Dear Editor
Mucormycosis has emerged as the newest threat among Coronavirus disease-2019 (COVID-19) patients [1]. Among 101 worldwide mucormycosis cases, 81.2% were from India alone during COVID-19 [2]. Hypoxia, hyperglycemia, acidosis, hyperferritinemia, and rampant steroid use create a fertile soil for Rhizopus to grow [2]. While diabetes and COVID-19 form unholy association since inception [3], advent of mucormycosis forms the deadly trinity (mortality rate ∼30.7%) [2]. Hyperglycemia, found in 83.3% cases, is the single most important risk factor for developing mucormycosis among COVID-19 patients [2]. Prompt diagnosis, normoglycemia, tapering of glucocorticoids, anti-fungals and surgical debridement are the cornerstones of management [4].
While amphotericin-B is the drug of choice, posoconazole and isavucoanzoleare alternatives [5]. Due to upsurge of both COVID-19 and mucormycosis, scarcity of these drugs has raised concern [6]. Authorities have cautioned against the use of prophylactic antifungals to curb mucormycosis [7]. Thus, there is urgent requirement of alternative, cheaper medications. In this context we examine whether statins can be repurposed as potential anti-COVID-19-cum-anti-Rhizopus therapy to combat mucormycosis.
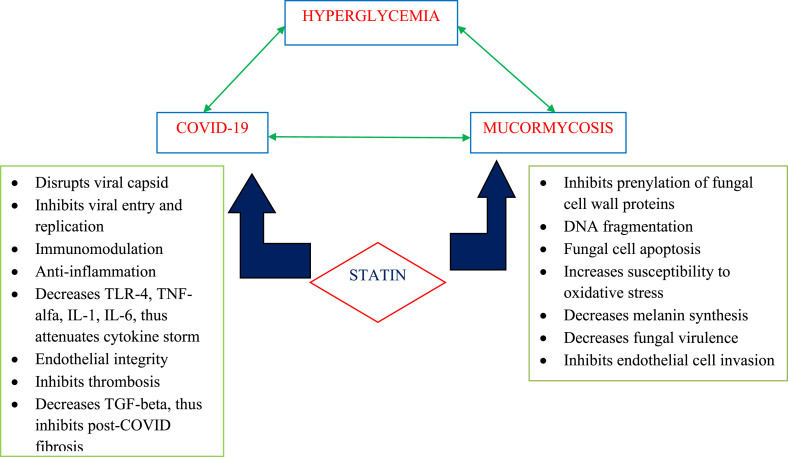
There is growing interest regarding statins to be deployed against COVID-19 because of their multifaceted pleiotropic effects [8,9]. Multiple studies and meta-analyses have shown improved outcome among COVID-19 patients with history of taking statins [[10], [11], [12], [13]]. Unfortunately, there is no randomized control trial available to explore the efficacy and benefits of statins in COVID-19 at present.Anti-fungal potential of statins is well-known and widespread use of statins is one of the reasons behind the lesser incidence of zygomycosis among diabetics since 1990s [14]. Lovastatin caused apoptosis of Mucor racemosus [15]. Amphotericin-B in combination with atorvastatin or lovastatin against Rhizopus oryzae was more effective than amphotericin-B alone [16]. Similar success has been noticed with fluvastatin and rosuvastatin against Rhizomucor and Rhizopus [17].I nvestigators showed statins impaired fungal morphogenesis by inhibiting isoprenylation of vital cell wall proteins, decreased germination, induced DNA fragmentation, increased susceptibility to oxidative stress, attenuated fungal virulence and prevented endothelial invasion (independent of GRP78/CotH interactions) [18]. Although these data from cell-basedand animal studies are encouraging, real world clinical data and human studies are needed to know whether statins reach enough tissue concentration to exert their antifungal activity when administered in usual therapeutic dosage (Fig. 1 ).
Fig. 1.
Mechanisms by which statins act against deadly duo of COVID-19 and mucormycosis.
(TLR- Toll like receptor, TNF- Tumor necrosis factor, IL- Interleukin, TGF- Transforming growth factor).
Diabetic patients, commonly being dyslipidemic should be screened for it and statins should be started without delay. Whether normolipdemic patients with diabetes on steroids are potential candidates for statin to prevent mucormycosis is to be explored. Although statins have been found to be safe among COVID-19 patients, their side effects and drug interactions with anti-fungals should be considered.
Authors’ contribution
SC generated the concept, did the literature search and wrote the first draft which was then critically reviewed and modified by BV, DS, AM and UKO. All authors agreed upon the final form of the article.
Funding
Nil.
Declaration of competing interest
Nil.
References
- 1.Soman R., Sunavala A. Post COVID-19 mucormycosis - from the frying Pan into the fire. J Assoc Phys India. 2021;69:13–14. [PubMed] [Google Scholar]
- 2.Singh A.K., Singh R., Joshi S., Misra A. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabet Metab Syndr. 2021 doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chatterjee S., Ghosh R., Biswas P., Dubey S., Guria R.T., Sharma C.B., et al. COVID-19: the endocrine opportunity in a pandemic. Minerva Endocrinol. 2020;45:204–227. doi: 10.23736/S0391-1977.20.03216-2. [DOI] [PubMed] [Google Scholar]
- 4.John T.M., Jacob C.N., Kontoyiannis D.P. When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for mucormycosis. J Fungi (Basel) 2021;7:298. doi: 10.3390/jof7040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornely O.A., Alastruey-Izquierdo A., Arenz D., Chen S.C.A., Dannaoui E., Hochhegger B., et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European confederation of medical mycology in cooperation with the mycoses study group education and research consortium. Lancet Infect Dis. 2019;19:e405–e421. doi: 10.1016/S1473-3099(19)30312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Today India. Shortage of antifungal drug as mucormycosis cases rise in India, states press panic button. https://www.indiatoday.in/coronavirus-outbreak/story/mucormycosis-amphotericin-b-drug-shortage-symptoms-treatment-1803854-2021-05-18 18th May, 2021.Available from:
- 7.Evidence based advisory in the time of COVID-19. https://www.icmr.gov.in/pdf/covid/techdoc/Mucormycosis_ADVISORY_FROM_ICMR_In_COVID19_time.pdf (last accessed on 19th May, 2021)
- 8.Pawlos A., Niedzielski M., Gorzelak-Pabiś P., Broncel M., Woźniak E. COVID-19: direct and indirect Mechanisms of statins. Int J Mol Sci. 2021;22:4177. doi: 10.3390/ijms22084177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vuorio A., Kovanen P.T. Statins as adjuvant therapy for COVID-19 to calm the stormy immunothrombosis and beyond. Front Pharmacol. 2021;11 doi: 10.3389/fphar.2020.579548. 579548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta A., Madhavan M.V., Poterucha T.J., DeFilippis E.M., Hennessey J.A., Redfors B., et al. Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19. Nat Commun. 2021;12:1325. doi: 10.1038/s41467-021-21553-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marić I., Oskotsky T., Kosti I., Le B., Wong R.J., Shaw G.M., et al. Decreased mortality rate among COVID-19 patients prescribed statins: data from electronic health records in the US. Front Med. 2021;8 doi: 10.3389/fmed.2021.639804. 639804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Permana H., Huang I., Purwiga A., Kusumawardhani N.Y., Sihite T.A., Martanto E., et al. In-hospital use of statins is associated with a reduced risk of mortality in coronavirus-2019 (COVID-19): systematic review and meta-analysis. Pharmacol Rep. 2021 Feb 20:1–12. doi: 10.1007/s43440-021-00233-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lohia P., Kapur S., Benjaram S., Mir T. Association between antecedent statin use and severe disease outcomes in COVID-19: a retrospective study with propensity score matching. J Clin Lipidol. 2021 Mar 6;(21):S1933–S2874. doi: 10.1016/j.jacl.2021.03.002. 00053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kontoyiannis D.P. Decrease in the number of reported cases of zygomycosis among patients with diabetes mellitus: a hypothesis. Clin Infect Dis. 2007;44:1089–1090. doi: 10.1086/512817. [DOI] [PubMed] [Google Scholar]
- 15.Roze L.V., Linz J.E. Lovastatin triggers an apoptosis-like cell death process in the fungus Mucor racemosus. Fungal Genet Biol. 1998;25:119–133. doi: 10.1006/fgbi.1998.1093. [DOI] [PubMed] [Google Scholar]
- 16.NaeimiEshkaleti M., Kordbacheh P., Hashemi S.J., Falahati M., Zaini F., Mirhendi H., et al. In Vitro activity of amphotericin B in combination with statins against clinical and environmental Rhizopus oryzae strains. Iran J Public Health. 2019;48:943–948. [PMC free article] [PubMed] [Google Scholar]
- 17.Galgóczy L., Lukács G., Nyilasi I., Papp T., Vágvölgyi C. Antifungal activity of statins and their interaction with amphotericin B against clinically important Zygomycetes. Acta Biol Hung. 2010;61:356–365. doi: 10.1556/ABiol.61.2010.3.11. [DOI] [PubMed] [Google Scholar]
- 18.Bellanger A.P., Tatara A.M., Shirazi F., Gebremariam T., Albert N.D., Lewis R.E., et al. Statin concentrations below the minimum inhibitory concentration attenuate the virulence of Rhizopus oryzae. J Infect Dis. 2016;214:114–121. doi: 10.1093/infdis/jiw090. [DOI] [PMC free article] [PubMed] [Google Scholar]