Youth and young adults (YYAs) with type 1 diabetes do not consistently meet A1C targets set forth by national and international guidelines (1,2). Diabetes care is further compromised for YYAs because they are at high risk of failure to transition from a pediatric to an adult endocrinologist (1,3). Additionally, people from minority racial/ethnic groups have poorer A1C, increased diabetes complications, and worse diabetes-related outcomes compared with those from nonminority groups (4–6). Youth from lower socioeconomic backgrounds have poorer diabetes-specific outcomes compared with those of higher socioeconomic backgrounds (7). Unfortunately, consistent with the medical field at large, research in type 1 diabetes consistently underrepresents YYAs of low socioeconomic status (SES) and racial/ethnic minority groups (8). Contributing factors to the disparities in A1C and type 1 diabetes–specific outcomes remain largely unexplored.
It is known that barriers to diabetes care such as cost, communication issues, and low health literacy affect diabetes-related health outcomes and the quality of care delivered (9). Psychosocial factors have long been associated with glycemic outcomes, quality of life, and self-care behaviors such as self-monitoring of blood glucose (SMBG) (10). Specifically, diabetes distress, general anxiety, depression, and generalized distress have been associated with poor type 1 diabetes–related outcomes (10). Furthermore, poor psychosocial states are associated with decreased SMBG and diabetes-related self-care behaviors (11).
Although well-being has been linked to positive general health outcomes in healthy young adult populations (12), little is known about the relationship between global well-being and diabetes-related outcomes. In addition, minority populations are underrepresented in the literature with regard to the impact of psychosocial factors and global well-being on diabetes-specific outcomes. Evaluating and addressing psychosocial determinants of diabetes-specific health may be important in the management of type 1 diabetes for YYAs from minority groups (1,13), and recognizing and addressing barriers may be vital for optimal delivery of care to YYAs with type 1 diabetes.
This study aimed to evaluate the relationships between self-reported psychosocial measures (global well-being, perceived stress, diabetes distress, and barriers to diabetes care) and diabetes outcomes (A1C and SMBG) in minority YYAs with type 1 diabetes receiving care at a major urban safety net medical center. We hypothesized that higher self-perceived well-being and lower perceived stress, diabetes distress, and barriers would be associated with lower A1C and higher frequency of SMBG among YYAs with type 1 diabetes of low SES and from racial/ethnic minority groups.
Research Design and Methods
Study Overview
We performed a cross-sectional study of objective and subjective measures collected at a single clinic visit at the Los Angeles County + University of Southern California (LAC + USC) Medical Center’s type 1 diabetes clinics, which predominantly serve patients who are uninsured or qualify for Medicaid. Written informed consent, or parental permission and youth assent where appropriate, was obtained before data collection. The study was approved by the University of Southern California institutional review board, and all study activities were carried out in accordance with the Declaration of Helsinki.
Participants
We recruited patients aged 13–30 years with type 1 diabetes to participate in the study between April and October 2016. All people with English literacy seen by the LAC + USC pediatric diabetes and diabetes transitional care clinics were eligible for the study. Surveys were only completed by the YYAs and not by their parents/guardians. Forty-seven eligible participants were approached, and all consented to participate in the study. Four participants were subsequently unable to complete the surveys, and their data were excluded from the analysis.
Variables
Demographic data, including sex, age, and race/ethnicity, were collected from a review of participants’ electronic health record (EHR). A1C was measured at the time of clinic visit using the DCA 2000 analyzer (Bayer, Tarrytown, NY). For 35 participants, glucose meter data were available and downloaded at the time of clinic visit to determine the frequency of SMBG. BMI (or BMI z score for patients <18 years of age) and diabetes duration were collected from participants’ EHR.
Psychosocial Study Measures
The study measures included three previously validated psychosocial measures addressing well-being, stress, and diabetes distress. A fourth measure was developed for the purposes of this study with methods outlined below.
The Arizona Integrative Outcomes Scale (AIOS) (12) measures global well-being using a single validated item that asks participants to consider the past month in responding to a prompt reflecting on their sense of well-being and marking their response on a 100-point visual analog scale. Higher scores indicated higher well-being.
The Diabetes Distress Scale-2 (DSS-2) (14,15) is a validated two-item Likert scale questionnaire specifically addressing the perception of stress caused by diabetes management. Each item in the DDS-2 is scored from 1 to 6, with higher scores indicative of greater distress. A summed total score of ≥6 or any single response ≥3 warrants further evaluation.
The Perceived Stress Scale-4 (PSS-4) (16) is a validated four-item Likert scale questionnaire aimed at evaluating a person’s perceptions of general life stress over the preceding month. Each item in the PPS-4 is scored from 0 to 4, for a total summed score range of 0 to 16, with higher scores indicative of greater stress. Normative values are 6.9 ± 2.9 for people <18 years of age and 6.7 ± 3.2 for those 18–29 years of age (16).
The Barrier Burden Scale (BBS) was developed specifically for this study. Current surveys on barriers to care are long and often difficult to administer in real-world practice. Therefore, we developed a brief four-question Likert assessment based on barriers reported in the literature (17) and including 1) logistics (supplies, appointments, medication), 2) diabetes education, 3) providers’ cultural competency, and 4) poor personal relationship with type 1 diabetes (Supplementary Table S1). Responses from each barrier domain were summed to create a Barrier Burden Scale-Sum (BBS-Sum).
We used cognitive testing and retrospective probing, which are evidence-based methods to evaluate the fidelity of survey measures, to ensure the reliability of the novel BBS (18,19). Consistent with cognitive testing, we solicited input from pediatric endocrinologists and individuals living with type 1 diabetes after development of the survey items to assess whether the questions satisfied the intended purposes. After the further refinement of survey items based on this feedback, we tested the scale with five participants, who completed the measure and then explained their interpretation of each question. This method was consistent with and founded in the principles of retrospective probing. Items did not require revision based on responses from the participants; therefore, these five participants were included in the analysis. After the data were collected, we sought to establish concurrent validity via correlation analyses with previously validated measures (the AIOS, DDS-2, and PPS-4).
Delivery of Study Measures
Participants completed the four measures on a digital tablet during the wait time for their clinic visits. The measures required ∼10 minutes to complete. Measures were collected and managed using REDCap, hosted at the University of Southern California (20,21). Once a participant completed the measures, results and clinically meaningful cutoffs were given to the provider scheduled to see the participant. The provider incorporated the findings from the measures into the clinic visit to the degree felt to be clinically appropriate.
Data Analysis
Linear regression was used to analyze the associations between objective data (A1C and SMBG) and the four self-reported measures. In a second step, a multivariate linear regression model controlling for age, sex, race/ethnicity, BMI, and diabetes duration was also carried out. Correlation testing among the four measures was performed using Pearson's correlation coefficient to evaluate concurrent validity of measures in this population and of our novel BSS. All statistical analyses were performed using R statistical computing software, v. 3 (22).
Results
Study Population
Participants’ age range was 14–29 years, and the majority of our cohort (n = 34, 79%) identified as Hispanic White (Table 1). For the validated measures, mean survey scores were in the normative ranges expected from prior reports (12,14–16). One-third of participants did endorse negative feelings toward diabetes as having a significant impact on their diabetes care. (See descriptive statistics in Supplementary Table S2A and free-text responses in Supplementary Table S2B).
TABLE 1.
Participant Demographics and Characteristics (N = 43)
| Male sex | 24 (55) |
| Age, years | 21.0 ± 3.7 |
| <18 | 10 (23) |
| 18–20 | 9 (21) |
| 21–29 | 24 (56) |
| Race/ethnicity | |
| Latinx | 34 (79) |
| Non-Hispanic Black | 4 (9) |
| Asian | 2 (5) |
| Non-Hispanic White | 2 (5) |
| Other | 1 (2) |
| BMI range | |
| Normal* | 21 (49) |
| Overweight† | 15 (35) |
| Obese‡ | 7 (16) |
| Type 1 diabetes duration, years | 10.1 ± 6.2 |
| A1C, % | 9.3 ± 2.3 |
| SMBG checks per day§ | 2.0 ± 1.3 |
| AIOS score | 66.4 ± 22 |
| PSS-4 score | 5.8 ± 3.0 |
| DDS-2 score | 5.4 ± 2.5 |
| BBS score | 2.2 ± 2.0 |
Data are n (%) or mean ± SD.
Normal BMI is defined as BMI ≤25 kg/m2 or BMI z score ≤1.04.
Overweight is defined as BMI 25–30 kg/m2 or BMI z score 1.04–1.96.
Obese is defined as BMI ≥30 kg/m2 or BMI z score ≥1.96.
SMBG data were only available for 35 participants.
Relationship of Psychosocial Survey Measures and Diabetes Outcomes
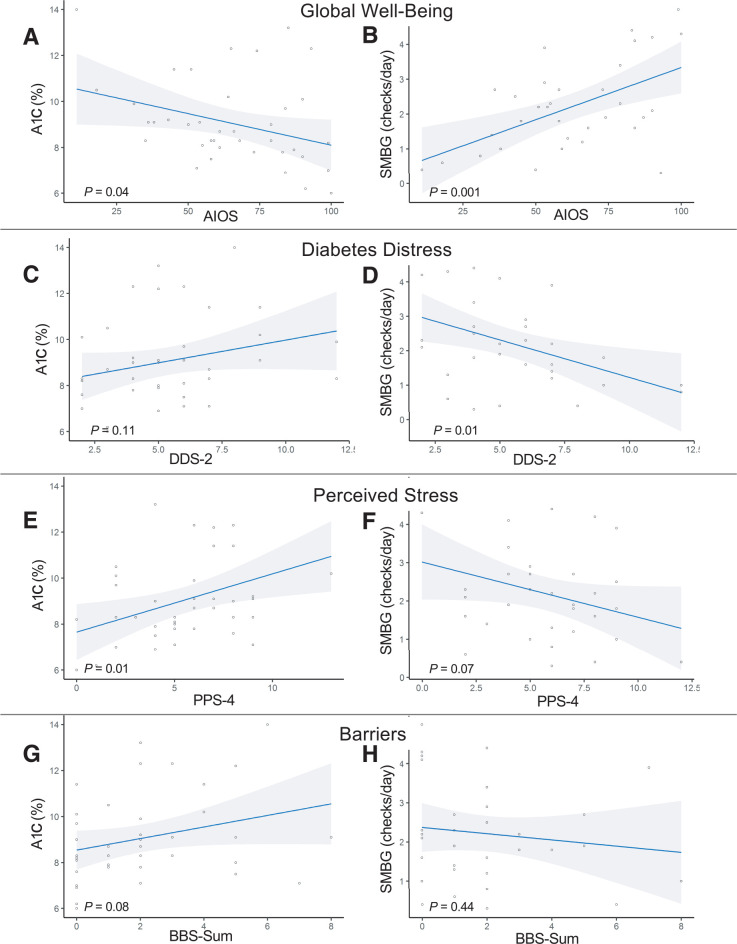
Results of the linear regression between the psychosocial measures and diabetes outcomes (A1C and SMBG) are shown in Figure 1 and Table 2. Global well-being (AIOS) was inversely correlated with A1C (β = −0.03 [95% CI −0.05 to 0], R2 = 0.11, P = 0.04) and positively correlated with SMBG (β = 0.03 [95% CI 0.01–0.05], R2 = 0.30, P = 0.001). An increase in the AIOS scale of 17 points corresponds to a decrease in A1C of 0.5%, and an increase of 33 points corresponds with an increase of one SMBG check per day. Self-reported diabetes distress (DDS-2) was inversely correlated with SMBG (β = −0.22 [95% CI −0.38 to −0.06], R2 = 0.19, P = 0.01); thus, a decrease in 4.5 points on the DDS-2 corresponds to an increase of one SMBG check per day. Perceived stress (PSS-4) was positively correlated with A1C (β = 0.25 [95% CI 0.06–0.44], R2 = 0.16, P = 0.01); thus, a reduction of PSS-4 by 2 points was associated with a decrease of 0.5% in A1C. Multivariate regression analysis was also performed but demonstrated no meaningful or statistically significant contributions of the variables evaluated (Supplementary Table S3).
FIGURE 1.
Relationship of psychosocial measures with A1C and SMBG. Blue lines are lines of best fit, shaded gray areas represent 95% CIs. Individual data points are represented by open circles. The relationship between AIOS and A1C and SMBG are depicted in panels A and B, respectively. The relationship between DDS-2 and A1C and SMBG are depicted in panels C and D, respectively. The relationship between PPS-4 and A1C and SMBG are depicted in panels E and F, respectively. The relationship between BBS-Sum and A1C and SMBG are depicted in panels G and H, respectively.
TABLE 2.
Univariate Relationships Between Psychosocial Measures and A1C and SMBG
| Measure | β (95% CI) | R2 | P |
|---|---|---|---|
| A1C | |||
| AIOS | −0.03 (−0.05 to 0) | 0.11 | 0.04 |
| DDS-2 | 0.12 (−0.05 to 0.44) | 0.07 | 0.11 |
| PSS-4 | 0.25 (0.06–0.44) | 0.16 | 0.01 |
| BBS-Sum | 0.25 (−0.03 to 0.53) | 0.08 | 0.08 |
| SMBG | |||
| AIOS | 0.03 (0.01–0.05) | 0.30 | 0.001 |
| DDS-2 | −0.22 (−0.38 to −0.06) | 0.19 | 0.01 |
| PSS-4 | −0.14 (−0.30 to 0.01) | 0.10 | 0.07 |
| BBS-Sum | −0.08 (−0.23 to 0.13) | 0.02 | 0.44 |
Correlation Between Measures
There was a strong relationship among the four survey measures, which speaks to concurrent validity in our results. Global well-being (AIOS) was strongly and inversely correlated with general stress (PSS-4: r = −0.44, P = 0.003) and diabetes-specific measures (DDS-2: r = −0.52, P <0.001; BBS-Sum: r = −0.40, P = 0.008). The newly developed BBS-Sum was strongly correlated with DDS-2 (r = 0.45, P = 0.002) and PSS-4 (r = 0.59, P <0.001). Finally, diabetes distress and general stress were strongly correlated (r = 0.48, P = 0.001).
Discussion
We report significant associations between self-reported survey measures (AIOS, PSS-4, DDS-2, and BBS-Sum) and diabetes clinical outcomes (A1C and SMBG) in 43 YYAs with type 1 diabetes from low SES and racial/ethnic minority backgrounds. Furthermore, we newly demonstrate the clinical usefulness of the AIOS and PSS-4 measures in this underrepresented YYA cohort. These findings are consistent with our hypothesis: higher well-being and lower diabetes distress and stress are associated with improved type 1 diabetes outcomes in this population.
Notably, our medical center primarily serves a low SES and Latinx population of transition age, for whom there are few data previously reported for these relationships. Prior studies evaluating psychosocial factors in type 1 diabetes have focused on youth or adults, and less commonly YYAs of transition age, but have not consistently included individuals with low SES or racial/ethnic minority status (10,13,23,24). Additionally, incorporating a measure to evaluate global health is exceedingly rare. Our findings support evaluation of psychosocial measures as one strategy to bridge disparities in diabetes health outcomes while promoting transition of care in YYAs.
The AIOS scale, a broad evaluation of a person’s health, demonstrated robust correlations with A1C and SMBG. Further studies are needed to explore whether clinically meaningful changes in A1C can be mediated through improvements in global well-being. The AIOS has also been used in the fields of integrative medicine (25,26), chronic pain (27), and educational interventions for type 1 diabetes (28–30). The AIOS is the only assessment of positive psychosocial state (well-being) in our study, whereas the other three measures assess negative psychosocial states (distress, stress, and barriers); it thus raises the question of the potential superiority of positive psychosocial measurements in underrepresented populations. Although our population has unique racial/ethnic and socioeconomic backgrounds with barriers specific to and outside of diabetes care (31–34), we anticipate that all people with type 1 diabetes would benefit from a simple scale that assesses well-being. The AIOS is such a tool; it is simple, readily available, and allows patients to consider the many needs that allow for optimal health, including type 1 diabetes management.
In our novel BBS, the most frequently reported barrier was negative feelings toward one’s own diabetes. It is telling that even in a resource-poor setting, negative feelings are still perceived to be the largest barrier. Given that attitude and perception of type 1 diabetes is a modifiable factor, providers can aim to assess and address a person’s relationship with their type 1 diabetes to affect diabetes outcomes. The BBS may be a tool to facilitate transition of care. Although the BBS was not validated via quantitative methods such as principal component analysis, we were able to establish fidelity of the measure with cognitive testing and retrospective probing, as well as the concurrent validity supportive of this measure.
We report that higher DDS-2 scores were associated with decreased SMBG, consistent with prior publications (14,15,35). YYAs of lower SES with type 1 diabetes often have public insurance, which has more strict requirements for diabetes supply coverage, including minimum number of glucose checks per day (34,36,37). Therefore, insurance requirements to maintain coverage for diabetes supplies may be one explanation of this correlation between DDS-2 and SMBG. Further studies are needed to systematically understand the driving factors behind this relationship in this low SES population.
Both the DDS-2 and the PSS-4 are associated with adverse effects on A1C and increased rates of diabetes-related complications, including severe hypoglycemia and diabetic ketoacidosis (16,17). The PSS-4 was correlated with A1C and has been used in patients with type 2 diabetes (38), obesity (39), working adults, pregnant/postpartum women, college students, patients with metal health disorders, and patients with cardiac disorders (40), but to our knowledge, it has not been used in type 1 diabetes. We demonstrate the clinical relevance of the PSS-4 in low SES YYAs with type 1 diabetes. Our results support further evaluation to better understand the impact of general stress versus diabetes-specific distress on type 1 diabetes outcomes in YYAs from lower SES populations.
Finally, we have demonstrated the feasibility of psychosocial assessment in an underrepresented population and resource-constrained hospital, thereby meeting psychosocial screening guidelines (1,13). The psychosocial screening strategy we describe can allow diabetes providers to address these important factors during clinical encounters, thereby improving the patient-provider relationship, which in turn is associated with improvement in diabetes management and outcome (41,42) and may be helpful in the successful transition of care. In particular, the clinical utility of AIOS warrants further evaluation as a single question to help stratify patients by risk and allocate resources to YYAs with type 1 diabetes. Furthermore, our population overwhelmingly identifies as Hispanic White; thus, our findings are supportive of expanding the use of previously validated scales in this subgroup.
There are several strengths to this study. The study population included a large proportion of both low SES and predominately Latinx young adult participants and fills an important need for the inclusion of minority populations in research (8). The study was well received by both participants and their treating clinicians, suggesting that our study instruments would incorporate well into clinical practice. Finally, the use of several instruments provided a robust picture of participants’ psychosocial state and perceived barriers, with concurrent validity of measures. Our novel BBS allowed for a brief but complete assessment of self-perceived barriers.
Limitations of the study include a small sample size. Additionally, survey-based studies are often influenced by self-selection bias; we believe our high recruitment rate reduced this effect. The survey format also raised concerns about reporting bias; although this was likely present, we feel that the high correlation between measures affords us some reassurance of concurrent validity. Finally, this is a cross-sectional study, so temporal effects were not discerned. Future longitudinal research is ongoing and may augment these findings.
Conclusion
We report that patient-reported markers of global well-being, diabetes distress, and stress were associated with measurable outcomes of diabetes care. Negative feelings toward diabetes are the most common self-reported barrier to diabetes care in this population of minority YYAs. We demonstrated successful psychosocial screening in a resource-limited urban hospital, and the methods described may facilitate transition of care. We conclude that psychosocial screening is both clinically meaningful and feasible, and therefore, clinics should strive to meet guidelines by screening all people with type 1 diabetes for psychosocial stressors as a means of improving type 1 diabetes care.
Article Information
Acknowledgments
The authors thank Joe Tapias for his work in recruiting the participants and administering the surveys, as well as all of the participants for their time.
Funding
A.A. was supported by the Maternal Child Health Research Institute and by Stanford University’s K12 (K12DK122550).
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
A.A. and M.J.W. conceived, designed, and conducted the study. R.Y.C. contributed to the study design, conducted the analysis, and assisted in the interpretation of the data, along with A.A. and M.J.W. A.A. wrote the first draft of the manuscript with assistance from J.V. All authors reviewed and revised the manuscript with critical contributions. A.A. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
This work was previously presented in a poster abstract form at the American Diabetes Association’s 78th Scientific Sessions in Orlando, FL, 22–26 June 2018.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.13269476.
References
- 1. American Diabetes Association . 13. Children and adolescents: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S163–S182 [DOI] [PubMed] [Google Scholar]
- 2. DiMeglio LA, Acerini CL, Codner E, et al. ISPAD clinical practice consensus guidelines 2018: glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatr Diabetes 2018;19(Suppl. 27):105–114 [DOI] [PubMed] [Google Scholar]
- 3. Daneman D, Nakhla M. Moving on: transition of teens with type 1 diabetes to adult care. Diabetes Spectr 2011;24:14–18 [Google Scholar]
- 4. Willi SM, Miller KM, DiMeglio LA, et al.; T1D Exchange Clinic Network . Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics 2015;135:424–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DeSalvo DJ, Miller KM, Hermann JM, et al.; T1D Exchange and DPV Registries . Continuous glucose monitoring and glycemic control among youth with type 1 diabetes: international comparison from the T1D Exchange and DPV Initiative. Pediatr Diabetes 2018;19:1271–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Miller KM, Beck RW, Foster NC, Maahs DM. HbA1c levels in type 1 diabetes from early childhood to older adults: a deeper dive into the influence of technology and socioeconomic status on HbA1c in the T1D Exchange Clinic Registry findings. Diabetes Technol Ther 2020;22:645–650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Addala A, Auzanneau M, Miller K, et al. A decade of disparities in diabetes technology use and HbA1c in pediatric type 1 diabetes: a transatlantic comparison. Diabetes Care. Epub ahead of print on 16 September 2020 (doi:10.2337/dc20-0257) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. AAP diversity and inclusion statement. Pediatrics 2018;141:e20180193. [DOI] [PubMed] [Google Scholar]
- 9. Valenzuela JM, Seid M, Waitzfelder B, et al.; SEARCH for Diabetes in Youth Study Group . Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr 2014;164:1369–1375.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Diabetes Association . 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S48–S65 [DOI] [PubMed] [Google Scholar]
- 11. Vincze G, Barner JC, Lopez D. Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. Diabetes Educ 2004;30:112–125 [DOI] [PubMed] [Google Scholar]
- 12. Bell IR, Cunningham V, Caspi O, Meek P, Ferro L. Development and validation of a new global well-being outcomes rating scale for integrative medicine research. BMC Complement Altern Med 2004;4:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Delamater AM, de Wit M, McDarby V, et al. ISPAD clinical practice consensus guidelines 2018: psychological care of children and adolescents with type 1 diabetes. Pediatr Diabetes 2018;19(Suppl. 27):237–249 [DOI] [PubMed] [Google Scholar]
- 14. Polonsky WH, Fisher L, Earles J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care 2005;28:626–631 [DOI] [PubMed] [Google Scholar]
- 15. Fisher L, Glasgow RE, Mullan JT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Ann Fam Med 2008;6:246–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Warttig SL, Forshaw MJ, South J, White AK. New, normative, English-sample data for the short form Perceived Stress Scale (PSS-4). J Health Psychol 2013;18:1617–1628 [DOI] [PubMed] [Google Scholar]
- 17. Hilliard ME, Yi-Frazier JP, Hessler D, Butler AM, Anderson BJ, Jaser S. Stress and A1c among people with diabetes across the lifespan. Curr Diab Rep 2016;16:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA, Sage Publications, 2005 [Google Scholar]
- 19. Willis G. Cognitive interviewing in survey design: state of the science and future directions. In The Palgrave Handbook of Survey Research. Vannette DL, Krosnick JA, Eds. Cham, Switzerland, Springer International Publishing, 2018, p. 103–107 [Google Scholar]
- 20. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Minor BL, et al.; REDCap Consortium . The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria, R Foundation for Statistical Computing, 2013 [Google Scholar]
- 23. Iturralde E, Adams RN, Barley RC, et al. Implementation of depression screening and global health assessment in pediatric subspecialty clinics. J Adolesc Health 2017;61:591–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hood KK, Iturralde E, Rausch J, Weissberg-Benchell J. Preventing diabetes distress in adolescents with type 1 diabetes: results 1 year after participation in the STePS Program. Diabetes Care 2018;41:1623–1630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bishop FL, Yardley L, Cooper C, Little P, Lewith G. Predicting adherence to acupuncture appointments for low back pain: a prospective observational study. BMC Complement Altern Med 2017;17:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Grant SJ, Bensoussan A. The process of care in integrative health care settings: a qualitative study of US practices. BMC Complement Altern Med 2014;14:410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nøst TH, Steinsbekk A, Bratås O, Grønning K. Twelve-month effect of chronic pain self-management intervention delivered in an easily accessible primary healthcare service: a randomised controlled trial. BMC Health Serv Res 2018;18:1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Weigensberg MJ, Vigen C, Sequeira P, et al. Diabetes Empowerment Council: integrative pilot intervention for transitioning young adults with type 1 diabetes. Glob Adv Health Med 2018;7:2164956118761808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sequeira PA, Pyatak EA, Weigensberg MJ, et al. Let’s Empower and Prepare (LEAP): evaluation of a structured transition program for young adults with type 1 diabetes. Diabetes Care 2015;38:1412–1419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pyatak EA, Sequeira PA, Vigen CLP, et al. Clinical and psychosocial outcomes of a structured transition program among young adults with type 1 diabetes. J Adolesc Health 2017;60:212–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Institute of Medicine . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C., National Academies Press, 2003 [PubMed] [Google Scholar]
- 32. Agency for Healthcare Research and Quality . Access and Disparities in Access to Health Care. Rockville, MD, Agency for Healthcare Research and Quality, 2015 [Google Scholar]
- 33. Cheng TL, Goodman E; Committee on Pediatric Research . Race, ethnicity, and socioeconomic status in research on child health. Pediatrics 2015;135:e225–e237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zimmerman FJ, Anderson NW. Trends in health equity in the United States by race/ethnicity, sex, and income, 1993–2017. JAMA Netw Open 2019;2:e196386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. van Son J, Nyklíček I, Pop VJ, Pouwer F. Testing the effectiveness of a mindfulness-based intervention to reduce emotional distress in outpatients with diabetes (DiaMind): design of a randomized controlled trial. BMC Public Health 2011;11:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Department of Health Care Services . Continuous glucose monitoring (CGM) as a CCS/GHPP program benefit: revised with attachment. Available from https://www.dhcs.ca.gov/services/ccs/Documents/CCS.NL.14-0818.Continuous.Glucose.Monitoring.pdf. Accessed 20 November 2020
- 37. Prahalad P, Addala A, Buckingham BA, Wilson DM, Maahs DM. Sustained continuous glucose monitor use in low-income youth with type 1 diabetes following insurance coverage supports expansion of continuous glucose monitor coverage for all. Diabetes Technol Ther 2018;20:632–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Singla M, Jain NP, Chaudhry R. Correlation of type 2 diabetes mellitus with perceived stress and family functioning. Diabetologie und Stoffwechsel 2018;13(Suppl. 1):S20–S21 [Google Scholar]
- 39. Lopez-Cepero A, Frisard C, Person S, Ockene I, Tucker K, Rosal M. Change in perceived stress moderates the association between weight change and HbA1c change in Puerto Rican women (P21-035-19). Curr Dev Nutr 2019;3(Suppl. 1):nzz041.P21-035-19 [Google Scholar]
- 40. Lee E-H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (Korean Soc Nurs Sci) 2012;6:121–127 [DOI] [PubMed] [Google Scholar]
- 41. Croom A, Wiebe DJ, Berg CA, et al. Adolescent and parent perceptions of patient-centered communication while managing type 1 diabetes. J Pediatr Psychol 2011;36:206–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Caccavale LJ, Corona R, LaRose JG, Mazzeo SE, Sova AR, Bean MK. Exploring the role of motivational interviewing in adolescent patient-provider communication about type 1 diabetes. Pediatr Diabetes 2019;20:217–225 [DOI] [PMC free article] [PubMed] [Google Scholar]