Abstract
Background and Aim
The health care and social assistance industry has one of the highest rates of non‐fatal occupational injuries and illnesses, both in California and nationally. In the coming years, the health care industry will face added pressure as both the population and workforce age. The aim of this study is to identify targeted populations that may benefit from interventions to prevent future injuries, keep the workforce healthy, and decrease injury‐related costs.
Methods
This retrospective study analyzed California workers' compensation claims from 2009 to 2018 in the health care and social assistance industry.
Results
Across the four industry sub‐groups, the highest number of claims came from hospitals (n = 243 605; 38.9%), followed by ambulatory care (n = 187 010; 29.9%), nursing/residential care (n = 133 206; 21.3%), and social assistance (n = 62 211; 9.9%). Nursing/residential care settings reported the highest proportion of both lifting injuries (15.8%) and low back injuries (16.9%) as compared to the other settings. Across all settings within California, nurses had the highest proportion of injuries (22.1%), followed by aides/assistants (20.4%), services staff (13.2%), administrative staff (11.0%), and technicians (10.3%). Thirty‐five of California's counties had an increasing rate of population‐adjusted claims during the study period.
Conclusion
This study found that while hospitals have the highest number of injuries, ambulatory care employee injuries are increasing. Employees involved in non‐patient care tasks, such as those working in facility service roles, would likely benefit from additional injury prevention interventions.
Keywords: California, health care and social assistance industry, workers' compensation, workplace injury and illness
1. BACKGROUND
The California workers' compensation system, a program for health care and wage replacement for those hurt on the job, provides coverage to 16.8 million employees working for more than one million employers. 1 In 2018 alone, the program cost was $23.5 billion to support occupationally injured or ill workers statewide. 1 The occupational injury and illness incidence rates for workers in California are statistically higher than the national incidence rate. 2 The health care and social assistance industry has one of the highest rates of non‐fatal occupational injuries and illnesses, both in California and nationally. 2 , 3
Demand for health care services and limited availability of well‐trained staff may explain some of the occupational injuries. The health care industry is one of the fastest growing job sectors in California. 4 Ambulatory care and social assistance jobs are experiencing the most growth as compared to relatively steady job counts in hospital and nursing/residential care settings. 5 In the coming years, the health care industry will face added pressure as both the population and workforce age. 6 Nearly one‐third of California's physicians and nurse practitioners are eligible for retirement in the next decade, and nurse hires are often replacing staff rather than filling new positions. 4 , 7 The health care sector also struggles with a high turnover rate of nearly 20%, which is second only to the hospitality industry. 8 , 9 Examples of health care positions with high annual turnover rates include certified nursing assistants (26.5%), patient care technicians (26.4%), and hospital executives (18.0%). 10 , 11
The aim of this study is to explore California workers' compensation data within the health care and social assistance industry to identify targeted populations that may benefit from interventions to prevent future injuries, keep the workforce healthy, and decrease injury‐related costs. These results can be used to support evidence‐based occupational health programs for high‐risk individuals in the California health care industry and may help inform similar programs in other jurisdictions.
2. METHODS
This retrospective study analyzed California workers' compensation claims from 2009 to 2018 in the health care and social assistance industry. Claims were reported to the State of California Department of Industrial Relations, Division of Workers' Compensation, and recorded by the Workers' Compensation Information System (WCIS). California employers report occupational injuries or illnesses that result in lost work time beyond the date of the incident or that require medical treatment beyond first aid. 12 Cases were included regardless of their status (open, closed, reopened) or the type of claim (medical, indemnity, time away from work), and were classified by year based on the date of initial injury. The nature of injury, cause, and body part affected were abstracted from the Employer's First Report of Injury or Illness form. “Strains or Injury By, NOC” (not otherwise classified) is defined as a strain or injury by something other than: continual noise, twisting, jumping or leaping, holding or carrying, lifting, pushing or pulling, reaching, using tool or machinery, wielding or throwing, or repetitive motion. “Miscellaneous, NOC” is defined as miscellaneous causes by something other than: absorption, ingestion or inhalation, foreign matter (body) in eye(s), natural disasters, person in act of a crime, other than physical cause of injury, mold, gunshot, terrorism, or cumulative NOC. 13 Workers' permanent impairments were abstracted from the Subsequent Report of Injury form.
Workers were included in the study if their employer's industry was either in the North American Industry Classification System (NAICS) Sector of Health Care and Social Assistance (NAICS = 62) or the equivalent Standard Industrial Classification (SIC) Major Groups of Health Services (SIC = 80) or Social Services (SIC = 83). These industry sub‐groups were: hospitals, nursing/residential care facilities (eg, mental health facilities, retirement communities), ambulatory care sites (eg, offices of physicians, outpatient clinics, laboratories), and social assistance settings (eg, family services, housing services, vocational rehabilitation). 14
The WCIS uses a free text field to capture claimants' job titles. There were 53 678 unique job titles that could not be classified into standard job titles like the Standard Occupational Classification system. To classify job titles, distinct keywords (n = 521) such as physician or janitor, were grouped according to job‐specific daily tasks, education requirements, job class, and physical requirements. Categories were adjusted using a modified‐Delphi method. Job titles without distinct keywords were manually classified into these categories. In total, jobs were classified into seven categories: nursing (eg, registered nurse, care manager, medic, licensed vocational nurse, physical therapist), assistant/aide (eg, certified nursing assistant, resident attendant, transporter, direct care attendant), clinician (eg, physician, physician assistant, nurse practitioner), services (eg, janitor, cook, environmental services, maintenance), social services (eg, counselor, case manager, teacher, dietary professional), administrative (eg, clerk, director, office manager), or technician (eg, health technician, laboratory assistant, sonographer, surgical technician). Job descriptions that were missing (n = 2365; 0.4%), those that were described as unknown (n = 10 863; 1.7%), or jobs that could not be classified due to insufficient detail (eg, volunteer, representative) or that were NOC (n = 60 552; 9.7%) were placed in the category “other.”
The employer's postal code was mapped to each county to analyze the geographical distribution of employers where injuries and illnesses occurred. California county end‐of‐year population data and industry employment counts (mid‐year average) from the State of California's Employment Development Department were used to transform case counts into incidence rates that accounted for changes in population and workforce. 5 , 15 The change in incidence rates by county over the 10‐year study period was estimated using a linear regression model with the year of injury as the independent variable and the incidence rate as the dependent variable. Data were de‐identified by WCIS and contained no personally identifiable information, and therefore, did not require Institutional Review Board (IRB) approval. All analyses were done using the R statistical software (R Core Team, 2020).
3. RESULTS
From 2009 to 2018, there were 626 032 injury or illness cases reported by health care and social assistance employees. The majority of injuries were sustained by women (78.1%), with three‐quarters of cases affecting individuals aged 32 to 53 years; the median annual salary was $40 450. Across the four industry sub‐groups, the highest number of claims came from hospitals (n = 243 605; 38.9%), followed by ambulatory care (n = 187 010; 29.9%), nursing/residential care (n = 133 206; 21.3%), and social assistance (n = 62 211; 9.9%). The total number of injuries increased over time from 54 743 in 2009 to 72 014 in 2018. When adjusted for job growth, there was a slight increase in injury rate from 300 injuries per 10 000 employees in 2009 to 307 injuries per 10 000 employees in 2018. The 10‐year injury rate averages varied across facility types, with hospitals reporting 642 injuries per 10 000 employees, ambulatory care reporting 255 injuries per 10 000 employees, nursing/residential care reporting 485 injuries per 10 000 employees, and social assistance settings reporting 95 injuries per 10 000 employees. Figure 1 compares workforce‐adjusted injury rates in each of the four industry sub‐categories. Hospitals had the greatest rate of injury compared to the other sub‐categories, although rates have been decreasing since 2013 while ambulatory care injury and illness rates have been increasing since 2014.
FIGURE 1.
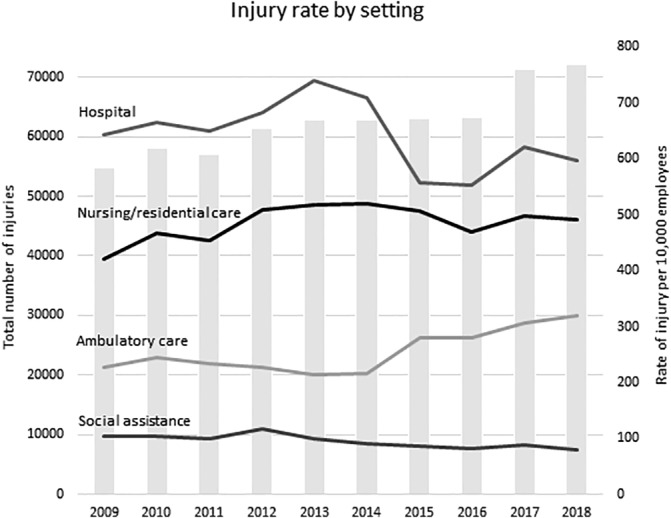
Total injury counts (gray bars, left axis) and rates of injury per 10 000 employees (trendlines, right axis) per year, across the four health care industry sub‐category settings
The top categories of nature of injury, cause of injury, and body part injured were compared across the four occupational settings studied. Table 1 compares the claim counts and proportional percentages across the four industry sub‐groups to evaluate where there may be higher than expected risk. Strains and tears (defined by the State of California as an injury of the muscle or the musculotendinous unit 13 ), were the most common injury, representing 34.4% of all claims, followed by contusions (11.0%), sprains (injury to ligaments) (10.0%), other specific injuries (9.6%), and puncture wounds (7.7%). These injury types were similar across the industry sub‐groups apart from ambulatory care, which had a higher proportion of puncture wounds than other settings (14.1% vs 3.4%‐5.9%, respectively). Across all settings, lifting injuries (10.8%) and strains NOC (9.1%) were the most common causes of injury, followed by miscellaneous NOC causes (6.6%), repetitive motion (6.0%), and injury due to being struck accidentally or on purpose by a fellow worker, patient, or other person (5.9%). The low back was the most frequently injured body part, representing 13.6% of all claims; followed by multiple body parts (12.8%), finger(s) (9.1%), shoulder(s) (6.8%), and knee(s) (6.1%). Nursing/residential care settings reported the highest proportion of both lifting injuries (15.8% vs 8.9%‐9.9%) and low back injuries (16.9% vs 10.0%‐13.1%) as compared to the other settings. Approximately 7.2% of employees became permanently disabled, defined as having 1% to 100% permanent impairment, with similar rates described across the different industry sub‐groups.
TABLE 1.
Top five categories for nature of injury, cause, anatomic location, and permanent (partial or otherwise) disability, across the four industry sub‐categories
| n = 626 032 | n = 243 605 (38.9%) | n = 187 010 (29.9%) | n = 133 206 (21.3%) | n = 62 211 (9.9%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Hospital | Ambulatory care | Nursing/ residential care | Social assistance | |||||||
| n | % | n | % | n | % | n | % | n | % | ||
| Top nature of injury | Strain or tear | 215 588 | 34.4 | 88 296 | 36.3 | 59 051 | 31.6 | 49 006 | 36.8 | 19 235 | 30.9 |
| Contusion | 68 604 | 11.0 | 27 149 | 11.1 | 16 104 | 8.6 | 16 704 | 12.5 | 8647 | 13.9 | |
| Sprain or tear | 62 824 | 10.0 | 27 356 | 11.2 | 13 955 | 7.5 | 14 348 | 10.8 | 7165 | 11.5 | |
| Other specific injuries | 59 974 | 9.6 | 25 265 | 10.4 | 16 700 | 8.9 | 11 640 | 8.7 | 6369 | 10.2 | |
| Puncture | 48 175 | 7.7 | 11 618 a | 4.8 | 26 457 | 14.2 | 7967 | 6.0 | 2133 a | 3.4 | |
| Top causes of injury | Lifting | 67 450 | 10.8 | 24 136 | 9.9 | 16 558 | 8.9 | 21 041 | 15.8 | 5715 | 9.2 |
| Strain or injury by, NOC | 57 056 | 9.1 | 23 448 | 9.6 | 17 923 | 9.6 | 10 313 | 7.7 | 5372 | 8.6 | |
| Miscellaneous, NOC | 41 479 | 6.6 | 16 110 | 6.6 | 12 828 | 6.9 | 8274 | 6.2 | 4267 | 6.9 | |
| Repetitive motion | 37 294 | 6.0 | 16 026 | 6.6 | 14 956 | 8.0 | 3942 a | 3.0 | 2370 a | 3.8 | |
| Fellow worker, patient, or other person | 36 714 | 5.9 | 15 076 | 6.2 | 5656 a | 3.0 | 12 112 | 9.1 | 3870 a | 6.2 | |
| Top injured body part | Low back area | 78 812 | 13.6 | 29 314 | 12.0 | 18 770 | 10.0 | 22 567 | 16.9 | 8161 | 13.1 |
| Multiple | 73 882 | 12.8 | 29 067 | 11.9 | 21 783 | 11.7 | 15 232 | 11.4 | 7800 | 12.5 | |
| Finger(s) | 52 906 | 9.1 | 17 039 | 7.0 | 22 146 | 11.8 | 10 221 | 7.7 | 3500 | 5.6 | |
| Shoulder(s) | 39 422 | 6.8 | 18 026 | 7.4 | 9111 a | 4.9 | 9286 | 7.0 | 2999 a | 4.8 | |
| Knee(s) | 35 480 | 6.1 | 14 315 | 5.9 | 8775 a | 4.7 | 7685 | 5.8 | 4705 | 7.6 | |
| Permanently impaired | 44 838 | 7.2 | 15 707 | 6.5 | 14 142 | 7.6 | 11 096 | 8.3 | 4893 | 7.9 | |
Categories that were outside of the top five reasons per industry setting. NOC (not otherwise classified).
Health care and social assistance settings each have a different proportion of job types, given the variety of health services offered. The proportion of job types injured are shown in Figure 2 for each of the four industry sub‐groups. Across all settings within California, nurses had the highest proportion of injuries (22.1%), followed by aides/assistants (20.4%), services staff (13.2%), administrative staff (11.0%), and technicians (10.3%). The highest proportion of injury occurred in nursing jobs in hospitals (32.2% vs 3.2%‐20.6%), aides/assistants in nursing/residential care sites (40.2% vs 12.1%‐16.7%), and social services in social assistance settings (40.6% vs 3.2%‐8.0%).
FIGURE 2.
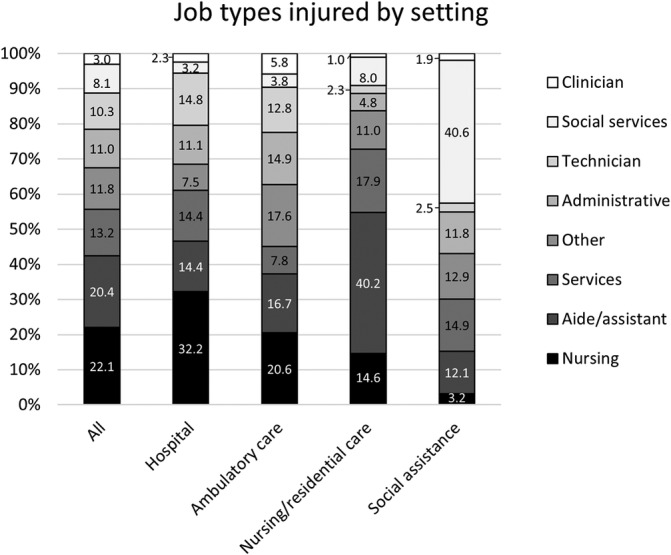
Proportions of job types injured in each of the health care industry settings
Changes in incidence rates over the 10‐year study period were compared across California's 58 counties with 34 of the counties showing an increasing rate of population‐adjusted claims. Darker shading in Figure 3 indicates higher counts of workers' compensation claims among health care employees (leftmost map), where rates of injury were high after being adjusted by county population (middle map), and where adjusted rates increased over time from 2009 to 2018 (rightmost map). The counties with the highest average annual case counts were heavily populated: Los Angeles (n = 15 121), San Diego (n = 6179), and Alameda (n = 5551). Alameda, Lassen, and Mono counties had the highest population‐adjusted average annual incidence rate over the 10 years of study, with 38, 31, and 29 claims per 10 000 population, respectively.
FIGURE 3.
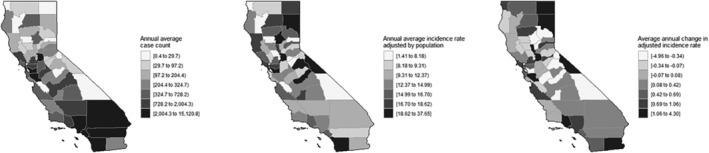
California county data by annual average case count (left), annual average incidence rate adjusted by county population (middle), and the change in adjusted annual incidence rates over the 10‐year study period (right)
During the study period, Lassen, Mono, and Sacramento counties had the greatest rate of increase in population‐adjusted case counts, with 4.3, 2.3, and 2.2 more claims per 10 000 population per year, respectively. Alameda, Alpine, and Butte counties saw the greatest decline in population‐adjusted claim counts, with −5.0, −1.7, and − 1.1 fewer claims per 10 000 population each year, respectively.
4. DISCUSSION
This analysis explored California's workers' compensation injury and illness trends across the four health care and social assistance industry sub‐categories to identify at‐risk populations in which preventative injury and illness programs may be valuable. Analyzing injury data and using it to inform preventative measures is an important research‐to‐practice tool to link departments such as employee health, workers' compensation, and workplace health and safety to ensure that appropriate workers are being targeted. Preventing injuries in these settings can also help patients, as care facilities with lower rates of workers compensation claims, higher employee retention rates, and higher rates of worker job satisfaction demonstrate better patient care outcomes. 16
When comparing the four settings, injury rates were highest in hospitals but increased in ambulatory care during the study period. The number of ambulatory care workers is expected to continue to rise as medical technology improvements, such as minimally invasive surgical techniques, become more available to support consumers' desire for alternative sources of convenient and cost‐effective outpatient care, such as walk‐in care clinics. 17 , 18 Ambulatory care sites present an opportunity to implement best‐practice health and safety programs by leveraging freely‐available learning materials from established hospital safety programs such as the U.S. Department of Veteran Affairs or programs recommended by the Occupational Safety and Health Administration. 19 , 20 Ideally, these materials support programs that build a culture of safety and shared responsibility to further reduce occupational injury risk. 21
Similar to national hospital‐based findings, musculoskeletal injuries such as sprains, strains, and tears, remain the greatest concern for California's health care system. 22 In addition, this analysis found that the high number of lifting and low back injuries in nursing/residential care facilities warrants continued preventative action and worker education. A study of Ohio's workers' compensation data reported that nursing care facilities were at the highest risk for musculoskeletal claims that could have been preventable with ergonomic or slip/trip/fall interventions. 23 Although direct patient care is likely a significant driver in these claims, workplace ergonomic programs for all employees can help raise awareness to minimize the need for force, repetitive motion, and awkward postures during the workday. 24 Ergonomic programs are good for both employees and employers as research has found them effective for increasing productivity and decreasing injuries, lost workdays, cost, and turnover. 25
Job type is also an important risk factor when considering how to decrease injuries in the workplace. Occupational health and safety professionals should continue to focus on injury prevention and outreach efforts with nursing staff in hospitals, aides/assistants in nursing/residential care sites, and social workers in social assistance settings, but support staff should not be overlooked. In this study, service jobs (including janitorial staff, kitchen workers, and grounds keepers), were the third most common job type with injuries across all settings. Workers in this job category often have heavy workloads and could benefit from additional ergonomic and educational training. This finding echoes a Canadian study that recommended health care facility support workers would benefit from non‐patient care focused injury prevention programs. 26
While large counties such as Los Angeles, San Diego, and Alameda reported high numbers of health care injuries and should continue ongoing prevention efforts, when adjusted for population size, several smaller counties also warrant attention on worker safety. When examining trends over time, Lassen, Mono, and Sacramento counties had the greatest increases in injury rates. Interestingly, Alameda county, despite having a large population and large volume of claims, showed the most success in protecting health care employees with the greatest decrease in claims per 10 000 employees per year. This finding is worthy of further exploration, as a quarter of Alameda county's largest employers are health‐related facilities. 27
A strength of this study was the utilization of a large database of claims combined with a novel categorization of job titles that covered a wide variety of work settings. In addition, whereas current health care research primarily focuses on direct patient care workers such as nurses and nursing assistants, this study included all employees serving the industry. However, our method of classifying job titles focused on broad categories when highly specific job duties exist that could have unique trends, notably in the “other” category. A limitation of this study is that the geographic analysis may not capture employees considered “traveling” or hired through a third‐party contracting company where the employer zip code may be different than the injury site. In addition, workplace injuries and workers' compensation claims are likely an underreported measure of work‐related disorders. 28 , 29 However, California's workers' compensation program offers a relatively low threshold to obtain benefits, so it allows more people to qualify for benefits including employees with less severe injuries as compared to other state programs. 30
5. CONCLUSION
Occupational health within the health care and social assistance industry encompasses a wide variety of job types and work sites. This study found that while hospitals have the highest number of injuries, ambulatory care employee injuries are increasing. While working in direct patient care likely presents significant risk for occupational injuries in California, employees involved in non‐patient care tasks, such as those working in facility service roles, would likely benefit from additional injury prevention interventions. This analysis of California health care and social assistance industry trends over a 10‐year period may help occupational health and safety professionals elsewhere identify high‐risk workers.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Conceptualization: Kerri Wizner.
Data Curation: Fraser Gaspar.
Formal Analysis: Kerri Wizner, Fraser Gaspar.
Methodology: Kerri Wizner, Fraser Gaspar, Adrianne Biggio.
Validation: Adrianne Biggio, Steve Wiesner.
Writing – Original Draft: Kerri Wizner.
Writing – Review and Editing: Fraser Gaspar, Adrianne Biggio, Steve Wiesner.
All authors have read and approved the final version of the manuscript.
Kerri Wizner had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
TRANSPARENCY STATEMENT
Kerri Wizner affirms that this manuscript is an honest, accurate, and transparent account of the study being reported that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
INSTITUTION AND ETHICS APPROVAL AND INFORMED CONSENT
This data did not contain personally identifiable information and was, therefore, not subject to IRB review. This research efforts were supported, but not directed from any of the author institutions.
Supporting information
Data S1. Supporting Information.
ACKNOWLEDGMENTS
A special thanks to Debbie Ehsan for her contribution to make the results of this research actionable and Anne Ahlman, MPT, for her thought leadership and detailed review.
Wizner K, Gaspar FW, Biggio A, Wiesner S. Occupational injuries in California's health care and social assistance industry, 2009 to 2018. Health Sci Rep. 2021;4:e306. 10.1002/hsr2.306
DATA AVAILABILITY STATEMENT
The data from this study were provided to authors under a data use agreement through the California Division of Workers' Compensation, which prohibits the authors from making the data set publicly available. More information is available here: https://www.dir.ca.gov/dwc/wcis/WCIS_Reports.html.
REFERENCES
- 1. McNally S, Bloch D, Bouma C, et al. California commission on health and Safety and Workers' compensation 2019 annual Report. 2020. https://www.dir.ca.gov/chswc/Reports/2019/CHSWC_AnnualReport2019.pdf
- 2. U.S. Bureau of Labor Statistics . 2017 Survey of Occupational Injuries and Illnesses. 2018. https://www.bls.gov/iif/osch0062.pdf
- 3. State of California Department of Industrial Relations . Nonfatal occupational injuries and illnesses in California. Office of Policy, Research and Legislation. https://www.dir.ca.gov/oprl/nonfatal.htm. Published 2020. Accessed January 12, 2019
- 4. State of California Employment Development Department . Health Care in California. 2013. https://www.labormarketinfo.edd.ca.gov/SpecialReports/Health_Care_in_CA.pdf
- 5. State of California Employment Development Department . Employment by Industry Data. Labor Market Information Resources and Data. Published 2020. https://www.labormarketinfo.edd.ca.gov/data/employment-by-industry.html
- 6. Dall T, Reynolds R, Jones K, Chakrabarti R, Iacobucci W. The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. 2019. https://aamc‐black.global.ssl.fastly.net/production/media/filer_public/31/13/3113ee5c‐a038‐4c16‐89af‐294a69826650/2019_update_‐_the_complexities_of_physician_supply_and_demand_‐_projections_from_2017‐2032.pdf
- 7. Coffman J, Geyn I, Himmerick K. California's Primary Care Workforce: Current Supply, Characteristics, and Pipeline of Trainees. 2017. https://healthforce.ucsf.edu/sites/healthforce.ucsf.edu/files/publication-pdf/Research-Report_CA-Primary-Care-Workforce.pdf
- 8. Willard‐Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K. Burnout and health care workforce turnover. Ann Fam Med. 2019;17(1):36‐41. 10.1370/afm.2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. CompData . 2018 Turnover Report. 2018. https://www2.salary.com/turnover
- 10. Nursing Solutions Incorporated . 2020 National Health Care Retention & RN Staffing Report. 2020. https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf
- 11. American College of Healthcare Executives . 2019 Annual Survey of Hospital CEOs. 2019. https://www.ache.org/about-ache/news-and-awards/news-releases/hospital-ceo-turnover
- 12. State of California Department of Industrial Relations . Office of Policy, Research, and Legislation Title 8 Regulations. 2019. https://www.dir.ca.gov/t8/14001.html#:~:text=§14001. Code Section 5401(a).
- 13. State of California Department of Industrial Relations . Injury Description Codes ‐ Nature of Injury. 2020. https://www.dir.ca.gov/dwc/WCIS/Nature_Of_Injury.pdf
- 14. United States Census Bureau. North American Industry Classification System . 2017. NAICS definition. Published 2017. https://www.census.gov/naics/
- 15. State of California Employment Development Department . Population and Census Data. Labor Market Information Resources and Data. Published 2020. https://www.labormarketinfo.edd.ca.gov/Population_and_Census.html
- 16. Boakye‐Dankwa E, Teeple E, Gore R, Punnett L. Associations among health care workplace Safety, resident satisfaction, and quality of Care in Long‐Term Care Facilities. J Occup Environ Med. 2017;59(11):1127‐1134. 10.1097/JOM.0000000000001163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Blue Cross Blue Shield . How Consumers Are Saving With the Shift To Outpatient Care. 2016. https://www.bcbs.com/sites/default/files/file-attachments/health-of-america-report/BCBS-HealthOfAmericaReport-Outpatient.pdf
- 18. Torpey E. Healthcare: millions of jobs now and in the Future. 2014. https://www.bls.gov/careeroutlook/2014/spring/art03.pdf
- 19. U.S. Department of Veterans Affairs . Safe Patient Handling and Mobility. https://www.publichealth.va.gov/employeehealth/patient-handling/index.asp. Published 2016. Accessed June 25, 2020
- 20. Occupational Safety and Health Administration . Worker Safety in hospitals. https://www.osha.gov/hospitals. Published 2020. Accessed August 1, 2020
- 21. Aljabri D, Vaughn A, Austin M, et al. An investigation of healthcare worker perception of their workplace Safety and incidence of injury. Workplace Health Saf. 2020;68(5):214‐225. 10.1177/2165079919883293. [DOI] [PubMed] [Google Scholar]
- 22. Occupational Safety and Health Administration . Worker Safety in your Hospital: Know the Facts. 2013. https://www.osha.gov/sites/default/files/1.2_Factbook_508.pdf
- 23. Meyers A, Al‐Tarawneh I, Wurzelbacher S, et al. Applying machine learning to Workers' compensation data to identify industry‐specific ergonomic and Safety prevention priorities: Ohio, 2001 to 2011. J Occup Environ Med. 2018;60(1):55‐73. 10.1097/JOM.0000000000001162.Applying. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hedge A, James T, Pavlovic‐Veselinovic S. Ergonomics concerns and the impact of healthcare information technology. Int J Ind Ergon. 2011;41(4):345‐351. 10.1016/j.ergon.2011.02.002. [DOI] [Google Scholar]
- 25. Goggins RW, Spielholz P, Nothstein GL. Estimating the effectiveness of ergonomics interventions through case studies: implications for predictive cost‐benefit analysis. J Saf Res. 2008;39(3):339‐344. 10.1016/j.jsr.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 26. Ngan K, Drebit S, Siow S, Yu S, Keen D, Alamgir H. Risks and causes of musculoskeletal injuries among health care workers. Occup Med. 2010;60(5):389‐394. 10.1093/occmed/kqq052. [DOI] [PubMed] [Google Scholar]
- 27. State of California Employment Development Department . Major Employers in Alameda County. https://www.labormarketinfo.edd.ca.gov/majorer/countymajorer.asp?CountyCode=000001. Published 2020. Accessed August 1, 2020
- 28. Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health. 2002;92(9):1421‐1429. 10.2105/AJPH.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Galizzi M, Miesmaa P, Punnett L, Slatin C. Injured workers' underreporting in the health care industry: an analysis using quantitative, qualitative, and observational data. Ind Relat. 2010;49(1):22‐43. 10.1111/j.1468-232X.2009.00585.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Leigh JP, Cone JE, Harrison R. Costs of occupational injuries and illnesses in California. Prev Med. 2001;406(32):393‐406. 10.1006/pmed.2001.0841. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting Information.
Data Availability Statement
The data from this study were provided to authors under a data use agreement through the California Division of Workers' Compensation, which prohibits the authors from making the data set publicly available. More information is available here: https://www.dir.ca.gov/dwc/wcis/WCIS_Reports.html.


