Abstract
Background
The ulnar collateral ligament (UCL) complex of the elbow plays a primary role in valgus and posteromedial stability of the elbow. The anterior oblique ligament (AOL) of the UCL is believed to provide the majority of resistance to external forces on the medial elbow. The transverse ligament (TL) of the UCL is generally thought to have minimal contribution to the elbow’s overall stability. However, recent studies have suggested a more significant role for the TL. The primary aim of this study was to identify the TL’s contribution to the stability of the elbow joint in determining the joint stiffness and neutral zone variation in internal rotation.
Methods
Twelve cadaveric elbows, set at a 90° flexion angle, were tested by applying an internal rotational force on the humerus to generate a medial opening torque at the level of the elbow. The specimens were preconditioned with 10 cycles of humeral internal rotation with sinusoidal torque ranging from 0 to 5 Nm. Elbow stiffness measures and joint neutral zone were first evaluated in its integrity during a final ramp loading. The test was subsequently repeated after cutting the TL at 33%, 66%, and 100% followed by the AOL in the same fashion.
Results
The native UCL complex joint stiffness to internal rotation measured 1.52 ± 0.51 Nm/°. The first observable change occurred with 33% sectioning of the AOL, with further sectioning of the AOL minimizing the joint stiffness to 1.26 ± 0.32 Nm/° (P = .004). A 33% resection of the TL found an initial neutral zone variation of 0.376 ± 0.23° that increased to 0.771 ± 0.41° (P < .01) at full resection. These values were marginal when compared with the full resection of the AOL for which we have found 3.69 ± 1.65° (P < .01).
Conclusion
The TL had no contribution to internal rotation elbow joint stiffness at a flexion angle of 90°. However, sequential sectioning of the TL was found to significantly increase the joint neutral zone when compared with the native cadaveric elbow at a flexion angle of 90°. This provides evidence toward the TL having some form of contribution to the elbow’s overall stability.
Keywords: Ulnar collateral ligament, Transverse ligament, Anterior oblique ligament, Cadaver, Biomechanics
The ulnar collateral ligament (UCL) complex is located on the medial side of the elbow and is composed of three ligamentous bundles: the anterior oblique ligament (AOL), the posterior oblique ligament (POL), and the transverse ligament (TL).22 The AOL and POL originate from the medial epicondyle of the humerus and insert onto the sublime tubercle of the medial coronoid process and the medial border olecranon of the ulna, respectively.17 The TL bridges the AOL and the POL, originating from the olecranon process and inserting onto the coronoid process.23 Each of these ligamentous bundles have been described to have individual contributions to the overall function of the UCL complex as the primary static stabilizer of the medial elbow.10,30
Injuries to the UCL complex are most commonly seen with athletes competing in overhead throwing sports, such as baseball pitchers or javelin throwers.6,38 This is owing to the large, repetitive tensile forces applied to the UCL complex from the acceleration phase of the throwing motion.2,34 UCL injuries can also occur from a traumatic fall onto an outstretched arm, resulting in high amounts of valgus and rotatory stress.43 Patients with UCL injuries typically present with medial-sided elbow pain, ulnar nerve paresthesia, or an occasional locking or clicking sensation in the joint.26,28,33 In most cases, conservative management is the first line of treatment. However, depending on the patient’s requirements or if they were to fail nonoperative treatment, surgical management may be indicated.11
No specific surgical technique or graft choice has been shown to be a consistently superior choice for the treatment of UCL injuries.16 Although, typically, these surgeries aim to reconstruct or repair the AOL alone.29 There is also no standard for measuring the objective success after undergoing UCL surgery.15 These inconsistencies may explain the variable postoperative clinical outcomes, with studies showing 68-93% of cases having good to excellent results.35 Postoperative rehabilitation time after undergoing surgery for UCL injuries has also been reported to be variable, with some cases ranging from 11.5 to 20.5 months.9
The AOL is the thickest of the three ligaments, and it acts as the primary stabilizer of the medial elbow by providing significant resistance to valgus stress and prevents humeroulnar distraction.19 The AOL is composed of an anterior band, which is taught between 0 and 60° of flexion, and a posterior band, which is taught between 90 and 120° of flexion.6,24 Both of these structures function as coprimary restraints between 60 and 90°, allowing for the AOL to provide support throughout the range of elbow flexion.22 The elbow especially requires extra support at 90°, where it has been shown to have the highest degree of instability.4,10 Further studies have demonstrated there is maximum ulnohumeral gapping with the elbow flexed at 90° when only the AOL is transected.31,40 The AOL also shows maximum lengthening at 90°, when both the anterior and posterior bands of the AOL are functioning together.5,22 The POL mostly plays a secondary support role for the AOL during higher degrees of flexion,41 although it has recently been shown to play a larger role in rotatory instability.21
It was previously accepted in the orthopedic community that the TL plays little, if any, role in medial elbow stability owing to its anatomic position being limited to the ulna.10 A study from 1985 by Morrey and An30 has previously stated that the ligament itself is poorly developed and not differentiable from the joint capsule. Other authors have also reported that it was not consistently present.4 However, more recent studies, using computed tomography-based 3-dimensional renderings5 and advanced mapping techniques, have been able to reliably locate the TL underneath the connective tissue covering the ulnar nerve and the aponeurosis of the flexor-pronator mass as well-demarcated fibers bridging the insertions of the AOL and POL.3,5,23 In addition, this has led to the assumption of a more important role in medial elbow stability for the TL because it has been found with a broad soft-tissue insertion onto the AOL, which could result in a reinforcement of the AOL’s connection to the POL. However, the same studies indicated the need of further biomechanical investigation to provide any significance to this observation.5,23
Because of its broad insertion onto the AOL, injury to the TL may lead to an overall decrease in function of the AOL, which would ultimately cause an increase in elbow joint laxity (Camp et al, 2018). In facts, clinical outcome data from surgical reconstruction or repair of the AOL alone have not been found to guarantee a 100% return to prior function.15
In the present study, we aim to identify the TL’s mechanical contribution to the stability of the elbow joint. More specifically, we want to identify the role of the UCL bundles in determining joint stiffness and neutral zone in internal rotation. We hypothesize that at a flexion angle of 90°, where the elbow has the highest degree of instability,10 the TL does not contribute to the medial elbow stiffness but influences the joint neutral zone.
Materials and methods
Specimen preparation
This study was conducted using twelve fresh frozen human cadaveric elbows (71.8 ± 19.8 years of age). The male-to-female ratio was 11:1. All specimens were preserved in cold storage at −10°C before retrieval and thawed at room temperature for dissection. Each cadaveric extremity was then transversely transected 15 cm proximally and distally from the tip of the olecranon process using a hand saw. Next, a standard medial approach to the elbow was carried out until the UCL was encountered. All surrounding superficial soft tissues were removed to clearly define the UCL complex, in addition to the joint capsule and lateral collateral ligament complex. Special care was taken to isolate and detach the common flexor-pronator mass to avoid disturbing the UCL complex. Finally, the humerus and forearm of each specimen were fixed into a steel pot using an acrylic resin (Bondo, 3M).
Mechanical testing
After preparations were completed, the specimens were connected to the rotational actuator of an Instron 8874 biaxial testing system through a custom-made fixture. The humerus was connected to the rotational actuator, while the forearm was attached to a mobile stage mounted on the Instron Frame.39 The frame allowed the forearm to move freely on the horizontal plane and rotate around the radioulnar axis (see Fig. 1). Following a previously validated protocol for mechanical testing of the elbow joint at 90° flexion, specimens were first preconditioned with 10 cycles of humeral internal rotation with a cycling load following a sinusoidal function ranging from 0 to 5 Nm.27 Medial elbow stability was then evaluated during the final ramp loading using joint stiffness and incremental neutral zone measurements. Joint stiffness was defined for our purposes as the slope of the reaction torque-rotation curve approximated using a linear function within the values of 0.5 to 5 Nm.25 Relative to the intact control configuration, joint neutral zone variation was defined as the rotational angular deviation observed at a minimum reaction load of 0.5 Nm14 to determine any descrete changes that would not be seen in clinical evaluations. To obtain control values, testing was first conducted on the specimens with intact UCL bundles. The loading sequence was then repeated after sequentially sectioning the TL at 33%, 66%, and 100% along its midsection. Partial sectioning of the TL was performed by first differentiating the ligamentous fibers and identifying the boundaries of the ligament as it has been previously described.37 Its width was then measured with a caliper and transected as per this value. The sectioned portion of the TL and the load-displacement curve were monitored throughout the loading process for any damage and drops in reaction loads; in addition, specimens were inspected between each cycle for any visible damage. Measurements were taken after the joint was fully destabilized by sequentially sectioning the TL.
Figure 1.
Cadaveric elbow specimen constrained to the mechanical testing machine using a custom made fixture. An internal rotational torque is applied to the humerus from the apparatus while being able to freely rotate around a medio-lateral axis. The radioulnar complex has valgus constraints while being able to freely rotate around the ulnar axis and move in the horizontal plane.
Statistical analysis
Progressive stiffness reduction and neutral zone increments were evaluated for means using paired T-tests between sequential resections, using a significance level of 0.05.37 All statistical analyses were performed using Microsoft Excel (Microsoft, Redmond, WA, USA).
Results
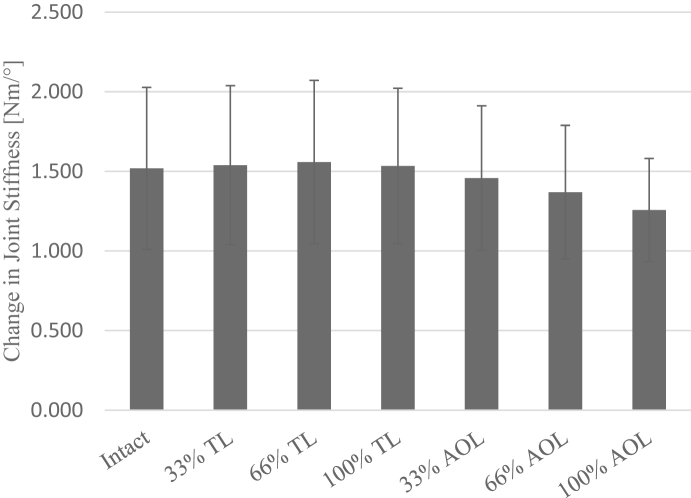
The native UCL complex joint stiffness to internal rotation measured 1.52 ± 0.51 Nm/° as the elbow was loaded from 0.5 to 5 Nm of internal rotational torque. Each sequential sectioning of the TL yielded no changes to the joint stiffness (P > .05, refer to Fig. 2). The first significant decrease in joint stiffness was observed when the AOL was sectioned at 33%, resulting in a value of 1.46 ± 0.45 Nm/° (P = .02). Joint stiffness progressively decreased to 1.37 ± 0.42 Nm/° with 66% sectioning of the AOL, until the complete sectioning of both bundles minimized the joint stiffness to 1.26 ± 0.32 Nm/° (P = .004).
Figure 2.
Mean elbow joint stiffness with successive sectioning of the TL and AOL under medial internal rotatory toque. AOL, anterior oblique ligament; TL, transverse ligament.
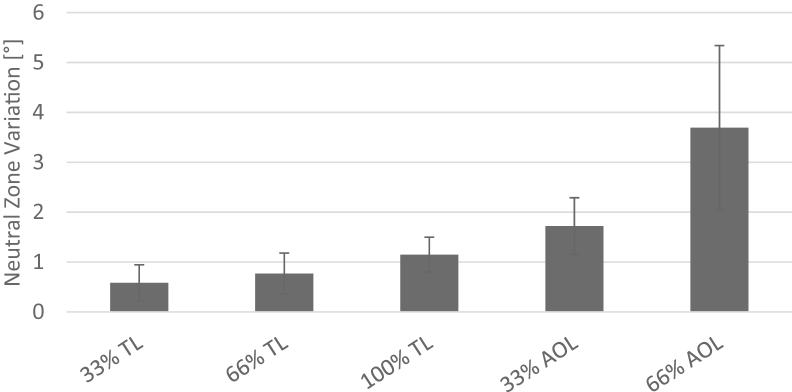
With each level of sectioning for the TL and the AOL, significant changes to the joint neutral zone (P ≤ .01) were observed (refer to Fig. 3). The joint neutral zone was initially measured to be 0.38 ± 0.23° after a 33% sectioning of the TL. Further sequential sectioning of the TL resulted in a progressive increase to 0.59 ± 0.36° at 66% and 0.77 ± 0.41° at 100% (P < .01). The results from successive sectioning of the AOL had larger incremental changes to the joint neutral zone compared with the TL. The joint neutral zone increased to 1.15 ± 0.35° and 1.72 ± 0.57° with sectioning of the AOL at 33% and 66%, respectively (P ≤ .01). Complete sectioning of the AOL resulted in the largest incremental increase to 3.69 ± 1.65° (P = .01).
Figure 3.
Mean neutral zone variation of sectioned TL and AOL compared with intact specimen. AOL, anterior oblique ligament; TL, transverse ligament.
Discussion
The TL is known to form a bridge between the distal insertions of the AOL and the POL on the ulna, and in previous studies, its role on elbow stability was thought to be negligible.4,30 However, more recent studies have brought new attention on the TL,24 and it has been suggested that the TL has a more significant contribution toward the elbow’s stability than what was previously thought.5,23 This study was designed to identify the biomechanical role of injury to the TL in elbow joint stability in internal rotation. We have found that the variation in stiffness from progressive sectioning of the TL is marginal compared with the contribution given by sectioning of the AOL. This reinforces the concept of the AOL’s role as the primary stabilizer of the medial elbow,19 as well as expresses the TL’s minimal role in contributing to the elbow’s stiffness.24 However, we have also found that progressive sectioning of the TL produces a significant increase to the joint’s neutral zone. The amplitude of the increases we found might be considered small, but it provides evidence toward the TL having contribution to the elbow’s overall stability. The small increases to the neutral zone variation observed at the reaction load of 0.5 Nm, used as the reference in this study, should be considered an indicator of any clinically relevant elbow instability that may develop during a throwing athlete’s motion, which has been reported to be as high as 64 Nm.34
Surgical reconstruction of the UCL after injury was first described by Jobe in 1974, and it has gradually evolved since then with many improvements and variations.29 Many of the evolutions to Jobe’s techniques have focused primarily on reconstruction of the AOL owing to its primary role in medial elbow stability.12 As a consequence of this, as well as its previously accepted minimalistic role, the TL is generally not evaluated with UCL injuries,32 and there are no indications for its reconstruction found in previous literature. Based on the findings of this study, reconstruction of the AOL alone can result in a return to normal joint stiffness, but the medial elbow joint’s neutral zone remains significantly increased with an applied stress due to an unaddressed injury to the TL. It has been reported that the recovery time for pitchers to return to competition level after undergoing UCL reconstruction ranges from 11.5 to 20.5 months.9 In addition, findings have shown that increased elbow laxity can cause the overestimation of apparent shoulder external rotation during physical examination, adding unnecessary rehabilitation time.27 Postoperative elbow instability also requires additional rehabilitation time to develop appropriate muscle strength, so that normal stability can be reestablished.13 Based on the observed influence of the TL on the elbow’s neutral zone found in our study, its reconstruction alongside the AOL may be able to decrease total elbow instability and ultimately shorten the length of postoperational rehabilitation time. Frangiamore et al19 performed partial sectioning of the AOL at different locations on the ligament using 2.5 and 5 Nm internal rotational torque on cadaveric elbows with flexion angles of 70°, 90°, and 120°. Their findings show that there was a decrease in joint stiffness regardless of the location of the cut or flexion angle, with a maximum normalized average of 31 ± 12% decrease to joint stiffness at all flexion angles after a posterior distal transection of the AOL. These findings correspond with our results on joint stiffness after partial sectioning of the AOL at 90°, while also having a similar maximum percentile decrease after we completely sectioned the AOL (29 ± 13%). Another study that performed complete sectioning sequences on the UCL complex of an elbow flexed at 70° found an increase to ulnohumeral joint gapping with the release of both of the AOL and the TL under valgus stress. Their results also showed that the release of the AOL provides a greater increase than the release of the TL.7 These findings have a similar trend to our results in regards to the joint’s neutral zone variation at a different flexion angle and testing load.
There are some limitations present in this study. The biggest limitation is from the dissections performed to visualize the UCL bundles of the specimens. Removal of the surrounding soft tissues compromises any secondary stabilizers, such as the flexor-pronator mass.20 This limitation is inherent to any cadaveric study; however our dissections were performed similar to other authors’ techniques, and we were careful during the dissections to create uniform specimens to evaluate medial elbow stability.1,8,19,20,23,37,38 Another limitation to our study is the joint flexion angle of 90° used during the testing procedures. Different flexion angles may produce different numerical results, but it must be considered that the flexion angle used in our present study was chosen because it is the flexion angle at which the highest degree of instability occurs, which would allow for better sensitivity in our results.10 A third limitation comes from our ability to create partial sectioning of the ligaments to mimic the physiological conditions of UCL injuries. We defined the boundaries of each ligament of the UCL complex to minimize any subjectivity in the lengths of our sectioning. However, it is not possible to perfectly reproduce the physiological tearing present in most cases of UCL injuries. Despite this limitation, partial sectioning of the ligaments allowed us to better appreciate variations in biomechanical behavior compared with complete transections found in other studies.7,36 As an additional limitation, our specimens had age of 71.8 ± 19.8 years, which would not accurately reflect young throwing athletes between the ages of 15 and 24 years, who more commonly sustain UCL injuries.42 However, it is of comparable age with other cadaveric studies involving UCL injuries that used specimens with average ages ranging from 69 ± 6.5 to 77 ± 1.3 years.18,37,38
Conclusion
In this study, the TL was found to have no contribution to internal rotation elbow joint stiffness at a flexion angle of 90°. However, sequential sectioning of the TL was found to significantly increase the joint neutral zone when compared with the native cadaveric elbow at a flexion angle of 90°. While further biomechanical and clinical studies are needed to precisely quantify the effects of TL repair or reconstruction in addition to AOL surgery in the setting of UCL injuries. The present study provides evidence toward the TL having contribution to the elbow’s overall stability.
Disclaimers:
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The study was supported by the Biomechanics Laboratory of LSUH-S.
Footnotes
Approved by the LSUHSC-Shreveport Institutional Revie Board (IRB ID: STUDY00001385).
References
- 1.Ahmad C.S., Lee T.Q., ElAttrache N.S. Biomechanical Evaluation of a New Ulnar Collateral Ligament Reconstruction Technique with Interference Screw Fixation. Am J Sports Med. 2003;31:332–337. doi: 10.1177/03635465030310030201. [DOI] [PubMed] [Google Scholar]
- 2.Azar F.M., Andrews J.R., Wilk K.E., Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28:16–23. doi: 10.1177/03635465000280011401. [DOI] [PubMed] [Google Scholar]
- 3.Beckett K.S., McConnell P., Lagopoulos M., Newman R.J. Variations in the normal anatomy of the collateral ligaments of the human elbow joint. J Anat. 2000;197:507–511. doi: 10.1046/j.1469-7580.2000.19730507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callaway G.H., Field L.D., Deng X.H., Torzilli P.A., O’Brien S.J., Altchek D.W. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223–1231. doi: 10.2106/00004623-199708000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Camp C.L., Jahandar H., Sinatro A.M., Imhauser C.W., Altchek D.W., Dines J.S. Quantitative anatomic analysis of the medial ulnar collateral ligament complex of the elbow. Orthop J Sport Med. 2018;6:1–9. doi: 10.1177/2325967118762751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen F.S., Rokito A.S., Jobe F.W. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9:99–113. doi: 10.5435/00124635-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Ciccotti M.C., Hammoud S., Dodson C.C., Cohen S.B., Nazarian L.N., Ciccotti M.G. Stress ultrasound evaluation of medial elbow instability in a cadaveric model. Am J Sports Med. 2014;42:2463–2469. doi: 10.1177/0363546514542805. [DOI] [PubMed] [Google Scholar]
- 8.Cohen S.B., Woods D.P., Siegler S., Dodson C.C., Namani R., Ciccotti M.G. Biomechanical comparison of graft fixation at 30° and 90° of elbow flexion for ulnar collateral ligament reconstruction by the docking technique. J Shoulder Elbow Surg. 2015;24:265–272. doi: 10.1016/j.jse.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Coughlin R.P., Gohal C., Horner N.S., Shanmugaraj A., Simunovic N., Cadet E.R. Return to play and in-game performance statistics among pitchers after ulnar collateral ligament reconstruction of the elbow: a systematic review. Am J Sports Med. 2019;47:2003–2010. doi: 10.1177/0363546518798768. [DOI] [PubMed] [Google Scholar]
- 10.de Haan J., Schep N.W.L., Eygendaal D., Kleinrensink G.-J., Tuinebreijer W.E., den Hartog D. Stability of the elbow joint: relevant anatomy and clinical implications of in vitro biomechanical studies. Open Orthop J. 2011;5:168–176. doi: 10.2174/1874325001105010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dines J.S., ElAttrache N.S. Morrey’s The Elbow and Its Disorders. Elsevier; 2009. Articular Injuries in the Athlete; pp. 680–696. [DOI] [Google Scholar]
- 12.Dugas J.R. Ulnar collateral ligament repair: an old idea with a new wrinkle. Am J Orthop (Belle Mead NJ) 2016;45:124–127. [PubMed] [Google Scholar]
- 13.Dunning C.E., Zarzour Z.D.S., Patterson S.D., Johnson J.A., King G.J.W. Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clin Orthop Relat Res. 2001;388:118–124. doi: 10.1097/00003086-200107000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Ellwein A., Füßler L., Ferle M., Smith T., Lill H., Pastor M.F. Suture tape augmentation of the lateral ulnar collateral ligament increases load to failure in simulated posterolateral rotatory instability. Knee Surg Sports Traumatol Arthrosc. 2021;29:284–291. doi: 10.1007/s00167-020-05918-5. [DOI] [PubMed] [Google Scholar]
- 15.Erickson B.J., Gupta A.K., Harris J.D., Bush-Joseph C., Bach B.R., Abrams G.D. Rate of return to pitching and performance after Tommy John surgery in major league baseball pitchers. Am J Sports Med. 2014;42:536–543. doi: 10.1177/0363546513510890. [DOI] [PubMed] [Google Scholar]
- 16.Erickson B.J., Harris J.D., Chalmers P.N., Bach B.R., Verma N.N., Bush-Joseph C.A. Ulnar collateral ligament reconstruction: anatomy, indications, techniques, and outcomes. Sports Health. 2015;7:511–517. doi: 10.1177/1941738115607208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eygendaal D., Olsen B.S., Jensen S.L., Seki A., Söjbjerg J.O. Kinematics of partial and total ruptures of the medial collateral ligament of the elbow. J Shoulder Elbow Surg. 1999;8:612–616. doi: 10.1016/s1058-2746(99)90099-x. [DOI] [PubMed] [Google Scholar]
- 18.Frangiamore S.J., Bigart K., Nagle T., Colbrunn R., Millis A., Schickendantz M.S. Biomechanical analysis of elbow medial ulnar collateral ligament tear location and its effect on rotational stability. J Shoulder Elbow Surg. 2018;27:2068–2076. doi: 10.1016/j.jse.2018.05.020. [DOI] [PubMed] [Google Scholar]
- 19.Frangiamore S.J., Moatshe G., Kruckeberg B.M., Civitarese D.M., Muckenhirn K.J., Chahla J. Qualitative and quantitative analyses of the dynamic and static stabilizers of the medial elbow: an anatomic study. Am J Sports Med. 2018;46:687–694. doi: 10.1177/0363546517743749. [DOI] [PubMed] [Google Scholar]
- 20.Golan E.J., Shukla D.R., Nasser P., Hausman M. Isolated ligamentous injury can cause posteromedial elbow instability: a cadaveric study. J Shoulder Elbow Surg. 2016;25:2019–2024. doi: 10.1016/j.jse.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 21.Karademir G., Bachman D.R., Stylianou A.P., Cil A. Posteromedial rotatory incongruity of the elbow: a computational kinematics study. J Shoulder Elbow Surg. 2019;28:371–380. doi: 10.1016/j.jse.2018.07.030. [DOI] [PubMed] [Google Scholar]
- 22.Karbach L.E., Elfar J. Elbow instability: anatomy, biomechanics, diagnostic maneuvers, and testing. J Hand Surg Am. 2017;42:118–126. doi: 10.1016/j.jhsa.2016.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kimata K., Yasui M., Yokota H., Hirai S., Naito M., Nakano T. Transverse ligament of the elbow joint: an anatomic study of cadavers. J Shoulder Elbow Surg. 2019;28:2253–2258. doi: 10.1016/j.jse.2019.04.048. [DOI] [PubMed] [Google Scholar]
- 24.Labott J.R., Aibinder W.R., Dines J.S., Camp C.L. Understanding the medial ulnar collateral ligament of the elbow: review of native ligament anatomy and function. World J Orthop. 2018;9:78–84. doi: 10.5312/wjo.v9.i6.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Massey P., Parker D., McClary K., Robinson J., Barton R.S., Solitro G.F. Biomechanical comparison of anterior cruciate ligament repair with internal brace augmentation versus anterior cruciate ligament repair without augmentation. Clin Biomech. 2020;77:105065. doi: 10.1016/j.clinbiomech.2020.105065. [DOI] [PubMed] [Google Scholar]
- 26.Mehta J.A., Bain G.I. Posterolateral rotatory instability of the elbow. J Am Acad Orthop Surg. 2004;12:405–415. doi: 10.5435/00124635-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Minata T., Safran M.R., McGarry M.H., Abe M., Lee T.Q. Elbow valgus laxity may result in an overestimation of apparent shoulder external rotation during physical examination. Am J Sports Med. 2008;36:978–982. doi: 10.1177/0363546507313086. [DOI] [PubMed] [Google Scholar]
- 28.Mitchell C., Cain E.L., Andrews J.R. Ulnar collateral ligament injuries of the elbow. Curr Orthop Pract. 2008;19:596–601. doi: 10.1097/BCO.0b013e3283060ebb. [DOI] [Google Scholar]
- 29.Moore A.R., Fleisig G.S., Dugas J.R. Ulnar collateral ligament repair. Orthop Clin North Am. 2019;50:383–389. doi: 10.1016/j.ocl.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Morrey B.F., An K.-N.N. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985:84–90. [PubMed] [Google Scholar]
- 31.Mullen D.J., Goradia V.K., Parks B.G., Matthews L.S. A biomechanical study of stability of the elbow to valgus stress before and after reconstruction of the medial collateral ligament. J Shoulder Elbow Surg. 2002;11:259–264. doi: 10.1067/MSE.2002.122622. [DOI] [PubMed] [Google Scholar]
- 32.Nathan B.H., Bucchieri J.S., Shon F., Miller T.T., Rosenwasser M.P. Magnetic resonance imaging of injury to the medial collateral ligament of the elbow: a cadaver model. J Shoulder Elbow Surg. 2000;9:418–422. doi: 10.1067/mse.2000.107392. [DOI] [PubMed] [Google Scholar]
- 33.Pearce McCarty L. Approach to medial elbow pain in the throwing athlete. Curr Rev Musculoskelet Med. 2019;12:30–40. doi: 10.1007/s12178-019-09534-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raducha J.E., Gil J.A., Harris A.P., Owens B.D. Ulnar collateral ligament injuries of the elbow in the throwing athlete. JBJS Rev. 2018;6:e1. doi: 10.2106/JBJS.RVW.17.00061. [DOI] [PubMed] [Google Scholar]
- 35.Rahman R.K., Levine W.N., Ahmad C.S. Elbow medial collateral ligament injuries. Curr Rev Musculoskelet Med. 2008;1:197–204. doi: 10.1007/s12178-008-9026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sard A., Dutto E., Rotini R., Vanni S., Pastorelli S., Battiston B. The posterior bundle of the elbow medial collateral ligament: biomechanical study and proposal for a new reconstruction surgical technique. Musculoskelet Surg. 2017;101(Suppl 2):181–186. doi: 10.1007/s12306-017-0495-7. [DOI] [PubMed] [Google Scholar]
- 37.Shukla D.R., Golan E., Nasser P., Culbertson M., Hausman M. Importance of the posterior bundle of the medial ulnar collateral ligament. J Shoulder Elbow Surg. 2016;25:1868–1873. doi: 10.1016/j.jse.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 38.Singh R., Sharma K., Singla M. Morphometry of ulnar collateral ligament and its role in kinematics of elbow. Basic Sci Med. 2019;8:18–21. doi: 10.5923/j.medicine.20190801.03. [DOI] [Google Scholar]
- 39.Smidt K., Fattori R., Barton R.S., Morandi M., Ogden A., Solitro G.F. Role of the Transverse Ligament of the Ulnar Collateral Ligament Complex in Posteromedial Elbow Instability [Abstract] ORS 2020 Annu Meet. 2020:45. [Google Scholar]
- 40.Wigton M.D., Schimoler P.J., Kharlamov A., Miller M.C., Frank D.A., DeMeo P.J. The moving valgus stress test produces more ulnar collateral ligament change in length during extension than during flexion: a biomechanical study. J Shoulder Elbow Surg. 2020:1–6. doi: 10.1016/j.jse.2019.12.025. [DOI] [PubMed] [Google Scholar]
- 41.Willemot L., Hendrikx F.R., Byrne A.M., van Riet R.P. Valgus instability of the elbow: acute and chronic form. Obere Extrem. 2018;13:173–179. doi: 10.1007/s11678-018-0465-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zaremski J.L., McClelland J.A., Vincent H.K., Horodyski M.B. Trends in sports-related elbow ulnar collateral ligament injuries. Orthop J Sport Med. 2017;5:1–7. doi: 10.1177/2325967117731296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang L., Wang L., Yu S., Lv Z., Zhang P., Fan C. Severe traumatic valgus instability of the elbow: pathoanatomy and outcomes of primary operation. J Orthop Surg Res. 2019;14:347. doi: 10.1186/s13018-019-1374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]