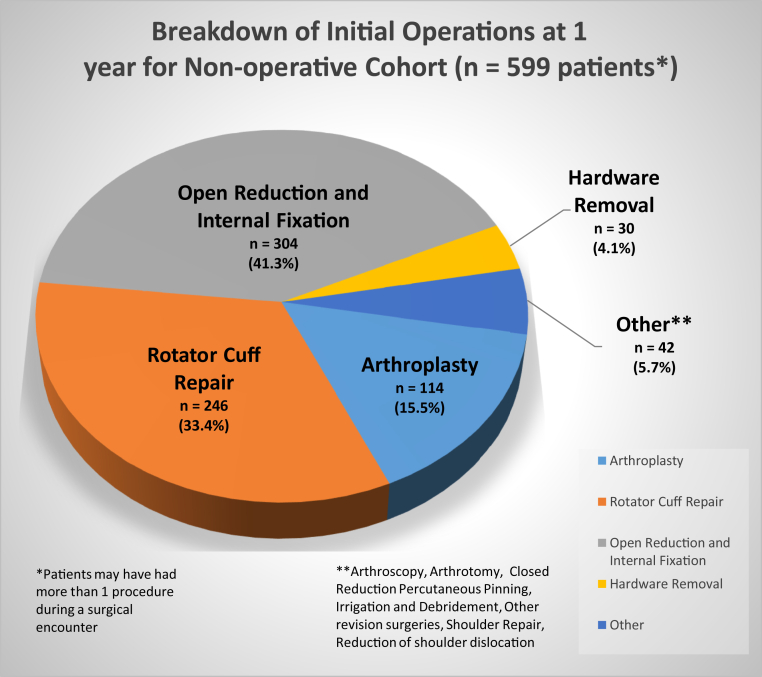
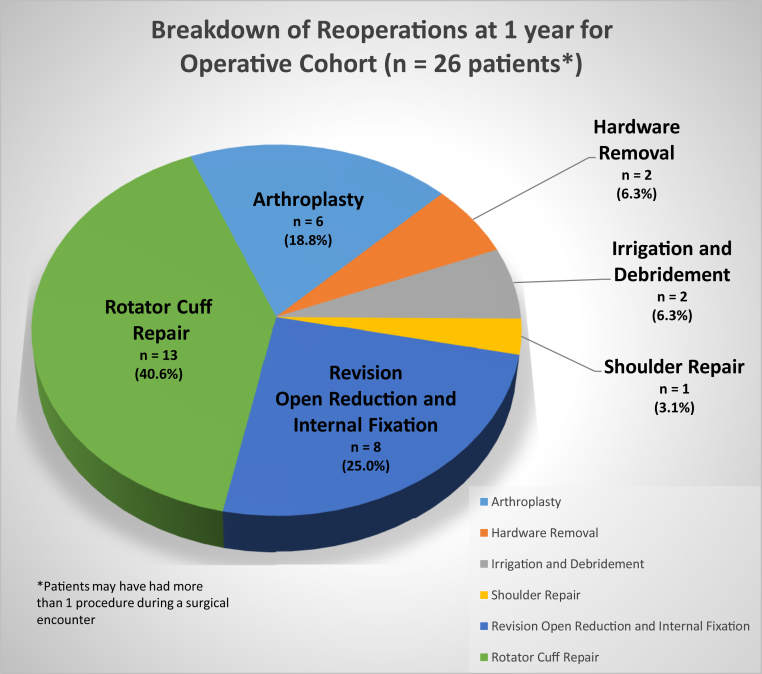
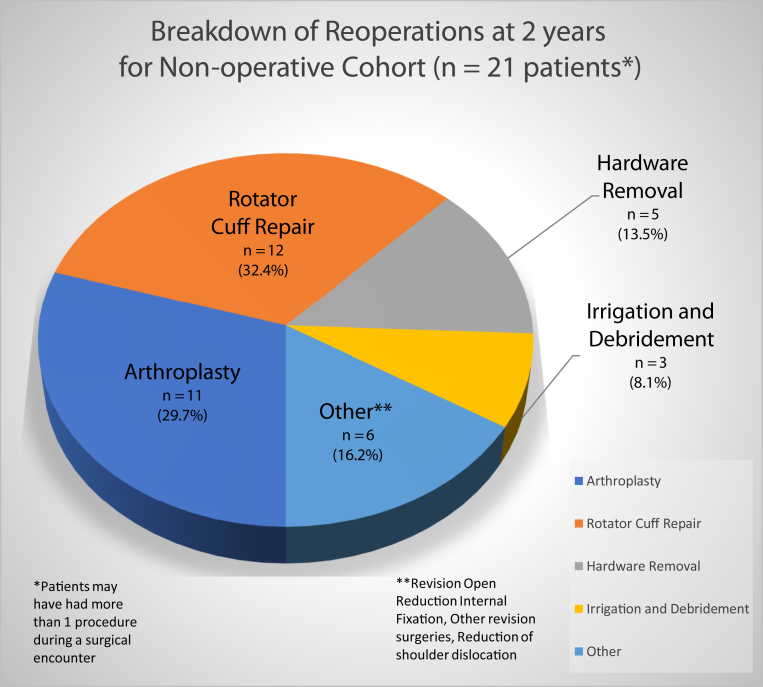
Patients undergoing operative fixation within the first 6 weeks of fracture diagnosis had had a reoperation rate of 2.7% (9 of 333, P < .001) at 90 days, 5.7% (19 of 333, P < .001) at 6 months, and 7.8% (26 of 333, P < .001) at 1 year. The types of reoperations in the operative cohort were RCR (40.6%), followed by revision ORIF (25.0%), arthroplasty (18.8%), irrigation and débridement (6.3%), and hardware removal (6.3%). Of the 8176 patients undergoing initial nonoperative care within the first 6 weeks of fracture diagnosis, 599 (7.3%) patients went on to have surgery within the first year. Most of the initial surgeries in the nonoperative cohort were ORIF (41.3%), followed by RCR (33.4%), arthroplasty (15.5%), and hardware removal (4.1%). A complete breakdown of the surgeries performed on the nonoperative cohort at 1 year can be seen in Figure 2. Of the 599 initial nonoperative patients who had surgery, 21 (3.5%) patients then underwent a reoperation in the following year. The predominant reoperation in the nonoperative cohort was RCR (32.4%) followed by arthroplasty (29.7%), hardware removal (13.5%), and irrigation and débridement (8.1%). The complete breakdown of reoperations within the operative and nonoperative cohorts can be seen in Figures 3 and 4, respectively.
Figure 2.
Breakdown of initial operations at 1 year for patients who failed nonoperative treatment within 6 weeks of sustaining a closed isolated greater tuberosity fracture.
Figure 3.
Breakdown of reoperations at 1 year for patients who failed operative fixation within 6 weeks of sustaining a closed isolated greater tuberosity fracture.
Figure 4.
Breakdown of reoperations at 2 years for patients who failed nonoperative care within 6 weeks of sustaining a closed isolated greater tuberosity fracture and then failed initial operative care.
The operative cohort had nerve injury at a rate of 2.7% (9 of 333, P = .004) at 90 days, 3.6% (12 of 333, P = .003) at 6 months, and 3.9% (13 of 333, P = .008) at 1 year. The ulnar nerve was the most commonly affected individual nerve in the operative cohort at all the time intervals accounting for 18.2% of nerve injuries at 90 days, 21.4% of nerve injuries at 6 months, and 25.0% of nerve injuries at 1 year. The operative cohort also had nonunion at a rate of 0.6% (2/333, P = .176) at 90 days, 1.8% (6/333, P = .023) at 6 months, and 2.7% (9/333, P = .004) at 1 year (Table II). The infection rate for the operative cohort was 3.0% (10/333, P = .020) at 90 days. Regarding systemic complications, patients initially treated operatively within the first 6 weeks of isolated greater tuberosity fracture developed anemia at a rate of 3.0% (10 of 333, P = .006) and had a myocardial infarction at a rate of 1.2% (4 of 333, P < .001) at 90 days as seen in Table III. The nonoperative cohort had nerve injury at a rate of 0.9% (73 of 8176) at 90 days, 1.4% (111 of 8176) at 6 months, and 1.7% (140 of 8176) at 1 year. The ulnar nerve was the most commonly affected individual nerve in the nonoperative cohort at all the time intervals accounting for 26.7% nerve injuries at 90 days, 34.3% nerve injuries at 6 months, and 38.8% nerve injuries at 1 year.
Table II.
Local complications of patients with operative fixation vs. nonoperative care within 6 weeks of sustaining a closed isolated greater tuberosity fracture.
| Local complications | Operative (n = 333) |
Nonoperative (n = 8176) |
OR | 95% CI | P value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Subsequent operation | |||||||
| 90 d | 9 | 2.7 | 487 | 6.0 | 34.31 | 26.76-44.12 | <.001 |
| 6 mo | 19 | 5.7 | 542 | 6.6 | 29.78 | 23.32-38.14 | <.001 |
| 1 yr | 26 | 7.8 | 599∗ | 7.3 | 26.10 | 20.50-33.33 | <.001 |
| Nerve injury | |||||||
| 90 d | 9 | 2.7 | 73 | 0.9 | 2.82 | 1.29-5.46 | .004 |
| 6 mo | 12 | 3.6 | 111 | 1.4 | 2.57 | 1.32-4.58 | .003 |
| 1 yr | 13 | 3.9 | 140 | 1.7 | 2.21 | 1.18-3.83 | .008 |
| Nonunion | |||||||
| 90 d | 2 | 0.6 | 43 | 0.5 | 2.05 | 0.61-5.19 | .176 |
| 6 mo | 6 | 1.8 | 80 | 1.0 | 2.38 | 1.04-4.71 | .023 |
| 1 yr | 9 | 2.7 | 106 | 1.3 | 2.58 | 1.29-4.68 | .004 |
| Infection | |||||||
| 90 d | 10 | 3.0 | 126 | 1.5 | 2.20 | 1.06-4.06 | .020 |
| 6 mo | 13 | 3.9 | 198 | 2.4 | 1.77 | 0.94-3.03 | .055 |
| 1 yr | 16 | 4.8 | 311 | 3.8 | 1.35 | 0.77-2.21 | .254 |
| Adhesive capsulitis | |||||||
| 90 d | 6 | 1.8 | 159 | 1.9 | 1.15 | 0.51-2.21 | .709 |
| 6 mo | 14 | 4.2 | 294 | 3.6 | 1.27 | 0.73-2.07 | .360 |
| 1 yr | 20 | 6.0 | 384 | 4.7 | 1.37 | 0.85-2.09 | .169 |
| Avascular necrosis | |||||||
| 90 d | 0 | 0.0 | 3 | 0.0 | N/A | N/A | N/A |
| 6 mo | 1 | 0.3 | 9 | 0.1 | 3.05 | 0.16-17.03 | .298 |
| 1 yr | 1 | 0.3 | 14 | 0.2 | 1.99 | 0.11-10.15 | .511 |
CI, confidence interval; OR, odds ratio.
21 patients went on to have a 2nd operation in year 2.
Table III.
Systemic complications of patients with operative fixation vs. nonoperative care within 6 weeks of sustaining a closed isolated greater tuberosity fracture.
| Systemic complications - 90 d | Operative (n = 333) |
Nonoperative (n = 8176) |
OR | 95% CI | P value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Cerebral vascular accident | 8 | 2.4 | 208 | 2.5 | 1.31 | 0.64-2.39 | .415 |
| Pneumonia | 5 | 1.5 | 157 | 1.9 | 0.87 | 0.31-1.93 | .558 |
| Pulmonary embolism | 3 | 0.9 | 53 | 0.6 | 1.42 | 0.34-3.92 | .759 |
| Myocardial infarction | 4 | 1.2 | 50 | 0.6 | 4.94 | 1.98-10.65 | <.001 |
| Acute renal failure | 6 | 1.8 | 182 | 2.2 | 0.90 | 0.35-1.88 | .794 |
| Deep vein thrombosis | 5 | 1.5 | 109 | 1.3 | 1.43 | 0.55-3.04 | .399 |
| Anemia | 10 | 3.0 | 134 | 1.6 | 2.41 | 1.21-4.35 | .006 |
| Respiratory failure | 4 | 1.2 | 106 | 1.3 | 0.98 | 0.30-2.38 | .970 |
| Urinary tract infection | 13 | 3.9 | 415 | 5.1 | 0.99 | 0.54-1.66 | .970 |
| Altered mental status | 4 | 1.2 | 154 | 1.9 | 0.66 | 0.20-1.58 | .415 |
CI, confidence interval; OR, odds ratio.
Discussion
The present study highlights several important points. Initial surgical and nonsurgical care for greater tuberosity fractures will require subsequent surgery at a similar rate, 7.8% and 7.3% respectively. After surgery, in patients treated either initially operatively or nonoperatively, 40.6% and 32.4% of them, respectively, will later need a RCR. Bhatia et al4 reported a reoperation rate as high as 14.3% in circumstances where the greater tuberosity was comminuted and directly impacted. The present study demonstrated a 7.8% surgical reoperation rate in the operative cohort in which all initial procedures were ORIF and a 3.5% reoperation rate in the nonoperative cohort in which the majority of initial procedures were ORIF. Secondary surgical intervention after ORIF is often due to displacement of the fracture fragment by deforming forces of the supraspinatus, infraspinatus, and teres minor. Small fracture fragments sometimes allow only tenuous fixation with screws and washers or suture anchors, which may not be sufficient to maintain reductions against the high forces observed in this footprint. This also applies to fractures treated nonsurgically as Platzeret al18 demonstrated 67% of nonoperative patients with minimally displaced greater tuberosity fractures had further fracture displacement of the greater tuberosity at a mean follow-up of 5.9 years. Although some secondary operations can be attributed to fracture fixation from the initial operation, reoperations may also be required owing to other causes unrelated to the surgery such as falls, traumatic accidents, bone quality, and metabolic processes.
Alterations in the greater tuberosity angle after a fracture may increase the risk of rotator cuff pathology as demonstrated by Cunningham et al.5 Schliemann et al22 further reported that secondary surgical intervention was often required to treat older patients who had initial nonoperative treatment with concomitant lesions of the rotator cuff and capsuloligamentous tissue. Complex injuries especially from a fracture dislocation type of injury, migration of the fracture fragment, and/or development of rotator cuff pathology in older patients may increase the need for another operation. This could be a potential explanation for RCR as the second most common initial operation (33.4%) in the nonoperative cohort and the main reoperation type demonstrated in both the operative (40.6%) and nonoperative cohorts (32.4%). Anatomic reduction is therefore important in treating greater tuberosity fractures regardless of giving operative or nonoperative treatment to minimize the risk of impingement and maintain the integrity of the rotator cuff.24 Barlow3 proposed revision ORIF for treating proximal humerus fractures especially in younger patients younger than the age of 60 years with preserved bone stock for failed greater tuberosity fractures. Revision ORIF was the second most frequent reoperation procedure (25.0%) observed in the operative cohort of this study, which consisted of adult patients at a mean age of 58 years with less comorbidities (P < .001). Punzi et al19 also reported the risk of post-traumatic osteoarthritis increases with a patient's age at the time of injury and with time from the onset of injury. In the present study, the population of the nonoperative cohort predominantly consisted of older adults at a mean age of 62 years (P < .001). Therefore, over time, these older patients may have developed glenohumeral osteoarthritis or rotator cuff arthropathy requiring shoulder arthroplasty, which was demonstrated in the nonoperative cohort to be the third most common initial operation (15.5%) and the second most common reoperation (29.7%).
The current data demonstrated the operative and nonoperative cohort to have elevated rates of nerve injury at 90 days, 6 months, and 1 year. Although previous studies have reported the axillary nerve to be the most commonly injured nerve during an isolated greater tuberosity fracture, the present study demonstrated the ulnar nerve to be the most affected individual nerve at all three-time intervals in both cohorts.8 As 5%-57% of greater tuberosity fractures are caused by glenohumeral dislocation, the nerve injuries in both cohorts could be attributed to the initial trauma.21 The elevated risk of nerve injuries at 90 days, 6 months, and 1 year specifically in the operative cohort may be due to more displaced and higher energy fractures being included in this group. The risk of neurological injury has been well documented in cases of displaced proximal humerus fractures as high as 67% owing to initial injury and subsequent treatment.23 The progressive increase in the rate of nerve injury over the year in the operative cohort may be attributed to detection of nerve injury with repeated examinations over the year in recovering patients or a definitive diagnosis of nerve injury at a later date.
Fracture-related infections have been documented to occur after initial injuries, and surgical procedures introduce a pathway of direct entry for contaminants such as endogenous flora.2,15 This may account for the elevated rate of infection in the operative cohort at 90 days (3.0%, P = .020). The operative cohort also demonstrated an elevated nonunion rate at 6 months (1.8%, P = .023) and 1 year (2.7%, P = .004). This is again presumably due to more severe injuries in the operative cohort possibly from polytrauma; however, this study revealed alcohol usage as a potentially relevant comorbidity. Regarding fracture healing, multiple studies have cited excessive alcohol use to be a risk factor for delayed union and nonunion.1,10,17 With a significant portion of the operative cohort in the present study having alcohol use as a preexisting comorbidity (P = .048), this confounder may have elevated the risk of nonunion at 6 months and 1 year in the operative cohort.
An inherent limitation of any database claims study is a human error created from medical billing code input, which may contribute to error within the results. This is not only mitigated by the large number of patients in this study but also a study from the Centers for Medicare and Medicaid Services reporting such instances make up only 1.0% of overall payments.26 This study defined nonoperative treatment as no operations within the first 6 weeks of an isolated greater tuberosity fracture diagnosis. Owing to this cutoff, the nonoperative cohort and nonoperative cohort that then underwent surgery may be overestimated, therefore underestimating the surgical cohort, for example a patient initially presented to a surgeon 7 weeks after diagnosis and was indicated for surgical fixation at that visit. However, in this large database, the sampling bias would be low. To reduce variability, this study defined operative fixation by 1 CPT code for open treatment of greater humeral tuberosity fracture as patients with displaced greater tuberosity fractures are generally treated with this code regardless of arthroscopic or open technique.18,25 However, this study did not specifically query for arthroscopic codes to determine whether arthroscopic techniques were also used. In addition, owing to the use of a nationwide database, the specific scope of practice and training expertise of each treating surgeon could not be determined, which could have influenced the complication profile. Although posteriorly displaced fractures are less debilitating and more amenable to nonsurgical management, fracture displacement direction or length could not be gathered from this database; therefore, no definitive conclusions can be made regarding severity of injury and displacement position leading to a specific treatment. In addition, the database does not include any functional outcome data.
Conclusion
The present study highlights a reoperation rate at 1 year of 7.8% when providing surgical care to patients with isolated greater tuberosity fractures and rotator cuff repair as the most common reoperation. Patients initially managed nonoperatively subsequently undergo operations related to this injury at a rate of 7.3% at 1 year with ORIF as the most frequent operation and reoperations at a rate of 3.5% at 2 years with rotator cuff repair again as the most common reoperation. With an elevated rate of subsequent operations and especially the need for rotator cuff repair after a greater tuberosity fracture, education of patients regarding the potential requirement for operations for the sequelae of this injury is paramount.
Disclaimers:
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board exemption was given by Tulane University Biomedical Institutional Review Board for study #: 2020-1368.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2020.12.002.
Supplementary data
References
- 1.Amroodi M.N., Behshad V., Motaghi P. Long-term results, functional outcomes and complications after open reduction and internal fixation of neglected and displaced greater tuberosity of humerus fractures. Arch Bone Jt Surg. 2016;4:330–336. doi: 10.22038/abjs.2016.7540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson P.A., Savage J.W., Vaccaro A.R., Radcliff K., Arnold P.M., Lawrence B.D. Prevention of surgical site infection in spine surgery. Neurosurgery. 2017;80(3S):S114–S123. doi: 10.1093/neuros/nyw066. [DOI] [PubMed] [Google Scholar]
- 3.Barlow J.D. Complications after ORIF of proximal humerus fractures—how to deal with them. Ann Jt. 2020 doi: 10.21037/aoj-20-77. [DOI] [Google Scholar]
- 4.Bhatia D.N., van Rooyen K.S., du Toit D.F., de Beer J.F. Surgical treatment of comminuted, displaced fractures of the greater tuberosity of the proximal humerus: a new technique of double-row suture-anchor fixation and long-term results. Injury. 2006;37:946–952. doi: 10.1016/j.injury.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham G., Nicodème-Paulin E., Smith M.M., Holzer N., Cass B., Young A.A. The greater tuberosity angle: a new predictor for rotator cuff tear. J Shoulder Elbow Surg. 2018;27:1415–1421. doi: 10.1016/j.jse.2018.02.051. [DOI] [PubMed] [Google Scholar]
- 6.DeBottis D., Anavian J., Green A. Surgical management of isolated greater tuberosity fractures of the proximal humerus. Orthop Clin North Am. 2014;45:207–218. doi: 10.1016/j.ocl.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 7.George M.S. Fractures of the greater tuberosity of the humerus. J Am Acad Orthop Surg. 2007;15:607–613. doi: 10.5435/00124635-200710000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Green A., Izzi J. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003;12:641–649. doi: 10.1016/S1058-2746(02)86811-2. [DOI] [PubMed] [Google Scholar]
- 9.Gruson K.I., Ruchelsman D.E., Tejwani N.C. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008;39:284–298. doi: 10.1016/j.injury.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 10.Healy W.L., Jupiter J.B., Kristiansen T.K., White R.R. Nonunion of the proximal humerus. A review of 25 cases. J Orthop Trauma. 1990;4:424–431. [PubMed] [Google Scholar]
- 11.Iannotti J.P., Gabriel J.P., Schneck S.L., Evans B.G., Misra S. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992;74:491–500. [PubMed] [Google Scholar]
- 12.Levy D.M., Erickson B.J., Harris J.D., Bach B.R., Verma N.N., Romeo A.A. Management of isolated greater tuberosity fractures: a systematic review. Am J Orthop (Belle Mead NJ) 2017;46:E445–E453. [PubMed] [Google Scholar]
- 13.Liao W., Zhang H., Li Z., Li J. Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures? Clin Orthop Relat Res. 2016;474:1269–1279. doi: 10.1007/s11999-015-4663-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mattyasovszky S.G., Burkhart K.J., Ahlers C., Proschek D., Dietz S.O., Becker I. Isolated fractures of the greater tuberosity of the proximal humerus: a long-term retrospective study of 30 patients. Acta Orthop. 2011;82:714–720. doi: 10.3109/17453674.2011.618912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Metsemakers W.J., Morgenstern M., McNally M.A., Moriarty T.F., McFadyen I., Scarborough M. Fracture-related infection: a consensus on definition from an international expert group. Injury. 2018;49:505–510. doi: 10.1016/j.injury.2017.08.040. [DOI] [PubMed] [Google Scholar]
- 16.Neer C.S. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 17.Papakonstantinou M.K., Hart M.J., Farrugia R., Gosling C., Kamali Moaveni A., van Bavel D. Prevalence of non-union and delayed union in proximal humeral fractures. ANZ J Surg. 2017;87:55–59. doi: 10.1111/ans.13756. [DOI] [PubMed] [Google Scholar]
- 18.Platzer P., Thalhammer G., Oberleitner G., Kutscha-Lissberg F., Wieland T., Vecsei V. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma. 2008;65:843–848. doi: 10.1097/01.ta.0000233710.42698.3f. [DOI] [PubMed] [Google Scholar]
- 19.Punzi L., Galozzi P., Luisetto R., Favero M., Ramonda R., Oliviero F. Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation. RMD open. 2016;2:e000279. doi: 10.1136/rmdopen-2016-000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rouleau D.M., Laflamme G.Y., Mutch J. Fractures of the greater tuberosity of the humerus: a study of associated rotator cuff injury and atrophy. Shoulder Elbow. 2016;8:242–249. doi: 10.1177/1758573216647896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rouleau D.M., Mutch J., Laflamme G.-Y. Surgical treatment of displaced greater tuberosity fractures of the humerus. J Am Acad Orthop Surg. 2016;24:46–56. doi: 10.5435/JAAOS-D-14-00289. [DOI] [PubMed] [Google Scholar]
- 22.Schliemann B., Heilmann L.F., Raschke M.J., Lill H., Katthagen J.C., Ellwein A. Isolated fractures of the greater tuberosity: when are they treated conservatively?: A baseline study. Obere Extrem. 2018;13:106–111. doi: 10.1007/s11678-018-0459-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Warrender W.J., Oppenheimer S., Abboud J.A. Nerve monitoring during proximal humeral fracture fixation what have we learned? Clin Orthop Relat Res. 2011;469:2631–2637. doi: 10.1007/s11999-010-1760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White E.A., Skalski M.R., Patel D.B., Gross J.S., Tomasian A., Heckmann N. Isolated greater tuberosity fractures of the proximal humerus: anatomy, injury patterns, multimodality imaging, and approach to management. Emerg Radiol. 2018;25:235–246. doi: 10.1007/s10140-018-1589-8. [DOI] [PubMed] [Google Scholar]
- 25.Williams G.R., Wong K.L. Two-part and three-part fractures: open reduction and internal fixation versus closed reduction and percutaneous pinning. Orthop Clin North Am. 2000;31:1–21. doi: 10.1016/s0030-5898(05)70124-3. [DOI] [PubMed] [Google Scholar]
- 26.2019 Medicare fee-for-service supplemental improper payment data. CMS; 2019. Available at: https://www.cms.gov/research-statistics-data-and-systemsmonitoring-programsmedicare-ffs-compliance-programscertcert/2019-medicare-fee-service-supplemental-improper-payment-data. Accessed September 17, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.