Abstract
Background
As the number of total shoulder arthroplasties (TSAs) performed annually increases, some surgeons have begun to shift toward performing TSAs in the outpatient setting. However, it is imperative to establish the safety of outpatient TSA. The purpose of this systematic review was to define complication, readmission, and reoperation rates and patient-reported outcomes after outpatient TSA.
Methods
A systematic review of the literature was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines using three databases (PubMed, Ovid, and Embase). English-language publications describing results on complication rates in patients who underwent TSA in an outpatient or ambulatory setting were included. All nonclinical and deidentified database studies were excluded. Bias assessment was conducted with the methodologic index for nonrandomized studies criteria.
Results
Seven studies describing outcomes in outpatient TSA were identified for inclusion. The included studies used varying criteria for selecting patients for an outpatient procedure. The total outpatient 90-day complication rate (commonly including hematomas, wound issues, and nerve palsies) ranged from 7.1%-11.5%. Readmission rates ranged from 0%-3.7%, and emergency and urgent care visits ranged from 2.4%-16.1%. Patient-reported outcomes improved significantly after outpatient TSA in all studies. Two studies found a higher complication rate in the comparative inpatient cohort (P = .023-.027). Methodologic index for nonrandomized studies scores ranged from 9 to 11 (of 16) for noncomparative studies (n = 3), while all comparative studies received a score of a 16 (of 24).
Conclusion
Outpatient TSA in properly selected patients results in a similar complication rate to inpatient TSA. Further studies are needed to aid in determining proper risk stratification to direct patients to inpatient or outpatient shoulder arthroplasty.
Keywords: Total shoulder arthroplasty (TSA), Reverse total shoulder arthroplasty (rTSA), Outpatient, Ambulatory
With an ever-increasing emphasis on cost-effective delivery of health care, total joint arthroplasty (TJA) has received continued attention as a target for improved efficiency and cost reduction.35 These efforts have resulted in decreased lengths of stay and gradual transition to outpatient and same-day discharges for various TJA procedures. This transition has initially been observed in total knee (TKA) and total hip (THA) arthroplasty.18,29 However, this move has recently received more attention in the total shoulder arthroplasty (TSA) literature, given the continued increase in the number of TSA procedures and concurrent decrease in both lengths of stay and complication rates.1,11,14,19, 20, 21,27,31,33,34 However, the push for improved efficiency and cost reduction must be continually balanced with concerns for patient safety, perioperative complications, and patient outcomes.
Retrospective investigations have demonstrated no significant differences between same-day discharge and inpatient TSA for several measures of perioperative complications including readmission rates, emergency department visits, and 1-year mortality.6,8,22,26 Given that candidates for outpatient arthroplasty are generally healthier with fewer comorbidities, they may even have significantly lower complication rates postoperatively.26,30 Additional studies have attempted to identify patient populations and characteristics that make them suitable candidates for outpatient arthroplasty procedure. This has included patient selection algorithms that are subsequently tested based on observed complications rates, including cardiopulmonary, thromboembolic events, wound complications, pain management issues, and readmission rates.5,16
As the economic and healthcare system pressures continue to push TSA procedures into the outpatient and ambulatory setting, it is imperative to have a comprehensive understanding of the current literature including perioperative complications, readmission rates, and ultimately patient-reported outcomes (PROs). Therefore, the purpose of this investigation was to perform a systematic review and summary of the available literature regarding outpatient TSA, including complications, and PROs.
Methods
Search strategy
Systematic review registration was performed in March 2020 using the International Prospective Register of Systematic Reviews (currently under editorial assessment). This investigation was completed in accordance with the 2009 Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. A search of the literature was performed to identify articles investigating complication rates after outpatient TSA or reverse TSA (rTSA). PubMed, Ovid, and Embase databases were searched for relevant studies from the inception of the databases to February 25, 2020. Search terms included a combination of the following: (1) “outpatient,” “ambulatory,” “same day,” “24-hour,” OR “23-hour,” AND (2) “shoulder,” AND (3) “arthroplasty” OR “replacement.”
Study selection and data extraction
A search of the databases resulted in 789 total studies. Studies were uploaded to and reviewed in Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org). Two independent reviewers (E.P. and H.H.) screened title and abstracts for relevance under the guidance of the senior author (N.V.), followed by full-text review. If the two reviewers did not reach a consensus, inclusion was ultimately decided by the senior author (N.V.). To have qualified for inclusions, studies must have (1) reported on TSA or rTSA, (2) described a procedure performed in an outpatient or ambulatory setting, and (3) included information on postoperative complication rate. Exclusion criteria were applied to (1) articles not in the English language, (2) nonhuman studies, (3) basic science studies, (4) systematic review articles, meta-analysis, and expert opinions, and (5) deidentified database studies. Based on these criteria, 9 articles were included in the final cohort. However, three of these studies had overlapping patient data sets, and thus the study with the largest patient cohort was included and the two others by the same senior author were removed.6,16,25 Owing to the absence of randomized controlled trials, pooled statistics and formal meta-analysis was not performed to avoid potentially inaccurate conclusions.
All articles then underwent data extraction by a single reviewer (H.H.). Extraction included information on demographics, comorbidities, outcomes (complication number and type, PROs), and the demographics and outcomes of the comparative inpatient cohort, if applicable.
Bias assessment
The quality and bias of the studies was assessed using the methodologic index for nonrandomized studies (MINORS) score.32 The MINORS score is an 8- (for noncomparative studies) or 12-question (for comparative studies) assessment that was developed to describe the quality of observational or nonrandomized trials. Questions range from clearly stating an aim to stating the percentage of patients lost to follow-up and to whether a power analysis was performed. Each question is scored with a “0” if it is not addressed, “1” if it addressed but inadequately, or “2” if it is addressed and adequate. Thus, each article could attain a maximum of 16 (noncomparative) or 24 (comparative study) points. Two authors (E.P. and H.H.) independently performed the MINORS assessment for each included study. Any disagreements were resolved by consensus.
Results
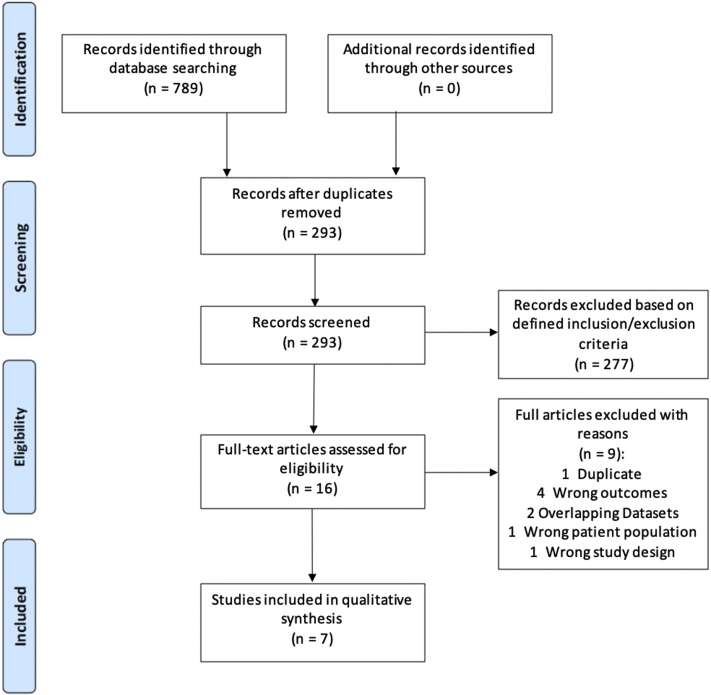
A search of the databases resulted in 789 studies (Figure 1). After duplicates were removed, 293 studies underwent title and abstract review. Sixteen of these studies underwent full-text review, and 9 studies were included. Of these studies, 2 were removed owing to overlapping patients.6,25 Thus, 7 studies accounting for 937 patients were ultimately included in the final qualitative assessment.4,8,12,16,22,23,26
Figure 1.
PRISMA flowchart of study selection. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Demographics
Article details and patient demographics for each study are included in Table I. All studies included both TSA and rTSA procedures except that of Erickson et al, which only included rTSA.12 Each study described unique criteria for selecting patients for outpatient TSA or rTSA. All articles except that by Kramer et al22 stated that patient comorbidities or current health status was accounted for in the decision-making process. Instead, Kramer et al22 used anesthesiologist and surgeon preference to make this decision. Four studies (Charles et al,8 Nwankwo et al,26 Erickson et al,12 and Leroux et al23) also took into account the patient’s current social and/or living situation. The mean American Society of Anesthesiologists (ASA) score was a mean of 2.3 for the 4 studies in which it was reported. In addition, Kramer et al22 reported that 36.3% of their cohort had an ASA score ≥ 3.
Table I.
Demographic information of the included studies.
| Author | Study type | Factors considered in for outpatient surgery selection | N (TSA/rTSA/Hemi) | Age | Male/Female | BMI | Charlson comorbidity index | ASA score | History of smoking | Comorbidities | Length of stay, hr |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fournier et al., 201916 | LOE IV: Case series | Age Preoperative anemia Pulmonary disease CAD HTN CHF |
61 (49/12/0) | 58 (range: 37 to 69) | 39/22 | 31 (range: 21 to 49) | Not Reported | 2.3 ± 0.5 | Not reported | Not reported | Not reported |
| Charles et al., 20198 | LOE IV: Case series | Medical comorbidities Prior narcotic use Social support at home |
50 (44/4/2) | 56.9 ± 6.9 | 40/10 | 29.8 ± 5.9 | 1.6 ± 1.2 | Not reported | 1 (2%) | Not reported | 9.6 |
| Nwankwo et al., 201826 | LOE III: Cohort Comparison | Social support Health status Patient preference |
118 (96/20/2) | 68.1 (range: 31 to 90) | 63/55 | Not reported | Not reported | 2.3 | Not reported | Not reported | NA not reported |
| Erickson et al., 201912 | LOE III: Cohort Comparison | Medical comorbidities Living status Patient preference |
241 (0/241/0) | 68.93 | 115/126 | 29.72 | Not Reported | NA not reported | 28 (11.6%) | Diabetes: 17 (7.1%) | Not reported |
| Leroux et al., 201823 | LOE IV: Case series | Exclusion criteria: COPD, renal disease, DVT, sleep apnea, active or untreated CAD or CVD | 41 (32/9/0) | 60.6 ± 4.8 | 19/22 | 31.8 ± 6.6 | 2.9 ± 1.9 | 2.3 ± 0.6 | 12 (29.3%) | Diabetes: 4 (10%) HTN: 25 (60%) Depression: 12 (28.6%) |
3.54 |
| Bean et al., 20184 | LOE III: Cohort Comparison | Inclusion Criteria: No history of significant cardiopulmonary disease, DVT, PE, or severe obstructive sleep apnea, ASA score of <3, age < 65 y, no preoperative opioid dependence, no walker or wheelchair dependence, social support at home, living within 1 h from the surgery center, motivated for the outpatient process Relative exclusion criteria: BMI > 30 |
21 (12/9/0) | 59.8 (IQR: 57.0 to 61.8) | 10/10 | 29.0 ± 7.2 | 1.76 ± 0.77 | 2.3 ± 0.5 | 9 (43%) | Diabetes: 3 (15%) Cardiopulmonary: 4 (19.1%) |
5.35 |
| Kramer et al., 201822 | LOE III: Cohort Comparison | Based on surgeon and anesthesiologist rather than specific preexisting condition, no exclusions were made based on comorbidities | 405 (294/111/0) | 69.4 ± 8.2 | 224/181 | < 30: 234 (57.8%) 30 to 34.9: 104 (25.7%) ≥ 35: 67 (16.5%) |
Not reported | ASA ≥ 3: 144 (36.3%) | 237 (58.5%) | Diabetes: 81 (20%) Chronic pulmonary disease: 90 (22.3%) Congestive heart failure: 13 (3.2%) Cognitive: 36 (8.9%) Drug abuse: 5 (1.2%) Pulmonary circulation disorders: 4 (1%) |
Not reported |
ASA, American Society of Anesthesiologists; BMI, body mass index; CAD, coronary artery disease; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; CVD, cerebrovascular disease; DVT, deep vein thrombosis; HTN, hypertension; IQR, interquartile range; LOE, level of evidence; PE, pulmonary embolism; rTSA, reverse total shoulder arthroplasty; TSA, total shoulder arthroplasty.
Complications
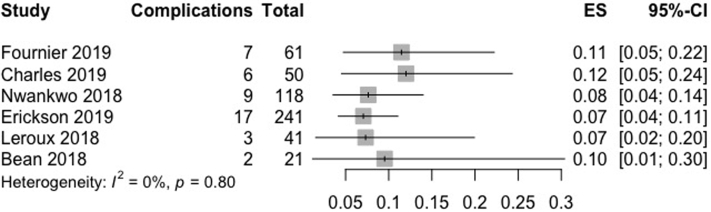
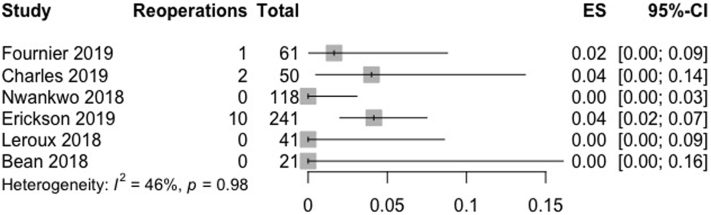
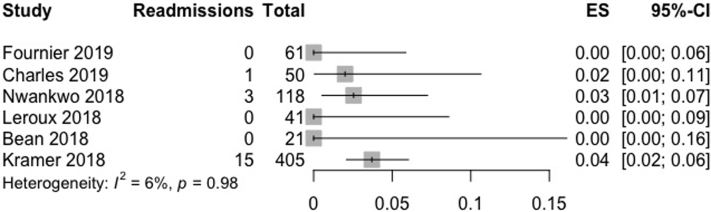
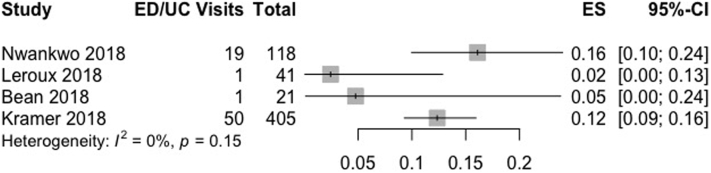
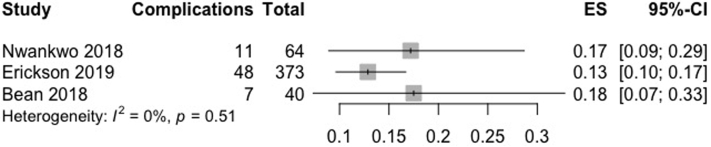
Complication, reoperation, readmission rates, and emergency department (ED) or urgent care visits are reported in Table II (Figure 2, Figure 3, Figure 4, Figure 5). All but 1 study reported on 90-day complication rates.12 Total 90-day complication rates ranged from 7.1%-11.5%. Commonly reported 90-day complications included wound issues, infections, and nerve palsies. Ninety-day reoperation rates were reported by 5 studies. Nwankwo et al,26 Bean et al,4 and Leroux et al23 reported 0 reoperations. Charles et al8 reported 1 incision and drainage procedure, while Fournier et al16 reported 1 hematoma evacuation. Three studies reported no readmissions (Fournier et al,16 Bean et al,4 Leroux et al23). Charles et al8 reported 1 readmission who was the same patient who underwent the incision and drainage procedure. Nwankwo et al26 and Kramer et al22 reported a readmission rate of 2.5% (3 patients: acute kidney injury, aortic dissection, and abdominal pain) and 3.7% (readmission reason not specified), respectively. However, these studies did not report how long after surgery these readmissions occurred. In addition, three studies reported on 90-day ED and/or urgent care visits. Nwankwo et al26 reported a 16% ED visit rate, while Leroux et al23 and Bean et al4 reported a rate of 2.4% and 4.8%, respectively. However, Nwankwo et al26 reported that many of these ED visits were related to exacerbations of preexisting chronic medical conditions.25
Table II.
Complication rates and types of complication for each included study.
| Author | Postoperative F/U | Reoperation | Reoperation type | Readmission | Readmission reason | ED/UC visits | Total complications | Complications |
|---|---|---|---|---|---|---|---|---|
| Fournier et al., 201916 | 90 days | 1 (1.6%) | Hematoma evacuation (1) | 0 | NA | Not reported | 7 (11.5%) | Hematoma: 1 (1.6%) Perioperative anesthesia issue: 2 (3.3%) Arthrofibrosis: 2 (3.3%) Anterior subluxation: 1 (1.6%) Subscapularis rupture: 1 (1.6%) |
| Charles et al., 20198 | 90 days Final f/u: 9.3 ± 6 months |
90 days: 1 (2%) Total at final f/u: 2 (4%) |
90 days: I&D (1) | 90 days: 1 (2%) | I&D (1) | Not reported | 90 days: 4 (8%) Total at final f/u: 6 (12%) |
90 days: Hematoma: 1 (2.0%) Infection: 1 (2.0%) Nerve palsy: 1 (2.0%) DVT: 1 (2.0%) Final f/u: Subscapularis rupture: 2 (4%) |
| Nwankwo et al., 201826 | 90 days | 0 | NA | 3 (2.5%) | Abdominal pain (1) Aortic dissection (1) AKI (1) |
ED: 19 (16.1%) | 9 (7.6%) | Death: 1 (0.8%) Undefined wound issue: 4 (3.4%) Nerve palsy: 1 (0.8%) Abdominal pain with identified liver lesions: 1 (0.8%) Ascending aortic dissection: 1 (0.8%) Acute kidney injury: 1 (0.8%) |
| Erickson et al., 201912 | 2 years | 10 (4.1%) | I&D (3) Baseplate revision for loosening (2) Revision for instability (2) ORIF (2) |
Not reported | NA | Not reported | 17 (7.1%) | MI/death: 1 (0.4%) Pneumonia: 1 (0.4%) Systemic Infection: 2 (0.8%) Localized Infection: 2 (0.8%) Implant Instability: 1 (0.4%) Shoulder dislocation: 4 (1.7%) Humeral fracture: 1 (0.4%) Acromial stress fracture: 3 (1.2%) Excessive pain: 2 (0.8%) |
| Leroux et al., 201823 | 90 days | 0 | NA | 0 | NA | UC: 1 (2.4%) | 3 (7.3%) | Hematoma: 1 (2.4%) Rash: 1 (2.4%) Superficial phlebitis: 1 (2.4%) |
| Bean et al., 20184 | 90 days | 0 | NA | 0 | NA | UC: 1 (4.8%) | 2 (9.5%) | Brachioplexopathy: 1 (4.8%) Fall: 1 (4.8%) |
| Kramer et al., 201822 | 90 days | Not reported | NA | 15 (3.7%) | Not reported | ED: 50 (12.3%) | Not reported | VTE: 1 (.2%) 1-year mortality: 5 (1.2%) |
AKI, acute kidney injury; DVT, deep vein thrombosis; ED, emergency department; F/U, follow-up; I&D, incision and drainage; MI, myocardial infarction; NA, not applicable; ORIF, open reduction internal fixation; UC, urgent care; VTE, venous thromboembolism.
Figure 2.
Pooled results for outpatient complication rates.
Figure 3.
Pooled results for outpatient reoperation rates.
Figure 4.
Pooled results for outpatient readmission rates.
Figure 5.
Pooled results for outpatient emergency department or urgent care rates. ED, emergency department; UC, urgent care.
Two studies reported on longer term complications. Charles et al8 reported at 9.3 ± 6 months that 1 additional patient underwent reoperation and 2 additional patients had complications (subscapularis failures). Erickson et al12 reported a 4.1% reoperation rate within the first 2 years postoperatively and a total complication rate of 7%.
Patient-reported outcomes
Three studies included PROs. Of the three, 1 study only reported preoperative PROs and 1 study only reported postoperative satisfaction (Table III). Bean et al4 did not compare preoperative with postoperative visual analog scale (VAS) pain scores, instead only compared them with the inpatient cohort. Charles et al8 reported significant improvements compared with baseline for Single Assessment Numeric Evaluation, American Shoulder and Elbow Surgeons (ASES) score, and VAS (all P < .001) and in forward elevation and external rotation (both P < .001). Similarly, Erickson et al12 reported improvements from preoperative to each of their two tested postoperative time points: 1 and 2 years (P < .0001 for all). Finally, Leroux et al23 reported that 84.9% of patients were very satisfied, 12.1% were satisfied, and 3% were adequately satisfied at a mean of 60 weeks postoperatively (range 16.4 to 156 weeks).
Table III.
Patient-reported outcomes for outpatient TSA/rTSA patient.
| SANE | ||||||
|---|---|---|---|---|---|---|
| F/U | Preoperative SANE | Postoperative SANE | Postoperative SANE | |||
| Charles et al., 20198∗ | 9.3 ± 6.0 mo (P < .001) | 39.6 ± 23.4 | 77.6 ± 19.0 | - | ||
| Erickson et al., 201912∗ |
1 y (P < .0001) 2 y (P < .0001) |
30.7 ± 19.4 |
74.3 ± 23.0 |
75.9 ± 21.4 |
||
| ASES | ||||||
| F/U |
Preoperative ASES |
Postoperative ASES |
Postoperative ASES |
|||
| Charles et al., 20198∗ | 9.3 ± 6.0 mo (P < .001) | 44.4 ± 17.1 | 80.2 ± 22.4 | - | ||
| Erickson et al., 201912∗ | 1 y (P < .0001) 2 y (P < .0001) |
40.5 ± 17.6 | 79.7 ± 17.3 | 82.6 ± 14.3 | ||
| Bean et al., 20184 |
NA |
37.7 ± 14.5 |
- |
- |
||
| VAS | ||||||
| F/U |
Preoperative VAS |
Postoperative VAS |
Postoperative VAS |
Postoperative VAS |
||
| Charles et al., 20198∗ | 9.3 ± 6.0 mo (P < .001) | 5.2 ± 2.0 | 1.5 ± 2.3 | - | - | |
| Erickson et al., 201912∗ | 1 y (P < .0001) 2 y (P < .0001) |
5.5 ± 2.6 | 1.5 ± 2.0 | 1.33 ± 1.7 | - | |
| Bean et al., 20184 |
2 weeks (NA) 6 weeks (NA)) 3 mo (NA) |
8.0 (range: 0 to 10) |
2 (range: 0 to 8) |
2 (range: 0 to 8) |
1 (range: 0 to 8) |
|
| VR-12 | ||||||
| F/U |
Preoperative VR-12 |
|||||
| Bean et al., 20184 | NA | |||||
| VR-12 M | 36.3 ± 11.4 | |||||
|
VR-12 P |
0.6 ± 0.1 |
|||||
| ROM | ||||||
| F/U |
Preoperative ROM |
Postoperative ROM |
||||
| Charles et al., 20198∗ | 9.3 ± 6.0 mo (P < .001) | |||||
| FE | 124.6 ± 35.3 degrees | 150.2 ± 29.7 degrees | ||||
|
ER |
31.3 ± 17.9 degrees |
49.5 ± 15.8 degrees |
||||
| Satisfaction | ||||||
| F/U |
Postoperative Satisfaction |
|||||
| Leroux et al., 201823 | 60 weeks (range: 16.4 -156 weeks) | |||||
| Satisfaction | Very 28 (84.9%) Satisfied 5 (15.2%) Adequate 1 (3%) |
|||||
| Would not do outpatient again? | 2 (5.7%) | |||||
| Did Not Feel Ready for Discharge? | 2 (5.7%) | |||||
ASES, American Shoulder and Elbow Surgeons assessment; ER, external rotation; FE, forward elevation; F/U, follow-up; NA, not applicable; ROM, range of motion; SANE, single assessment numeric evaluation; VAS, visual analog scale; VR-12, Veteran RAND 12 item health survey.
Statistically significant.
Comparison with an inpatient cohort
Four of the included studies compared outpatient complication rates with an inpatient cohort (Table IV, Figure 6). Three studies compared the preoperative demographics of the cohorts. Bean et al4 only reported differences in the number of patients receiving an interscalene block (2 in outpatient vs. 18 in inpatient, P = .005). In contrast, the inpatient cohort described by Nwankwo et al26 was significantly older (P = .01) and had a significantly higher ASA score (P < .01) than the outpatient cohort. Erickson et al12 also had an inpatient cohort that was older (P < .0001), had a greater proportion of female patients (P < .001), had a higher average body mass index (P = .022), and had a higher rate of diabetes (P = .007).
Table IV.
Complication rates and types of complication for each included study.
| F/U | N (TSA/rTSA/hemi) | Age | Male/Female | BMI | Comorbidities | Reoperation | Reoperation type | Readmission | Readmission reason | ED/UC | Total complications | Complications | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nwankwo et al., 201826 | 90 d | 64 (45/25/4) | 68.1 (range: 31 to 90) (P = .01) | 55/63 (P = .15) | NA | NA | 1 (1.6%) | Implant revision (1) | 6 (9.4%) (P = .27) | CHF exacerbation (1) AMS/TIA (1) Decompensated cirrhosis (1) Atrial fibrillation (1) Fall (1) Pneumonia (1) |
ED: 18 (28.1%) (P = .150 - .774) | 11 (17.1%) | CVA: 2 Wound issue: 2 Nerve issue: 1 CHF exacerbation: 1 AMS/TIA: 1 Decompensated cirrhosis: 1 Atrial fibrillation: 1 Fall: 1 Pneumonia: 1 |
| Erickson et al., 201912 | 2 y | 373 (0/373/0) | 72.43 (P < .001) | 128/245 (P < .001) | 29.72 ± 11.5 (P = .022) | Diabetes: 58 (15.5%) (P = .007) | 17 (4.6%) | Humeral fracture ORIF (4) I&D (4) Revision for instability (3) Distal clavicle excision (3) Conversion to hemiarthroplasty (1) Revision for stiffness (1) Revision biceps tenodesis (1) |
Not Reported | NA | Not Reported | 48 (12.9%) (P = .023) | Acromion stress fracture: 8 Subscapularis tear: 2 Localized infection: 2 Biceps injection: 8 PE: 2 Dislocation: 4 Wound dehiscence: 2 MI or death: 1 Hematoma evacuation: 1 Acromioclavicular joint injection: 2 Instability of implant: 2 Swelling and/or urinary retention: 1 Excessive pain: 1 Subluxation: 1 Hypoxia: 3 Deep venous thrombosis: 1 Humeral fracture: 1 Numbness and/or nerve injury: 6 |
| Bean et al., 20184 | 90 d | 40 (22/17/0) | 59.9 (IQR: 55.9 to 62.8) (P = .5116) | 18/19 | 30.6 ± 7.3 (P = .3958) | Cardiac/pulmonary disease/CVA: 14 (35%), (P = 0.1943) Diabetes: 9 (24.3%) (P = .5124) |
0 | NA | 1 (2.5%) (P =0.9999) | NA | ED: 2 (5%) (P = .54) UC: 0 (0%) |
7 (17.5%) (P = .9999) | MI: 1 Transient axillary neurapraxia: 1 Fall: 1 Transient brachial plexopathy: 1 Postoperative bigeminy and hypoxia: 1 Constipation: 1 Superior mesenteric vein thrombosis: 1 |
| Kramer et al., 201822 | 90 d | 6098 (1894/4204/0) | 70.1 ± 8.9 | 2810/3288 | < 30: 3376 30-34.9: 1540 ≥ 35: 4954 |
Alcohol abuse: 236 (4%) Chronic pulmonary disease: 1337 (22.5%) Cognitive disorders: 749 (12.6%) CHF: 281 (4.7%) Diabetes: 1674 (27.5%) Drug abuse: 152 (2.6%) Pulmonary circulation disorders: 90 (1.5%) |
Not Reported | NA | 342 (5.6%) (P = .198) | NA | ED: 760 (12.5%) (P = .609) | Not reported | VTE: 66 (1.1%) Deep Infection: 16 (0.3%) 1 y: 66 (1.1%) (P = .320) |
AMS, altered mental status; BMI, body mass index; CHF, congestive heart failure; CVA, cerebrovascular accident; ED, emergency department; F/U, follow-up; IQR, interquartile range; MI, myocardial infarction; ORIF, open reduction internal fixation; PE, pulmonary embolism; rTSA, reverse total shoulder arthroplasty; TIA, transient ischemic attack; TSA, total shoulder arthroplasty; UC, urgent care; VTE, venous thromboembolism.
Included P values refer to comparisons between inpatient and outpatient cohorts.
Figure 6.
Pooled results for inpatient complication rates.
Bean et al4 and Nwankwo et al26 reported an inpatient 90-day complication rate of 17.5% and 17.1%, respectively. Similar to the outpatient cohort, the high complication rate reported by Nwankwo et al26 was likely owing to the high rate of ED visits, most of which, the authors stated, were likely not surgery related but because of exacerbations of preexisting chronic medical conditions.25 One reoperation (implant revision) was reported by Nwankwo et al26 during this period. The inpatient 90-day readmission rate was 2% to 5% to 9.4%. Kramer et al22 and Bean et al4 reported no significant differences between outpatient and inpatient readmissions, ED/urgent care visits, or complication rate. In contrast, Nwankwo et al26 observed a higher inpatient readmission rate (P = .027). Erickson et al12 compared complications at 2 years and found the inpatient group to have a significantly higher rate of complications (P = .023).
Erickson et al12 and Bean et al4 compared preoperative and postoperative PROs between the inpatient and outpatient TSA/rTSA cohorts (Table V). Erickson et al12 reported a significantly lower preoperative ASES score in the inpatient cohort (36.3 ± 17.6 vs. 40.5 ± 17.6, P = .0046). Otherwise, no differences were observed between cohorts for the ASES, VAS, or Single Assessment Numeric Evaluation score preoperatively or at the 1- or 2-year follow-up. In addition, Erickson et al12 reported no significant differences between the change in ASES, VAS, and Single Assessment Numeric Evaluation scores from baseline to 1 or 2 years postoperatively between the cohorts. Bean et al4 only noted significant differences between cohorts for VAS scores at 2 weeks postoperatively (P = .0441).
Table V.
Patient-reported outcomes for outpatient TSA/rTSA patient.
| SANE | ||||||
|---|---|---|---|---|---|---|
| F/U | Preoperative SANE | Postoperative SANE | Postoperative SANE | |||
| Erickson et al., 201912 |
1 y 2 y |
30.0 ± 19.4 (P = .668) |
74.2 ± 22.3 (P = .954) |
75.8 ± 23.9 (P=.961) |
||
| ASES | ||||||
| F/U |
Preoperative ASES |
Postoperative ASES |
Postoperative ASES |
|||
| Erickson et al., 201912 | 1 y 2 y |
36.3 ± 17.6 (P =.046) | 77.6 ± 18.3 (P = .158) | 78.9 ± 19.6 (P = .0392) | ||
| Bean et al., 20184 |
NA |
33.6 ± 13.3 (P = .4401) |
- |
- |
||
| VAS | ||||||
| F/U |
Preoperative VAS |
Postoperative VAS |
Postoperative VAS |
Postoperative VAS |
||
| Erickson et al., 201912 | 1 y 2 y |
5.8 ± 2.6 (P = .135) | 1.7 ± 2.2 (P = .154) | 1.68 ± 2.3 (P = .108) | - | |
| Bean et al., 20184 |
2 weeks 6 weeks 3 mo |
6.0 (range: 2.0 to 10.0) (P = .2517) |
3.0 (range: 0.0 to 9.0) (P = .0441) |
2.0 (range: 0.0 to 9.0) (P = .5153) |
2.0 (range: 0.0 to 6.0) (P = .1999) |
|
| VR-12 | ||||||
| F/U |
Preoperative VR-12 |
|||||
| Bean et al., 20184 | NA | |||||
| VR-12 M | 54.0 ± 11.9 (P = .9130) | |||||
| VR-12 P | 34.3 ± 10.7 (P = .6245) | |||||
ASES, American Shoulder and Elbow Surgeons assessment; F/U, follow-up; SANE, single assessment numeric evaluation; VAS, visual analog scale; VR-12, Veteran RAND 12 item health survey.
All P values refer to comparisons between inpatient and outpatient scores.
Bias assessment
Results of the MINORS criteria for each study are illustrated in Table VI. The three case series had a total score of 11 of 16 (Fournier et al16), 9 of 16 (Charles et al8) and 10 of 16 (Leroux et al23). In contrast, the cohort studies all had a total score of 16 of 24 (Nwankwo et al,12 Erickson et al,12 Bean et al,4 and Kramer et al22).
Table VI.
MINORS assessment for each included study. Assessment was performed independently by two authors. Any disagreements were resolved by consensus.
| Clearly states aim | Consecutive patients | Prospective collection | Relevant end points | Unbiased assessment | Appropriate follow-up period | Loss to follow-up < 5% | Power analysis | Comparative studies |
Total | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adequate control group | Contemporary groups | Baseline equivalence | Adequate statistical analysis | ||||||||||
| Fournier et al., 201916 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 1 | NA | NA | NA | NA | 11 |
| Charles et al., 20198 | 2 | 2 | 1 | 2 | 0 | 2 | 0 | 0 | NA | NA | NA | NA | 9 |
| Nwankwo et al., 201826 | 2 | 2 | 1 | 2 | 0 | 2 | 0 | 0 | 2 | 2 | 1 | 2 | 16 |
| Erickson et al., 201912 | 2 | 2 | 1 | 2 | 0 | 2 | 0 | 0 | 2 | 2 | 1 | 2 | 16 |
| Leroux et al., 201823 | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 0 | NA | NA | NA | NA | 10 |
| Bean et al., 20184 | 2 | 2 | 1 | 2 | 0 | 2 | 0 | 0 | 2 | 2 | 1 | 2 | 16 |
| Kramer et al., 201822 | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 16 |
Discussion
The most important finding of this investigation was that outpatient TSA and rTSA had a relatively low 90-day complication rate, comparable with inpatient complication rates. This review complied data from TSA and rTSA procedures in more than 900 patients performed by multiple surgeons across a variety of clinical settings including institution-owned hospitals and ambulatory surgery centers. Our findings support the idea that TSA is successful in the outpatient setting without compromising outcomes when compared with inpatient counterparts.
A 90-day complication rate was reported by 6 of 7 studies and ranged from 7.1%-11.5%.4,8,16,22,23,26 In the literature, short-term complication rates after inpatient TSA vary from 2.8%-9.4% depending on complication definition and follow-up time period.2,7,13,36 Of the studies included in this review, many of the most common complications, including hematoma, nerve palsy, and wound issues, are likely independent of discharge timing and more consequence of the procedure, regardless of the surgery setting. Further study is necessary to fully understand this relationship. Kramer et al22 only tracked venous thromboembolism and deep infection; however, because of the rarity of these events, the authors were not able to perform an adjusted analysis between inpatient and outpatient procedures.3 Erickson et al12 found that complications were significantly more frequent in patients undergoing rTSA as inpatients vs. as outpatients. Expectedly, death was a rare complication of outpatient TSA, with Nwankwo et al26 reporting 1 death at the 90-day follow-up from aortic dissection, which was deemed unrelated to the index TSA. Erickson et al12 reported 1 death from myocardial infarction at the 2-year follow-up and Kramer et al22 found 1.2% 1-year mortality after outpatient TSA, comparable with the inpatient TSA cohort (1.1%) and likely related to underlying comorbidities.
Reoperation rate was low or 0 in all studies that measured this outcome. Erickson et al12 was the only study that reported reoperation for mechanical issues such as instability and loosening but measured this outcome at 2 years postoperatively rather than 90 days as in the other studies. Ninety-day readmission rates were also low, ranging from 0 to 3.7%. Three of the 4 recorded readmissions were for medical issues, whereas most readmissions came from the cohort reported by Erickson et al,12 where the reason for readmission was not available. Furthermore, readmission and reoperation after outpatient TSA were equivalent to or lower than inpatient procedures. In addition, it is unclear how far these readmissions occurred and would likely have been no different in the inpatient setting as many patients are discharged by postoperative day 1 or 2.
All studies included in this review cited proper patient screening as an important factor in selecting patients suitable for outpatient TSA. Patient selection was noted as a significant influencer of low complication, readmission, and reoperation rate after these procedures. Patient selection is often more stringent for outpatient cohorts than inpatient, which can account for lower rates of readmission, reoperation, and complications. In the hip and knee arthroplasty literature, careful patient selection, multidisciplinary care coordination, multimodal pain control strategies, and patient education have been consistently noted to be essential for optimizing outcomes and avoiding complications after outpatient procedures.3,17,28 Inpatient cohorts undergoing TKA/THA have been shown to have higher rates of medical comorbidities such as diabetes, obesity, and congestive heart failure. Older patients and those with greater comorbidities were shown to have a higher chance of being readmitted after primary TKA.9,10 Historically, TSA has been shown to have shorter hospital stays, fewer readmissions, and lower rates of complications such as pulmonary embolism and mortality than TKA and THA.13,15 Following the model of successful transition to outpatient TKA and THA, it is reasonable to expect similar or better success in TSA.
The ideal risk assessment tool for patient selection for outpatient TSA has yet to be identified. The ASA and Charlson comorbidity index have been used previously to identify patients at risk for complications. Age, ASA score, and comorbidity have been shown to be risk factors for complications after shoulder arthroplasty.36 However, the ASA score has not demonstrated validity in selecting appropriate patients for same-day joint arthroplasty.24 While only Bean et al4 explicitly used ASA score < 3 as a criteria in selecting patients, all 4 studies that reported an ASA score had mean of 2.3, with Kramer et al22 reporting only 36.3% of their cohort having ASA score > 3. Five studies used medical comorbidities as selection criteria, and 4 studies incorporated living status and social support as factors in selecting patients. In the largest cohort included in this review by Kramer et al,22 the decision to discharge patients the same day was made by the surgeon and anesthesiologist, and no patients were excluded based on comorbidities alone.
The results from our cohort demonstrate that screening may be effective: patients who underwent outpatient TSA are generally younger and healthier than inpatient cohorts translating into equivalent or improved postoperative outcomes and equivalent or decreased rates of complications, readmissions, and reoperations. However, future study is necessary to develop a formal risk stratification tool to stratify patients most suitable for same-day discharge and those at risk for higher complications who would benefit from an inpatient stay. Fournier et al16 developed a patient selection algorithm for outpatient TSA that stratifies patients based on age and cardiopulmonary comorbidities. Although they found that patients undergoing outpatient TSA as selected by their algorithm have a low rate of complication and no readmissions, there was no comparison with an inpatient cohort. Further investigation is necessary to offer a comparison between these two settings.
Limitations
This study is not without limitations. First, only 7 of 293 unique studies met inclusion criteria, highlighting the general paucity of study on outpatient TSA in the literature. Although the combined sample size was large at 937 patients, 646 of them came from just two cohorts. Furthermore, all studies included were level of evidence III or IV, and accordingly, owing to the limitations of available literature, a meta-analysis was unable to be performed. This made it difficult to facilitate direct comparisons between study cohorts. Furthermore, not all studies reported on comparative outcomes between outpatient and inpatient cohorts, so the sample sizes of these comparisons are considerably smaller than the total pooled cohort. Finally, there was a large variation in the collection and reporting PROs between studies. This lack of standardization yielded general trends but made comparisons difficult.
Conclusion
Outpatient TSA in properly selected patients results in a similar complication rate to inpatient TSA. Further studies are needed to aid in determining proper risk stratification to direct patients to inpatient or outpatient shoulder arthroplasty.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: Michael Fu reports other from Arthroscopy, other from DJ Orthopaedics, other from HSS Journal, outside the submitted work. Nikhil Verma reports other from AOSSM, other from ASES, nonfinancial support from Arthrex, Inc, personal fees and nonfinancial support from Arthroscopy, other from AANA, nonfinancial support from Breg, personal fees from Cymedica, other from Knee, personal fees from Minivasive, personal fees from Omeros, personal fees from Orthospace, nonfinancial support from Ossur, other from SLACK Inc, personal fees and nonfinancial support from Smith & Nephew, personal fees and nonfinancial support from Vindico Medical-Orthopedics Hyperguide, nonfinancial support from Wright Medical Technology, Inc, other from Stryker, other from Relievant MedSystems, personal fees from Medacta USA, Inc, other from Medwest Associates, outside the submitted work. Adam Yanke reports personal fees from CONMED Linvatec, personal fees from JRF Ortho, personal fees from Olympus, grants from Organogenesis, nonfinancial support and other from Patient IQ, nonfinancial support from Smith & Nephew, nonfinancial support from Sparta Biomedical, grants from Vericel, grants from Arthrex, Inc., outside the submitted work.
Footnotes
This study was performed at Rush University Medical Center.
Institutional review board approval was not required for this systematic review.
References
- 1.Anakwenze O.A., O’Donnell E.A., Jobin C.M., Levine W.N., Ahmad C.S. Medical Complications and Outcomes After Total Shoulder Arthroplasty: A Nationwide Analysis. Am J Orthop. 2018;47 doi: 10.12788/ajo.2018.0086. [DOI] [PubMed] [Google Scholar]
- 2.Anthony C.A., Westermann R.W., Gao Y., Pugely A.J., Wolf B.R., Hettrich C.M. What Are Risk Factors for 30-day Morbidity and Transfusion in Total Shoulder Arthroplasty? A Review of 1922 Cases. Clin Orthop Relat Res. 2014;473:2099–2105. doi: 10.1007/s11999-014-4107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayalon O., Liu S., Flics S., Cahill J., Juliano K., Cornell C.N. A multimodal clinical pathway can reduce length of stay after total knee arthroplasty. Hss J Musculoskelet J Hosp Special Surg. 2010;7:9–15. doi: 10.1007/s11420-010-9164-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bean B.A., Connor P.M., Schiffern S.C., Hamid N. Outpatient Shoulder Arthroplasty at an Ambulatory Surgery Center Using a Multimodal Pain Management Approach. Jaaos Global Res Rev. 2018;2:e064. doi: 10.5435/jaaosglobal-d-18-00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biron D.R., Sinha I., Kleiner J.E., Aluthge D.P., Goodman A.D., Sarkar I.N. A Novel Machine Learning Model Developed to Assist in Patient Selection for Outpatient Total Shoulder Arthroplasty. J Am Acad Orthop Surg. 2019;28:e580–e585. doi: 10.5435/jaaos-d-19-00395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brolin T.J., Mulligan R.P., Azar F.M., Throckmorton T.W. Neer Award 2016: Outpatient total shoulder arthroplasty in an ambulatory surgery center is a safe alternative to inpatient total shoulder arthroplasty in a hospital: a matched cohort study. J Shoulder Elb Surg. 2017;26:204–208. doi: 10.1016/j.jse.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Chalmers P.N., Gupta A.K., Rahman Z., Bruce B., Romeo A.A., Nicholson G.P. Predictors of Early Complications of Total Shoulder Arthroplasty. J Arthroplast. 2014;29:856–860. doi: 10.1016/j.arth.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Charles M.D., Cvetanovich G., Sumner-Parilla S., Nicholson G.P., Verma N., Romeo A.A. Outpatient shoulder arthroplasty: outcomes, complications, and readmissions in 2 outpatient settings. J Shoulder Elb Surg. 2019;28:S118–S123. doi: 10.1016/j.jse.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 9.Cram P., Lu X., Kaboli P.J., Vaughan-Sarrazin M.S., Cai X., Wolf B.R. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991-2008. Jama. 2011;305:1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cram P., Lu X., Kates S.L., Singh J.A., Li Y., Wolf B.R. Total Knee Arthroplasty Volume, Utilization, and Outcomes Among Medicare Beneficiaries, 1991-2010. Jama. 2012;308:1227. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunn J.C., Lanzi J., Kusnezov N., Bader J., Waterman B.R., Belmont P.J. Predictors of length of stay after elective total shoulder arthroplasty in the United States. J Shoulder Elb Surg. 2015;24:754–759. doi: 10.1016/j.jse.2014.11.042. [DOI] [PubMed] [Google Scholar]
- 12.Erickson B.J., Shishani Y., Jones S., Sinclair T., Griffin J., Romeo A.A. Outpatient vs. inpatient reverse total shoulder arthroplasty: outcomes and complications. J Shoulder Elb Surg. 2020;29:1115–1120. doi: 10.1016/j.jse.2019.10.023. [DOI] [PubMed] [Google Scholar]
- 13.Farmer K.W., Hammond J.W., Queale W.S., Keyurapan E., McFarland E.G. Shoulder Arthroplasty versus Hip and Knee Arthroplasties. Clin Orthop Relat R. 2007;455:183–189. doi: 10.1097/01.blo.0000238839.26423.8d. [DOI] [PubMed] [Google Scholar]
- 14.Farng E., Zingmond D., Krenek L., Soohoo N.F. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elb Surg Am Shoulder Elb Surg Et Al. 2011;20:557–563. doi: 10.1016/j.jse.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Fehringer E.V., Mikuls T.R., Michaud K.D., Henderson W.G., O’Dell J.R. Shoulder Arthroplasties have Fewer Complications than Hip or Knee Arthroplasties in US Veterans. Clin Orthop Relat Res. 2009;468:717–722. doi: 10.1007/s11999-009-0996-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fournier M.N., Brolin T.J., Azar F.M., Stephens R., Throckmorton T.W. Identifying appropriate candidates for ambulatory outpatient shoulder arthroplasty: validation of a patient selection algorithm. J Shoulder Elb Surg. 2019;28:65–70. doi: 10.1016/j.jse.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 17.Hoffmann J.D., Kusnezov N.A., Dunn J.C., Zarkadis N.J., Goodman G.P., Berger R.A. The Shift to Same-Day Outpatient Joint Arthroplasty: A Systematic Review. J Arthroplast. 2017;33:1265–1274. doi: 10.1016/j.arth.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 18.Jaibaji M., Volpin A., Haddad F.S., Konan S. Is Outpatient Arthroplasty Safe? A Systematic Review. J Arthroplast. 2020;35:1941–1949. doi: 10.1016/j.arth.2020.02.022. [DOI] [PubMed] [Google Scholar]
- 19.Jiang J.J., Toor A.S., Shi L.L., Koh J.L. Analysis of perioperative complications in patients after total shoulder arthroplasty and reverse total shoulder arthroplasty. J Shoulder Elb Surg. 2014;23:1852–1859. doi: 10.1016/j.jse.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Kim S.H., Wise B.L., Zhang Y., Szabo R.M. Increasing Incidence of Shoulder Arthroplasty in the United States. J Bone Jt Surgery-american. 2011;93:2249–2254. doi: 10.2106/jbjs.j.01994. [DOI] [PubMed] [Google Scholar]
- 21.Kolz J.M., Aibinder W.R., Adams R.A., Cofield R.H., Sperling J.W. Symptomatic Thromboembolic Complications After Shoulder Arthroplasty: An Update. J Bone Jt Surg Am Volume. 2019;101:1845–1851. doi: 10.2106/jbjs.18.01200. [DOI] [PubMed] [Google Scholar]
- 22.Kramer J.D., Chan P.H., Prentice H.A., Hatch J., Dillon M.T., Navarro R.A. Same-day discharge is not inferior to longer length of in-hospital stay for 90-day readmissions following shoulder arthroplasty. J Shoulder Elb Surg. 2020;29:898–905. doi: 10.1016/j.jse.2019.09.037. [DOI] [PubMed] [Google Scholar]
- 23.Leroux T.S., Zuke W.A., Saltzman B.M., Go B., Verma N.N., Romeo A.A. Safety and patient satisfaction of outpatient shoulder arthroplasty. Jses Open Access. 2018;2:13–17. doi: 10.1016/j.jses.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meneghini R.M., Ziemba-Davis M., Ishmael M.K., Kuzma A.L., Caccavallo P. Safe Selection of Outpatient Joint Arthroplasty Patients With Medical Risk Stratification: the “Outpatient Arthroplasty Risk Assessment Score”. J Arthroplast. 2017;32:2325–2331. doi: 10.1016/j.arth.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 25.Nelson C.G., Murphy W.G., Mulligan R.P., Brolin T.J., Azar F.M., Throckmorton T.W. A retrospective comparative study of patient satisfaction following ambulatory outpatient and inpatient total shoulder arthroplasty. Curr Orthop Pract. 2019;30:435–438. doi: 10.1097/bco.0000000000000787. [DOI] [Google Scholar]
- 26.Nwankwo C.D., Dutton P., Merriman J.A., Gajudo G., Gill K., Hatch J. Outpatient Total Shoulder Arthroplasty Does Not Increase the 90-Day Risk of Complications Compared With Inpatient Surgery in Prescreened Patients. Orthopedics. 2018;41:e563–e568. doi: 10.3928/01477447-20180524-04. [DOI] [PubMed] [Google Scholar]
- 27.Padegimas E.M., Maltenfort M., Lazarus M.D., Ramsey M.L., Williams G.R., Namdari S. Future Patient Demand for Shoulder Arthroplasty by Younger Patients: National Projections. Clin Orthop Relat Res. 2015;473:1860–1867. doi: 10.1007/s11999-015-4231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters C.L., Shirley B., Erickson J. The Effect of a New Multimodal Perioperative Anesthetic Regimen on Postoperative Pain, Side Effects, Rehabilitation, and Length of Hospital Stay After Total Joint Arthroplasty. J Arthroplast. 2006;21:132–138. doi: 10.1016/j.arth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 29.Pollock M., Somerville L., Firth A., Lanting B. Outpatient Total Hip Arthroplasty, Total Knee Arthroplasty, and Unicompartmental Knee Arthroplasty. Jbjs Rev. 2016;4:1. doi: 10.2106/jbjs.rvw.16.00002. [DOI] [PubMed] [Google Scholar]
- 30.Qin C., Curtis D.M., Reider B., Shi L.L., Lee M.J., Athiviraham A. Orthopaedic Shoulder Surgery in the Ambulatory Surgical Center: Safety and Outcomes. Arthrosc J Arthrosc Relat Surg. 2019;35:2545–2550.e1. doi: 10.1016/j.arthro.2019.03.031. [DOI] [PubMed] [Google Scholar]
- 31.Singh J.A., Ramachandran R. Age-related differences in the use of total shoulder arthroplasty over time: use and outcomes. Bone Jt J. 2015;97-B:1385–1389. doi: 10.1302/0301-620x.97b10.35696. [DOI] [PubMed] [Google Scholar]
- 32.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. Anz J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 33.Streubel P.N., Simone J.P., Sperling J.W., Cofield R. Thirty and Ninety-Day Reoperation Rates After Shoulder Arthroplasty. J Bone Jt Surg. 2014;96:e17. doi: 10.2106/jbjs.m.00127. [DOI] [PubMed] [Google Scholar]
- 34.Trofa D., Rajaee S.S., Smith E.L. Nationwide trends in total shoulder arthroplasty and hemiarthroplasty for osteoarthritis. Am J Orthop (Belle Mead NJ) 2014;43:166–172. [PubMed] [Google Scholar]
- 35.Walters J.D., Walsh R.N., Smith R.A., Brolin T.J., Azar F.M., Throckmorton T.W. Bundled Payment Plans Are Associated With Notable Cost Savings for Ambulatory Outpatient Total Shoulder Arthroplasty. J Am Acad Orthop Surg. 2019;28:795–801. doi: 10.5435/jaaos-d-19-00441. [DOI] [PubMed] [Google Scholar]
- 36.Waterman B.R., Dunn J.C., Bader J., Urrea L., Schoenfeld A.J., Belmont P.J. Thirty-day morbidity and mortality after elective total shoulder arthroplasty: patient-based and surgical risk factors. J Shoulder Elb Surg. 2015;24:24–30. doi: 10.1016/j.jse.2014.05.016. [DOI] [PubMed] [Google Scholar]