Abstract
Background
More than one-half of breast cancer cases are diagnosed among women aged younger than 62 years, which may result in employment challenges. This study examined whether cancer-related employment disruption was associated with increased financial hardship in a national US study of women with breast cancer.
Methods
Women with breast cancer who were enrolled in the Sister or Two Sister Studies completed a survivorship survey in 2012. Employment disruption was defined as stopping work completely or working fewer hours after diagnosis. Financial hardship was defined as: 1) experiencing financial problems paying for cancer care, 2) borrowing money or incurring debt, or 3) filing for bankruptcy because of cancer. Prevalence ratios and 95% confidence intervals for the association between employment disruption and financial hardship were estimated using multivariable Poisson regression with robust variance.
Results
We analyzed data from women employed at diagnosis (n = 1628). Women were a median age of 48 years at diagnosis and 5.6 years from diagnosis at survey completion. Overall, 27.3% of women reported employment disruption (15.4% stopped working; 11.9% reduced hours), and 21.0% experienced financial hardship (16.0% had difficulty paying for care; 12.6% borrowed money or incurred debt; 1.8% filed for bankruptcy). In adjusted analysis, employment disruption was associated with nearly twice the prevalence of financial hardship (prevalence ratio = 1.93, 95% confidence interval = 1.58 to 2.35).
Conclusions
Women experiencing employment disruptions after breast cancer may be more vulnerable to financial hardship. Findings highlight the need to target risk factors for employment disruption, facilitate return to work or ongoing employment, and mitigate financial consequences after cancer.
Female breast cancer is the most common cancer in the United States (excluding nonmelanoma skin cancer), with >250 000 cases diagnosed each year and 5-year survival of nearly 90% (1). Therefore, the survivorship concerns of this large and growing population are of critical importance. Changes to employment due to cancer and its treatment can be particularly relevant within this population, because more than one-half of cases are diagnosed among women aged younger than 62 years (2).
Changes in employment status due to cancer have been reported by 30%-42% of cancer survivors in nationally representative surveys (3,4). Cancer survivors as a broad group may have an increased risk of work cessation, with survivors of breast cancer at particularly increased risk compared with healthy controls (pooled relative risk from 10 studies = 1.28, 95% confidence interval [CI] = 1.11 to 1.49) (5). Lost or reduced wages at a time of increased out-of-pocket medical expenditures (6,7) can contribute to financial hardship and consequential poor health outcomes (8-12), including increased mortality (13). However, few studies have directly addressed the specific relation of cancer-related employment disruption to financial hardship.
Given the risks of unemployment after cancer diagnosis and increased health care expenses, this study examined whether cancer-related employment disruption was associated with increased financial hardship among a national US sample of women diagnosed with breast cancer.
Methods
Study Sample
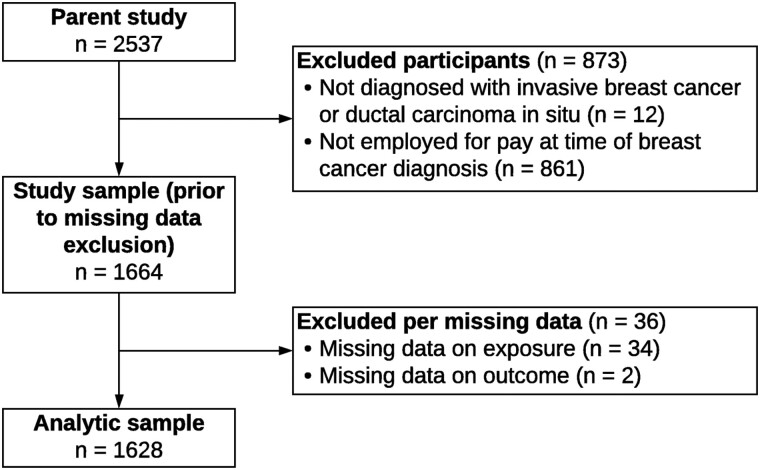
The analytic sample was derived from a survivorship survey conducted in 2012 (Data Release 7.2) among a cohort of women with breast cancer (n = 2537; 90% survey response rate). Women who completed the survey were enrolled in 1 of 2 studies: the Sister Study, a prospective cohort of women aged 35-74 years in the United States without a history of breast cancer at enrollment (2003-2009) but who had a biologic sister with breast cancer and who subsequently developed breast cancer themselves (14); or the Two Sister Study, a sister-matched cohort of women with young-onset breast cancer (aged <50 years at diagnosis) who had a sister enrolled in the Sister Study, with enrollment between 2008 and 2010 (15,16). Recruitment for the Sister Study used multi-faceted strategies to target diverse groups of women, including community-based efforts, media campaigns, and partnerships with national organizations (14). We excluded the following women: those not diagnosed with invasive breast cancer or ductal carcinoma in situ, those not employed for pay at the time of diagnosis, and those with missing data on employment disruption or financial hardship. The final analytic sample consisted of 1628 women (Figure 1). The study was determined to not constitute human patient research and was exempt from institutional review board approval.
Figure 1.
Flow diagram of inclusion into the analytic sample.
Exposure Assessment
Cancer-related employment disruption was derived from multiple items on the survivorship survey and operationalized as a binary indicator. Women who reported that they stopped work completely or reduced work hours were defined as having disrupted employment, including those who 1) reported “there was no provision for time off and I had to quit working” in response to “What kind of time off or leave did your job provide during your treatment and recovery?”; 2) responded “no” to “After your treatment and recovery, did you continue working for pay?”; 3) responded “yes” to “Have you ever had to quit a job or decided to retire early because of your cancer, its treatment, or its lasting effects?”; 4) responded “yes” to “Have you ever been let go, laid off, or fired from a job because of your cancer, its treatment, or its lasting effects?”; or 5) responded working “fewer hours” to “When you returned to work after treatment and recovery, did you typically work.…” Otherwise, women with nonmissing responses to those items were defined as not having disrupted employment.
Outcome Assessment
Financial hardship due to cancer or its treatment was operationalized as a binary response for women who responded “yes” to any of the following 3 items on the survivorship survey: “Have you experienced financial problems or difficulties in paying for your cancer drugs or treatment?”; “Have you or has someone in your family had to borrow money or go into debt because of your cancer, its treatment, or the lasting effects of treatment?”; or “Have you or your family ever had to file for bankruptcy because of your cancer, its treatment, or the lasting effects of treatment?” The latter 2 items were from the Medical Expenditure Panel Survey (MEPS): Experiences with Cancer Survivorship Supplement (17,18). Women who responded “no” to all 3 items were defined as not experiencing financial hardship.
Covariate Assessment
Sociodemographic characteristics were obtained from self-report at the time of study enrollment in the Sister Study or Two Sister Study, including census region of current or primary residence, self-classification of race and ethnicity, highest year or level of school completed, and total household income. Marital or partner status at diagnosis and caregiving for someone else during cancer treatment (“provided care for parents, children, grandchildren, or someone who was ill or disabled while you were receiving care for breast cancer”) were self-reported in the survivorship survey.
Work-related characteristics were self-reported in the survivorship survey, including type of employment at diagnosis (part-time or full-time), employer-provided leave benefits (paid sick leave, other paid time off, unpaid sick leave, Family and Medical Leave Act, or no provision for time off), and health insurance coverage during cancer treatment. Few women (n = 12) reported having no health insurance, so multivariable analysis grouped these women into a “no private health insurance” category, which also included Medicare; Medicaid; military, Tri-Care, Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), or the Veterans Affairs (VA); some other government program; and insurance from somewhere else. All other women were categorized as having “any private health insurance,” which included “a plan through my employer or union”; “a plan through someone else’s employer or union”; and “a plan that you or someone else buys on your own.”
Prediagnosis comorbid conditions were obtained primarily from self-report in baseline and follow-up questionnaires in the Sister and Two Sister Studies. When timing relative to breast cancer diagnosis could be determined, comorbidities from the Charlson Comorbidity Index (19) were included, which were prior cancer other than nonmelanoma skin cancer, diabetes, heart attack, heart failure, and cerebrovascular disease (stroke or transient ischemic attack). Medical record was available for more than 50% of prior cancers; all other conditions or events were self-reported. Cancer clinical characteristics were obtained primarily from medical records, including age at diagnosis (>97% from medical record), years since diagnosis, and stage at diagnosis (>97% from medical record). Cancer treatment (surgery only, radiation with no chemotherapy, or any chemotherapy) from medical record was used as the primary treatment source (available for 73%), with data supplemented from self-report in follow-up questionnaires and the survivorship survey. Time since last surgery, radiation, or chemotherapy was self-reported in the survivorship survey. Cancer-related treatment effects were self-reported in the survivorship survey by response to “Since your breast cancer diagnosis, has a doctor or any other health professional told you that you have [lymphedema, neuropathy, heart disease, osteoporosis]?” All study questionnaires can be accessed on the Sister Study website (15).
Statistical Analysis
Prevalence ratios (PRs) and 95% confidence intervals for the association between employment disruption and financial hardship were estimated using Poisson regression with robust error variance (20). Adjusted analysis included the following covariates, identified a priori as confounders using a directed acyclic graph (21): age at diagnosis (linear); region of residence at study enrollment (Northeast, Midwest, South, West); race or ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic all other races); highest educational attainment (high school degree or GED or less, some college or associate or technical degree, bachelor’s degree or higher); married or in a serious relationship at diagnosis (yes, no); caregiver for someone else during cancer treatment (yes, no); employment status at diagnosis (part-time, full-time); paid leave (did not take leave, took leave but no paid leave provided, took leave and paid leave provided); health insurance during treatment (any private insurance, no private insurance); prediagnosis comorbidities (0, 1+); cancer stage (in situ, stages I-II, stages III-IV); and time since last surgery, radiation, or chemotherapy (currently receiving treatment, <12 months, 1 to <5 years, 5+ years). Cancer treatment was not included due to its strong collinearity with stage.
Modification of the association between employment disruption and financial hardship was assessed a priori in unadjusted analysis for the following covariates: age at diagnosis (<50 years vs ≥50 years), time since last treatment (currently or <12 months vs 1 to <5 years vs ≥5 years), race or ethnicity (non-Hispanic White vs non-Hispanic Black vs Hispanic vs non-Hispanic all other races), employment type (part-time vs full-time), and caregiver for someone else during cancer treatment (yes vs no). Effect measure modification on the multiplicative scale was assessed by examining stratum-specific estimates for the effect of the exposure within strata of the modifier and by using likelihood ratio tests comparing a full model with the interaction term(s) with a main effects model. All analyses were conducted in SAS 9.4 (SAS Institute, Cary, NC), and all tests of statistical significance were 2-sided with a P value less than .05 considered statistically significant.
Sensitivity Analysis
Multiple sensitivity analyses were conducted to assess the robustness of results. First, to assess how type of employment disruption may differentially affect financial hardship, the association between employment disruption and financial hardship was analyzed separately for those who stopped working completely relative to those with no disruption, and for those who reduced hours relative to those with no disruption.
Second, we evaluated inclusion of cancer treatment, rather than cancer stage, in adjusted analysis. Though the variables exhibited strong collinearity—and thus were not both included in the multivariable model—some variability in treatment was present among cancers that were in situ or stages I-II, which could lead to disparate employment and financial outcomes based on treatment itself and its downstream health consequences.
Third, although timing of lymphedema, neuropathy, heart disease, or osteoporosis diagnosis (cancer-related treatment effects) relative to employment disruption could not be determined—and therefore these factors were not considered for inclusion in the final multivariable model—we examined their potential effect as confounders by adjusting for each separate condition (yes, no) in the model.
Fourth, we assessed unmeasured confounding by prediagnosis income; data collected at baseline were only prediagnosis for Sister Study enrollees due to study design. Multivariable analysis adjusting for prediagnosis income (<$50 000, $50 000-$99 999, ≥$100 000) was conducted among Sister Study enrollees with incident breast cancer (n = 702).
Results
Participant Characteristics
In a national US sample of 1628 women with breast cancer who were enrolled in the Sister or Two Sister Studies and employed at diagnosis, women were a median age of 48 years at diagnosis and 5.6 years from diagnosis at survey completion (Tables 1 and 2). Women were primarily non-Hispanic White (88.9%) and highly educated (60.7% with a bachelor’s degree or higher), and many had a high income at enrollment (44.0% reported an annual household income of ≥$100 000). Nearly all women (99.3%) had health insurance at diagnosis and most (97.3%) maintained insurance coverage throughout treatment. Cancer-related employment disruption was reported by 27.3% of women, including 15.4% who stopped working completely and 11.9% who worked fewer hours after diagnosis. Among women who stopped working completely, 18 reported retiring (median age = 62 years).
Table 1.
Sociodemographic characteristics of Sister Study and Two Sister Study participants who were employed at breast cancer diagnosis and completed the Survivorship Survey (n = 1628), overall, and stratified by employment disruption and financial hardship
| Characteristic | Overall, No. (%)a | No employment disruption, No. (%)a | Employment disruption, No. (%)a | No financial hardship, No. (%)a | Financial hardship No. (%)a |
|---|---|---|---|---|---|
| Total No. | 1628 | 1184 | 444 | 1286 | 342 |
| Study | |||||
| Sister Study | 725 (45.5) | 544 (45.9) | 181 (40.8) | 596 (46.3) | 129 (37.7) |
| Two Sister Study | 903 (55.5) | 640 (54.1) | 263 (59.2) | 690 (53.7) | 213 (62.3) |
| Census region of residence at enrollment | |||||
| Northeast | 290 (17.8) | 223 (18.8) | 67 (15.1) | 241 (18.7) | 49 (14.3) |
| Midwest | 506 (31.1) | 371 (31.3) | 135 (30.4) | 405 (31.5) | 101 (29.5) |
| South | 460 (28.3) | 331 (28.0) | 129 (29.1) | 362 (28.1) | 98 (28.7) |
| West | 370 (22.7) | 259 (21.9) | 111 (25.0) | 277 (21.5) | 93 (27.2) |
| Puerto Rico | 2 (0.1) | 0 (0) | 2 (0.5) | 1 (0.1) | 1 (0.3) |
| Race or ethnicity | |||||
| Non-Hispanic White | 1448 (88.9) | 1060 (89.5) | 388 (87.4) | 1158 (90.0) | 290 (84.8) |
| Non-Hispanic Black | 79 (4.9) | 59 (5.0) | 20 (4.5) | 56 (4.4) | 23 (6.7) |
| Hispanic | 57 (3.5) | 40 (3.4) | 17 (3.8) | 41 (3.2) | 16 (4.7) |
| Non-Hispanic all other races | 44 (2.7) | 25 (2.1) | 19 (4.3) | 31 (2.4) | 13 (3.8) |
| Education | |||||
| High school degree or GED or less | 189 (11.6) | 134 (11.3) | 55 (12.4) | 139 (10.8) | 50 (14.6) |
| Some college or associate or technical degree | 451 (27.7) | 324 (27.4) | 127 (28.6) | 336 (26.1) | 115 (33.6) |
| Bachelor’s degree or higher | 988 (60.7) | 726 (61.3) | 262 (59.0) | 811 (63.1) | 177 (51.8) |
| Household income at enrollmentb | |||||
| <$20 000 | 21 (1.3) | 9 (0.8) | 12 (2.8) | 10 (0.8) | 11 (3.3) |
| $20 000-49 999 | 208 (13.1) | 144 (12.5) | 64 (14.8) | 140 (11.2) | 68 (20.2) |
| $50 00-99 999 | 659 (41.5) | 497 (43.1) | 162 (37.4) | 504 (40.3) | 155 (46.0) |
| ≥$100 000 | 699 (44.0) | 504 (43.7) | 195 (45.0) | 596 (47.7.) | 103 (30.6) |
| Missing | 41 (2.5) | 30 (2.5) | 11 (2.5) | 36 (2.8) | 5 (1.5) |
| Marital or partner status at cancer diagnosis | |||||
| Married or in serious relationship | 1355 (83.4) | 980 (83.0) | 375 (84.5) | 1091 (85.0) | 264 (77.4) |
| Not married and not in a serious relationship | 270 (16.6) | 201 (17.0) | 69 (15.5) | 193 (15.0) | 77 (22.6) |
| Missing | 3 (0.2) | 3 (0.3) | 0 (0) | 2 (0.2) | 1 (0.3) |
| Caregiving status during cancer treatment | |||||
| Caregiver for parents, children, grandchildren, or someone who was ill or disabled | 543 (33.4) | 376 (31.8) | 167 (37.6) | 415 (32.3) | 128 (37.5) |
| Not a caregiver | 1084 (66.6) | 807 (68.2) | 277 (62.4) | 871 (67.7) | 213 (62.5) |
| Missing | 1 (0.06) | 1 (0.08) | 0 (0) | 0 (0) | 1 (0.3) |
| Type of employment at diagnosis | |||||
| Part-time | 386 (23.7) | 268 (22.6) | 118 (26.6) | 305 (23.7) | 81 (23.7) |
| Full-time | 1242 (76.3) | 916 (77.4) | 326 (73.4) | 981 (76.3) | 261 (76.3) |
| Leave benefits provided during treatmentc | |||||
| Paid leave | 916 (56.3) | 712 (60.1) | 204 (45.9) | 747 (58.2) | 169 (49.7) |
| Unpaid leave (including FMLA) | 539 (33.1) | 374 (31.6) | 165 (37.2) | 400 (31.2) | 139 (40.9) |
| Did not take at least a week of leave | 274 (16.8) | 237 (20.0) | 37 (8.3) | 226 (17.6) | 48 (14.1) |
| Type of health insurance during treatmentc | |||||
| Private insurance | 1525 (93.9) | 1118 (94.7) | 407 (91.9) | 1206 (93.9) | 319 (93.8) |
| Medicare | 68 (4.2) | 47 (4.0) | 21 (4.7) | 58 (4.5) | 10 (2.9) |
| Medicaid or other government program (includes military, Tri-Care, CHAMPUS, or the VA) | 68 (4.2) | 45 (3.8) | 23 (5.2) | 58 (4.5) | 10 (2.9) |
| Other | 15 (0.9) | 9 (0.8) | 6 (1.4) | 10 (0.8) | 5 (1.5) |
| No insurance | 12 (0.7) | 3 (0.3) | 9 (2.0) | 6 (0.5) | 6 (1.8) |
| Missing | 4 (0.2) | 3 (0.3) | 1 (0.2) | 2 (0.2) | 2 (0.6) |
| Health insurance coverage | |||||
| Covered during entirety of treatment | 1578 (97.3) | 1161 (98.5) | 417 (94.1) | 1267 (98.8) | 311 (91.5) |
| Not covered during at least some part of treatment | 44 (2.7) | 18 (1.5) | 26 (5.9) | 15 (1.2) | 29 (8.5) |
| Missing | 6 (0.4) | 5 (0.4) | 1 (0.2) | 4 (0.3) | 2 (0.6) |
| Prediagnosis comorbiditiesd | |||||
| 1+ comorbid condition | 142 (8.7) | 91 (7.7) | 51 (11.5) | 108 (8.4) | 34 (9.9) |
Nonmissing observations: percentage of nonmissing observations; missing observations: percentage of all observations. CHAMPUS = Civilian Health and Medical Program of the Uniformed Services; FMLA = Family and Medical Leave Act; VA = Veterans Affairs.
Prediagnosis income for Sister Study participants with incident breast cancer and postdiagnosis income for Sister Study participants who were identified as having a diagnosis that preceded enrollment activities, and Two Sister participants.
Categories are not mutually exclusive.
Conditions diagnosed before breast cancer diagnosis, including prior cancer (except for nonmelanoma skin cancer), diabetes, heart attack, heart failure, or stroke.
Table 2.
Cancer diagnosis and treatment characteristics of Sister Study and Two Sister Study participants who were employed at breast cancer diagnosis and completed the Survivorship Survey (n = 1628), overall and by employment disruption and financial hardship
| Characteristic | Overall | No employment disruption | Employment disruption | No financial hardship | Financial hardship |
|---|---|---|---|---|---|
| Total No. | 1628 | 1184 | 444 | 1286 | 342 |
| Median age at cancer diagnosis (IQR), y | 48.2 (9.8) | 48.4 (10.2) | 47.7 (9.4) | 48.5 (10.6) | 46.8 (6.9) |
| Age at cancer diagnosis, No. (%)a | |||||
| 28 to <40 y | 125 (7.7) | 84 (7.1) | 41 (9.2) | 84 (6.5) | 41 (12.0) |
| 40 to <50 y | 943 (57.9) | 679 (57.3) | 264 (59.5) | 738 (57.4) | 205 (59.9) |
| 50 to <60 y | 335 (20.6) | 253 (21.4) | 82 (18.5) | 275 (21.4) | 60 (17.5) |
| 60-80 y | 225 (13.8) | 168 (14.2) | 57 (12.8) | 189 (14.7) | 36 (10.5) |
| Cancer stage, No. (%)a | |||||
| Stage 0 (in situ) | 308 (19.0) | 266 (22.5) | 42 (9.5) | 265 (20.7) | 43 (12.6) |
| Stages I-II | 1,138 (70.1) | 812 (68.8) | 326 (73.4) | 899 (70.1) | 239 (70.1) |
| Stages III-IV | 178 (11.0) | 102 (8.6) | 76 (17.1) | 119 (9.3) | 59 (17.3) |
| Missing | 4 (0.2) | 4 (0.3) | 0 (0) | 3 (0.2) | 1 (0.3) |
| Cancer treatment, No. (%)a | |||||
| Surgery only | 273 (16.8) | 215 (18.2) | 58 (13.1) | 233 (18.1) | 40 (11.7) |
| Radiation with no chemotherapy | 440 (27.0) | 375 (31.7) | 65 (14.6) | 373 (29.0) | 67 (19.6) |
| Any chemotherapy | 913 (56.1) | 593 (50.1) | 320 (72.1) | 679 (52.8) | 234 (68.4) |
| No surgery, radiation, or chemotherapy | 1 (0.06) | 0 (0) | 1 (0.2) | 0 | 1 (0.3) |
| Missing | 1 (0.06) | 1 (0.08) | 0 (0) | 1 (0.08) | 0 (0) |
| Time since last surgery, radiation, or chemotherapy, No. (%)a | |||||
| Currently receiving treatment | 38 (2.4) | 17 (1.5) | 21 (4.8) | 18 (1.4) | 20 (6.0) |
| <12 months | 115 (7.2) | 80 (6.9) | 35 (8.0) | 92 (7.3) | 23 (6.8) |
| 1 to <5 years | 760 (47.4) | 543 (46.6) | 217 (49.4) | 583 (46.0) | 177 (52.7) |
| 5+ years | 690 (43.0) | 524 (45.0) | 166 (37.8) | 574 (45.3) | 116 (34.5) |
| Missing | 25 (1.5) | 20 (1.7) | 5 (1.1) | 19 (1.5) | 6 (1.8) |
| Treatment effects, No. (%)a | |||||
| Yesb | 612 (38.6) | 385 (33.2) | 227 (53.3) | 438 (35.0) | 174 (52.4) |
| Lymphedema | 271 (16.7) | 163 (13.8) | 108 (24.6) | 183 (14.3) | 88 (26.0) |
| Neuropathy | 303 (19.0) | 173 (14.8) | 130 (30.4) | 210 (16.6) | 93 (28.4) |
| Heart disease | 63 (3.9) | 33 (2.8) | 30 (6.9) | 45 (3.5) | 18 (5.3) |
| Osteoporosis | 171 (10.6) | 110 (9.4) | 61 (13.9) | 123 (9.7) | 48 (14.2) |
| No | 972 (61.4) | 773 (66.8) | 199 (46.7) | 814 (65.0) | 158 (47.6) |
| Missing | 44 (2.7) | 26 (2.2) | 18 (4.1) | 34 (2.6) | 10 (2.9) |
Nonmissing observations: percentage of nonmissing observations; missing observations: percentage of all observations. IQR = interquartile range.
Categories are not mutually exclusive.
Financial Hardship
Roughly 1 in 5 women (21.0%) reported some form of financial hardship related to their cancer or its treatment, defined as difficulty paying for cancer drugs or treatment (16.0%), borrowing money or going into debt (12.6%), or filing for bankruptcy (1.8%) (Table 3). Financial hardship differed substantially by employment disruption (36.0% vs 15.4% among women with and without disruption, respectively). After adjustment, cancer-related employment disruption was associated with nearly 2 times the prevalence of financial hardship (PR = 1.93, 95% CI = 1.58 to 2.35) (Table 3).
Table 3.
Adverse financial outcomes due to cancer
| Characteristic | Total No. | Financial hardship, No. (%) | Unadjusted PRa (95% CI) | Adjusted PRa,b (95% CI) |
|---|---|---|---|---|
| Overall | 1628 | 342 (21.0) | ||
| No employment disruption | 1184 | 182 (15.4) | 1 | 1 |
| Employment disruption | 444 | 160 (36.0) | 2.34 (1.95 to 2.81) | 1.93 (1.58 to 2.35) |
| Stratified by race or ethnicity | ||||
| Non-Hispanic White | 1448 | 290 (20.0) | 2.28 (1.87 to 2.79) | 1.91 (1.54 to 2.37) |
| Non-Hispanic Black | 79 | 23 (29.1) | 4.59 (2.36 to 8.94) | 3.14 (1.61 to 6.14) |
| Hispanic | 57 | 16 (28.1) | 1.41 (0.61 to 3.26) | 1.11 (0.46 to 2.70) |
| Non-Hispanic all other races | 44 | 13 (29.5) | 2.11 (0.82 to 5.42) | 1.90 (0.76 to 4.74) |
Comparing women with employment disruption with women without employment disruption. CI = confidence interval; PR = prevalence ratio.
Adjusted for age at diagnosis, region of residence at enrollment, race or ethnicity, education, marital or partner status at diagnosis, caregiving for someone else during treatment, type of employment at diagnosis, paid leave, health insurance during treatment, prediagnosis comorbidities, cancer stage, and time since last surgery, radiation, or chemotherapy. Twelve women who reported no insurance were included with women without private health insurance, with minimal influence on the analysis compared with excluding these women. Excludes women with missing covariate data (n = 42).
Based on unadjusted analysis, race or ethnicity was the only covariate further examined as a modifier in the multivariable model. Stratum-specific estimates by race or ethnicity suggest a stronger association between employment disruption and financial hardship among non-Hispanic Black women (PR = 3.14, 95% CI = 1.61 to 6.14) than among non-Hispanic White women (PR = 1.91, 95% CI = 1.54 to 2.37) and Hispanic women (PR = 1.11, 95% CI = 0.46 to 2.70), though the estimate for non-Hispanic Black women is less precise and its confidence interval overlaps with the estimates for non-Hispanic White and Hispanic women (likelihood ratio test P = .52) (Table 3).
Sensitivity Analysis
Employment disruption as a result of cancer was statistically significantly associated with financial hardship for women who stopped working as well as those who reduced work hours, though the association appeared stronger among women who stopped working (PR = 2.00, 95% CI = 1.59 to 2.52) than among women who reduced work hours (PR = 1.82, 95% CI = 1.42 to 2.35). The effect estimate adjusted for cancer treatment was nearly identical to the effect estimate adjusted for cancer stage. Adjusting for cancer-related treatment effects (lymphedema, neuropathy, heart disease, and osteoporosis) in the fully adjusted model moved the effect estimate slightly closer to the null (decrease of 9% on the log scale; multivariable model without treatment effects: PR = 1.88, 95% CI = 1.54 to 2.31 vs multivariable model with treatment effects: PR = 1.78, 95% CI = 1.45 to 2.19). We assessed the impact of adjustment for prediagnosis income among Sister Study participants with incident breast cancer. Estimates for the association between employment disruption and financial hardship remained substantively similar with and without adjustment for income overall (without income adjustment: PR = 2.12, 95% CI = 1.51 to 2.97 vs with income adjustment: PR = 2.18, 95% CI = 1.56 to 3.06) and within strata of racial or ethnic groups.
Discussion
In a national study of women diagnosed with breast cancer, 27.3% either stopped work altogether or reduced their work hours due to cancer. Financial hardship was also prevalent (21.0%) despite relatively high household income and health insurance coverage throughout cancer treatment. Women who experienced cancer-related employment disruption had approximately twice the prevalence of financial hardship as those who did not experience employment disruption, even after adjustment for sociodemographic, employment, and clinical characteristics. The assessment of the relative importance of employment disruption to financial hardship after cancer remains a gap within cancer survivorship research (22). Our study demonstrates that among US women with breast cancer, the effect of cancer-related employment disruption on financial hardship is substantial, regardless of whether they stop work or reduce their work hours.
Only 3 studies, to our knowledge, have estimated the magnitude of the association between employment disruption specifically due to cancer and financial hardship, each of which reported results that align with our findings. In 2 nationally representative studies using 2011 and 2016 MEPS: Experiences with Cancer data, cancer survivors aged 18-64 years who experienced employment change had 1.5 times the probability of any financial hardship compared with those with no employment change (23), and female cancer survivors had 2.2 times the probability of material financial hardship (3). However, both studies lacked data on clinical characteristics (eg, confirmation of cancer diagnosis, stage at diagnosis), data that our study had available primarily from medical records. The MEPS surveys were also unable to stratify by cancer type, a relevant consideration given that breast cancer survivors report a higher prevalence of borrowing money, going into debt, or making other financial sacrifices relative to those with a history of colorectal cancer, prostate cancer, or melanoma (24). A third study of women with breast cancer identified from 2 Surveillance, Epidemiology, and End Results (SEER) registries (diagnosed 2005-2007 with financial outcomes assessed through 2011) found that women who had reduced work hours due to cancer had an increased likelihood of self-perceived financial decline (odds ratio = 1.68) and privations related to cancer (odds ratio = 2.00), including broad financial hardships due to medical expenses (25).
Addressing employment disruption as a risk factor for financial hardship lends itself to diverse targets of intervention, as employer-level factors intersect with risk factors that extend from the patient and family level up to state and national policies (22). For instance, employer features such as paid sick leave and flexible work schedules have been strongly associated with lower risk of job loss among women with breast cancer (26–30). Further, among women with breast cancer who were employed at 1 year postdiagnosis, those who reported lack of employer accommodations were more likely to report financial stress (31).
In addition to intervention at the employer level, further study is warranted regarding policies at the state and national levels that not only address the ability of cancer survivors to maintain employment after diagnosis and treatment but that also address their ability to return to work after a disruption and/or mitigate the financial consequences of such a disruption. The expansion of leave policies—paid and unpaid—beyond the existing limits may better protect against lost wages and job loss (32). The federal Family and Medical Leave Act mandates 12 weeks of unpaid leave for individuals diagnosed with cancer, but only for those who have been employed for at least 12 months at a business with 50 and more employees (33). Policies at the state level may offer further wage and job protection after cancer diagnosis but are typically only provided short term. For instance, only 5 states and Puerto Rico currently provide temporary disability insurance for nonwork-related illness, with limits on the length of period and benefit amount provided (34). For those who do experience employment disruption after diagnosis, studies indicate the effectiveness of multidisciplinary interventions (eg, physical, psychosocial, and educational components) throughout the cancer care continuum that call on patients, health-care professionals, and employers to facilitate return to work (35,36).
A defined cohort of women eligible for the parent Sister Study is unknown, though 75% of identified eligible women enrolled (14). Similarly, the ancillary survivorship survey from which the analytic sample is derived had a response rate of 90%, minimizing concern of selection bias from nonresponse. However, selection bias from survivor bias is a potential threat to validity (37), because both employment disruption and financial hardship may be indicators of worse cancer prognosis and proxy causes of mortality. This potential bias could result in the analytic sample containing healthier women who may experience less cancer-related employment disruption relative to the target population of working-age women diagnosed with breast cancer in the United States. In our study, few deaths occurred between enrollment into the parent Sister and Two Sister Studies and administration of the survivorship survey (n = 57 and 67, respectively). The sample also consisted of women with relatively high socioeconomic status, so findings may not generalize to breast cancer survivors with lower income or education, who are at particularly high risk of job loss following diagnosis (38,39).
Further, employment disruption and financial hardship measures were based on self-report with unknown validity. Measurements of these variables are subject to respondent perceptions and interpretation of the survey items. However, 2 of the 3 items used to assess financial hardship were directly from the Medical Expenditure Panel Survey and underwent cognitive testing for item comprehension and response processes (17), likely minimizing measurement error. Responses may also be subject to errors in recall, because women were a median of 5.6 years from diagnosis at the time of survey completion.
Though we had limited statistical power to detect effect measure modification by race or ethnicity due to the small sample size of women of color, analysis suggests that further exploration of this modification is warranted given a potentially stronger association among non-Hispanic Black women than among non-Hispanic White and Hispanic women. Further study is particularly relevant given that Black women with breast cancer have disparate rates of cancer-related job loss (25,27,39–42) and financial hardship (29,40,42) compared with White women, though the relative importance of employment disruption to financial hardship among Black women is unclear.
Survivorship concerns related to employment and financial stability can be particularly relevant for women with breast cancer given high rates of disease survival and the large number of women who receive this diagnosis each year. This study demonstrates the substantial impact of employment disruption after breast cancer diagnosis on financial hardship, even among women who had insurance coverage and financial resources at diagnosis. Findings highlight the need to target risk factors for cancer-related employment disruption, implement interventions and policies that facilitate return to work, and mitigate financial consequences after a disruption.
Funding
This work was supported in part by the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences (Z01 ES-044005), and by the Centers for Disease Control and Prevention, Division of Cancer Prevention and Control (Survivorship Survey). CM was supported by the UNC Lineberger Cancer Control Education Program (T32 CA057726).
Notes
Role of the funder: The study sponsor had no role in the design of the study, the data collection, the analysis or interpretation of the data, the writing of the article, or the decision to submit for publication.
Disclosures: VSB helped develop www.workplacetransitions.org, a free toolkit for employers seeking to accommodate cancer patients, funded by the Anthem Foundation and Pfizer Oncology. SBW has received unrelated grant funding to her institution from Pfizer in the past 3 years. All other authors have no conflicts of interest to disclose.
Author contributions: CM: Conceptualization, formal analysis, writing—original draft, writing—review and editing. DPS: Funding acquisition, writing—review and editing. LAP: Writing--review and editing. MEH: Writing—review and editing. VSB: Writing—review and editing. SBW: Writing—review and editing. HBN: Conceptualization, supervision, writing—review and editing.
Disclaimers: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Web site addresses of nonfederal organizations are provided solely as a service to readers. Provision of an address does not constitute an endorsement of this organization by CDC or the federal government, and none should be inferred. CDC is not responsible for the content of other organizations’ Web pages.
Prior presentations: This study was presented in part at the American Society of Preventive Oncology Annual Meeting (March 2020).
Data Availability
The data underlying this article were accessed from the Sister Study (https://sisterstudy.niehs.nih.gov/english/data-requests.htm). The Sister Study makes data available to NIEHS and external investigators following an approval process.
References
- 1. U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2019 submission data (1999-2017): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. 2020. https://gis.cdc.gov/Cancer/USCS/DataViz.html. Accessed October 24, 2019.
- 2. Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA A Cancer J Clin. 2019;69(5):363–385. [DOI] [PubMed] [Google Scholar]
- 3. Yabroff KR, Dowling EC, Guy GP, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ekwueme DU, Yabroff KR, Guy GP, et al. ; Centers for Disease Control and Prevention (CDC). Medical costs and productivity losses of cancer survivors--United States, 2008-2011. MMWR Morb Mortal Wkly Rep. 2014;63(23):505–510. [PMC free article] [PubMed] [Google Scholar]
- 5. de Boer AGEM, Taskila T, Ojajärvi A, van Dijk FJH, Verbeek JHAM.. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA. 2009;301(7):753–762. [DOI] [PubMed] [Google Scholar]
- 6. Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR.. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2017;109(2):djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pisu M, Henrikson NB, Banegas MP, Yabroff KR.. Costs of cancer along the care continuum: what we can expect based on recent literature. Cancer. 2018;124(21):4181–4191. [DOI] [PubMed] [Google Scholar]
- 8. Park J, Look KA.. Relationship between objective financial burden and the health-related quality of life and mental health of patients with cancer. J Oncol Pract. 2018;14(2):e113–e121. [DOI] [PubMed] [Google Scholar]
- 9. Kale HP, Carroll NV.. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer. 2016;122(8):283–289. [DOI] [PubMed] [Google Scholar]
- 10. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract. 2014;10(5):332–338. [DOI] [PubMed] [Google Scholar]
- 11. Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D.. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol. 2016;34(15):1732–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D.. Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34(9):980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sandler DP, Hodgson ME, Deming-Halverson SL, et al. ; the Sister Study Research Team. The Sister Study cohort: baseline methods and participant characteristics. Environ Health Perspect. 2017;125(12):127003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National Institute of Environmental Health Sciences. The Sister Study. http://www.sisterstudy.niehs.nih.gov. Accessed July 27, 2020.
- 16. Fei C, Deroo LA, Sandler DP, Weinberg CR.. Fertility drugs and young-onset breast cancer: results from the Two Sister Study. J Natl Cancer Inst. 2012;104(13):1021–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yabroff KR, Dowling E, Rodriguez J, et al. The Medical Expenditure Panel Survey (MEPS) experiences with cancer survivorship supplement. J Cancer Surviv. 2012;6(4):407–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. National Cancer Institute. Medical Expenditure Panel Survey (MEPS): Experiences with Cancer Survivorship Supplement. 2011. https://healthcaredelivery.cancer.gov/meps/. Accessed June 19, 2020.
- 19. Charlson ME, Pompei P, Ales KL, MacKenzie CR.. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 20. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 21. Greenland S, Pearl J, Robins JM.. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. [PubMed] [Google Scholar]
- 22. Yabroff KR, Zhao J, Zheng Z, Rai A, Han X.. Medical financial hardship among cancer survivors in the United States: what do we know? What do we need to know? Cancer Epidemiol Biomarkers Prev. 2018;27(12):1389–1397. [DOI] [PubMed] [Google Scholar]
- 23. Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR.. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(2):308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nekhlyudov L, Walker R, Ziebell R, Rabin B, Nutt S, Chubak J.. Cancer survivors’ experiences with insurance, finances, and employment: results from a multisite study. J Cancer Surviv. 2016;10(6):1104–1111. [DOI] [PubMed] [Google Scholar]
- 25. Jagsi R, Pottow JAE, Griffith KA, et al. Long-term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol. 2014;32(12):1269–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mujahid MS, Janz NK, Hawley ST, et al. Racial/ethnic differences in job loss for women with breast cancer. J Cancer Surviv. 2011;5(1):102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ.. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Res Treat. 2010;119(1):213–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blinder V, Eberle C, Patil S, Gany FM, Bradley CJ.. Women with breast cancer who work for accommodating employers more likely to retain jobs after treatment. Health Aff (Millwood). 2017;36(2):274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jagsi R, Abrahamse PH, Lee KL, et al. Treatment decisions and employment of breast cancer patients: results of a population-based survey. Cancer. 2017;123(24):4791–4799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Peipins LA, Dasari S, Rodriguez JL, White MC, Hodgson ME, Sandler DP.. Employment after breast cancer diagnosis and treatment among women in the sister and the two sister studies [published online ahead of print]. J Occup Rehabil. January 2021; doi: 10.1007/s10926-020-09951-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rosenberg SM, Vaz-Luis I, Gong J, et al. Employment trends in young women following a breast cancer diagnosis. Breast Cancer Res Treat. 2019;177(1):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dean LT, Moss SL, Rollinson SI, Frasso Jaramillo L, Paxton RJ, Owczarzak JT.. Patient recommendations for reducing long-lasting economic burden after breast cancer. Cancer. 2019;125(11):1929–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. U.S. Department of Labor. Family and Medical Leave Act. https://www.dol.gov/agencies/whd/fmla. Accessed March 20, 2020.
- 34. Triage Cancer Organisation. Triage cancer - legal and financial education. https://triagecancer.org/. Accessed March 18, 2020.
- 35. de Boer AGEM, Taskila TK, Tamminga SJ, Feuerstein M, Frings-Dresen MHW, Verbeek JH.. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2015;(9):CD007569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bilodeau K, Tremblay D, Durand M-J.. Exploration of return-to-work interventions for breast cancer patients: a scoping review. Support Care Cancer. 2017;25(6):1993–2007. [DOI] [PubMed] [Google Scholar]
- 37. Hernán MA, Hernández-Díaz S, Robins JA.. Structural approach to selection bias. Epidemiology. 2004;15(5):615–625. [DOI] [PubMed] [Google Scholar]
- 38. Blinder V, Patil S, Eberle C, Griggs J, Maly RC.. Early predictors of not returning to work in low-income breast cancer survivors: a 5-year longitudinal study. Breast Cancer Res Treat. 2013;140(2):407–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang L, Hong BY, Kennedy SA, et al. Predictors of unemployment after breast cancer surgery: a systematic review and meta-analysis of observational studies. J Clin Oncol. 2018;36(18):1868–1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wheeler SB, Spencer JC, Pinheiro LC, Carey LA, Olshan AF, Reeder-Hayes KE.. Financial impact of breast cancer in Black versus White women. J Clin Oncol. 2018;36(17):1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Spencer JC, Rotter JS, Eberth JM, et al. Employment changes following breast cancer diagnosis: the effects of race and place. J Natl Cancer Inst. 2020;112(6):647–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Samuel CA, Spencer JC, Rosenstein DL, et al. Racial differences in employment and cost-management behaviors in patients with metastatic breast cancer. Breast Cancer Res Treat. 2020;179(1):207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article were accessed from the Sister Study (https://sisterstudy.niehs.nih.gov/english/data-requests.htm). The Sister Study makes data available to NIEHS and external investigators following an approval process.