Abstract
Coronavirus disease 2019 (COVID-19) is a devastating viral infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The incidence and mortality of COVID-19 patients have been increasing at an alarming rate. The mortality is much higher in older individuals, especially the ones suffering from respiratory distress, cardiac abnormalities, renal diseases, diabetes, and hypertension. Existing evidence demonstrated that SARS-CoV-2 makes its entry into human cells through angiotensin-converting enzyme 2 (ACE-2) followed by the uptake of virions through cathepsin L or transmembrane protease serine 2 (TMPRSS2). SARS-CoV-2-mediated abnormalities in particular cardiovascular and neurological ones and the damaged coagulation systems require extensive research to develop better therapeutic modalities. As SARS-CoV-2 uses its S-protein to enter into the host cells of several organs, the S-protein of the virus is considered as the ideal target to develop a potential vaccine. In this review, we have attempted to highlight the landmark discoveries that lead to the development of various vaccines that are currently under different stages of clinical progression. Besides, a brief account of various drug candidates that are being tested to mitigate the burden of COVID-19 was also covered. Further, in a dedicated section, the impact of SARS-CoV-2 infection on neuronal inflammation and neuronal disorders was discussed. In summary, it is expected that the content covered in this article help to understand the pathophysiology of COVID-19 and the impact on neuronal complications induced by SARS-CoV-2 infection while providing an update on the vaccine development.
Keywords: SARS-CoV-2, Neurological damage, Coagulation, ACE-2, S-protein, Vaccine
Introduction
Coronaviruses (CoVs) are RNA viruses, which belong to the Coronaviridae family and Coronavirinae subfamily. They are widely distributed among animals and humans, causing respiratory, enteric, hepatic, and neurological disorders [1, 2]. SARS-CoV, SARS-CoV-2, hCoV-229E, OC43, NL63, and HKU1 are currently circulating in the human population, causing mild and self-limiting upper respiratory tract infections [3]. Severe acute respiratory syndrome-coronavirus (SARS)-CoV and Middle East respiratory syndrome-coronavirus (MERS)-CoV have emerged as two highly pathogenic CoVs over the past two decades [4]. The outbreak of highly contagious SARS-CoV-2 is a variant of coronavirus, which is currently causing a pandemic infection globally. Infection with SARS-CoV-2 causes a severe respiratory disease referred to as the COVID-19, which is accompanied by the symptoms of fever, cough, pneumonia, dysphonia, and occasional diarrhea, after 3–14 days of incubation [5, 6]. As of April 6th 2021, over 131.8 million confirmed cases and 2.8 million deaths were reported worldwide due to COVID-19 disease (https://www.who.int.).
Key Insights in to the Structural Features of SARS-CoV-2
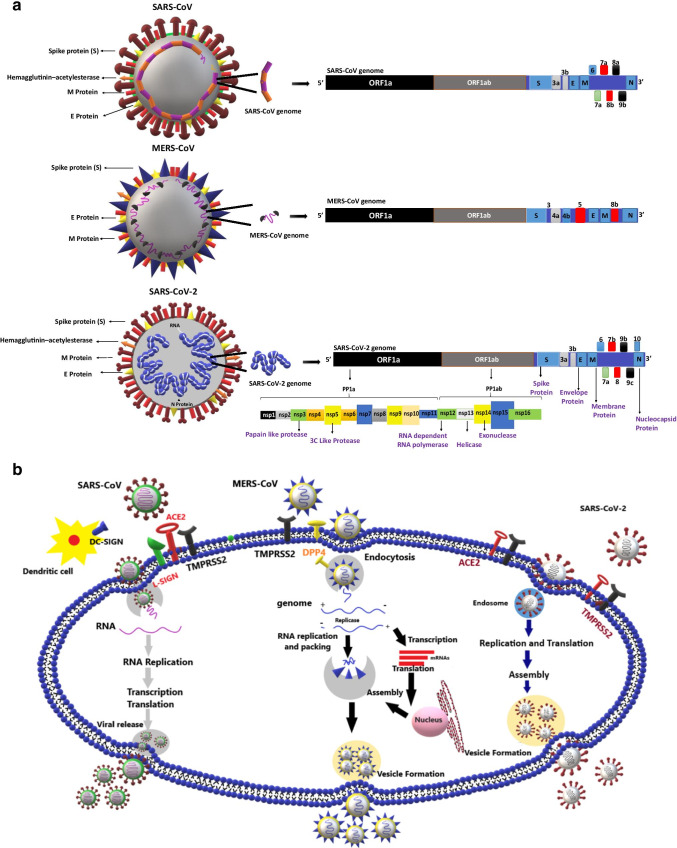
Structurally, SARS-CoV-2 is a 65–125 nm in diameter virus with club-shaped spikes on the enveloped surface. The virus contains a helical nucleocapsid, which is bound to a single positive-strand RNA of 27–32 kbp [7, 8]. Phylogenetic studies of the SARS-CoV-2 genome revealed its homology to other beta coronaviruses that were reported in bats. SARS-CoV-2 has a similarity of 79% to SARS-CoV and 50% to the MERS-CoV [9]. The genome of SARS-CoV-2 contains 14 open reading frames (ORFs) [10]. The ORF1a/ORF1ab is located at the 5′ end and encodes two polypeptides, PP1a and PP1ab. Polypeptides upon proteolytic cleavage encode nonstructural proteins (Nsp 1–16) that form a replicase and transcriptase complex, which is required for replication and transcription of the virus [11, 12]. The other 13 ORFs at 3′ encode four main structural proteins and nine putative accessory factors. Structural proteins include: spike (S) protein, nucleocapsid (N) protein, membrane (M), and envelope (E) proteins, which are essential for virus assembly and infection [13] (Fig. 1). “S” protein interacts efficiently with various host receptors and facilitates the attachment of the virus on the host cell surface and mediates the entry of the virus into the host cells. “M” protein maintains the virus in its intact shape [14]. “E” protein is the smallest structural protein that plays a significant role in the viral pathogenesis, viral assembly, and viral release inside the host cells [15]. “N” protein interacts with RNA substrates, transcriptional regulatory sequences, and genomic packing signals and plays a critical role in the pathogenicity [16, 17]. The other essential structural and accessory proteins coded by the open reading frames are hemagglutinin esterase protein, 3a/b protein, and 4a/b protein [8]. Recent research reports have identified many mutations in the genome of SARS-CoV-2, suggesting the ability of viruses to acquire adaptations to their new host. The enhanced infection abilities of the SARS-CoV-2 are believed to be imparted by mutations in NSP2 and NSP3 molecules [18].
Fig. 1.
Genome organization of coronaviruses and variations in their mode of entry into human cells: a Structural representation and genome organization of SARS-CoV, MERS-CoV, and SARS-CoV-2: SARS-CoV-2 genome encodes four major proteins viz., spike (S) protein, the nucleocapsid (N) protein, the membrane (M) protein, and the envelope (E) protein. Total six open reading frames (ORFs), ORF3a, ORF6, ORF7a, ORF7b, ORF8, ORF10, and the polyprotein ORF1ab encodes several enzymatic proteins for the effective viral invasion of the host cells. b Host cell receptors and replication mechanism of SARS-CoV, MERS-CoV, and SARS-COV-2: the spike protein of the CoVs interacts with receptors on the host cell to make its entry. ACE-2 serves as a receptor for SARS-CoV and SARS-CoV-2. DC-SIGN and L-SIGN serve as co-receptors for SARS-CoV. DPP4 serves as a receptor for MERS-CoV. CoVs replicate in the host causing cellular damage leading to further complications
Mitigating SARS-CoV-2-Induced COVID-19 Disease: Strategies That Are Under Evaluation
Several basic-, clinical-, and public health research findings have reported the efficacy of several molecules against the target proteins in SARS-CoV-2. Besides, several immunomodulators and drug repurposing strategies have been described as effective against SARS-CoV-2; however, their usage was constrained by adverse drug reactions and systemic toxicity. For instance, the administration of ACE-2 inhibiting anti-malarial drug hydroxychloroquine (HCQ) was proven effective against SARS-CoV-2-induced damage. However, monotherapeutic approaches using HCQ were reported unsuccessful, hence, strategies combining HCQ with other pharmacological agents for treating COVID-19 cases are currently being explored [19]. Also, several novel small molecule inhibitors (NSMIs), antiviral agents such as umifenovir, remdesivir, nitazoxanide, favipiravir, ritonavir, lopinavir, interferons (IFNs), anti-cytokine drugs, anticoagulants, and passive antibody therapies are currently being tested in different stages of clinical development (Table 1) [19].
Table 1.
Therapeutic strategies to target ACE-2 receptor and S-protein interaction in SARS-CoV-2 infection
| Type | Target | Description |
|---|---|---|
| Synthetic compounds | ||
| RS504393 | ACE-2 and S-protein of SARS-CoV-2 | Treated for lung injury and bronchial wall thickening [20] |
| KT185 | S-protein of SARS-CoV-2 | Anti-inflammatory [21] |
| TNP | ACE-2 | Tyrosine kinase inhibitor [22, 23] |
| GNF-5 | ACE-2 | Kinase inhibitor [24] |
| GR127935 hydrochloride hydrate | ACE-2 | Vasoconstriction monitoring [25] |
| Eptifibatide acetate | ACE-2 | Protects lung injury and inflammation [26] |
| Monoclonal antibody | ||
| 47D11 | Entry of SARS-CoV-2 | Human antibody specific to SARS-CoV-2 [27] |
| Antiviral agents | ||
| HrsACE-2 | ACE-2 | Recombinant protein [28] |
| CR3022 | S-protein | Neutralizing antibody [29] |
| Umifenovir (Arbidol) | Endocytosis | Membrane fusion inhibitor [30, 31] |
| EK1C4 | Endocytosis | Pan-coronavirus fusion inhibitor [32] |
| Camostat mesilate | TMPRSS2 | Serine protease inhibitor [33, 34] |
| Nafamostat | TMPRSS2 | Serine protease inhibitor [30, 35] |
| Bromhexine hydrochloride | TMPRSS2 | Mucolytic drug [36] |
| PAI-1 | TMPRSS2 | Serine protease inhibitor [37] |
| Chloroquine | Cell fusion/virus | Drug for autoimmune disease [38] |
Key Therapeutic Targets
SARS-CoV-2 Interactions with Host Cells
Angiotensin-Converting Enzyme 2 (ACE-2)
ACE-2 is a zinc-dependent metallocarboxypeptidase ectoenzyme, which is reported to be a key mediator of SARS-CoV-2 entry into host cells [39]. ACE-2 is located on the apical membrane of polarized cells of the testis, cardiovascular epithelium, cardiac myocytes, cardiac fibroblasts, epithelial cells of the kidney, liver, intestine, brain, and lungs [39–43]. ACE-2 is a type I integral membrane protein sharing 40% homology with ACE (angiotensin-converting enzyme). It is a key player in the renin-angiotensin system (RAS) [44]. ACE activates RAS by converting angiotensin I to angiotensin II. Angiotensin II activity is mediated through selective interactions with angiotensin II type 1 receptor (AT1R) and angiotensin II type 2 receptor (AT2R), a type of G-protein-coupled receptors (GPCRs). However, additional data is currently warranted to delineate the role of ACE in the entry of human CoVs [44].
ACE-2 acts as a functional cellular receptor for coronaviruses, namely, NL63 and SARS-CoV, by facilitating viral entry into the lungs [45, 46]. Studies using fluorescent probes have confirmed that SARS-CoV-2 could act on the same ACE-2 receptor for entering the host cell [47, 48]. ACE-2 consists of an N-terminal peptidase domain and a C-terminal collectrin-like domain joined together with a single transmembrane helix and an intracellular segment of about 40 amino acid residues [49, 50]. The peptidase domain of ACE-2 cleaves angiotensin II to angiotensin (1–7), which functions in association with a G-protein-coupled Mas-receptor. The ACE-2-angiotensin-Mas receptor axis mediates a regulatory effect, which antagonizes the effects of the ACE-angiotensin II axis and consequently protects the pulmonary and cardiovascular system from the harmful impact of RAS activation [51–53].
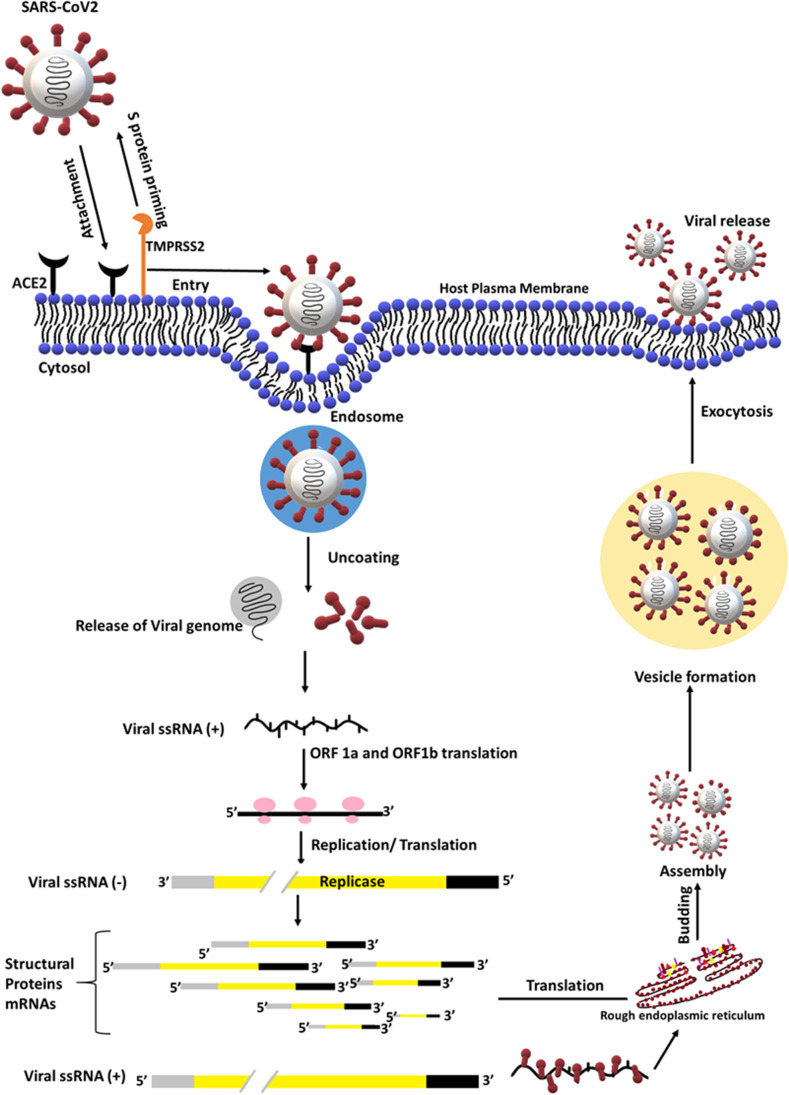
In the lungs, ACE-2 is expressed in pulmonary endothelium, type I and type II alveolar epithelial cells, and smooth muscle cells [41]. Several studies have reported that the downregulation of ACE-2 contributes to the development and progression of lung disease accompanied by the changes in vascular permeability, increased edema, neutrophil accumulation in lungs leading to respiratory failure, and death [52]. SARS-CoV-2 spike (S) protein binds to ACE-2, inducing ACE-2 shedding by activating disintegrin and metalloproteinase-17 [54] (Fig. 2). S1 subunit has the receptor-binding domain, which upon binding to ACE-2, undergoes conformational changes facilitating viral attachment to the host [55]. S1 subunit in S-protein undergoes priming by the transmembrane serine protease 2 (TMPRSS2) or pH-sensitive endosomal proteases cathepsin B and L at S1/S2 and S2 sites. S-protein priming mediates the entry of SARS-CoV-2 into the host, by the viral envelope and host cellular membrane fusion thereby triggers endocytosis [33, 56–58]. The enhanced binding affinity of SARS-CoV-2 to the ACE-2 receptor is due to a single N501T mutation in the gene coding for S-protein in SARS-CoV-2, which makes this disease transmission more likely to other organs [59].
Fig. 2.
Interaction of SARS-CoV-2 with ACE-2 receptors in lungs: the lysosomal proteases, such as elastase, and cell surface proteases TMPRSS2 could induce activation of SARS-CoV-2 S-protein for membrane fusion through ACE-2 receptors, which consequently causes lung tropism through endosome formation, multiple virion replication, and exocytosis
The acidic environment in the endosomes is capable of facilitating the fusion of SARS-CoV-2 viral and endosomal membranes, releasing the viral genome to the cytosol [60]. The released positive-strand viral RNA is translated on host ribosomes into a replicase, which upon proteolytic cleavage yields proteins needed for genome replication. The full-length antisense negative-strand viral RNA template is generated by viral RNA-dependent RNA polymerase for replicating positive strands of viral genomic RNA and shorter subgenomic negative-strand RNAs [61]. Negative-strand viral RNA serves as templates for the translation of mRNAs in the endoplasmic reticulum that code for the structural proteins of the virus. In the endoplasmic reticulum, viral proteins get encapsulated and bud into membranes. Upon viral assembly, virions form vesicles are released through exocytosis [61].
ACE-2 gene polymorphism plays a crucial role in inducing severe lung damage, as it accounts for the differences in the ACE expression level in the general population [62]. ACE-2 polymorphism is identified by the insertion (I) or deletion (D) of a 287 bp Alu repeat sequence in intron 16 of the ACE gene [63]. Further studies are needed to assess ACE gene polymorphism in COVID-19 patients in the ongoing clinical trials using ACE-2 inhibitors and angiotensin II receptor blockers therapy.
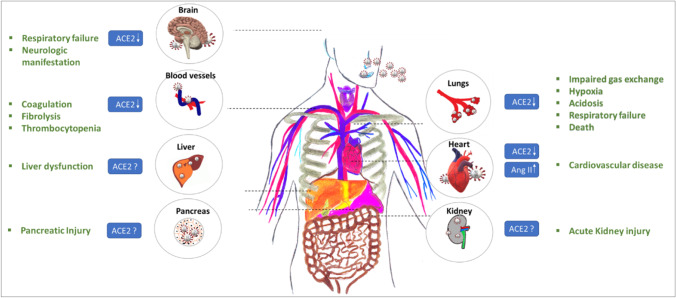
ACE-2 is expressed in many other organs, hence, SARS-CoV-2 is likely to enter tissues and organs through ACE-2 binding, causing multiple organ damage including kidney injury, cardiac injury, liver dysfunction, and cerebral damage [41, 64–66] (Fig. 3). The current understanding of the pathogenic mechanisms of SARS-CoV-2 binding to ACE-2 in the brain, liver, kidney, and heart are poorly described, hence, further studies are warranted.
Fig. 3.
Multiple organ dysfunctions induced by the interaction of SARS-CoV-2 with host cell ACE-2 receptors. The figure represents multi-organ dysfunction which is characterized by acute kidney injury, respiratory failure, liver failure, neurological complications, and cardiovascular disease upon SARS-CoV-2 infection
Addressing this gap, recent studies have shown that in the brain, ACE-2 is expressed in glial cells and neurons, suggesting the neurotrophic potential of SARS-CoV-2, entering through circulation or an upper nasal transcribrial route causing cerebral damage [64]. More research studies are required to elucidate the specific mechanisms behind neuronal damage mediated by SARS-CoV-2 infection (Fig. 3).
In addition to the brain, ACE-2 is expressed in hepatocytes of the liver, and bile duct cells consequently invoke damage to the liver [67]. Moderate microvascular steatosis, mild lobular, and portal activity were observed in biopsies of COVID-19 individuals [65]. Nevertheless, a mechanism underlying the liver dysfunction needs to be explored further, as the injuries could be caused by SARS-CoV-2 infection or antiviral drugs used during the treatment [65]. For example, several recent studies have shown that the antiviral drugs lopinavir/ritonavir causes injury to the liver [68]. Addressing this aspect will help to develop better strategies for mitigating SARS-CoV-2-induced liver damage (Fig. 3).
The kidney is another organ with elevated ACE-2 expression. The renal tubular cells are known to express high levels of ACE-2 [69]; however, no research evidence has been reported for the SARS-CoV-2 invoked kidney injury. In a statistical survey of 1099 COVID-19 patients, 0.5% reported acute kidney injury with a severity rate of 83.3%. In some COVID-19 patients, SARS-CoV-2 was detected in the urine [69]. Additional studies are immediately warranted to test whether SARS-CoV-2 infections cause kidney damage, if so, the mechanisms involved in such cellular damage. Further, it is currently unknown whether urine collected from COVID-19 patients could also be used to detect SARS-CoV-2. Establishing methods to detect SARS-CoV-2 in urine will help in minimizing the distress caused due to nasal/throat sample collection (Fig. 3).
In the case of heart, SARS-CoV-2 follows the mechanisms similar to SARS-CoV to trigger cardiovascular complications [70]. ACE-2 expressed in cardiomyocytes is capable of interacting with SARS-CoV and fosters the extensive levels of Ang-II, consequently promoting cardiovascular abnormalities [70]. But it is currently unknown whether SARS-CoV-2 can also directly infect cardiomyocytes.
ACE-2 expression is also detected in exocrine glands and islets of the pancreas. ACE-2 expression in the pancreas is slightly higher compared to the lungs, indicating the possibility of binding of SARS-CoV-2 to ACE-2 in the pancreas, causing severe pancreatic injury [71].
Studies have reported coagulation and fibrinolysis in COVID-19 patients, which is due to the activation of host defense mechanisms to limit the spread of the virus upon infection [72]. The initial phase of viral infection triggers a systemic inflammatory response characterized by an elevated level of cytokine activity and generation of thrombin and fibrinogen [72]. This response induces the expression of tissue factors, which initiate the coagulation. The measurement of coagulation and fibrinolysis factors in bronchoalveolar lavage (BAL) fluid showed elevated thrombin levels and the suppression of fibrinolysis, indicating the pathogenesis of respiratory distress. Furthermore, massive endothelial cell apoptosis, which is caused by vascular endothelial damage upon SARS-CoV-2 infection contributes to procoagulant changes in COVID-19 [72]. Recent studies have shown thrombocytopenia in COVID-19 patients, but the mechanism of SARS-CoV-2 involvement is still unclear [73] (Fig. 3).
Cytokine Storm
Innate- and acquired-immunity mediated antiviral responses triggered by recognizing pathogen-associated molecular patterns (PAMPs) and induced antigen-specific adaptive immunity are the key defense systems that protect the host organisms from devastating effects of infections [74, 75]. The response to viral infections depends on the release of cytokines, chemokines, leukotrienes, proteases, reactive oxygen species, and the rate of viral clearance [76]. The balance between the antagonistic signals and cellular reactions influences the immune response to pathogens by preventing damage to host tissues. As a result, the activated immune system returns to a resting state and prevents the damage, which is otherwise caused by continuously activated host immune reactions [76]. Excessive synthesis of cytokines in response to viral infections results in an acute and severe systemic inflammatory response known as “cytokine storm,” which causes multi-organ damage [76]. Studies have shown that IL-6 and IL-17 are predictive of disease severity and correlate with respiratory failure [77]. Potential therapeutic strategies targeting IL-17 alone or in combination with IL-6 for COVID-19 are currently under investigation. Tocilizumab, which targets IL-6, is currently approved by the United States Food and Drug Administration (US-FDA) for treating COVID-19 patients [78].
SARS-CoV-2-Induced Neurological Complications
The SARS-CoV-2 primarily affects pulmonary, cardio-, and renal functions [79]. However, recently it has been reported that SARS-CoV-2 can cause secondary complications on other systems as well [79]. Neurological complications are one such set of complications that require more attention to develop novel therapeutic modalities. Frequently, SARS-CoV-2 infections-induced neurological disorders are combined with either pre-existing metabolic abnormalities such as diabetes, other infections, or chronic- to acute inflammatory episodes of the nervous system [80]. However, it is currently not clear whether all COVID-19 patients develop neurological complications or only a portion is prone. Therefore, it is important to know the signs and features of susceptible individuals who are at risk for developing neurological infections.
Routes of SARS-CoV-2 Entry into the Nervous System
The SARS-CoV-2 virus, which enters the bloodstream can spread into the central and peripheral nervous systems (PNS) via retrograde axonal transport or by infecting the pericytes and astrocytes, which are the central part of the blood–brain barrier (BBB) [81]. Neuro-invasion of SARS-CoV-2 may also be mediated through the olfactory nerve or infection of vascular endothelium or by infected leukocyte migration across the BBB. Once the virus enters CNS through the conceded BBB, the SARS-CoV-2 can be distributed along the neurotransmission or hematogenous pathways that include serotonergic dorsal raphe system and Virchow-Robin spaces, respectively. The neuro-invasive potential of SARS-CoV-2 predominantly relies on the medullary structures interacting with the brain stem, accompanied by the respiratory system. This could be one of the conducive factors responsible for the high incidence of respiratory failures in COVID-19 patients [81].
The neurological effects of COVID-19 are due to either direct viral entry or indirect infection into the CNS [82, 83]. Epidemiological studies have shown that the latency of 1-week gap between the initial infection and severe infection for COVID-19 patients provides space sufficient for potential viral entry into the CNS [84]. Neurotropism activity is commonly detected in coronaviruses; neuro-invasive properties are well documented in SARS-CoV, MERS-CoV, HCoV-229E, and HCoV-OC43 [85–87]. Further, the spike protein of SARS-CoV-2 alters the blood–brain barrier (BBB) function, which provides an additional mechanism of potential CNS entry [88]. The conserved viral structure and genetic similarity of SARS-CoV-2 with SARS-CoV provide further evidence that the virus can enter into the CNS [89, 90].
Kanberg et al. reported CNS damage in COVID-19 patients by measuring the variations in serological biomarkers. For instance, elevated plasma glial fibrillary acidic protein (GFAp) and neurofilament light chain (NfL), which are the markers of astrocytic and neuronal injury, were reported in 47 COVID-19 patients [91]. The authors of this study demonstrated a significant increase in GFAp and NfL in 18 patients with severe COVID-19; however, GFAp levels were reported to decrease upon treatment follow-up. But a continuous increase in NfL level was reported throughout the treatment. Similar to severe COVID-19 cases, an increase in the levels of plasma GFAp was also reported even in 9 patients with moderate COVID-19 [91]. But no treatment follow-up status is reported in this study. This phenomenon is evident in astrocytes’ early involvement and delayed axonal injury in the CNS due to COVID-19 infection [91].
Coolen et al. have provided evidence of central nervous system involvement in COVID-19 patients [92]. Authors of this study have performed magnetic resonance imaging (MRI) on COVID-19 patients within 24 h of death and showed parenchymal abnormalities, including white matter changes, posterior reversible encephalopathy syndrome, and hemorrhage in four individuals [92]. This could be due to the breakdown of the BBB and COVID-19 based endothelial abnormalities, irrespective of SARS-CoV-2 virus infection in endothelial cells. The study also showed an indication of olfactory bulb unevenness and anosmia in four other patients [92]. A study conducted in Strasbourg, France, on the neurological function of 58 COVID-19 patients with acute respiratory distress syndrome (ARDS) admitted into the intensive care unit (ICU) was assessed and showed neurological abnormalities in the 8/58 patients (~ 14%) during admission to the ICU. However, 67% (39/58) patients exhibited profound neurological signs while 69% (40/58) of patients exhibited agitation after the withdrawal of sedation or a neuromuscular blocker. Also, approximately 45% (26/58) of patients were characterized by a state of confusion, while 67% (39/58) of patients reported exhibiting corticospinal tract signs. Serendipitously 13 patients (22.41%) exhibited encephalopathic features followed by leptomeningeal enhancement in (8/13) patients and bilateral frontotemporal hypoperfusion (11/13) in MRI scans. Follow-up clinical studies were performed on 45 patients in which 15 patients typically exhibited dysexecutive syndrome followed by the presence of in-attention, disorientation, alterations in movements, and responses [93]. A research study on 214 COVID-19 patients from Wuhan, China, delineated severe SARS-CoV-2 infection in 41.1% (88/214) patients. The remaining had non-severe infection (58.9%; 126/214); among them 36.4% (78/214) of patients had orchestrated distinct neurologic signs due to damage to sensory neurons that consequently foster defects in sensations of olfaction and gustation and invoke neuropathic pain, seizures, and strokes [83]. Furthermore, these defects were more evident in COVID-19 patients across the world [83].
Based on the symptoms, neurological manifestations underlying the COVID-19 were segregated into skeletal, muscular injury indexes, and CNS indexes [94]. Among these neurological manifestations, acute cerebrovascular disease, headache, dizziness, ataxia, defects in consciousness, and seizures were reported as critical ones. For instance, the SARS-CoV-2 infection invoked alterations in the peripheral nervous system (PNS) as indicated by nerve pain, impaired taste, smell, or vision [6]. Results of this study showed that 78/214 patients exhibited neurological abnormalities exhibiting symptoms related to CNS dysfunction, skeletal muscle injury, and defects in PNS function [83]. All these neurological symptoms were predominantly reported in older patients [60 years or above], who had existing co-morbid conditions viz., hypertension, diabetes, chronic malignancy, and cerebrovascular diseases [95–98].
A plethora of recent research reports depicted that the ACE-2 receptor extensively plays a crucial role in SARS-CoV-2 virus entry into the host body. This protein is also widely reported in CNS, predominantly in the brainstem and subfornical organ, paraventricular nucleus, nucleus of the tractus solitarius, and the rostral ventrolateral medulla regions [99]. These regions of the brain are known to control cardiovascular functions [99]. ACE-2 expression is also reported in neurons and astrocytes [99]. Li et al. deciphered that COVID-19 infection could induce changes in gut microbial composition and invoke neuropathogenesis which confers neuropsychiatric symptoms through the gut-brain axis [100].
Initial studies using RT-PCR depicted the extensive ACE-2 expression in the brain [101], but ACE-2 immunoreactivity was typically reported in the brain endothelial and smooth muscle cells [102]. The expression of ACE-2 in glial cells [99, 103] concludes that brain tissue could be a potential target for SARS-CoV-2. SARS-CoV-2 RNA was evident during CNS infection indicating the possibility of direct infection of CNS by SARS-CoV-2.
The COVID-19 patients with meningitis exhibit seizures, hippocampal atrophy, and pan-paranasal sinusitis [104]. A recent case study showed the existence of SARS-CoV-2 virus in the CNS of a 56-year-old encephalitis patient who had reported mitigation of consciousness. These findings in COVID-19 patients are in line with past reports with HCoV-OC43 infected patients [105]. Likewise, SARS-CoV was observed in CSF from SARS patients with persistent epilepsy [106]. A retrospective study of COVID-19 patients showed acute ischemic stroke, cerebral venous sinus thrombosis, and cerebral hemorrhage [83]. Hence, it was concluded that the SARS-CoV-2 exhibits a capacity to bypass the respiratory tract and the capability to confer infection in other tissues, which could be a critical feature of the SARS-CoV-2 virus.
SARS-CoV-2 and a Robust Mitochondrial System and Immune-Competency Rely on Hormesis
Recent studies have shown the ability of SARS-CoV-2 to impair autophagy and block mitophagy [107]. This effect is similar to SARS-CoV, which is capable of mitochondrial fusion, impairs mitophagy, and induces cell death [108, 109]. Studies are currently investigating the SARS-CoV-2-induced modulation of mitochondrial- and immune system changes by unraveling the modulation of the viral-mediated inflammasome. Irisin, a muscle-derived hormone, is reported to protect mitochondria and ischemia/reperfusion injury in the lung during exercise [110]. But it is unknown whether SARS-CoV-2-induced mitochondrial dysfunctions are mediated by irisin modulation. Furthermore, studies have demonstrated that irisin could facilitate changes in the genes in adipocytes that are affected by SARS-CoV-2 and neutralize the ROS in macrophages thereby display anti-oxidant and anti-inflammatory properties [111, 112]. Since mitochondria play an important role in immune response, and several viruses can modulate mitochondrial function, it is presumed that SARS-CoV-2-induced effects could also be mediated through the dysregulation of mitochondrial function [109]. The altered mitochondrial function might be a variant process, which occurs in SARS-CoV-2-mediated pathophysiology [113]. Several immune cells possess mitochondria and are now embraced by the “immunometabolism concept” [114, 115]. However, age and lifestyle are two crucial factors that determine susceptibility to the virus based on hormetic-like preconditioning [115]. Any “virus-induced exogenous hormetic stimuli” could be mitigated by the recurrent physical activity consequently decreasing the viral-mediated mitochondrial stress [116–118]. Preconditioning signal through hormone-like irisin by the physical activity is leading to cellular protection via hormesis, which is an important redox-dependent anti-inflammatory and anti-oxidant-associated mechanism [113]. Thus, mitochondrial hijacking and hormetic-like preconditioning through SARS-CoV-2 could be considered as a significant factor in the pathophysiology of neuroinflammation [113].
SARS-CoV-2 is reported to enhance aerobic glycolysis (Warburg shift) to promote replication, which is a strategic tactic used by many viruses (similar to cancer cells) via metabolic reprogramming [119]. For instance, melatonin can impair this metabolic reprogramming mediated by SARS-CoV-2, hence, melatonin could be considered as the powerful antioxidant which can protect mitochondria [120, 121]. This kind of divergent SARS-CoV-2 signaling should be unraveled in neuronal cells by studying the melatonin-induced mitochondrial antioxidant system [121]. Several viruses including SARS-CoV-2 can modulate mitochondrial bioenergetics and redox function in both immune systems and acquire the capability of infecting other cells to enhance their replication, which consequently fosters viral-mediated pathophysiology due to extensive oxidative stress [121]. Hormetic dose–response of novel anti-viral molecules may provide the central underpinning of neuroprotective responses against viral infections. The study of hormetic dose-responses is crucial to illustrate the cellular defense pathways including sirtuin and Nrf-2 related signaling cascades about SARS-CoV-2-induced neuronal diseases [122]. Furthermore, it is crucial to unravel the underlying viral-mediated pathophysiology as SARS-CoV-2 may modulate the functions of neuronal mitochondria to generate oxidative stress. As mitochondria-mediated aging is associated with dysregulated metabolism and requires novel therapeutic modalities viz., mitochondrial anti-oxidants and anti-inflammatory molecules are likely to correct these dysregulated metabolic and physiological processes before the administration of vaccines against SARS-CoV-2-induced neuropathology [123]. “Hydroxytyrosol (HT)-rich aqueous olive pulp extract (HIDROX®)” has been reported to mitigate SARS-CoV-2-induced pathophysiology by inducing potent virucidal activity [124]. Hydroxytyrosol (HT) and oleuropein aglycone (OLE) are two potential molecules reported being beneficial to mitigate the pathophysiology of neurodegeneration [124]. Hormesis and anti-oxidant nature, which enhances the activity of proteasome and phase II detoxifying enzymes, are potential mechanisms of action by which these pharmacological molecules work against SARS-CoV-2-induced neuropathophysiology [125, 126]. In addition to the above therapies, the vaccinomics approach might be useful to mitigate the complications accelerated with immunosenescence factors against SARS-CoV-2 in the infected individuals over 65 years of age [123, 127]. Additional studies are warranted to prove the role of vaccinomics-based approaches for reducing the complications of SARS-CoV-2 infections.
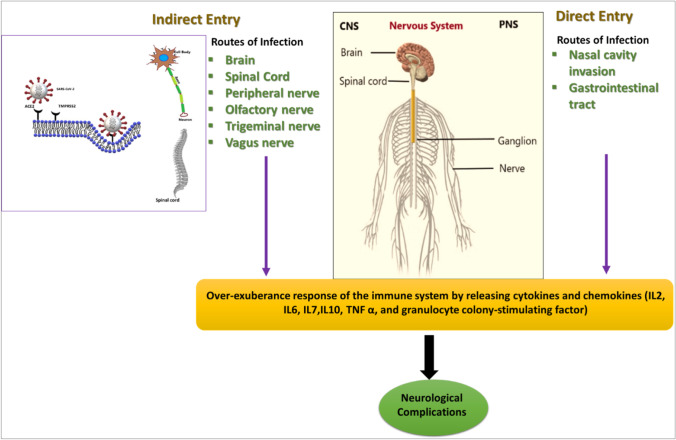
Mechanism of Infection of Central Nervous System (CNS) and Peripheral Nervous System (PNS) by SARS-CoV-2
Extensive scientific evidence now proved that COVID-19 can cause many neurological complications [128]. Also, neurological complications have attracted widespread attention among researchers to delineate the short- and long-term impact on population health during COVID-19 infections [129]. Yet, in-depth studies are required to ascertain the underlying mechanisms/pathways involved in the COVID-19 induced neuronal complications.
Indirect Entry
SARS-CoV-2 may enter the nervous tissue through retrograde and anterograde transport along with peripheral nerves [130]. Existing data showed that SARS-CoV-2 can infect the olfactory bulb through TMPRSS2 and ACE-2 receptors [131, 132]. Once infected, the transfer of virus may occur through extracellular vesicles (EVs) in the olfactory ensheathing cells (OECs), independent of the ACE-2 receptors. In addition to the olfactory nerve, the virus can migrate via the trigeminal and vagus nerves [130].
SARS-CoV-2 may invade the nervous tissue through the ACE-2 or TMPRSS2 receptors. Since, ACE-2 receptors are also expressed on the membrane of the spinal cord, the virus may invade the spinal cord through its binding to the ACE-2 receptors on the surface of peripheral neurons. The virus can penetrate the cribriform plate located closely to the olfactory bulb and the olfactory epithelium (OE), thereby enters the CNS system indirectly. Anosmia or hyposmia are considered as novel complications of COVID-19 patients to confirm this route of infection [133].
COVID-19 induced neural infection is accompanied by the uptake of the virus into the ciliated dendrites/soma [134]. The virus could effectively enter via anterograde axonal machinery transport along the olfactory nerve [134]. Moreover, the virus can also infect and cross non-neuronal olfactory epithelium cells and directly enter the CSF around the olfactory nerve bundles [135]. ACE-2 and TMPRSS2 receptors of these cells could propagate the infection in elderly individuals, which may be considered as the higher risk of SARS-CoV-2 accumulation in OE cells [135] (Fig. 4).
Fig. 4.
Overview of SARS-CoV-2 entry in the nervous system. SARS-CoV-2 virus is reported to infect CNS and PNS by direct and indirect pathways. This results in the generation of cytokines and chemokines by elevating the immune response and causing severe neurological complications
Direct Pathway
Even though it is now confirmed that SARS-CoV-2 infection leads to neurological complications, the direct entry of the SARS-CoV-2 into the nervous system and its exact microinvasion are yet to be unraveled. For instance, the virus may directly confer invasion of brain tissues as indicated by the presence of nucleic acid materials in both CSF and brain tissue [130]. This kind of viremia occurred through a direct pathway likely to provoke virus transcytosis across the endothelial cells of the blood–brain barrier (BBB) of the brain or the virus infection across the epithelial cells of the blood-cerebrospinal fluid barrier (BCSFB) in the choroid plexus (CP) of brain ventricles. Besides, the leukocytes may also act as a vector to transport the virus across the BBB [136, 137]. The Braak hypothesis says that an invasive neuro-virus could enter the CNS through the nasal cavity and the gastrointestinal tract [138] (Fig. 4).
COVID-19 Induced Neuroinflammation
One of the significant neuropathological mechanisms of SARS-CoV-2 infection is the induction of a hyperinflammatory state in infected individuals [66]. The over-exuberance response of the immune system could foster the generation of cytokines and chemokines viz., interleukins 2, 6, 7, and 10, TNF α, and granulocyte colony-stimulating factor (GCSF) [139]. These cytokines and chemokines provoke extensive activation of neuroinflammatory cascades and drive neuronal hyperexcitability via glutamate receptor activation followed by induction of seizures [140, 141]. An inflammatory theory of SARS-CoV-2 infection was also supported by the steroid response of COVID-19 patients comorbid with severe encephalitis [142].
Over-exuberance response of the immune system in SARS-COV-2 infection may cause inflammatory injury and brain edema, which consequently induce defects in consciousness [143]. Inflammatory and immunologic responses further amplify the cytokine storm [144]. Intracranial cytokine storm potentially confers BBB breakdown and leading to the migration of leukocytes. During this condition, the virus is failed to exhibit the potential of direct invasion or para-infectious demyelination [130].
It has been reported that COVID-19 patients experience defects in gustation (sense of taste) and olfaction due to direct damage to the olfactory bulb leading to inflammation in the nasal cavity. This inflammation blocks binding of odorants to the olfactory receptors thereby affect the olfactory responses [145]. Regeneration and repair of damaged neurons during COVID-19 take a longer time within the olfactory bulb [145]. Similarly, COVID-19 led to the dysfunction of taste buds thereby cause ageusia (loss of taste function of the tongue) [146]. In acute phases of this infection, the loss of olfaction could be due to nasal inflammation and mucosal edema. These symptoms may persist for months to years due to extensive olfactory insult triggered by the virus [145].
Impact of COVID-19 on Neurological Disorders
COVID-19 pandemic exhibited numerous short-term and long-term adverse effects on a large group of elderly people with neurological disorders and neurodegenerative diseases [147]. For instance, Parkinson’s disease (PD) is one of the devastating neurological diseases, which occurs due to the defects in the mesolimbic system of basal ganglia [148]. PD patients infected with COVID-19 exhibit adverse effects that include motor symptoms, such as tremors, freezing of gait, or dyskinesias [149], and diminished dopaminergic medication efficacy [150–152]. Thus, the COVID-19 pathophysiology and alteration in the dopamine synthesis pathway have been hypothesized. Recent reports have demonstrated the co-expression of dopa decarboxylase (DDC), a significant enzyme of both dopamine and synthetic serotonin pathways, and ACE-2 receptor [153]. SARS-CoV-2 binding with ACE-2 has been reported to invoke a downregulation of ACE-2 [154]. The possible functional connection between ACE-2 and DDC indicates the alterations in dopamine synthesis, which further confer PD-related complications [153]. An imbalance in dopamine levels can worsen the severity of PD. In addition to the impact of COVID-19 on PD patients, the virus may invoke sporadic PD during infection. For instance, ACE-2 is reported to be involved in co-regulating the dopa decarboxylase (DDC) during dopamine synthesis; any SARS-CoV-2-induced downregulation of ACE-2 expression would invoke alterations in both serotonin and dopamine pathways, which are significant pathways involved in PD pathophysiology [53, 153]. Hence, it is hypothesized that the SARS-CoV-2 can effectively induce alterations in dopamine during defective expression of ACE-2 and DDC [153].
Multiple sclerosis (MS) is another neurological complication reported to be worsened by SARS-CoV-2 infection. The mortality/morbidity risk was reported to be relatively low with disease-modifying therapies (DMTs) in the MS patients suffering from COVID-19 infection. Furthermore, the intake of immunomodulatory drugs in these patients could invoke low pulmonary capacity, which further enhances the risk of COVID-19 related pneumonia [155]. Hence, the decision to avoid the intake of DMTs in COVID-19 patients comorbid with MS relies upon several miscellaneous factors viz., immunomodulation, and disease severity. Complications of COVID-19 infection are much higher due to the over-reaction of the immune system to the SARS-CoV-2. However, further studies are warranted to decipher the molecular pathways to be targeted to mitigate the complications. Furthermore, the establishment of appropriate preclinical animal models would help in developing better therapeutic agents for combating COVID-19 induced complications in individuals suffering from MS [156–158].
SARS-CoV-2 infection may also invoke a severe neurodegeneration process, which could reduce the overall survival of COVID-19 patients with Alzheimer’s disease (AD) [130]. But, currently, no evidence suggests a correlation between COVID-19 and AD development [159]. One of the key factors responsible for AD induction is the accumulation of amyloid-beta plaques (Aβ plaques) in the brain [160, 161]. Aβ is produced from the enzymatic processing of amyloid precursor protein (APP). An intriguing relation between viral infections and Aβ has been delineated by several researchers and the data supports that Aβ is an antimicrobial peptide (AMP) [162]. The whole-brain homogenates obtained from AD patients compared to the age-matched non-AD samples suggested a strong correlation between AMP action and Aβ levels [162]. However, the extensive anti-microbial activity of Aβ was ablated in the models of immune depletion of AD brain homogenates, who were subjected to treatment with anti-Aβ antibodies. Transient infection with SARS-CoV-2 virus could either initiate or accelerate Aβ accumulation inside the brain and cause AD [159] Further, a positive inflammatory response was stimulated through transient viral infection inside the CNS, which may foster the abnormal self-perpetuating innate immune responses due to the severe cerebral Aβ stagnation [159]. Neuroinflammation is another early characteristic of AD. CNS tropism of the virus across brain tissues expressing ACE-2 can induce ACE-2 expression, which may enhance the risk of virus invasion and activate molecular processes that invoke neurodegeneration [159]. However, these molecular mechanisms in SARS-CoV-2 infection are yet to be unraveled to delineate the viral-induced alterations in neurodegeneration.
SARS-CoV-2-Associated Neurological Diseases
Guillain–Barré Syndrome (GBS) and SARS-CoV-2
Guillain–Barré syndrome (GBS) is an inflammatory poly-radiculo-neuropathy and it is associated with several viral infections [163]. The incidence of GBS is considered to be the most significant aspect in the SARS-CoV-2 infected patients as GBS could confer respiratory failure, which is the most devastating complication observed with SARS-CoV-2 infection [164]. The other disease complications of GBS are flaccid paralysis, sensory abnormalities, and autonomic dysfunction due to autoimmune-mediated pathophysiology [165].
GBS in a COVID-19 patient was first reported in Wuhan, China, where demyelination of motor and sensory nerves was detected with a prolonged distal latency [166]. It is caused due to the cross-reaction of antibodies produced by the host against the viral infection, binding to peripheral nerves causing neuronal dysfunction [167]. Reports suggested symptoms like facial and limb paresis (a muscular weakness caused due to nerve damage), paresthesia, and immune-inflammatory responses were evident in SARS-CoV-2-mediated neuronal pathophysiology in GBS patients [168]. For instance, a variant of GBS Miller Fisher syndrome and polycranial neuritis was reported by Gutiérrez-Ortiz et al. [169]. Albumin cytologic dissociation was observed in the CSF after few days of COVID-19 infection in the individuals with Miller Fisher syndrome and polycranial neuritis [169]. Few reports suggested that the demyelination of multiple peripheral nerves might be another reason associated with SARS-CoV-2 that may induce deteriorating conditions of the patients with GBS [170]; however, extensive research studies are required to elucidate this pathophysiology vividly to develop counteracting therapeutic modalities [171].
Encephalomyelitis and SARS-CoV-2
Acute disseminated encephalomyelitis (ADEM) is one of the reported diseases generated through the central infiltration of SARS-CoV-2 components in the olfactory and trigeminal nerve endings [172]. Patients diagnosed with ADEM associated with SARS-CoV-2 infection suffer from weakness and numbness in the limbs and few urinary disorders; however, to date, the complete pathophysiology is not investigated. The complete CSF analysis in these patients has been reported with xanthochromia with high protein and glucose [172].
Myalgia and Neuromuscular Junction Damage
Myalgia, referred to as the general muscle pain accompanied by the presence of fatigue, is worsened in SARS-CoV-2 infected individuals due to chronic muscle injury [173]. Myalgic symptoms are due to respiratory complications invoked via acute respiratory distress syndrome (ARDS) and inflammatory-cytokine storm-induced via SARS-CoV-2 pathophysiology through muscle cell ACE-2 receptors [173]. Another evident chronic effect is the immune-mediated muscle damage due to inflammatory cytokine responses in these patients [174, 175] (Table 2).
Table 2.
List of neurological disorders due to SARS-CoV-2 infection
| Neurological diseases | Disease—clinical manifestations | SARS-CoV-2-induced clinical manifestations | References |
|---|---|---|---|
| Parkinson’s disease (PD) | Tremors, dyskinesia | Chronic defects in the mesolimbic system of basal ganglia mainly in the dopaminergic neurons; enhanced neurodegeneration | [148, 149] |
| Alzheimer’s disease (AD) | Cognitive decline and memory loss | Enhanced accumulation of amyloid-beta plaques in the brain; enhanced neurodegeneration | [130] |
| Multiple sclerosis | Severe lymphopenia, optic neuritis | Extensive demyelination | [155] |
| Guillain–Barré syndrome (GBS) | Progressive flaccid paralysis, dyssynergia, areflexia | Severe autonomic dysfunction, respiratory failure, demyelination through immune response in the peripheral nervous system (PNS) | [163, 165, 166] |
| Miller Fisher syndrome | Diplopia, balance disturbances, and areflexia | Chronic demyelination of cranial and facial nerves | [169] |
| Acute disseminated encephalomyelitis (ADEM) | Encephalopathy, transverse myelitis, weakness, numbness of the limbs, and urinary disorders | Immune-mediated inflammatory demyelination affecting the white matter of brain and spinal cord | [172] |
SARS-CoV-2 and Animal Models of Neuronal Damage
Animal studies on SARS-CoV-2 can deliver key information on the pathophysiology of CNS [159]. For instance, mice, hamsters, ferret, and non-human primate models were already in use to examine the effects of virulence in vivo [176]. Transgenic models of mice expressing the human ACE-2 (hACE-2) gene, which is the receptor for SARS-CoV-2 in humans, are one such animal model to study the role of viral infection on neuronal damage.
Potential treatment strategies include pre-treatment with pan-coronavirus fusion inhibitors like EK1 peptide (an amino acid modified OC43-HR2P) and TMPRSS2 inhibitors like Camostat mesylate, Nafamostat mesylate should be tested for the efficacy in these animal models before considering for further assessment. The neural tissues of animal models are beneficial to examine the SARS-CoV-2-induced modulation in ACE-2 [33, 177, 178]. Dysregulation of RAS systems in COVID-19 infection contributes to ischemic brain injury through small-vessel hypoperfusion and arterial atherothrombosis [179]. Molecular mechanisms regulating these processes can be deciphered using mice models of SARS-CoV-2 infection.
SARS-CoV and Models for CNS Research
Accumulating evidence has demonstrated the presence of coronaviruses in the autopsies isolated from CNS of patients suffering from MS, PD, and AD. Experimental studies have shown that human CoVs can easily infect neurons, glial cells viz., astrocytes, and microglia in primary cultures as well as immortalized human microglial cells [180]. This suggests that SARS-CoV-2 may use the brain as a reservoir, which potentially favors the development of neurodegenerative diseases [181]. Therefore, there is a need to analyze the effect of SARS-CoV-2 infection on CNS.
SARS-CoV and CNS Cell Lines
The existing data, which is available from research on SARS-CoV, showed approximately 78% nucleotide homology with SARS-CoV-2. However, there are no specific neural cell lines developed to study the models of SARS-CoV-2 [182]. Currently neural progenitor cells, neurons, and microglia cells (obtained from human induced pluripotent stem cells (hIPSCs)) are being used to ascertain the in vitro studies of SARS-CoV-2 viral infections and the impact of infection on cellular metabolism and various signaling cascades involved in cellular survival [182–184]. However, few other studies have used neurotropic human coronaviruses and neural cell lines such as human oligodendroglioma cell line HOG and rat glial tumor cell line C6. These cell lines are sensitive to SARS-CoV-2 infection and help to decipher the underlying virulence mechanisms through which the virus attacks the human CNS [185–187]. Even though both cell lines are reported to be sensitive to SARS-CoV infection, it was mentioned that viral replication is very low in cell lines such as Vero E6 and Caco-2 [188]. Miscellaneous neural cell lines viz., “human H4 brain neuroglioma cells, LA–N-5 human neuroblastoma cells, CHME-5 human fetal microglia cells, and U-373 MG and U-87 MG astrocytic cells” were also used for studying the infection ability of the HCoV-229E and HCoV-OC43 in the CNS [189–193]. Cultures of human primary neurons, glial cells such as astrocytes, oligodendrocytes, and microglia could also be used to study the virulence of the above viruses. Further studies are warranted to test the suitability of these neural cell lines to conduct experiments using SARS-CoV-2.
SARS-CoV-2 and Models of Brain Organoids
Organoids are the miniaturized, simplified, three-dimensional versions of an organ developed in vitro [194]. Organoids represent the cellular structure and functioning of a particular organ [195, 196]. The implementation of organoids could foster researchers to develop and ascertain the complex physiological or pathological processes in an in vivo system. SARS-CoV-2 infection, tropism, and potential treatments were examined in human organoids of the lung, liver, intestine, blood vessels, and kidney [196–198]. Currently, human brain organoids are being developed to study the pathophysiological aspects associated with SARS-CoV-2-induced alterations in the brain [198, 199]. These organoids are useful to study the early stages of neuronal development during COVID-19 infection.
SARS-CoV-2 infect mature cortical neurons that are present in brain organoids [182]. Besides, the neurodegenerative effects observed in SARS- CoV-2 infected cells are due to cellular death and hyperphosphorylation, followed by the mislocation of Tau protein. These changes were more evident in tauopathies or AD [182]. However, there is no productive viral replication observed in these cells during the initial phase of infection, which would support the hypothesis that the CNS can be considered as a long-term reservoir for the virus [181]. In contrast, Bullen et al. delineated overaccumulation of viral particles across neurons in brain organoid models between 6 and 72 h after SARS-CoV-2 infection [200]. This is indicating that an active replication was more evident during the initial phase of viral infection. Furthermore, the viral particles were noticed significantly across the neuronal soma as well as in neurites. Mesci et al. [201] have successfully implemented the brain organoid model to assess whether the SARS-CoV-2 could be able to infect neurons, NPCs, and other cortical neurons to foster the cell death accompanied by the failure of excitatory synapses. Also, the above work was examined for Sofosbuvir’s efficiency, which is an FDA-approved brain-penetrant antiviral drug for ( +) ss RNA viruses, as a part of therapeutic modality during SARS-CoV-2 infection [202]. This study has concluded that Sofosbuvir could reinstate the altered synaptogenesis and mitigate neural cell death induced by viral accumulation in these brain organoids. Another study reported that SARS-CoV-2 exhibits neuro-invasive property in human brain organoids, typically in NPCs and mature cortical neurons [183]. These cells are exemplified by the hypermetabolic state where the viral particles undergo accumulation across the endoplasmic reticulum-like structures. From these evidences, it is now confirmed that SARS-CoV-2 has the capability to utilize neural cell machinery to replicate in the cells. Furthermore, hypoxia, as well as extensive neuronal death, was more evident across the infected brain tissues with high-density SARS-CoV-2, suggesting that SARS-CoV-2 could foster bystander cell death [203]. This study also concluded that IgG antibodies generated against SARS-CoV-2 in the CSF of COVID-19 patients could confer blockade of SARS-CoV-2 infection in brain organoids [183]. Thus, these studies reported that SARS-CoV-2 could infect neural cells and invoke neurological complications with devastating adverse effects. In conclusion results of these studies depicted the immense potential of the usage of human brain organoids for the study of the SARS-CoV-2 effects in the CNS.
MHV-CoV Infection in Mice and Neural Complications
Mouse hepatitis virus (MHV) is a βCoV, which has no risk to humans but typically presents a similarity with other viruses from the same family viz., SARS-CoV, MERS-CoV, and SARS-CoV-2. Furthermore, this virus can cross CNS and invoke white matter lesions; hence this model could be proposed as a viral model of demyelinating disease [204, 205]. MHV can undergo replication in white matter, hence, is a useful model for the study of coronavirus-induced CNS infection. Neurotropic strains of MHV-CoV were previously reported to be implicated to cause acute and chronic demyelinating disease mediated by neuroinflammation [206, 207]. Based on the inoculation route and the MHV-CoV strain, it is now feasible to predict and identify the CNS region that was significantly affected. Inoculation with experimental MHV-A59 neurotropic strains could invoke an acute meningoencephalitis followed by the occurrence of subacute, chronic inflammatory demyelination in both brain and spinal cord [208]. Virus translocation from the initial site of inoculation in the brain to the spinal cord is caused by the transit of virus particles in neural and glial cells and mechanisms that involve the fusion of lipid membranes, probably during the virus internalization step [209]. Intranasal and intracranial inoculation of JHM-CoV induces similar symptoms in BALB/c mice to those caused by MHV-A59. After intranasal inoculation of mice, MHV-CoV accesses the CNS through the olfactory nerve and propagates from the olfactory system to limbic system structures and their connections with the brainstem [210].
In order to study the immune system role in demyelination induction caused by MHV infection, Wang et al. [211] treated infected animals with gamma radiation to cause immunosuppression and, subsequently, reconstituted immunity by transferring cells from other immunocompetent animals. The results concluded that demyelination was prevented by radiation and was reinstated again when the immunity was restored, indicating that immunity is directly involved in the demyelination process. Moreover, CD4 and CD8 T cells have been observed to play a critical role in developing the demyelinating process, with T cells being the most important for this process [212, 213]; MHV offers a unique model for studying host defense-mediated demyelination during chronic viral infection and acute phase of viral infection (for instance, SARS-CoV-2) [214].
COVID-19 and Impact on Neurodevelopment
The global COVID-19 pandemic raised concern for pregnant women regarding the outcomes of SARS-CoV-2 infections, as this viral infection may invoke potential fetal defects viz., long-term neurodevelopmental impacts [215].There are three primary considerations for a developing fetus:
Vertical transmission of the disease from the mother
The prenatal effects of maternal systemic infection on the fetus
The possible effects on placental functioning and consequent pregnancy outcomes [179]
The presence of ACE-2 receptors in the placenta suggests the potential risk of getting SARS-CoV-2 transmission. In addition to vertical transmission, the maternal infection may invoke neurodevelopmental alterations during fetal development. However, the SARS-CoV-2-induced neurodevelopmental alterations should be unraveled fully to understand the infection-induced pathophysiology in early pregnancy [216]. For instance, this infection could foster the incidence of cytokine storm accompanied by the modulation of maternal immune systems and generate a cascade of cytokines and chemokines (TNF-α, IL-6) and other immune alterations that may be transmitted to the fetus. Subsequently, the critically ill pregnant women with viral infection could be at a higher risk of placental hypoxia, compromising fetal oxygen supply consequently invoke defects in regional growth and brain development [217–219]. Thus, the impact of COVID-19 on pregnancy remains undetermined in terms of neurological complications in both mother and newborn. Even though reports suggested critical illness and maternal death in few cases, to date, no evidences are reported indicating pregnancy as one of the risk factors for acquiring COVID-19.
Proteins of Virus- and Host-Origin Involved in the Pathogenesis
S-Protein
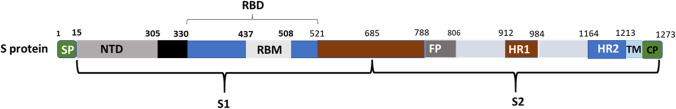
S-protein is one of the viral proteins, which consists of a large ectodomain, a single-pass transmembrane anchor, and a short intracellular tail (Fig. 5) [220]. Ectodomain consists of two subunits: viz., S1 (receptor-binding subunit) and S2 (membrane fusion subunit), serving as primary targets for human inventions. S1 and S2 subunits are highly conserved with 70% and 99% similarity with bat SARS-CoV and human SARS-CoV, respectively [1, 221]. S1 functional domains include the N-terminal domain (NTD), receptor-binding domain (RBD), and receptor-binding motif (RBM) (Fig. 5). S2 has a fusion peptide, heptad repeat 1 (HR1), heptad repeat 2 (HR2), transmembrane domain (TM), and a cytoplasmic domain (CP) (Fig. 5) [2, 59, 220]. Electron microscopy studies revealed that the spike appears as a clove-shaped trimer with three S1 heads and a trimeric S2 stalk [222–225]. The receptor-binding subunit interacts efficiently with various host receptors and facilitates the virus attachment on the host cell surface. The membrane fusion subunit fuses the host and viral membrane, mediating the entry of the virus into the host cells [226].
Fig. 5.
Structural motifs of S-protein: the S-protein of SARS-CoV-2 is composed of S1 and S2 subunits. Whereas the S1 domain is composed of N-terminal domain (NTD), receptor-binding domain (RBD), receptor-binding motif (RBM), the S2 domain is composed of fusion peptide, heptad repeat 1 (HR1), heptad repeat 2 (HR2), transmembrane domain (TM), and a cytoplasmic domain (CP)
ACE-2 receptor is the binding partner of SARS-CoV-2′s S-protein [2, 59]. Studies have reported and confirmed the existence of cross-reaction, by amino-acid sequence analysis of S1 subunit revealing 77% similarity of SARS-CoV-2 to SARS-CoV [29, 227, 228], while S2 subunit of SARS-CoV-2 was highly conserved and shared 99% homology with human SARS-CoV [1].
The difference in RBD of SARS-CoV and SARS-CoV-2 was that SARS-CoV specific ACE-2 binding neutralizing antibodies (m96, CR3014) failed to bind with the S-protein of SARS-CoV-2 [29]. Analysis of RBD of SARS-CoV and SARS-CoV-2 showed the presence of arginine (R426) in SARS-CoV RBD compared to asparagine (N439) in SARS-CoV-2, which leads to a significant decrease in the strong polar interactions [229]. Similarly, a replacement of valine (V404 in SARS-CoV) by lysine (K417 in SARS-CoV-2) on β6 formed an extra salt bridge with D30 on ACE-2 [228]. The structural changes in the RBM modulate the hACE-2-binding ridge into a more compact one, which facilitates better interaction with N-terminal hACE-2, making SARS-CoV-2 a more favorable binding partner [230] (Fig. 5).
TMPRSS2
TMPRSS2 is a cellular serine protease, which [57, 231, 232] plays a significant role in the entry of coronaviruses such as SARS-CoV and MERS-CoV into host cells [233, 234]. Several investigators have confirmed that TMPRSS2 causes S-protein priming for SARS-CoV-2 entry into primary target cells and enables the spreading of the virus in the infected host [33, 56, 235, 236]. Thus, TMPRSS2 is an attractive drug target for blocking the initial step of SARS-CoV-2 infection to avoid multiorgan dysfunction. However, the above intricate structure of S-protein interaction with TMPRSS2 is a challenging aspect for virologists to develop suitable therapeutic interventions against SARS-CoV-2.
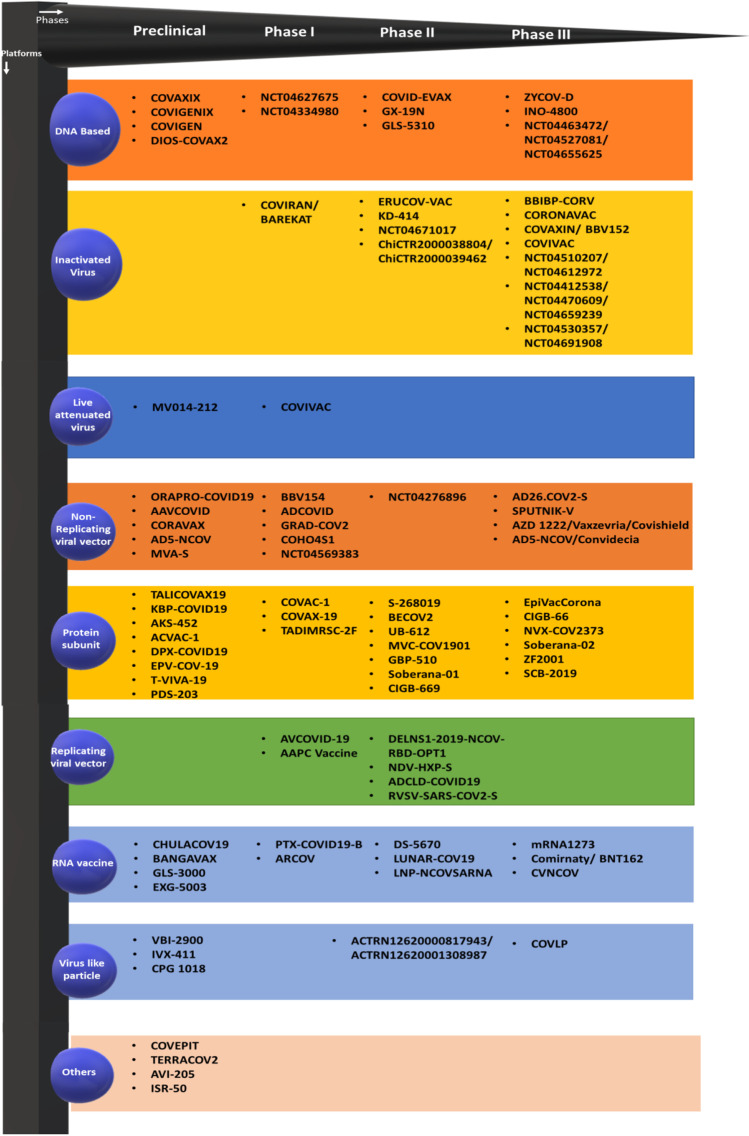
Targeting COVID-19 Using Vaccines
As of 3 April 2021, 83 vaccine candidates are currently in clinical trials on humans and 77 vaccine candidates are under investigation in animals. Among which 48 are in phase I, 33 in phase II, and 23 in phase III evaluation (Table 3, Fig. 6). Some of the vaccine candidates are currently in phase III clinical trials and the clinical data is supportive of large-scale manufacturing in several industrial production units worldwide with complete FDA approval [237].
Table 3.
List of US-FDA approved vaccines under clinical trials
| Vaccine name | Type of vaccine | Current stage of the clinical trial | Efficacy | Dosing regimen | Type of administration | Manufacturer of the vaccine |
|---|---|---|---|---|---|---|
| Comirnaty/tozinameran/BNT162b2 | mRNA vaccine | Phases 2, 3 | 95% | 2 doses, 3 weeks apart | Muscle injection | Pfizer and BioNTech |
| mRNA-1273 | mRNA vaccine | Phase 3 | 94.5% | 2 doses, 4 weeks apart | Muscle injection | Moderna |
| Sputnik V/Gam-Covid-Vac | Viral vector (Ad26, Ad5) | Phase 3 | 91.6% | 2 doses, 3 weeks apart | Muscle injection | Gamaleya Research Institute |
| AZD1222/Covishield | Viral vector (ChAd0 × 1) | Phases 2, 3 | 82.4% | 2 doses | Muscle injection | University of Oxford and AstraZeneca |
| Convidecia/Ad5-nCoV | Viral vector (Ad5) | Phase 3 | Unknown | Single dose | Muscle injection | CanSino Biologics |
| EpiVacCorona | Protein subunit | Phase 3 | Unknown | 2 doses, 3 weeks apart | Muscle injection | Vector Institute |
| BBIBP-CorV | Inactivated | Phase 3 | 79.34% | 2 doses, 3 weeks apart | Muscle injection | Sinopharm and Beijing Institute of Biological Products |
| CoronaVac | Inactivated | Phase 3 | 50.38% | 2 doses, 2 weeks apart | Muscle injection | Sinovac Biotech |
| Covaxin | Inactivated | Phase 3 | Unknown | 2 doses, 4 weeks apart | Unknown | Indian Council of Medical Research, National Institute of Virology and Bharat Biotech |
| Name not announced | Inactivated | Phase 3 | Unknown | Unknown | Unknown | Sinopharm and Wuhan Institute of Biological Products |
Fig. 6.
List of vaccines in various stages of clinical trials: current SARS-CoV-2 vaccine candidates targeting various biomolecules of the virus. Viral biomolecules targeting vaccine candidates include DNA-based vaccines, inactivated virus, live attenuated virus, non-replicating viral vector, protein subunit, replicating viral vector, RNA-based, and virus-like particle-based vaccines
The current COVID-19 vaccine candidates are antibody and/or T cell immune response promoting agents [237]. For instance, the protein-based vaccines are safe and induce immune responses through the adjuvants used along with the vaccine. Mainly, the S-protein, which is composed of S1 RBD, RBD-Fc, and N-terminal regions, could exert immune protection in several in vivo and nonhuman primate models [238–242]. Furthermore, the subunit vaccines could invoke immune responses in the host through one or more antigens in the presence of a suitable adjuvant. However, the immunization through subunit vaccine in animal models is capable of inducing fusion of S1 RBD with IgG1 FC portion consequently actuate generation of highly potent antibodies to foster neutralization of SARS-CoV [243, 244]. The clinical models of SARS-CoV-2 are yet to be examined for subunit vaccine as there is a very minimal success with clinical efficacy in animal models.
Ozonation of Vaccine
Systemic ozone therapy (OT) could be referred to as the potential approach useful in SARS-CoV-2 [245]. OT can be beneficial for the effective clinical management of complications secondary to SARS-CoV-2 [245]. OT improves oxygenation and exerts protection against lung fibrosis [246] and renal failure [247]. Furthermore, this therapy can stabilize the plasma levels in viral-infected patients by improving hepatic protein synthesis [248]. It could also exert a cytoprotective effect by preventing oxidative damage to the heart [249, 250], liver [251, 252], and renal tissues [253]. Systemic OT has the capacity to modulate the expression of the NF-κB/Nrf2 pathway and IL-6/IL-1β pathway consequently foster cytoprotection by blocking viral replication [245]. Previously, hormetic responses and oxidative preconditioning have been examined experimentally to the chronic oxidative stress during OT [254]. However, the hormetic responses of ozone were delineated vividly. For instance, a high dose of ozone can modulate gene transcription of pro-inflammatory cytokines and inflammatory cytokines while inducing a negative regulation of type 1 IFN in response to viral infection pathways [255]. Despite OT has no significant effect to kill the virus but it has the ability to modulate oxidative stress and inflammatory cytokines; hence OT could be considered as a complementary proposed treatment in COVID-19 patients. Exemplarily, the global vaccine preparation against HIV involves the prolonged and controlled exposure of plasma to a “precise dose of ozone” [245]. Similarly, therapeutic human albumin and ozonated ethyl oleate are predominantly mixed to enhance the absorption and boost the immune function through the vaccine [248, 256, 257]. This kind of ozonation of the vaccine approach towards the preparation of the COVID-19 vaccine can enhance the “oxidation of free viral components” thereby improves the efficacy.
Viral Vector-Based Vaccines.
These vaccines could promote the delivery of one or more antigens coded through a modified viral vector [258]. This technology promotes the delivery of antigens into the host cells and fosters the generation of both humoral and cell-based immune responses against viral pathogen [244, 259, 260]. The efficacy of viral vectors is yet to be examined against SARS-CoV and SARS- CoV-2. Previous reports delineated the efficacy of the modified vaccinia Ankara (MVA) vector, a live attenuated vector-based vaccine that encodes S-protein [261]. It induces a potent neutralizing antibody in mice, rabbits, and monkeys [262]. Immunization of mice models using recombinant adenovirus has been shown to induce neutralizing antibodies in serum and CD8 + T cells of lungs [263–266].
DNA vaccines consist of plasmid DNA molecules, which encode for immunogens and proven to be more effective than mRNA vaccines for stability and easy delivery [267]. However, their implications are constrained by the risk of getting mutations by integrating with the host genome [267, 268]. The passive transfer of sera from immunized mice with DNA that encodes the S-domain of MERS-CoV has been shown to protect naïve mice infected with MERS-CoV [269]. Another study showed that DNA encoding S1 and S-proteins invoke the generation of cross-neutralizing antibodies towards multiple MERS-CoV strains originated from humans and camels [270]. Furthermore, the immunization of mice with S-protein encoding DNA has been conducive to the generation of CD4 + and CD8 + T cells specific peptides, which consequently enhanced the extensive cytokine expression [271]. In the case of pseudotyped lentiviral vector-based DNA, the vaccine-induced potent neutralizing antibodies in SARS-CoV consequently invoked S-protein-specific CD4 + and CD8 + T cell immune responses in immunized volunteers [272]. A summary of the ongoing DNA/subunit/protein-based vaccine trials are provided in Table 2. However, the implications of these vaccine models in SARS-CoV-2 are constrained by the antibody-dependent enhancement (ADEs) and Th2-immunopathology.
Successful Phase II COVAXIN (Bharat Biotech)
BBV152 (COVAXIN) is a whole-virion β-propiolactone-inactivated SARS-CoV-2 vaccine investigated and formulated along with a toll-like receptor 7/8 agonist (imidazoquinoline molecule) to foster Th-1 immune responses through the intramuscular route of administration [273, 274]. A double-blind, multicenter, and randomized controlled phase I trial was conducted across 11 hospitals in India by Bharat Biotech. Further, this study assessed the safety and immunogenicity of BBV152 (Clinical Trials.gov NCT04471519) assessment of safety and immunogenicity of BBV152 [275]. However, additional studies are required to ascertain the cell-mediated responses.
Covishield is another vaccine developed by Serum Institute of India (SII) in collaboration with Oxford-AstraZeneca, UK, and Bharat Biotech. This vaccine was approved by the Drugs Controller General of India (DCGI) recently for emergency usage through the intramuscular route of administration in SARS-CoV-2 infected patients in India (DCGI, India).
Vaccine-Induced Neurological Complications
To date, 665 million vaccine doses have been administered worldwide. Several recent reports suggest that the COVID-19 vaccination has no- or minimal risk to the neurological system [171, 276]. However, mild side effects such as dizziness, headache, pain, muscle spasms, myalgia, and paresthesias were reported in the clinical trials of the vaccines during phase III study [276]. For instance, AZD1222 adenoviral vector vaccine administration during phase III trial in two patients was reported with neurological complications. Upon detailed investigation, it was concluded that one patient exhibited multiple sclerosis, which was undiagnosed at the time of vaccination, and the later reports concluded that the other factors might be contributing to this side effect [277–279]. Subsequently, these reports delineated that this vaccine had no neurological side effects and the study was resumed, with approvals in India, Argentina, and the UK [277]. In an mRNA vaccine trial, 7 out of 37,000 participants developed Bell’s palsy (a temporary weakness or paralysis of the muscles in the face); US-FDA concluded that the rate of the disease was not higher than expected in the population [280]. A vaccine candidate developed by Johnson & Johnson has been reported with GBS in two patients in the phase III trial. Among them, one participant was vaccinated and the other was a placebo, suggesting that there was no association between GBS and COVID-19 infection [281]. A case study by Waheed et al. reported the first case of GBS after 2 weeks of the first dose of Pfizer COVID-19 vaccine (mRNA vaccine) [171]. In rare case, the vaccine administration that was associated with tremor, diplopia (simultaneous perception of two images of a single object), tinnitus (experience of ringing or other noises in one or both the ears), dysphonia (abnormal voice), seizures, and reactivation of herpes zoster has been reported [276]. To date, 17 cases of stroke, 32 cases of GBS, 190 cases of Bell’s palsy, and 6 cases of encephalomyelitis have been reported in the “Vaccine Adverse Event Reporting System database” [276]. However, there is no significant report that suggests a higher rate of neurological complications with COVID-19 vaccination [276].
Conclusions
Infection with SARS-CoV-2, the culprit for the COVID-19 pandemic, has caused several health complications, including the disturbances associated with the neurological system and cognition-related behavioral changes. Fundamental molecular mechanisms that triggered these alterations are reported to be inflammation, induction of cell death, and poor cell-to-cell communications. However, further studies are warranted to address and further confirm (a) whether SARS-CoV-2 can directly enter the neuronal cells? If so, what is the route of entry? (b) The pathogenic responses triggered in infected cells? (c) Why only certain COVID-19 patients develop neurological complications? Moreover, (d) is there any association between age group and susceptibility to COVID-19 induced neurological damage? Further, it is also unknown whether the vaccines that the FDA approves could also extend protection to prevent the entry of SARS-CoV-2 into neuronal cells. Addressing these queries would likely provide clues and mechanisms that can be considered for developing better treatment agents and protection strategies from SARS-CoV-2 infections.
Acknowledgements
Dr. Gjumrakch Aliev (GA) would like to thank the GALLY International Research Institute, San Antonio, TX, USA. Prof. Aliev passed away in the month of December 2020. Chinnappa A. Uthaiah (CAU) would like to thank the Department of Science and Technology—Cognition Science Research Initiative (DST-CSRI), Govt of India for providing a Senior Research Fellowship as a part of research grant (No. SR/CSRI/44/2016); Suma M. Nataraj (SMN) would like to thank the Indian Council of Medical Research, Govt of India for sanctioning a research project (No. 54/06/2019-HUM/BMS); and SubbaRao V. Madhunapantula (SVM) thank the research grant award by the Department of Biotechnology, Govt of India (No. BT/PR29598/PFN/20/1392/2018). SVM would also like to thank the Special Interest Group in Cancer Biology and Cancer Stem Cells (SIG-CBCSC), JSS Academy of Higher Education & Research (JSS AHER), Mysore 570015, Karnataka, India.
Abbreviations
- COVID-19
Coronavirus disease
- SARS-CoV
Severe acute respiratory syndrome coronavirus
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- CoV
Coronavirus
- MERS
Middle East respiratory syndrome
- hCoV
Human coronavirus
- ACEIs
Angiotensin-converting enzyme inhibitors
- ARBs
Angiotensin II receptor blockers
- NTD
N-terminal domain
- RBD
Receptor-binding domain
- RBM
Receptor-binding motif
- RNA
Ribonucleic acid
- ORF
Open reading frame
- Nsp
Non-structural proteins
- S-protein
Spike protein
- N-protein
Nucleocapsid protein
- M-protein
Membrane protein
- E-protein
Envelope protein
- DC-SIGN
Dendritic cell-specific intercellular adhesion molecule-3-grabbing non-integrin
- L-SIGN
Liver/lymph node-specific intercellular adhesion molecules-3-grabbing non-integrin
- DPP4
Dipeptidyl peptidase 4
- HCQ
Hydroxychloroquine
- IFNs
Interferons
- RAS
Renin-angiotensin system
- ACE
Angiotensin-converting enzyme
- AT1R
Angiotensin type 1 receptor
- AT2R
Angiotensin type 2 receptor
- GPCRs
G-protein-coupled receptors
- TMPRSS2
Transmembrane serine protease 2
- PAMPs
Pathogen-associated molecular patterns
- US-FDA
US Food and Drug Administration
- IL
Interleukins
- BBB
Blood–brain barrier
- BAL
Bronchoalveolar lavage
- CNS
Central nervous system
- GFAp
Glial fibrillary acidic protein
- NfL
Neurofilament light chain
- MRI
Magnetic resonance imaging
- ICU
Intensive care unit
- ARDS
Acute respiratory distress syndrome
- PNS
Peripheral nervous system
- RT-PCR
Real-time polymerase chain reaction
- CSF
Cerebrospinal fluid
- BCSFB
Blood-cerebrospinal fluid barrier
- CP
Choroid plexus
- PD
Parkinson’s disease
- OE
Olfactory epithelium
- OECs
Olfactory ensheathing cells
- EV
Extracellular vesicles
- GCSF
Granulocyte colony-stimulating factor
- DDC
DOPA decarboxylase
- DMTs
Disease-modifying therapies
- MS
Multiple sclerosis
- Aβ
Beta-amyloid
- AD
Alzheimer’s disease
- AMP
Antimicrobial peptide
- hIPSCs
human induced pluripotent stem cells
- NPCs
Neural progenitor cells
- MHV
Mouse hepatitis virus
- NTD
N-terminal domain
- HR1
Heptad repeat 1
- HR2
Heptad repeat 2
- CP
Cytoplasmic domain
- TM
Transmembrane domain
- HT
Hydroxytyrosol
- OLE
Oleuropein aglycone
- OT
Ozone therapy
- GBS
Guillain–Barré syndrome
- ADEM
Acute disseminated encephalomyelitis
Author Contribution
Medha Karnik (MK), Narasimha M. Beeraka (NMB), Chinnappa A. Uthaiah (CAU), SubbaRao V. Madhunapantula (SVM), Suma M. Nataraj (SMN), Anjali Devi S. Bettadapura (ASB), and Gjumrakch Aliev (GA) conceptualized and designed the study. MK and NMB contributed equally to this work. MK, NMB, and CAU performed the literature analysis and wrote the original manuscript draft. MK, NMB, and SVM revised and improved the final draft. All authors have reviewed and approved the manuscript before submission.
Data availability
Not applicable.
Declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
All authors have reviewed and approved the manuscript before submission.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Medha Karnik and Narasimha M. Beeraka contributed equally to this article.
References
- 1.Chan JF-W, Kok K-H, Zhu Z, Chu H, To KK-W, Yuan S, Yuen K-Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerging microbes & infections. 2020;9(1):221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Q, Zhang Y, Wu L, Niu S, Song C, Zhang Z, Lu G, Qiao C, Hu Y, Yuen K-Y. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell. 2020;181(4):894–904.e899. doi: 10.1016/j.cell.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tyrrell D, Bynoe M. Cultivation of a novel type of common-cold virus in organ cultures. BMJ. 1965;1(5448):1467. doi: 10.1136/bmj.1.5448.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, Dequanter D, Blecic S, El Afia F, Distinguin L. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020;277(8):2251–2261. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan W-j, Ni Z-y, Hu Y, Liang W-h, Ou C-q, He J-x, Liu L, Shan H, Lei C-l, Hui DS. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cui J, Li F, Shi Z-L. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Liu Q, Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020;92(4):418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gordon DE, Jang GM, Bouhaddou M, Xu J, Obernier K, White KM, O’Meara MJ, Rezelj VV, Guo JZ, Swaney DL. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020;583(7816):459–468. doi: 10.1038/s41586-020-2286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain S, Chen Y, Yang Y, Xu J, Peng Y, Wu Y, Li Z, Zhu Y, Tien P, Guo D. Identification of novel subgenomic RNAs and noncanonical transcription initiation signals of severe acute respiratory syndrome coronavirus. J Virol. 2005;79(9):5288–5295. doi: 10.1128/JVI.79.9.5288-5295.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snijder EJ, Van Der Meer Y, Zevenhoven-Dobbe J, Onderwater JJ, Van Der Meulen J, Koerten HK, Mommaas AM. Ultrastructure and origin of membrane vesicles associated with the severe acute respiratory syndrome coronavirus replication complex. J Virol. 2006;80(12):5927–5940. doi: 10.1128/JVI.02501-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Demogines A, Farzan M, Sawyer SL. Evidence for ACE2-utilizing coronaviruses (CoVs) related to severe acute respiratory syndrome CoV in bats. J Virol. 2012;86(11):6350–6353. doi: 10.1128/JVI.00311-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neuman BW, Kiss G, Kunding AH, Bhella D, Baksh MF, Connelly S, Droese B, Klaus JP, Makino S, Sawicki SG. A structural analysis of M protein in coronavirus assembly and morphology. J Struct Biol. 2011;174(1):11–22. doi: 10.1016/j.jsb.2010.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeDiego ML, Álvarez E, Almazán F, Rejas MT, Lamirande E, Roberts A, Shieh W-J, Zaki SR, Subbarao K, Enjuanes L. A severe acute respiratory syndrome coronavirus that lacks the E gene is attenuated in vitro and in vivo. J Virol. 2007;81(4):1701–1713. doi: 10.1128/JVI.01467-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fehr A, HJ PSM, Bickerton E, Britton P (2015) An overview of their replication and pathogenesis; section 2 genomic organization. Methods in molecular biology. Springer 1282:1-23 [DOI] [PMC free article] [PubMed]
- 17.Cui L, Wang H, Ji Y, Yang J, Xu S, Huang X, Wang Z, Qin L, Tien P, Zhou X. The nucleocapsid protein of coronaviruses acts as a viral suppressor of RNA silencing in mammalian cells. J Virol. 2015;89(17):9029–9043. doi: 10.1128/JVI.01331-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angeletti S, Benvenuto D, Bianchi M, Giovanetti M, Pascarella S, Ciccozzi M. COVID-2019: the role of the nsp2 and nsp3 in its pathogenesis. J Med Virol. 2020;92(6):584–588. doi: 10.1002/jmv.25719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beeraka NM, Sadhu SP, Madhunapantula SV, Rao Pragada R, Svistunov AA, Nikolenko VN, Mikhaleva LM, Aliev G (2020) Strategies for targeting SARS CoV-2: small molecule inhibitors—the current status. Front Immunol 11 (2264). 10.3389/fimmu.2020.552925 [DOI] [PMC free article] [PubMed]
- 20.Yang D, Tong L, Wang D, Wang Y, Wang X, Bai C. Roles of CC chemokine receptors (CCRs) on lipopolysaccharide-induced acute lung injury. Respir Physiol Neurobiol. 2010;170(3):253–259. doi: 10.1016/j.resp.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 21.Bottemanne P, Paquot A, Ameraoui H, Alhouayek M, Muccioli GG. The α/β–hydrolase domain 6 inhibitor WWL70 decreases endotoxin-induced lung inflammation in mice, potential contribution of 2-arachidonoylglycerol, and lysoglycerophospholipids. FASEB J. 2019;33(6):7635–7646. doi: 10.1096/fj.201802259R. [DOI] [PubMed] [Google Scholar]
- 22.Chakraborty A, Koldobskiy MA, Bello NT, Maxwell M, Potter JJ, Juluri KR, Maag D, Kim S, Huang AS, Dailey MJ. Inositol pyrophosphates inhibit Akt signaling, thereby regulating insulin sensitivity and weight gain. Cell. 2010;143(6):897–910. doi: 10.1016/j.cell.2010.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kindrachuk J, Ork B, Hart BJ, Mazur S, Holbrook MR, Frieman MB, Traynor D, Johnson RF, Dyall J, Kuhn JH. Antiviral potential of ERK/MAPK and PI3K/AKT/mTOR signaling modulation for Middle East respiratory syndrome coronavirus infection as identified by temporal kinome analysis. Antimicrob Agents Chemother. 2015;59(2):1088–1099. doi: 10.1128/AAC.03659-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sisk JM, Frieman MB, Machamer CE. Coronavirus S protein-induced fusion is blocked prior to hemifusion by Abl kinase inhibitors. J Gen Virol. 2018;99(5):619. doi: 10.1099/jgv.0.001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheng H, Lear-Rooney CM, Johansen L, Varhegyi E, Chen ZW, Olinger GG, Rong L. Inhibition of Ebola and Marburg virus entry by G protein-coupled receptor antagonists. J Virol. 2015;89(19):9932–9938. doi: 10.1128/JVI.01337-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fatma B, Kumar R, Singh VA, Nehul S, Sharma R, Kesari P, Kuhn RJ, Tomar S. Alphavirus capsid protease inhibitors as potential antiviral agents for Chikungunya infection. Antiviral Res. 2020;179:104808. doi: 10.1016/j.antiviral.2020.104808. [DOI] [PubMed] [Google Scholar]
- 27.Wang C, Li W, Drabek D, Okba NM, van Haperen R, Osterhaus AD, van Kuppeveld FJ, Haagmans BL, Grosveld F, Bosch B-J. A human monoclonal antibody blocking SARS-CoV-2 infection. Nat Commun. 2020;11(1):1–6. doi: 10.1038/s41467-020-16256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monteil V, Kwon H, Prado P, Hagelkrüys A, Wimmer RA, Stahl M, Leopoldi A, Garreta E, Del Pozo CH, Prosper F. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181(4):905–913.e907. doi: 10.1016/j.cell.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yuan M, Wu NC, Zhu X, Lee C-CD, So RT, Lv H, Mok CK, Wilson IA. A highly conserved cryptic epitope in the receptor binding domains of SARS-CoV-2 and SARS-CoV. Science. 2020;368(6491):630–633. doi: 10.1126/science.abb7269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zumla A, Chan JF, Azhar EI, Hui DS, Yuen K-Y. Coronaviruses—drug discovery and therapeutic options. Nat Rev Drug Discovery. 2016;15(5):327–347. doi: 10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sawicki SG, Sawicki DL, Siddell SG. A contemporary view of coronavirus transcription. J Virol. 2007;81(1):20–29. doi: 10.1128/JVI.01358-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xia S, Liu M, Wang C, Xu W, Lan Q, Feng S, Qi F, Bao L, Du L, Liu S. Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res. 2020;30(4):343–355. doi: 10.1038/s41422-020-0305-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu N-H, Nitsche A. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280.e278. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323(18):1824–1836. doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 35.Bittmann S, Luchter E, Weissenstein A, Villalon G, Moschuring-Alieva E. TMPRSS2-inhibitors play a role in cell entry mechanism of COVID-19: an insight into camostat and nefamostat. J Regen Biol Med. 2020;2(2):1–3. [Google Scholar]
- 36.Sonawane K, Barale SS, Dhanavade MJ, Waghmare SR, Nadaf NH, Kamble SA, Mohammed AA, Makandar AM, Fandilolu PM, Dound AS (2020) Homology modeling and docking studiesof TMPRSS2 with experimentally known inhibitors camostatmesylate, nafamostat and bromhexine hydrochloride to controlSARS-coronavirus-2. ChemRxiv. 10.26434/chemrxiv.12162360.v1
- 37.Jankun J. COVID-19 pandemic; transmembrane protease serine 2 (TMPRSS2) inhibitors as potential drugs. Translation. 2020;7:1–5. doi: 10.46570/utjms.vol7-2020-361. [DOI] [Google Scholar]
- 38.Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275(43):33238–33243. doi: 10.1074/jbc.M002615200. [DOI] [PubMed] [Google Scholar]
- 40.Warner FJ, Lew RA, Smith AI, Lambert DW, Hooper NM, Turner AJ. Angiotensin-converting enzyme 2 (ACE2), but not ACE, is preferentially localized to the apical surface of polarized kidney cells. J Biol Chem. 2005;280(47):39353–39362. doi: 10.1074/jbc.M508914200. [DOI] [PubMed] [Google Scholar]
- 41.Hamming I, Timens W, Bulthuis M, Lely A, Gv Navis, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paizis G, Tikellis C, Cooper ME, Schembri JM, Lew RA, Smith AI, Shaw T, Warner FJ, Zuilli A, Burrell LM. Chronic liver injury in rats and humans upregulates the novel enzyme angiotensin converting enzyme 2. Gut. 2005;54(12):1790–1796. doi: 10.1136/gut.2004.062398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Doobay MF, Talman LS, Obr TD, Tian X, Davisson RL, Lazartigues E. Differential expression of neuronal ACE2 in transgenic mice with overexpression of the brain renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol. 2007;292(1):R373–R381. doi: 10.1152/ajpregu.00292.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hartupee J, Mann DL. Neurohormonal activation in heart failure with reduced ejection fraction. Nat Rev Cardiol. 2017;14(1):30–38. doi: 10.1038/nrcardio.2016.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hofmann H, Pyrc K, Van Der Hoek L, Geier M, Berkhout B, Pöhlmann S. Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry. Proc Natl Acad Sci. 2005;102(22):7988–7993. doi: 10.1073/pnas.0409465102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426(6965):450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gralinski LE, Menachery VD. Return of the coronavirus: 2019-nCoV. Viruses. 2020;12(2):135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, Zhong W, Hao P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, Donovan M, Woolf B, Robison K, Jeyaseelan R. A novel angiotensin-converting enzyme–related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9. Circ Res. 2000;87(5):e1–e9. doi: 10.1161/01.RES.87.5.e1. [DOI] [PubMed] [Google Scholar]
- 50.Zhang H, Wada J, Hida K, Tsuchiyama Y, Hiragushi K, Shikata K, Wang H, Lin S, Kanwar YS, Makino H. Collectrin, a collecting duct-specific transmembrane glycoprotein, is a novel homolog of ACE2 and is developmentally regulated in embryonic kidneys. J Biol Chem. 2001;276(20):17132–17139. doi: 10.1074/jbc.M006723200. [DOI] [PubMed] [Google Scholar]
- 51.Harding S, Vescovo G, Kirby M, Jones S, Gurden J, Poole-Wilson P. Contractile responses of isolated adult rat and rabbit cardiac myocytes to isoproterenol and calcium. J Mol Cell Cardiol. 1988;20(7):635–647. doi: 10.1016/S0022-2828(88)80121-4. [DOI] [PubMed] [Google Scholar]
- 52.Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, Yang P, Sarao R, Wada T, Leong-Poi H. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436(7047):112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, Huan Y, Yang P, Zhang Y, Deng W. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus–induced lung injury. Nat Med. 2005;11(8):875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simmons G, Zmora P, Gierer S, Heurich A, Pöhlmann S. Proteolytic activation of the SARS-coronavirus spike protein: cutting enzymes at the cutting edge of antiviral research. Antiviral Res. 2013;100(3):605–614. doi: 10.1016/j.antiviral.2013.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh C-L, Abiona O, Graham BS, McLellan JS. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Iwata-Yoshikawa N, Okamura T, Shimizu Y, Hasegawa H, Takeda M, Nagata N (2019) TMPRSS2 contributes to virus spread and immunopathology in - coronavirus infection. J Virol 93(6):e01815-18. 10.1128/JVI.01815-18 [DOI] [PMC free article] [PubMed]
- 57.Matsuyama S, Nagata N, Shirato K, Kawase M, Takeda M, Taguchi F. Efficient activation of the severe acute respiratory syndrome coronavirus spike protein by the transmembrane protease TMPRSS2. J Virol. 2010;84(24):12658–12664. doi: 10.1128/JVI.01542-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Belouzard S, Chu VC, Whittaker GR. Activation of the SARS coronavirus spike protein via sequential proteolytic cleavage at two distinct sites. Proc Natl Acad Sci. 2009;106(14):5871–5876. doi: 10.1073/pnas.0809524106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wan Y, Shang J, Graham R, Baric RS, Li F (2020) Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol 94(7):e00127–20 [DOI] [PMC free article] [PubMed]
- 60.Bosch BJ, Van der Zee R, De Haan CA, Rottier PJ. The coronavirus spike protein is a class I virus fusion protein: structural and functional characterization of the fusion core complex. J Virol. 2003;77(16):8801–8811. doi: 10.1128/JVI.77.16.8801-8811.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fehr AR, Perlman S (2015) Coronaviruses: an overview of their replication and pathogenesis. Methods in Molecular Biology (Clifton, N.J.) 1282:1–23. 10.1007/978-1-4939-2438-7_1 [DOI] [PMC free article] [PubMed]
- 62.Severe Covid-19 GWAS Group, Ellinghaus D, Degenhardt F, Bujanda L, Buti M, Albillos A, Invernizzi P, Fernández J, Prati D, Baselli G, Asselta R, Grimsrud MM, Milani C, Aziz F, Kässens J, May S, Wendorff M, Wienbrandt L, Uellendahl-Werth F, Zheng T, … Karlsen TH (2020) Genomewide association study of severe Covid-19 with respiratory failure. The New England Journal of Medicine 383(16):1522–1534 10.1056/NEJMoa2020283 [DOI] [PMC free article] [PubMed]
- 63.Rigat B, Hubert C, Alhenc-Gelas F, Cambien F, Corvol P, Soubrier F. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Investig. 1990;86(4):1343–1346. doi: 10.1172/JCI114844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–998. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- 65.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang X, Yu Y, Xu J, Shu H, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chai X, Hu L, Zhang Y, Han W, Lu Z, Ke A, Zhou J, Shi G, Fang N, Fan J (2020) Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. Biorxiv. 10.1101/2020.02.03.931766
- 68.Fan Z, Chen L, Li J, Cheng X, Yang J, Tian C, Zhang Y, Huang S, Liu Z, Cheng J. Clinical features of COVID-19-related liver functional abnormality. Clin Gastroenterol Hepatol. 2020;18(7):1561–1566. doi: 10.1016/j.cgh.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fan C, Lu W, Li K, Ding Y, Wang J. ACE2 expression in kidney and testis may cause kidney and testis infection in COVID-19 patients. Front Med. 2021;7:1045. doi: 10.3389/fmed.2020.563893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oudit G, Kassiri Z, Jiang C, Liu P, Poutanen S, Penninger J, Butany J. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39(7):618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu F, Long X, Zhang B, Zhang W, Chen X, Zhang Z. ACE2 expression in pancreas may cause pancreatic damage after SARS-CoV-2 infection. Clin Gastroenterol Hepatol. 2020;18(9):2128–2130.e2122. doi: 10.1016/j.cgh.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gomez-Pinedo U, Matias-Guiu J, Sanclemente-Alaman I, Moreno-Jimenez L, Montero-Escribano P, Matias-Guiu JA. Is the brain a reservoir organ for SARS-CoV2? J Med Virol. 2020;92(11):2354–2355. doi: 10.1002/jmv.26046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu Y, Sun W, Guo Y, Chen L, Zhang L, Zhao S, Long D, Yu L. Association between platelet parameters and mortality in coronavirus disease 2019: retrospective cohort study. Platelets. 2020;31(4):490–496. doi: 10.1080/09537104.2020.1754383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Betakova T, Kostrábová A, Lachova V, Turianová L. Cytokines induced during influenza virus infection. Curr Pharm Des. 2017;23(18):2616–2622. doi: 10.2174/1381612823666170316123736. [DOI] [PubMed] [Google Scholar]
- 75.Freeman CM, Martinez FJ, Han MK, Ames TM, Chensue SW, Todt JC, Arenberg DA, Meldrum CA, Getty C, McCloskey L. Lung dendritic cell expression of maturation molecules increases with worsening chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180(12):1179–1188. doi: 10.1164/rccm.200904-0552OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gu Y, Hsu AC-Y, Pang Z, Pan H, Zuo X, Wang G, Zheng J, Wang F. Role of the innate cytokine storm induced by the influenza A virus. Viral Immunol. 2019;32(6):244–251. doi: 10.1089/vim.2019.0032. [DOI] [PubMed] [Google Scholar]
- 77.England JT, Abdulla A, Biggs CM, Lee AY, Hay KA, Hoiland RL, Wellington CL, Sekhon M, Jamal S, Shojania K (2020) Weathering the COVID-19 storm: lessons from hematologic cytokine syndromes. Blood Reviews 45:100707. 10.1016/j.blre.2020.10070 [DOI] [PMC free article] [PubMed]
- 78.Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473–474. doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- 79.Zheng J. SARS-CoV-2: an emerging coronavirus that causes a global threat. Int J Biol Sci. 2020;16(10):1678. doi: 10.7150/ijbs.45053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nikpouraghdam M, Farahani AJ, Alishiri G, Heydari S, Ebrahimnia M, Samadinia H, Sepandi M, Jafari NJ, Izadi M, Qazvini A. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: a single center study. J Clin Virol. 2020;127:104378. doi: 10.1016/j.jcv.2020.104378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Huang J, Zheng M, Tang X, Chen Y, Tong A, Zhou L. Potential of SARS-CoV-2 to cause CNS infection: biologic fundamental and clinical experience. Front Neurol. 2020;11:659. doi: 10.3389/fneur.2020.00659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. China JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dube M, Le Coupanec A, Wong AHM, Rini JM, Desforges M, Talbot PJ (2018) Axonal transport enables neuron-to-neuron propagation of human coronavirus OC43. J Virol 92 (17). 10.1128/JVI.00404-18 [DOI] [PMC free article] [PubMed]
- 86.Talbot PJ, Ekande S, Cashman NR, Mounir S, Stewart JN. Neurotropism of human coronavirus 229E. Adv Exp Med Biol. 1993;342:339–346. doi: 10.1007/978-1-4615-2996-5_52. [DOI] [PubMed] [Google Scholar]
- 87.Li YC, Bai WZ, Hirano N, Hayashida T, Hashikawa T. Coronavirus infection of rat dorsal root ganglia: ultrastructural characterization of viral replication, transfer, and the early response of satellite cells. Virus Res. 2012;163(2):628–635. doi: 10.1016/j.virusres.2011.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Buzhdygan TP, DeOre BJ, Baldwin-Leclair A, Bullock TA, McGary HM, Khan JA, Razmpour R, Hale JF, Galie PA, Potula R. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood–brain barrier. Neurobiol Dis. 2020;146:105131. doi: 10.1016/j.nbd.2020.105131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wan Y, Shang J, Graham R, Baric RS, Li F (2020) Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol 94 (7). 10.1128/JVI.00127-20 [DOI] [PMC free article] [PubMed]
- 91.Kanberg N, Ashton NJ, Andersson L-M, Yilmaz A, Lindh M, Nilsson S, Price RW, Blennow K, Zetterberg H, Gisslén M. Neurochemical evidence of astrocytic and neuronal injury commonly found in COVID-19. Neurology. 2020;95(12):e1754–e1759. doi: 10.1212/WNL.0000000000010111. [DOI] [PubMed] [Google Scholar]
- 92.Coolen T, Lolli V, Sadeghi N, Rovai A, Trotta N, Taccone FS, Creteur J, Henrard S, Goffard JC, Dewitte O, Naeije G, Goldman S, De Tiege X (2020) Early postmortem brain MRI findings in COVID-19 non-survivors. Neurology 95(14):e2016–e2027. 10.1212/WNL.0000000000010116 [DOI] [PubMed]
- 93.Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, Collange O, Boulay C, Fafi-Kremer S, Ohana M, Anheim M, Meziani F (2020) Neurologic features in severe SARS-CoV-2 infection. N Engl J Med 382(23):2268–2270. 10.1056/NEJMc2008597 [DOI] [PMC free article] [PubMed]
- 94.Garg RK. Spectrum of neurological manifestations in Covid-19: a review. Neurol India. 2020;68(3):560. doi: 10.4103/0028-3886.289000. [DOI] [PubMed] [Google Scholar]
- 95.Varatharaj A, Thomas N, Ellul MA, Davies NW, Pollak TA, Tenorio EL, Sultan M, Easton A, Breen G, Zandi M. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. The Lancet Psychiatry. 2020;7(10):875–882. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Abdel-Mannan O, Eyre M, Löbel U, Bamford A, Eltze C, Hameed B, Hemingway C, Hacohen Y. Neurologic and radiographic findings associated with COVID-19 infection in children. JAMA Neurol. 2020;77(11):1440–1445. doi: 10.1001/jamaneurol.2020.2687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, Sánchez-Larsen Á, Layos-Romero A, García-García J, González E, Redondo-Peñas I, Perona-Moratalla AB, Del Valle-Pérez JA. Neurologic manifestations in hospitalized patients with COVID-19: the ALBACOVID registry. Neurology. 2020;95(8):e1060–e1070. doi: 10.1212/WNL.0000000000009937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kamil K, Yazid MD, Idrus RBH, Das S, Kumar J. Peripheral demyelinating diseases: from biology to translational medicine. Front Neurol. 2019;10:87. doi: 10.3389/fneur.2019.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gowrisankar YV, Clark MA. Angiotensin II regulation of angiotensin-converting enzymes in spontaneously hypertensive rat primary astrocyte cultures. J Neurochem. 2016;138(1):74–85. doi: 10.1111/jnc.13641. [DOI] [PubMed] [Google Scholar]
- 100.Li N, Ma WT, Pang M, Fan QL, Hua JL. The commensal microbiota and viral infection: a comprehensive review. Front Immunol. 2019;10:1551. doi: 10.3389/fimmu.2019.01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, Donovan M, Woolf B, Robison K, Jeyaseelan R, Breitbart RE, Acton S. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9. Circ Res. 2000;87(5):E1–9. doi: 10.1161/01.res.87.5.e1. [DOI] [PubMed] [Google Scholar]
- 102.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xiao L, Haack KK, Zucker IH. Angiotensin II regulates ACE and ACE2 in neurons through p38 mitogen-activated protein kinase and extracellular signal-regulated kinase 1/2 signaling. Am J Physiol Cell Physiol. 2013;304(11):C1073–1079. doi: 10.1152/ajpcell.00364.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jarrahi A, Ahluwalia M, Khodadadi H, Salles EdSL, Kolhe R, Hess DC, Vale F, Kumar M, Baban B, Vaibhav K. Neurological consequences of COVID-19: what have we learned and where do we go from here? J Neuroinflammation. 2020;17(1):1–12. doi: 10.1186/s12974-020-01957-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yeh EA, Collins A, Cohen ME, Duffner PK, Faden H. Detection of coronavirus in the central nervous system of a child with acute disseminated encephalomyelitis. Pediatrics. 2004;113(1 Pt 1):e73–76. doi: 10.1542/peds.113.1.e73. [DOI] [PubMed] [Google Scholar]
- 106.Hui DSC, Zumla A. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am. 2019;33(4):869–889. doi: 10.1016/j.idc.2019.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gassen NC, Papies J, Bajaj T, Dethloff F, Emanuel J, Weckmann K, Heinz DE, Heinemann N, Lennarz M, Richter A (2020) Analysis of SARS-CoV-2-controlled autophagy reveals spermidine, MK-2206, and niclosamide as putative antiviral therapeutics. BioRxiv. 10.1101/2020.04.15.997254
- 108.Ll X, Shi F, Tan Z, Li Y, Bode AM, Cao Y. Mitochondrial network structure homeostasis and cell death. Cancer Sci. 2018;109(12):3686–3694. doi: 10.1111/cas.13830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang Y, Cao Y, Yamada S, Thirunavukkarasu M, Nin V, Joshi M, Rishi MT, Bhattacharya S, Camacho-Pereira J, Sharma AK (2015) Cardiomyopathy and worsened ischemic heart failure in SM22-α Cre-mediated neuropilin-1 null mice: dysregulation of PGC1α and mitochondrial homeostasis. Arterioscler Thromb Vasc Biol 35(6):1401–1412 [DOI] [PMC free article] [PubMed]
- 110.Chen K, Xu Z, Liu Y, Wang Z, Li Y, Xu X, Chen C, Xia T, Liao Q, Yao Y (2017) Irisin protects mitochondria function during pulmonary ischemia/reperfusion injury. Sci Transl Med 9(418):eaao6298. 10.1126/scitranslmed.aao6298 [DOI] [PMC free article] [PubMed]
- 111.de Oliveira M, De Sibio MT, Mathias LS, Rodrigues BM, Sakalem ME, Nogueira CR (2020) Irisin modulates genes associated with severe coronavirus disease (COVID-19) outcome in human subcutaneous adipocytes cell culture. Mol Cell Endocrinol 515:110917 [DOI] [PMC free article] [PubMed]
- 112.Korta P, Pocheć E, Mazur-Biały A. Irisin as a multifunctional protein: implications for health and certain diseases. Medicina. 2019;55(8):485. doi: 10.3390/medicina55080485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nunn AV, Guy GW, Brysch W, Botchway SW, Frasch W, Calabrese EJ, Bell JD. SARS-CoV-2 and mitochondrial health: implications of lifestyle and ageing. Immun Ageing. 2020;17(1):1–21. doi: 10.1186/s12979-020-00204-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Monlun M, Hyernard C, Blanco P, Lartigue L, Faustin B. Mitochondria as molecular platforms integrating multiple innate immune signalings. J Mol Biol. 2017;429(1):1–13. doi: 10.1016/j.jmb.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 115.Tiku V, Tan M-W, Dikic I. Mitochondrial functions in infection and immunity. Trends Cell Biol. 2020;30(4):263–275. doi: 10.1016/j.tcb.2020.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Nunn AV, Bell JD, Guy GW. Lifestyle-induced metabolic inflexibility and accelerated ageing syndrome: insulin resistance, friend or foe? Nutr Metab. 2009;6(1):1–26. doi: 10.1186/1743-7075-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.van der Zalm I, van der Valk E, Wester V, Nagtzaam N, van Rossum E, Leenen P, Dik W. Obesity-associated T-cell and macrophage activation improve partly after a lifestyle intervention. Int J Obes. 2020;44(9):1838–1850. doi: 10.1038/s41366-020-0615-6. [DOI] [PubMed] [Google Scholar]
- 118.Petersen AMW, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005;98(4):1154–1162. doi: 10.1152/japplphysiol.00164.2004. [DOI] [PubMed] [Google Scholar]
- 119.Yu L, Chen X, Wang L, Chen S. Oncogenic virus-induced aerobic glycolysis and tumorigenesis. J Cancer. 2018;9(20):3699. doi: 10.7150/jca.27279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Leon J, Acuña-Castroviejo D, Sainz RM, Mayo JC, Tan D-X, Reiter RJ. Melatonin and mitochondrial function. Life Sci. 2004;75(7):765–790. doi: 10.1016/j.lfs.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 121.Reiter RJ, Sharma R, Ma Q, Dominquez-Rodriguez A, Marik PE, Abreu-Gonzalez P. Melatonin inhibits COVID-19-induced cytokine storm by reversing aerobic glycolysis in immune cells: a mechanistic analysis. Medicine in drug discovery. 2020;6:100044. doi: 10.1016/j.medidd.2020.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Calabrese V, Cornelius C, Dinkova-Kostova AT, Calabrese EJ, Mattson MP. Cellular stress responses, the hormesis paradigm, and vitagenes: novel targets for therapeutic intervention in neurodegenerative disorders. Antioxid Redox Signal. 2010;13(11):1763–1811. doi: 10.1089/ars.2009.3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kennedy RB, Ovsyannikova IG, Haralambieva IH, Oberg AL, Zimmermann MT, Grill DE, Poland GA. Immunosenescence-related transcriptomic and immunologic changes in older individuals following influenza vaccination. Front Immunol. 2016;7:450. doi: 10.3389/fimmu.2016.00450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Takeda Y, Jamsransuren D, Matsuda S, Crea R, Ogawa H. The SARS-CoV-2-inactivating activity of hydroxytyrosol-rich aqueous olive pulp extract (HIDROX®) and its use as a virucidal cream for topical application. Viruses. 2021;13(2):232. doi: 10.3390/v13020232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Brunetti G, Di Rosa G, Scuto M, Leri M, Stefani M, Schmitz-Linneweber C, Calabrese V, Saul N. Healthspan maintenance and prevention of Parkinson’s-like phenotypes with hydroxytyrosol and oleuropein aglycone in C. elegans. Int J Mol Sci. 2020;21(7):2588. doi: 10.3390/ijms21072588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Siracusa R, Fusco R, Peritore AF, Cordaro M, D’Amico R, Genovese T, Gugliandolo E, Crupi R, Smeriglio A, Mandalari G. The antioxidant and anti-inflammatory properties of Anacardium occidentale L. cashew nuts in a mouse model of colitis. Nutrients. 2020;12(3):834. doi: 10.3390/nu12030834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Frasca D, Blomberg BB. The impact of obesity and metabolic syndrome on vaccination success. Vaccines for older adults. 2020;43:86–97. doi: 10.1159/000504440. [DOI] [PubMed] [Google Scholar]
- 128.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger KA, Skliut M, Weinberger J, Dangayach NS, Bederson JB, Tuhrim S, Fifi JT. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382(20):e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Pleasure SJ, Green AJ, Josephson SA. The spectrum of neurologic disease in the severe acute respiratory syndrome coronavirus 2 pandemic infection: neurologists move to the frontlines. JAMA Neurol. 2020;77(6):679–680. doi: 10.1001/jamaneurol.2020.1065. [DOI] [PubMed] [Google Scholar]
- 130.Yavarpour-Bali H, Ghasemi-Kasman M (2020) Update on neurological manifestations of COVID-19. Life Sciences 257:118063. 10.1016/j.lfs.2020.118063 [DOI] [PMC free article] [PubMed]
- 131.Nemoto W, Yamagata R, Nakagawasai O, Nakagawa K, Hung W-Y, Fujita M, Tadano T, Tan-No K. Effect of spinal angiotensin-converting enzyme 2 activation on the formalin-induced nociceptive response in mice. Eur J Pharmacol. 2020;872:172950. doi: 10.1016/j.ejphar.2020.172950. [DOI] [PubMed] [Google Scholar]
- 132.Zhao K, Huang J, Dai D, Feng Y, Liu L, Nie S (2020) Acute myelitis after SARS-CoV-2 infection: a case report. MedRxiv. 10.1101/2020.03.16.20035105
- 133.Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82(15):7264–7275. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Butowt R, Bilinska K. SARS-CoV-2: olfaction, brain infection, and the urgent need for clinical samples allowing earlier virus detection. ACS Chem Neurosci. 2020;11(9):1200–1203. doi: 10.1021/acschemneuro.0c00172. [DOI] [PubMed] [Google Scholar]
- 135.Harberts E, Yao K, Wohler JE, Maric D, Ohayon J, Henkin R, Jacobson S. Human herpesvirus-6 entry into the central nervous system through the olfactory pathway. Proc Natl Acad Sci U S A. 2011;108(33):13734–13739. doi: 10.1073/pnas.1105143108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Attoub S, Hassan AH, Vanhoecke B, Iratni R, Takahashi T, Gaben A-M, Bracke M, Awad S, John A, Kamalboor HA. Inhibition of cell survival, invasion, tumor growth and histone deacetylase activity by the dietary flavonoid luteolin in human epithelioid cancer cells. Eur J Pharmacol. 2011;651(1–3):18–25. doi: 10.1016/j.ejphar.2010.10.063. [DOI] [PubMed] [Google Scholar]
- 137.Chow CCN, Magnussen J, Ip J, Su Y. Acute transverse myelitis in COVID-19 infection. BMJ Case Reports CP. 2020;13(8):e236720. doi: 10.1136/bcr-2020-236720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rietdijk CD, Perez-Pardo P, Garssen J, van Wezel RJ, Kraneveld AD. Exploring Braak’s hypothesis of Parkinson’s disease. Front Neurol. 2017;8:37. doi: 10.3389/fneur.2017.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Libbey JE, Kennett NJ, Wilcox KS, White HS, Fujinami RS. Interleukin-6, produced by resident cells of the central nervous system and infiltrating cells, contributes to the development of seizures following viral infection. J Virol. 2011;85(14):6913–6922. doi: 10.1128/JVI.00458-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Singhi P. Infectious causes of seizures and epilepsy in the developing world. Dev Med Child Neurol. 2011;53(7):600–609. doi: 10.1111/j.1469-8749.2011.03928.x. [DOI] [PubMed] [Google Scholar]
- 142.Pilotto A, Odolini S, Masciocchi S, Comelli A, Volonghi I, Gazzina S, Nocivelli S, Pezzini A, Foca E, Caruso A, Leonardi M, Pasolini MP, Gasparotti R, Castelli F, Ashton NJ, Blennow K, Zetterberg H, Padovani A. Steroid-responsive encephalitis in coronavirus disease 2019. Ann Neurol. 2020;88(2):423–427. doi: 10.1002/ana.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Durrani M, Kucharski K, Smith Z, Fien S. Acute transverse myelitis secondary to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a case report. Clin Pract Cases Emerg Med. 2020;4(3):344–348. doi: 10.5811/cpcem.2020.6.48462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, Collaboration HAS, UK, COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Soler ZM, Patel ZM, Turner JH, Holbrook EH. A primer on viral-associated olfactory loss in the era of COVID-19. International Forum of Allergy & Rhinology 10(7): 814–820. 10.1002/alr.22578 [DOI] [PMC free article] [PubMed]
- 146.Vaira LA, Salzano G, Fois AG, Piombino P, De Riu G. Potential pathogenesis of ageusia and anosmia in COVID-19 patients. Int Forum Allergy Rhinol. 2020;10(9):1103–1104. doi: 10.1002/alr.22593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Liu Y-Z, Wang Y-X, Jiang C-L. Inflammation: the common pathway of stress-related diseases. Front Hum Neurosci. 2017;11:316. doi: 10.3389/fnhum.2017.00316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Vriend C, Pattij T, van der Werf YD, Voorn P, Booij J, Rutten S, Berendse HW, van den Heuvel OA. Depression and impulse control disorders in Parkinson’s disease: two sides of the same coin? Neurosci Biobehav Rev. 2014;38:60–71. doi: 10.1016/j.neubiorev.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 149.Zach H, Dirkx MF, Pasman JW, Bloem BR, Helmich RC. Cognitive stress reduces the effect of levodopa on Parkinson’s resting tremor. CNS Neurosci Ther. 2017;23(3):209–215. doi: 10.1111/cns.12670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ehgoetz Martens KA, Hall JM, Georgiades MJ, Gilat M, Walton CC, Matar E, Lewis SJG, Shine JM. The functional network signature of heterogeneity in freezing of gait. Brain. 2018;141(4):1145–1160. doi: 10.1093/brain/awy019. [DOI] [PubMed] [Google Scholar]
- 151.Macht M, Kaussner Y, Moller JC, Stiasny-Kolster K, Eggert KM, Kruger HP, Ellgring H. Predictors of freezing in Parkinson’s disease: a survey of 6,620 patients. Mov Disord. 2007;22(7):953–956. doi: 10.1002/mds.21458. [DOI] [PubMed] [Google Scholar]
- 152.Zach H, Dirkx M, Pasman JW, Bloem BR, Helmich RC. The patient’s perspective: the effect of levodopa on Parkinson symptoms. Parkinsonism Relat Disord. 2017;35:48–54. doi: 10.1016/j.parkreldis.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 153.Nataf S. An alteration of the dopamine synthetic pathway is possibly involved in the pathophysiology of COVID-19. J Med Virol. 2020;92(10):1743–1744. doi: 10.1002/jmv.25826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Silhol F, Sarlon G, Deharo J-C, Vaïsse B (2020) Downregulation of ACE2 induces overstimulation of the renin–angiotensin system in COVID-19: should we block the renin–angiotensin system? Hypertension Research: Official Journal of the Japanese Society of Hypertension 43(8):854–856. 10.1038/s41440-020-0476-3 [DOI] [PMC free article] [PubMed]
- 155.Carod-Artal FJ. Neurological complications of coronavirus and COVID-19. Rev Neurol. 2020;70(9):311–322. doi: 10.33588/rn.7009.2020179. [DOI] [PubMed] [Google Scholar]
- 156.Barzegar M, Mirmosayyeb O, Nehzat N, Sarrafi R, Khorvash F, Maghzi AH, Shaygannejad V (2020) COVID-19 infection in a patient with multiple sclerosis treated with fingolimod. Neurol Neuroimmunol Neuroinflamm 7(4). 10.1212/NXI.0000000000000753 [DOI] [PMC free article] [PubMed]
- 157.Foerch C, Friedauer L, Bauer B, Wolf T, Adam EH. Severe COVID-19 infection in a patient with multiple sclerosis treated with fingolimod. Mult Scler Relat Disord. 2020;42:102180. doi: 10.1016/j.msard.2020.102180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Berger JR, Brandstadter R, Bar-Or A (2020) COVID-19 and MS disease-modifying therapies. Neurology-Neuroimmunology Neuroinflammation 7(4):e761. 10.1212/NXI.0000000000000761 [DOI] [PMC free article] [PubMed]
- 159.Abate G, Memo M, & Uberti D (2020) Impact of COVID-19 on alzheimer's Disease Risk: Viewpoint for Research Action. Healthcare (Basel, Switzerland) 8(3):286. 10.3390/healthcare8030286 [DOI] [PMC free article] [PubMed]
- 160.Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med. 2016;8(6):595–608. doi: 10.15252/emmm.201606210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Serrano-Pozo A, Frosch MP, Masliah E, Hyman BT. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med. 2011;1(1):a006189. doi: 10.1101/cshperspect.a006189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman B, Burton MA, Goldstein LE, Duong S, Tanzi RE. The Alzheimer’s disease-associated amyloid β-protein is an antimicrobial peptide. PLoS ONE. 2010;5(3):e9505. doi: 10.1371/journal.pone.0009505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Caress JB, Castoro RJ, Simmons Z, Scelsa SN, Lewis RA, Ahlawat A, Narayanaswami P. COVID-19–associated Guillain-Barré syndrome: the early pandemic experience. Muscle Nerve. 2020;62(4):485–491. doi: 10.1002/mus.27024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lunn MP, Cornblath DR, Jacobs BC, Querol L, van Doorn PA, Hughes RA, Willison HJ. COVID-19 vaccine and Guillain-Barré syndrome: let’s not leap to associations. Brain. 2021;144(2):357–360. doi: 10.1093/brain/awaa444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Haber P, Sejvar J, Mikaeloff Y, DeStefano F. Vaccines and Guillain-Barre syndrome. Drug Saf. 2009;32(4):309–323. doi: 10.2165/00002018-200932040-00005. [DOI] [PubMed] [Google Scholar]
- 166.Zhao H, Shen D, Zhou H, Liu J, Chen S (2020) Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol 19(5):383–384 [DOI] [PMC free article] [PubMed]
- 167.Bhandari R, Khanna G, Kaushik D, Kuhad A (2021) Divulging the intricacies of crosstalk between NF-Kb and Nrf2-Keap1 pathway in neurological complications of COVID-19. Molecular Neurobiology:1–15. 10.1007/s12035-021-02344-7 [DOI] [PMC free article] [PubMed]
- 168.Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, Cuzzoni MG, Franciotta D, Baldanti F, Daturi R, Postorino P. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020;382(26):2574–2576. doi: 10.1056/NEJMc2009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Gutiérrez-Ortiz C, Méndez-Guerrero A, Rodrigo-Rey S, San Pedro-Murillo E, Bermejo-Guerrero L, Gordo-Mañas R, de Aragón-Gómez F, Benito-León J. Miller Fisher Syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020;95(5):e601–e605. doi: 10.1212/WNL.0000000000009619. [DOI] [PubMed] [Google Scholar]
- 170.Pfefferkorn T, Dabitz R, von Wernitz-Keibel T, Aufenanger J, Nowak-Machen M, Janssen H. Acute polyradiculoneuritis with locked-in syndrome in a patient with Covid-19. J Neurol. 2020;267:1883–1884. doi: 10.1007/s00415-020-09897-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Waheed S, Bayas A, Hindi F, Rizvi Z, Espinosa PS (2021) Neurological complications of COVID-19: Guillain-Barre syndrome following Pfizer COVID-19 vaccine. Cureus 13(2):e13426. 10.7759/cureus [DOI] [PMC free article] [PubMed]
- 172.Parsons T, Banks S, Bae C, Gelber J, Alahmadi H, Tichauer M. COVID-19-associated acute disseminated encephalomyelitis (ADEM) J Neurol. 2020;267:2799–2802. doi: 10.1007/s00415-020-09951-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Madia F, Merico B, Primiano G, Cutuli SL, De Pascale G, Servidei S. Acute myopathic quadriplegia in patients with COVID-19 in the intensive care unit. Neurology. 2020;95(11):492–494. doi: 10.1212/WNL.0000000000010280. [DOI] [PubMed] [Google Scholar]
- 175.Tankisi H, Tankisi A, Harbo T, Markvardsen L, Andersen H, Pedersen T (2020) Critical illness myopathy as a consequence of Covid 19 infection. Clin Neurophysiol 131(8):1931 [DOI] [PMC free article] [PubMed]
- 176.Cockrell AS, Leist SR, Douglas MG, Baric RS. Modeling pathogenesis of emergent and pre-emergent human coronaviruses in mice. Mamm Genome. 2018;29(7–8):367–383. doi: 10.1007/s00335-018-9760-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.McKee DL, Sternberg A, Stange U, Laufer S, Naujokat C (2020) Candidate drugs against SARS-CoV-2 and COVID-19. Pharmacological Research 157:104859. 10.1016/j.phrs.2020.104859 [DOI] [PMC free article] [PubMed]
- 178.Wang X, Xia S, Zhu Y, Lu L, Jiang S (2021) Pan-coronavirus fusion inhibitors as the hope for today and tomorrow. Protein & Cell 12(2):84–88. 10.1007/s13238-020-00806-7 [DOI] [PMC free article] [PubMed]
- 179.Pantelis C, Jayaram M, Hannan AJ, Wesselingh R, Nithianantharajah J, Wannan CM, Syeda WT, Choy KC, Zantomio D, Christopoulos A, Velakoulis D, O'Brien T J (2020) Neurological, Neuropsychiatric and Neurodevelopmental Complications of COVID-19. Aust NZ J Psychiatry 0004867420961472. 10.1177/0004867420961472 [DOI] [PMC free article] [PubMed]
- 180.Rabaan AA, Al-Ahmed SH, Haque S, Sah R, Tiwari R, Malik YS, Dhama K, Yatoo MI, Bonilla-Aldana DK, Rodriguez-Morales AJ. SARS-CoV-2, SARS-CoV, and MERS-CoV: a comparative overview. Infez Med. 2020;28(2):174–184. [PubMed] [Google Scholar]
- 181.Gomez‐Pinedo U, Matias‐Guiu J, Sanclemente‐Alaman I, Moreno‐Jimenez L, Montero‐Escribano P (2020) SARS‐CoV2 as a potential trigger of neurodegenerative diseases. Movement Disorders [DOI] [PMC free article] [PubMed]
- 182.Ramani A, Müller L, Ostermann PN, Gabriel E, Abida-Islam P, Müller-Schiffmann A, Mariappan A, Goureau O, Gruell H, Walker A, Andrée M, Hauka S, Houwaart T, Dilthey A, Wohlgemuth K, Omran H, Klein F, Wieczorek D, Adams O, Timm J, … Gopalakrishnan J (2020) SARS-CoV-2 targets neurons of 3D human brain organoids. The EMBO Journal 39(20):e106230. 10.15252/embj.2020106230 [DOI] [PMC free article] [PubMed]
- 183.Song E, Zhang C, Israelow B, Lu-Culligan A, Prado AV, Skriabine S, Lu P, Weizman OE, Liu F, Dai Y, Szigeti-Buck K, Yasumoto Y, Wang G, Castaldi C, Heltke J, Ng E, Wheeler J, Alfajaro MM, Levavasseur E, Fontes B, … Iwasaki A (2020) Neuroinvasive potential of SARS-CoV-2 revealed in a human brain organoid model. bioRxiv:the preprint server for biology, 2020.06.25.169946. 10.1101/2020.06.25.169946
- 184.Yang L, Han Y, Nilsson-Payant BE, Gupta V, Wang P, Duan X, Tang X, Zhu J, Zhao Z, Jaffré F. A human pluripotent stem cell-based platform to study SARS-CoV-2 tropism and model virus infection in human cells and organoids. Cell stem cell. 2020;27(1):125–136.e127. doi: 10.1016/j.stem.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Post GR, Dawson G. Characterization of a cell line derived from a human oligodendroglioma. Mol Chem Neuropathol. 1992;16(3):303–317. doi: 10.1007/BF03159976. [DOI] [PubMed] [Google Scholar]
- 186.De Kleijn K, Zuure WA, Peijnenborg J, Heuvelmans JM, Martens GJ. Reappraisal of human HOG and MO3. 13 cell lines as a model to study oligodendrocyte functioning. Cells. 2019;8(9):1096. doi: 10.3390/cells8091096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Benda P, Lightbody J, Sato G, Levine L, Sweet W. Differentiated rat glial cell strain in tissue culture. Science. 1968;161(3839):370–371. doi: 10.1126/science.161.3839.370. [DOI] [PubMed] [Google Scholar]
- 188.Yamashita M, Yamate M, Li G-M, Ikuta K. Susceptibility of human and rat neural cell lines to infection by SARS-coronavirus. Biochem Biophys Res Commun. 2005;334(1):79–85. doi: 10.1016/j.bbrc.2005.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Arbour N, Côté G, Lachance C, Tardieu M, Cashman NR, Talbot PJ. Acute and persistent infection of human neural cell lines by human coronavirus OC43. J Virol. 1999;73(4):3338–3350. doi: 10.1128/JVI.73.4.3338-3350.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Favreau DJ, Meessen-Pinard M, Desforges M, Talbot PJ. Human coronavirus-induced neuronal programmed cell death is cyclophilin d dependent and potentially caspase dispensable. J Virol. 2012;86(1):81–93. doi: 10.1128/JVI.06062-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Lachance C, Arbour N, Cashman NR, Talbot PJ. Involvement of aminopeptidase N (CD13) in infection of human neural cells by human coronavirus 229E. J Virol. 1998;72(8):6511–6519. doi: 10.1128/JVI.72.8.6511-6519.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Meessen-Pinard M, Le Coupanec A, Desforges M, Talbot PJ (2016) Pivotal role of receptor-interacting protein kinase 1 and mixed lineage kinase domain-like in neuronal cell death induced by the human neuroinvasive coronavirus OC43. J Virol 91(1):e01513-16. 10.1128/JVI.01513-16 [DOI] [PMC free article] [PubMed]
- 193.St-Jean JR, Desforges M, Talbot PJ (2006) Genetic evolution of human coronavirus OC43 in neural cell culture. Adv Exp Med Biol 581:499–502. 10.1007/978-0-387-33012-9_88 [DOI] [PMC free article] [PubMed]
- 194.Fatehullah A, Tan SH, Barker N. Organoids as an in vitro model of human development and disease. Nat Cell Biol. 2016;18(3):246–254. doi: 10.1038/ncb3312. [DOI] [PubMed] [Google Scholar]
- 195.Dutta D, Heo I, Clevers H. Disease modeling in stem cell-derived 3D organoid systems. Trends Mol Med. 2017;23(5):393–410. doi: 10.1016/j.molmed.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 196.Rossi G, Manfrin A, Lutolf MP. Progress and potential in organoid research. Nat Rev Genet. 2018;19(11):671–687. doi: 10.1038/s41576-018-0051-9. [DOI] [PubMed] [Google Scholar]
- 197.Busquet F, Hartung T, Pallocca G, Rovida C, Leist M (2020) Harnessing the power of novel animal-free test methods for the development of COVID-19 drugs and vaccines. Arch Toxicol 94(6):2263–2272. 10.1007/s00204-020-02787-2 [DOI] [PMC free article] [PubMed]
- 198.Takayama K. In vitro and animal models for SARS-CoV-2 research. Trends Pharmacol Sci. 2020;41(8):513–517. doi: 10.1016/j.tips.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Harschnitz O, Studer L (2021) Human stem cell models to study host-virus interactions in the central nervous system. Nature reviews. Immunology 10.1038/s41577-020-00474-y. 10.1038/s41577-020-00474-y [DOI] [PMC free article] [PubMed]
- 200.Bullen CK, Hogberg HT, Bahadirli-Talbott A, Bishai WR, Hartung T, Keuthan C, Looney MM, Pekosz A, Romero JC, Sillé FC. Infectability of human BrainSphere neurons suggests neurotropism of SARS-CoV-2. ALTEX-Alternatives to animal experimentation. 2020;37(4):665–671. doi: 10.14573/altex.2006111. [DOI] [PubMed] [Google Scholar]
- 201.Mesci P, Macia A, Saleh A, Martin-Sancho L, Yin X, Snethlage C, Avansini S, Chanda S, Muotri A (2020) Sofosbuvir protects human brain organoids against SARS-CoV-2. bioRxiv. 10.1101/2020.05.30.125856
- 202.Sayad B, Sobhani M, Khodarahmi R. Sofosbuvir as repurposed antiviral drug against COVID-19: why were we convinced to evaluate the drug in a registered/approved clinical trial? Arch Med Res. 2020;51(6):577–581. doi: 10.1016/j.arcmed.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Simoneau CR, Ott M. Modeling multi-organ infection by SARS-CoV-2 using stem cell technology. Cell Stem Cell. 2020;27(6):859–868. doi: 10.1016/j.stem.2020.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Walsh KB, Edwards RA, Romero KM, Kotlajich MV, Stohlman SA, Lane TE. Expression of CXC chemokine ligand 10 from the mouse hepatitis virus genome results in protection from viral-induced neurological and liver disease. J Immunol. 2007;179(2):1155–1165. doi: 10.4049/jimmunol.179.2.1155. [DOI] [PubMed] [Google Scholar]
- 205.Savarin C, Bergmann CC. Fine tuning the cytokine storm by IFN and IL-10 following neurotropic coronavirus encephalomyelitis. Front Immunol. 2018;9:3022. doi: 10.3389/fimmu.2018.03022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wege H, Stühler A, Lassmann H, Wege H (1998) Coronavirus infection and demyelination. Sequence conservation of the S-gene during persistent infection of Lewis-rats. Advances in Experimental Medicine and Biology 440:767–773 [PubMed]
- 207.Zalinger ZB, Elliott R, Weiss SR. Role of the inflammasome-related cytokines Il-1 and Il-18 during infection with murine coronavirus. J Neurovirol. 2017;23(6):845–854. doi: 10.1007/s13365-017-0574-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Gruslin E, Moisan S, St-Pierre Y, Desforges M, Talbot PJ. Transcriptome profile within the mouse central nervous system and activation of myelin-reactive T cells following murine coronavirus infection. J Neuroimmunol. 2005;162(1–2):60–70. doi: 10.1016/j.jneuroim.2005.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Choi KS, Aizaki H, Lai MM. Murine coronavirus requires lipid rafts for virus entry and cell-cell fusion but not for virus release. J Virol. 2005;79(15):9862–9871. doi: 10.1128/JVI.79.15.9862-9871.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Singh M, Khan RS, Dine K, Das Sarma J, Shindler KS. Intracranial inoculation is more potent than intranasal inoculation for inducing optic neuritis in the mouse hepatitis virus-induced model of multiple sclerosis. Front Cell Infect Microbiol. 2018;8:311. doi: 10.3389/fcimb.2018.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Wang F-I, Stohlman SA, Fleming JO. Demyelination induced by murine hepatitis virus JHM strain (MHV-4) is immunologically mediated. J Neuroimmunol. 1990;30(1):31–41. doi: 10.1016/0165-5728(90)90050-W. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Dandekar AA, Perlman S. Virus-induced demyelination in nude mice is mediated by γδ T cells. Am J Pathol. 2002;161(4):1255–1263. doi: 10.1016/S0002-9440(10)64402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Glass WG, Chen BP, Liu MT, Lane TE (2002) Mouse hepatitis virus infection of the central nervous system: chemokine-mediated regulation of host defense and disease. Viral Immunol 15(2):261–272 [DOI] [PubMed]
- 214.Hosking MP, Lane TE (2010) The pathogenesis of murine coronavirus infection of the central nervous system. Crit Rev Immunol 30(2):119–130. 10.1615/critrevimmunol.v30.i2.20 [DOI] [PMC free article] [PubMed]
- 215.Madjunkov M, Dviri M, Librach C. A comprehensive review of the impact of COVID-19 on human reproductive biology, assisted reproduction care and pregnancy: a Canadian perspective. J Ovarian Res. 2020;13(1):1–18. doi: 10.1186/s13048-020-00737-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Meyer U. Neurodevelopmental resilience and susceptibility to maternal immune activation. Trends Neurosci. 2019;42(11):793–806. doi: 10.1016/j.tins.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 217.Choi GB, Yim YS, Wong H, Kim S, Kim H, Kim SV, Hoeffer CA, Littman DR, Huh JR. The maternal interleukin-17a pathway in mice promotes autism-like phenotypes in offspring. Science. 2016;351(6276):933–939. doi: 10.1126/science.aad0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.UK G (2020) COVID-19: investigation and initial clinical management of possible cases. Gov Uk:1–5
- 219.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, Oczkowski S, Levy MM, Derde L, Dzierba A, Du B, Aboodi M, Wunsch H, Cecconi M, Koh Y, Chertow DS, Maitland K, Alshamsi F, Belley-Cote E, Greco M, … Rhodes A (2020) Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Medicine 46(5):854–887. 10.1007/s00134-020-06022-5 [DOI] [PMC free article] [PubMed]
- 220.Li F. Structure, function, and evolution of coronavirus spike proteins. Annu Rev Virol. 2016;3:237–261. doi: 10.1146/annurev-virology-110615-042301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Malik YS, Sircar S, Bhat S, Sharun K, Dhama K, Dadar M, Tiwari R, Chaicumpa W. Emerging novel coronavirus (2019-nCoV)—current scenario, evolutionary perspective based on genome analysis and recent developments. Veterinary Quarterly. 2020;40(1):68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, Diz DI, Gallagher PE. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111(20):2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 224.Gao Y, Yan L, Huang Y, Liu F, Zhao Y, Cao L, Wang T, Sun Q, Ming Z, Zhang L. Structure of the RNA-dependent RNA polymerase from COVID-19 virus. Science. 2020;368(6492):779–782. doi: 10.1126/science.abb7498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Gorbalenya A, Baker S, Baric R, de Groot R, Drosten C, Gulyaeva A, Haagmans B, Lauber C, Leontovich A, Neuman B. The species severe acute respiratory syndrome related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Xia S, Zhu Y, Liu M, Lan Q, Xu W, Wu Y, Ying T, Liu S, Shi Z, Jiang S, & Lu L (2020) Fusion mechanism of 2019-nCoV and fusion inhibitors targeting HR1 domain in spike protein. Cellular & Molecular Immunology 17(7):765–767. 10.1038/s41423-020-0374-2 [DOI] [PMC free article] [PubMed]
- 227.Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, Si H-R, Zhu Y, Li B, Huang C-L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Tian X, Li C, Huang A, Xia S, Lu S, Shi Z, Lu L, Jiang S, Yang Z, Wu Y. Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. Emerg Microbes Infect. 2020;9(1):382–385. doi: 10.1080/22221751.2020.1729069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Walls AC, Xiong X, Park Y-J, Tortorici MA, Snijder J, Quispe J, Cameroni E, Gopal R, Dai M, Lanzavecchia A. Unexpected receptor functional mimicry elucidates activation of coronavirus fusion. Cell. 2019;176(5):1026–1039.e1015. doi: 10.1016/j.cell.2018.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367(6485):1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Glowacka I, Bertram S, Müller MA, Allen P, Soilleux E, Pfefferle S, Steffen I, Tsegaye TS, He Y, Gnirss K. Evidence that TMPRSS2 activates the severe acute respiratory syndrome coronavirus spike protein for membrane fusion and reduces viral control by the humoral immune response. J Virol. 2011;85(9):4122–4134. doi: 10.1128/JVI.02232-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Shulla A, Heald-Sargent T, Subramanya G, Zhao J, Perlman S, Gallagher T. A transmembrane serine protease is linked to the severe acute respiratory syndrome coronavirus receptor and activates virus entry. J Virol. 2011;85(2):873–882. doi: 10.1128/JVI.02062-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Kleine-Weber H, Elzayat M, Hoffmann M, Pöhlmann S. Functional analysis of potential cleavage sites in the MERS-coronavirus spike protein. Sci Rep. 2018;8:16597. doi: 10.1038/s41598-018-34859-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Park J-E, Li K, Barlan A, Fehr AR, Perlman S, McCray PB, Gallagher T. Proteolytic processing of Middle East respiratory syndrome coronavirus spikes expands virus tropism. Proc Natl Acad Sci. 2016;113(43):12262–12267. doi: 10.1073/pnas.1608147113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Kawase M, Shirato K, van der Hoek L, Taguchi F, Matsuyama S. Simultaneous treatment of human bronchial epithelial cells with serine and cysteine protease inhibitors prevents severe acute respiratory syndrome coronavirus entry. J Virol. 2012;86(12):6537–6545. doi: 10.1128/JVI.00094-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Zhou Y, Vedantham P, Lu K, Agudelo J, Carrion R, Jr, Nunneley JW, Barnard D, Pöhlmann S, McKerrow JH, Renslo AR. Protease inhibitors targeting coronavirus and filovirus entry. Antiviral Res. 2015;116:76–84. doi: 10.1016/j.antiviral.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Le TT, Cramer JP, Chen R, Mayhew S. Evolution of the COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19(10):667–668. doi: 10.1038/d41573-020-00151-8. [DOI] [PubMed] [Google Scholar]
- 238.Deng Y, Lan J, Bao L, Huang B, Ye F, Chen Y, Yao Y, Wang W, Qin C, Tan W. Enhanced protection in mice induced by immunization with inactivated whole viruses compare to spike protein of Middle East respiratory syndrome coronavirus. Emerg Microbes Infect. 2018;7(1):1–10. doi: 10.1038/s41426-018-0056-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Tse LV, Meganck RM, Graham RL, Baric RS. The current and future state of vaccines, antivirals and gene therapies against emerging coronaviruses. Front Microbiol. 2020;11:658. doi: 10.3389/fmicb.2020.00658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Lan J, Yao Y, Deng Y, Chen H, Lu G, Wang W, Bao L, Deng W, Wei Q, Gao GF. Recombinant receptor binding domain protein induces partial protective immunity in rhesus macaques against Middle East respiratory syndrome coronavirus challenge. EBioMedicine. 2015;2(10):1438–1446. doi: 10.1016/j.ebiom.2015.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Wang Y, Tai W, Yang J, Zhao G, Sun S, Tseng C-TK, Jiang S, Zhou Y, Du L, Gao J. Receptor-binding domain of MERS-CoV with optimal immunogen dosage and immunization interval protects human transgenic mice from MERS-CoV infection. Hum Vaccin Immunother. 2017;13(7):1615–1624. doi: 10.1080/21645515.2017.1296994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Zhang N, Channappanavar R, Ma C, Wang L, Tang J, Garron T, Tao X, Tasneem S, Lu L, Tseng C-TK. Identification of an ideal adjuvant for receptor-binding domain-based subunit vaccines against Middle East respiratory syndrome coronavirus. Cell Mol Immunol. 2016;13(2):180–190. doi: 10.1038/cmi.2015.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Du L, Zhao G, Chan CC, Sun S, Chen M, Liu Z, Guo H, He Y, Zhou Y, Zheng B-J. Recombinant receptor-binding domain of SARS-CoV spike protein expressed in mammalian, insect and E. coli cells elicits potent neutralizing antibody and protective immunity. Virology. 2009;393(1):144–150. doi: 10.1016/j.virol.2009.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.He Y, Zhou Y, Liu S, Kou Z, Li W, Farzan M, Jiang S. Receptor-binding domain of SARS-CoV spike protein induces highly potent neutralizing antibodies: implication for developing subunit vaccine. Biochem Biophys Res Commun. 2004;324(2):773–781. doi: 10.1016/j.bbrc.2004.09.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Martínez-Sánchez G, Schwartz A, Di Donna V. Potential cytoprotective activity of ozone therapy in SARS-CoV-2/COVID-19. Antioxidants. 2020;9(5):389. doi: 10.3390/antiox9050389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Venkataraman T, Frieman MB. The role of epidermal growth factor receptor (EGFR) signaling in SARS coronavirus-induced pulmonary fibrosis. Antiviral Res. 2017;143:142–150. doi: 10.1016/j.antiviral.2017.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Khan G. A novel coronavirus capable of lethal human infections: an emerging picture. Virol J. 2013;10(1):1–6. doi: 10.1186/1743-422X-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Bocci V. Ozone a new medical drug. Springer; 2005. [Google Scholar]
- 249.Simonetti V, Quagliariello V, Franzini M, Iaffaioli RV, Maurea N, Valdenassi L (2019) Ozone exerts cytoprotective and anti-inflammatory effects in cardiomyocytes and skin fibroblasts after incubation with doxorubicin. Evidence-Based Complementary and Alternative Medicine:eCAM 2019:2169103. 10.1155/2019/2169103 [DOI] [PMC free article] [PubMed]
- 250.Delgado-Roche L, Hernández-Matos Y, Medina EA, Morejón DÁ, González MR, Martínez-Sánchez G. Ozone-oxidative preconditioning prevents doxorubicin-induced cardiotoxicity in Sprague-Dawley Rats. Sultan Qaboos Univ Med J. 2014;14(3):e342. [PMC free article] [PubMed] [Google Scholar]
- 251.Adali Y, Eroǧlu HA, Makav M, Guvendi GF (2019) Efficacy of ozone and selenium therapy for alcoholic liver injury: an experimental model. in vivo 33(3):763–769 [DOI] [PMC free article] [PubMed]
- 252.Tezcan AH, Ozturk O, Ustebay S, Adali Y, Yagmurdur H. The beneficial effects of ozone therapy in acetaminophen-induced hepatotoxicity in mice. Pharmacol Rep. 2018;70(2):340–345. doi: 10.1016/j.pharep.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 253.Wang L, Chen H, Liu X-H, Chen Z-Y, Weng X-D, Qiu T, Liu L, Zhu H-C. Ozone oxidative preconditioning inhibits renal fibrosis induced by ischemia and reperfusion injury in rats. Exp Ther Med. 2014;8(6):1764–1768. doi: 10.3892/etm.2014.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Re L, Malcangi G, Martinez-Sanchez G. Medical ozone is now ready for a scientific challenge: current status and future perspectives. J Exp Integr Med. 2012;2(3):193–196. doi: 10.5455/jeim.070612.ir.012. [DOI] [Google Scholar]
- 255.Di Mauro R, Cantarella G, Bernardini R, Di Rosa M, Barbagallo I, Distefano A, Longhitano L, Vicario N, Nicolosi D, Lazzarino G. The biochemical and pharmacological properties of ozone: the smell of protection in acute and chronic diseases. Int J Mol Sci. 2019;20(3):634. doi: 10.3390/ijms20030634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Bocci V, Zanardi I, Travagli V. Ozonation of human HIV-infected plasmas for producing a global vaccine: how HIV-patients may help fight the HIV pandemia. Virulence. 2010;1(3):215–217. doi: 10.4161/viru.1.3.11830. [DOI] [PubMed] [Google Scholar]
- 257.Bocci V, Travagli V, Zanardi I. The failure of HIV vaccines: a new autovaccine may overcome some problems. Med Hypotheses. 2009;72(6):662–664. doi: 10.1016/j.mehy.2008.12.034. [DOI] [PubMed] [Google Scholar]
- 258.Ura T, Okuda K, Shimada M. Developments in viral vector-based vaccines. Vaccines. 2014;2(3):624–641. doi: 10.3390/vaccines2030624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Rauch S, Jasny E, Schmidt KE, Petsch B. New vaccine technologies to combat outbreak situations. Front Immunol. 2018;9:1963. doi: 10.3389/fimmu.2018.01963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Faber M, Lamirande EW, Roberts A, Rice AB, Koprowski H, Dietzschold B, Schnell MJ. A single immunization with a rhabdovirus-based vector expressing severe acute respiratory syndrome coronavirus (SARS-CoV) S protein results in the production of high levels of SARS-CoV-neutralizing antibodies. J Gen Virol. 2005;86(Pt 5):1435. doi: 10.1099/vir.0.80844-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Sutter G, Staib C. Vaccinia vectors as candidate vaccines: the development of modified vaccinia virus Ankara for antigen delivery. Curr Drug Targets Infect Disord. 2003;3(3):263–271. doi: 10.2174/1568005033481123. [DOI] [PubMed] [Google Scholar]
- 262.Chen Z, Zhang L, Qin C, Ba L, Christopher EY, Zhang F, Wei Q, He T, Yu W, Yu J. Recombinant modified vaccinia virus Ankara expressing the spike glycoprotein of severe acute respiratory syndrome coronavirus induces protective neutralizing antibodies primarily targeting the receptor binding region. J Virol. 2005;79(5):2678–2688. doi: 10.1128/JVI.79.5.2678-2688.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Du L, He Y, Wang Y, Zhang H, Ma S, Wong CK, Wu SH, Ng F, Huang J-D, Yuen K-Y. Recombinant adeno-associated virus expressing the receptor-binding domain of severe acute respiratory syndrome coronavirus S protein elicits neutralizing antibodies: Implication for developing SARS vaccines. Virology. 2006;353(1):6–16. doi: 10.1016/j.virol.2006.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kobinger GP, Figueredo JM, Rowe T, Zhi Y, Gao G, Sanmiguel JC, Bell P, Wivel NA, Zitzow LA, Flieder DB. Adenovirus-based vaccine prevents pneumonia in ferrets challenged with the SARS coronavirus and stimulates robust immune responses in macaques. Vaccine. 2007;25(28):5220–5231. doi: 10.1016/j.vaccine.2007.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Liu R-Y, Wu L-Z, Huang B-J, Huang J-L, Zhang Y-L, Ke M-L, Wang J-M, Tan W-P, Zhang R-H, Chen H-K. Adenoviral expression of a truncated S1 subunit of SARS-CoV spike protein results in specific humoral immune responses against SARS-CoV in rats. Virus Res. 2005;112(1–2):24–31. doi: 10.1016/j.virusres.2005.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Shim B-S, Stadler K, Nguyen HH, Yun C-H, Kim DW, Chang J, Czerkinsky C, Song MK. Sublingual immunization with recombinant adenovirus encoding SARS-CoV spike protein induces systemic and mucosal immunity without redirection of the virus to the brain. Virol J. 2012;9(1):1–9. doi: 10.1186/1743-422X-9-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Liu MA. A comparison of plasmid DNA and mRNA as vaccine technologies. Vaccines. 2019;7(2):37. doi: 10.3390/vaccines7020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Ledwith B, Manam S, Troilo P, Barnum A, Pauley C, Griffiths T, 2nd, Harper L, Schock H, Zhang H, Faris J. Plasmid DNA vaccines: assay for integration into host genomic DNA. Dev Biol (Basel) 2000;104:33–43. [PubMed] [Google Scholar]
- 269.Chi H, Zheng X, Wang X, Wang C, Wang H, Gai W, Perlman S, Yang S, Zhao J, Xia X. DNA vaccine encoding Middle East respiratory syndrome coronavirus S1 protein induces protective immune responses in mice. Vaccine. 2017;35(16):2069–2075. doi: 10.1016/j.vaccine.2017.02.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Al-Amri SS, Abbas AT, Siddiq LA, Alghamdi A, Sanki MA, Al-Muhanna MK, Alhabbab RY, Azhar EI, Li X, Hashem AM. Immunogenicity of candidate MERS-CoV DNA vaccines based on the spike protein. Sci Rep. 2017;7:44875. doi: 10.1038/srep44875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Huang J, Cao Y, Du J, Bu X, Ma R, Wu C. Priming with SARS CoV S DNA and boosting with SARS CoV S epitopes specific for CD4+ and CD8+ T cells promote cellular immune responses. Vaccine. 2007;25(39–40):6981–6991. doi: 10.1016/j.vaccine.2007.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Martin JE, Louder MK, Holman LA, Gordon IJ, Enama ME, Larkin BD, Andrews CA, Vogel L, Koup RA, Roederer M. A SARS DNA vaccine induces neutralizing antibody and cellular immune responses in healthy adults in a phase I clinical trial. Vaccine. 2008;26(50):6338–6343. doi: 10.1016/j.vaccine.2008.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Philbin VJ, Dowling DJ, Gallington LC, Cortés G, Tan Z, Suter EE, Chi KW, Shuckett A, Stoler-Barak L, Tomai M. Imidazoquinoline toll-like receptor 8 agonists activate human newborn monocytes and dendritic cells through adenosine-refractory and caspase-1–dependent pathways. J Allergy Clin Immunol. 2012;130(1):195–204.e199. doi: 10.1016/j.jaci.2012.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Shukla NM, Salunke DB, Balakrishna R, Mutz CA, Malladi SS, David SA. Potent adjuvanticity of a pure TLR7-agonistic imidazoquinoline dendrimer. PLoS ONE. 2012;7(8):e43612. doi: 10.1371/journal.pone.0043612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Ella R, Vadrevu KM, Jogdand H, Prasad S, Reddy S, Sarangi V, Ganneru B, Sapkal G, Yadav P, Abraham P (2021) Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBV152: a double-blind, randomised, phase 1 trial. The Lancet Infectious Diseases 21(5):637–646. 10.1016/S1473-3099(20)30942-7 [DOI] [PMC free article] [PubMed]
- 276.Goss AL, Samudralwar RD, Das RR, Nath A (2021) ANA investigates: neurological complications of COVID‐19 vaccines. Annals of Neurology 89(5):856–857. 10.1002/ana.26065 [DOI] [PMC free article] [PubMed]
- 277.Kyriakidis NC, López-Cortés A, González EV, Grimaldos AB, Prado EO. SARS-CoV-2 vaccines strategies: a comprehensive review of phase 3 candidates. npj Vaccines. 2021;6(1):1–17. doi: 10.1038/s41541-021-00292-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Allen A, Szabo L (2020) NIH “very concerned” about serious side effect in coronavirus vaccine trial. Scientific American, September 15
- 279.Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, Angus B, Baillie VL, Barnabas SL, Bhorat QE. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Ledford H (2020) US authorization of first COVID vaccine marks new phase in safety monitoring. Nature 588(7838):377–378. 10.1038/d41586-020-03542-4 [DOI] [PubMed]
- 281.Keddie S, Pakpoor J, Mousele C, Pipis M, Machado PM, Foster M, Record CJ, Keh RY, Fehmi J, Paterson RW. Epidemiological and cohort study finds no association between COVID-19 and Guillain-Barré syndrome. Brain. 2021;144(2):682–693. doi: 10.1093/brain/awaa433. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.