Abstract
Background:
Effective interventions for overdose survivors are needed in the emergency departments (EDs). One promising model is the use of peer recovery coaches to engage with survivors in EDs, followed by partnering with community case management navigators to connect survivors to recovery support and treatment services. This paper describes the evaluation of a pilot program, the Recovery Opioid Overdose Team (ROOT), a warm hand-off system that links survivors to treatment services post-ED discharge.
Methods:
The ROOT program is composed of a peer recovery coach who is in long-term recovery, and a case management navigator who specializes in mental health care and provides guidance for accessing community services. After an overdose reversal, law enforcement contacts a county 24/7 Crisis Team, who then notifies ROOT. The peer recovery coach engages with the survivor in the ED, and then follow up continues with the case management navigator and the peer recovery coach for up to 90 days post-ED discharge. Retrospective chart reviews were conducted to evaluate ROOT in two Midwest EDs from September 2017 through March 2019.
Results:
Of the 122 referrals, 77.0% (n=94) of the survivors initially engaged with ROOT in the ED or in the community. The remaining 23.0% (n=28) left the ED against medical advice or were unengaged. The majority of overdose survivors were male (63.9%; n=78), White (43.4%; n=53), had housing (80.2%; n=48), and access to transportation (48.4%; n=59). From the 122 referrals, 33.6% (n=41) received ongoing treatment services (n=20 outpatient, n=17 residential, n=2 detoxification facility, n=1 recovery housing, n=1 medication treatment for opioid use disorder), 2.5% (n=3) were incarcerated, 2.5% (n=3) were deceased, and 61.5 % (n=75) declined services.
Conclusions:
The ROOT, a community-wide coordinated program in the EDs, shows promise in linking overdose survivors to recovery support and treatment services post-overdose.
Keywords: Peer recovery, opioid overdose, law enforcement, emergency department, naloxone, case management, mental illness
Introduction
In 2018, drug overdoses contributed to over 67,000 American deaths.1 However, not all overdoses result in death, and for those who experience a nonfatal overdose, the emergency department (ED) is one of the key access points to engage and connect overdose survivors to community services.2 From July 2016 to September 2017, ED visits for overdoses increased by 30% nationally, with a 79% increase in the Midwest.3 Frequent ED visits were associated with higher likelihood of subsequent hospitalizations and near-fatal events.4 Thus, effective, timely, and community-wide coordinated secondary prevention interventions—occurring after an overdose has been reversed by naloxone—are urgently needed in the ED.
One rapidly adopted approach is the use of peer recovery coaches to engage and establish ongoing relationships with overdose survivors in the ED setting.5–10 Peer recovery coaches provide emotional, informational, instrumental, and affiliated support.11 Systematic reviews have shown positive evidence for peer recovery coaches on substance use outcomes12,13 such as reducing substance use,14,15 relapse rates,16 ED visits,14 and re-hospitalization rates,17 as well as increasing treatment retention.18,19
Prior studies in urban, suburban, and rural EDs have shown that peer recovery coaches were able to achieve high levels of engagement with overdose survivors and people at risk of overdose in EDs, with subsequent referrals to inpatient and outpatient substance use disorder treatment.6,8,10,20 Although these studies show that peer recovery coaches in EDs are feasible, acceptable, and able to engage with people at risk for an opioid overdose, limited research exists on the type and composition of peer engagement and case management models that are most effective. A peer recovery coach, focused on connecting with the survivor, allows for an easier transition to a case manager, who delivers case management services using a strengths-based approach.21 The use of case management navigators in the ED may reduce ED visits22 and help improve clinical and social outcomes among frequent users of the ED.23
In an observational study, intensive case management improved psychosocial factors and engagement with care for people with severe mental illness and substance use disorders.24 Furthermore, in a systematic review of case management interventions for people with substance use disorders, most studies demonstrated that connection with—and among—healthcare providers seemed to improve treatment adherence along with overall functioning.25
To date, one study has described the partnership between peer recovery coaches and case management navigators to engage with survivors in the ED post-overdose.26 However, the authors did not report on project outcomes. Toward the goal of gaining new insights into a program with peer recovery coaches and case management navigators, we evaluated a pilot program, the Recovery Opioid Overdose Team (ROOT), a warm hand-off program that links overdose survivors to support and treatment services post-ED discharge. Due to grant stipulations, the ROOT program only included opioid overdoses.
Methods
Setting and Study Population
From 2012 to 2017, the rate of opioid overdose death in Washtenaw County increased from 7.12 to 16.86 deaths per 100,000 people.27 Recognizing the need to improve linkages to treatment for overdose survivors after an overdose reversal, the ROOT was developed under the leadership of the authors (MS, GA, and CHD). The ROOT program involved coordination of care with a county 24/7 Crisis Team, local law enforcement agencies, a substance use disorder treatment facility, a community mental health organization, and two local EDs. The two EDs were level one trauma hospitals that serve 85,000–104,000 patients a year.
Intervention
The goal of the ROOT was to engage with overdose survivors in the EDs and link them to treatment and recovery support services for up to 90 days post-ED discharge. The ROOT team was composed of a certified peer recovery coach with long-term recovery experience and a case management navigator who guides survivors to treatment and recovery services. The case management navigator also specialized in mental health care as many people who use drugs have a co-occurring mental health illness.28,29 The case management navigator had a bachelor’s degree in a mental health-related field with a limited license and community case management experience. The peer recovery coach had at least two years in recovery and state certification as a peer recovery coach along with a certification from the Connecticut Community for Addiction Recovery. The full-time certified peer recovery coach was deployed on a flexible schedule to meet the demand for overdose calls. The case management navigator was assigned within 24 hours of the overdose reversal.
The peer recovery coach and case management navigator worked together for the benefit of the survivor. The case management navigator’s purpose was to help the survivor identify barriers that limit their access to treatment. The case management navigator conducted an intake assessment to identify social, mental, and physical needs of the survivor and helped the survivor access social services (e.g., housing, insurance, utilities, cell phone). The peer recovery coach provided support for the survivor and helped the survivor integrate into the recovery community. The peer recovery coach, as a person who formerly used drugs, was able to identify with the survivor and encourage a contemplative move towards change through trust-building. By connecting with the survivor, the peer recovery coach and the case management navigator worked together to determine a plan of care.
Procedure
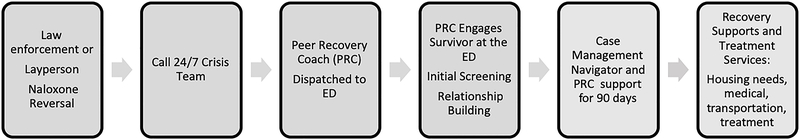
Originally, law enforcement contacted the county 24/7 Crisis Team at the time of an overdose, who then notified and activated the ROOT. At the scene of an overdose, law enforcement is usually the first responder. However, as the ROOT was being implemented, some law enforcement agencies were not notifying the 24/7 Crisis Team. Thus, the protocol was modified and ED physicians, nurses, and social workers were educated about the ROOT. It was these professionals who contacted the 24/7 Crisis Team if law enforcement failed to do so. In the ED, a peer recovery coach presented within one hour after the ROOT was notified to engage with the survivor and stayed with the survivor as long as they were welcome (Figure One). Once the peer recovery coach engaged with the survivor, an initial screening was completed: (1) demographic information; (2) the Adapted Recovery Capital Scale; (3) an assessment for safe housing, transportation, follow-up appointments, and up to three phone numbers; and (4) the release of information. However, the focus was not on completing the screening assessments, but establishing enough trust that was sufficient to connect with the survivor post-ED discharge. Therefore, the most critical information collected was how to contact the survivor in the community after discharge.
Figure 1.
Recovery Opioid Overdose Team Process
The peer recovery coach and case management navigator attempted to contact each survivor in the community 24 to 48 hours post-ED discharge for follow-up care that included: the initiation of a recovery plan, the provision of support (e.g., housing, transportation, clothing), and a referral to treatment and recovery support services. If the survivor continued to engage with ROOT, the recovery support services were tailored to the person. The list of recovery support services could include obtaining insurance, food stamps, clothing, household items, mental and medical health services, substance use disorder treatment options, housing, phones, and identification cards. If the survivor did not engage, ROOT conducted follow-up phone calls for 24 to 48 hours or made a face-to-face outreach attempt until the person requested not to be contacted or failed to respond. The present evaluation study of ROOT was deemed exempt by University of Michigan Institutional Review Board.
Measures
All data were collected using a retrospective chart review and included several demographic variables: sex, race/ethnicity, age, housing status, history of mental illness, and access to transportation.
ROOT process variables included: (1) who initiated the ROOT call and in which ED; (2) did a face-to-face encounter occur within 5 hours of the ROOT referral (yes/no); (3) was a recovery plan developed within the first week of ED discharge (yes/no); and (4) the number of in-person outreach attempts and phone calls. We defined initial ROOT engagement as any face-to-face interaction or telephone conversation with the survivor in the ED or in the community. Outcome variables included: (1) outpatient services; (2) residential treatment; (3) detoxification; (4) recovery housing; (5) medication treatment for opioid use disorder; (6) incarceration; (7) declined ROOT services; (8) left against medical advice; and (9) death.
Data analysis
Statistical analyses were conducted using Stata/SE software version 16.0 (StataCorp LLC, College Station, Texas, USA) with an emphasis on descriptive statistics.
Review
Between September 2017 and March 2019, 122 nonfatal overdose cases were referred to ROOT. The majority were male (63.9%), White (43.4%), between the ages of 19–39 years old (79.4%), had access to housing (80.2%), had a history of mental illness (54.9%), and had access to transportation (48.4%). (Table 1).
Table 1:
Demographic Characteristics
| N | % | |
|---|---|---|
| Sex | ||
| Male | 78 | 63.9 |
| Female | 44 | 36.1 |
| Race/Ethnicity | ||
| African American | 12 | 9.8 |
| Arab American | 2 | 1.6 |
| Asian | 1 | 0.8 |
| Hispanic | 1 | 0.8 |
| White | 53 | 43.4 |
| Missing | 53 | 43.4 |
| Age in Years | ||
| 19 – 29 | 51 | 41.8 |
| 30 – 39 | 46 | 37.6 |
| 40 – 49 | 9 | 7.4 |
| 50 – 59 | 8 | 6.6 |
| 60 – 69 | 8 | 6.6 |
| Housing in the Past 28 Days | ||
| House | 48 | 39.3 |
| Living with others | 41 | 33.6 |
| Structured living | 7 | 5.7 |
| Shelter | 2 | 1.6 |
| On the street | 14 | 11.5 |
| Missing | 10 | 8.2 |
| Mental Illness History | ||
| Yes | 67 | 54.9 |
| No | 55 | 45.1 |
| Access to Transportation | ||
| Yes | 59 | 48.4 |
| No | 42 | 34.4 |
| Missing | 21 | 17.2 |
The ROOT referrals were initiated largely by law enforcement officers (47.5%; n=58) and social workers (39.3%; n=48), with the remaining referrals by nurses (4.9%; n=6), physicians (4.1%; n=5), and unknown (4.1%; n=5). The majority (67.2%; n=82) of referrals were seen at one of the two hospital systems. Face-to-face encounters with ROOT occurred within 5 hours of the referral for 69.7% (n=85) of the survivors. Within a week of ED discharge, 81.1% (n=99) did not develop a recovery plan. The range of face-to-face interaction included 1 to 5 times for any given survivor, with 26 (21.3%) survivors receiving at least one face-to-face interaction post-ED discharge. The range of phone calls was 0–39 times per survivor with a median of two phone calls for any given survivor.
Out of 122 referrals received, 77.0% (n=94) of the survivors engaged with ROOT in the ED or in the community, and 23.0% (n=28) either left the ED against medical advice or were unengaged. To further delineate the 122 referrals received, 64.8% (n=79) of the survivors engaged with the peer recovery coach in the ED; 11.5% (n=14) were referred to ROOT, but left the ED against medical advice and were unengaged in the ED or community; 11.5% (n=14) did not leave against medical advice, but were unengaged in the ED or community; 7.4% (n=9) were engaged in the community; and 4.9% (n=6) left against medical advice, but were engaged with ROOT prior to leaving against medical advice. Thus, 16.4% (n=20) of the survivors left against medical advice. From the survivors who initially engaged with ROOT (n=94), follow-up interaction through a phone call or a face-to-face visit was successful for 48.9% (n=46) of the survivors.
Of the 122 referrals, 33.6% (n=41) received ongoing treatment services (n=20 outpatient, n=17 residential, n=2 detoxification facility, n=1 recovery housing, n=1 medication treatment for opioid use disorder), 2.5% were incarcerated (n=3), 2.5% were deceased (n=3), and 61.5 % (n=75) declined services.
Conclusions
To our knowledge, this is the first study to report outcomes for a community-wide coordinated service that used a team of peer recovery coaches and a case management navigator to connect overdose survivors to recovery support. Our pilot evaluation demonstrated that the ROOT, a program that extends the peer recovery coach model by including a case management navigator, was able to connect many overdose survivors to treatment services. Out of 122 referrals received by ROOT, 33.6% received some form of treatment services. As in other studies, we found that providing both a peer recovery coach and a case management navigator for each overdose survivor is feasible and often connects survivors from the ED to important services in the community.6,8,20,26
Interestingly, only one person chose to receive medication treatment for opioid use disorder. We do not know why so few sought this treatment over other treatments, since medication treatment for opioid use disorder is highly efficacious. Possible explanations could be stigma surrounding medication treatment for opioid use disorder treatment among people who use drugs30,31 and the limited number of providers for medication treatment for opioid use disorder available in the county during the evaluation period.
Different types of post-overdose community interventions have been implemented across the US, but limited evidence exists on the team composition that is most effective, as well as the timing of intervention and frequency of follow-ups.32 Anecdotal evidence from the ROOT program showed that including a case management navigator who has a deeper understanding of social services was critical to engaging the survivors with the community. The peer recovery coach with their “lived experience” was also important in identifying with the overdose survivor and motivating them to engage in treatment. Additional studies are needed to investigate if specific team compositions are more effective than others in engaging with survivors’ post-overdose reversals.
Although the ROOT pilot program shows promise, problems exist. Due to implementation barriers, the ROOT program received only one-third of non-fatal overdose referrals during the study period. In addition, overdose survivors who did not go to the ED were not referred because initial release agreements with ambulance services were not obtained. Both EDs had ongoing naloxone distribution programs, but we did not collect information on whether or not the individual received overdose education and naloxone upon discharge. In addition, we did not have a systematic follow-up procedure and thus, some details on follow-up activities were not captured. These included the type of social and recovery support services received, location of follow-up encounters, and referral to syringe access services. The data collection was limited by a retrospective chart review and thus, substance use disorder treatment history was not collected. In addition, the peer recovery coach and case management navigator were from two different agencies that had limited access to each other’s records. In the future when evaluating programs such as ROOT, better survivor data needs to be collected and could include: history of and current substance use and substance use treatment experiences; history of and current mental illness; prior overdose history; and use of medication treatment for opioid use disorder. Better process data must also be collected that includes the length of time to establish a recovery plan. Future studies should also include a larger sample and conduct an evaluation with a more rigorous design. Despite the limitations, our study describes an innovative, promising model using peer recovery coaches and case management navigators to connect overdose survivors to treatment and recovery support services post-overdose.
ACKNOWLEDGEMENTS
The authors thank the peer recovery coaches and case management navigators, Shad Jordan, Tami Lewis, Robert Johnson, Christina Mersereau, and Brent Steenbergh, for their passion and commitment to caring for overdose survivors. In addition, the authors wish to acknowledge Kathryn Lundquist and Kate Leary for their reviews of the manuscript.
FUNDING
Funding for the Recovery Opioid Overdose Team was provided by the Michigan Department of Health and Human Services, Office of Recovery Oriented Systems of Care through the Substance Abuse Prevention and Treatment Block Grant. The funders were not involved in the manuscript process and submission.
References
- 1.Hedegaard H, Miniño AM, Warner M. Drug Overdose Deaths in the United States, 1999–2018 Key Findings Data from the National Vital Statistics System, Mortality.; 1999. https://www.cdc.gov/nchs/products/index.htm. Accessed March 3, 2020.
- 2.Duber HC, Barata IA, Cioè-Peña E, et al. Identification, Management, and Transition of Care for Patients With Opioid Use Disorder in the Emergency Department. Ann Emerg Med. 2018;72(4):420–431. doi: 10.1016/j.annemergmed.2018.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vivolo-Kantor AM, Seth P, Gladden RW. Vital Signs: Trends in Emergency Department Visits for Suspected Opioid Overdoses — United States, July 2016–September 2017. MMWR Morb Mortal Wkly Rep. 2018;67(9):279–285. doi: 10.15585/mmwr.mm6709e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasegawa K, Brown DF, Tsugawa Y, Camargo CA Jr. Epidemiology of emergency department visits for opioid overdose: a population-based study. Mayo Clin Proc. 2014;89(4):462–471. doi: 10.1016/j.mayocp.2013.12.008 [doi] [DOI] [PubMed] [Google Scholar]
- 5.Samuels EA, Bernstein SL, Marshall BDL, Krieger M, Baird J, Mello MJ. Peer navigation and take-home naloxone for opioid overdose emergency department patients: Preliminary patient outcomes. J Subst Abuse Treat. 2018;94:29–34. doi: 10.1016/J.JSAT.2018.07.013 [DOI] [PubMed] [Google Scholar]
- 6.Waye KM, Goyer J, Dettor D, et al. Implementing peer recovery services for overdose prevention in Rhode Island: An examination of two outreach-based approaches. Addict Behav. 2019;89:85–91. doi: 10.1016/J.ADDBEH.2018.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samuels EA, Baird J, Yang ES, Mello MJ. Adoption and Utilization of an Emergency Department Naloxone Distribution and Peer Recovery Coach Consultation Program. Hwang U, ed. Acad Emerg Med. 2018;26(2):acem.13545. doi: 10.1111/acem.13545 [DOI] [PubMed] [Google Scholar]
- 8.Ashford RD, Meeks M, Curtis B, Brown AM. Utilization of Peer-Based Substance Use Disorder and Recovery Interventions in Rural Emergency Departments: Patient Characteristics and Exploratory Analysis. 2018. doi: 10.1037/rmh0000106 [DOI]
- 9.Wagner KD, Oman RF, Smith KP, et al. “Another tool for the tool box? I’ll take it!”: Feasibility and acceptability of mobile recovery outreach teams (MROT) for opioid overdose patients in the emergency room. J Subst Abuse Treat. May 2019. doi: 10.1016/j.jsat.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 10.Welch AE, Jeffers A, Allen B, Paone D, Kunins H V. Relay: A Peer-Delivered Emergency Department-Based Response to Nonfatal Opioid Overdose. Am J Public Health. 2019;109(10):1392–1395. doi: 10.2105/AJPH.2019.305202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.SERVICES USDOFHANDH. Emerging Peer Recovery Support Services And Indicators of Quality. Rockville, MD: Health Systems Research, Inc. (HSR); 2006. http://attcnetwork.org/ondcp_docs/CSATRCSPConferenceRpt2006.pdf. [Google Scholar]
- 12.Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer-Delivered Recovery Support Services for Addictions in the United States: A Systematic Review. J Subst Abuse Treat. 2016;63:1–9. doi: 10.1016/j.jsat.2016.01.003 [doi] [DOI] [PubMed] [Google Scholar]
- 13.Eddie D, Hoffman L, Vilsaint C, et al. Lived experience in new models of care for substance use disorder: A systematic review of peer recovery support services and recovery coaching. Front Psychol. 2019;10(JUN). doi: 10.3389/fpsyg.2019.01052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamon W. J& T. Recovery Coaching in Recovery Centers: What the Initial Data Suggest: A Brief Report from the Vermont Recovery Network. Montpelier, VT: Evidence-Based Solutions; 2013. https://vtrecoverynetwork.org/PDF/VRN_RC_eval_report.pdf. [Google Scholar]
- 15.Smelson DA, Kline A, Kuhn J, et al. A wraparound treatment engagement intervention for homeless veterans with co-occurring disorders. Psychol Serv. 2013;10(2):161–167. doi: 10.1037/a0030948 [doi] [DOI] [PubMed] [Google Scholar]
- 16.Boisvert Rosemary A, Martin Linda M, Maria G, Clarie AJ. Effectiveness of a peer‐support community in addiction recovery: participation as intervention. Occup Ther Int. 2008;15(4):205–220. doi: 10.1002/oti.257 [DOI] [PubMed] [Google Scholar]
- 17.Min SY, Whitecraft J, Rothbard AB, Salzer MS. Peer support for persons with co-occurring disorders and community tenure: a survival analysis. Psychiatr Rehabil J. 2007;30(3):207–213. [DOI] [PubMed] [Google Scholar]
- 18.Mangrum L Creating Access to Recovery through Drug Courts: Final Evaluation Report for the Texas Department of State Health Services. Austin, TX: University of Texas Addiction Research Institute; 2008. https://socialwork.utexas.edu/dl/files/cswr/institutes/ari/pdf/ATRFinalEvaluationReport-Final.pdf. [Google Scholar]
- 19.Tracy K, Burton M, Nich C, Rounsaville B. Utilizing peer mentorship to engage high recidivism substance-abusing patients in treatment. Am J Drug Alcohol Abuse. 2011;37(6):525–531. doi: 10.3109/00952990.2011.600385 [doi] [DOI] [PubMed] [Google Scholar]
- 20.Samuels EA, Baird J, Yang ES, Mello MJ. Adoption and Utilization of an Emergency Department Naloxone Distribution and Peer Recovery Coach Consultation Program. Acad Emerg Med. 2019;26(2):160–173. doi: 10.1111/acem.13545 [DOI] [PubMed] [Google Scholar]
- 21.Darnell JS. Navigators and assisters: Two case management roles for social workers in the Affordable Care Act. Health Soc Work. 2013;38(2):123–126. doi: 10.1093/hsw/hlt003 [DOI] [PubMed] [Google Scholar]
- 22.Bodenmann P, Velonaki VS, Griffin JL, et al. Case Management may Reduce Emergency Department Frequent use in a Universal Health Coverage System: a Randomized Controlled Trial. J Gen Intern Med. 2017;32(5):508–515. doi: 10.1007/s11606-016-3789-9 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumar GS, Klein R. Effectiveness of Case Management Strategies in Reducing Emergency Department Visits in Frequent User Patient Populations: A Systematic Review. J Emerg Med. 2013;44(3):717–729. doi: 10.1016/j.jemermed.2012.08.035 [DOI] [PubMed] [Google Scholar]
- 24.Morandi Silva B, Golay P, & Bonsack CS Intensive Case Management for Addiction to promote engagement with care of people with severe mental and substance use disorders: an observational study. Subst Abuse Treat Prev Policy. 2017;12(26). doi: 10.1186/s13011-017-0111-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Penzenstadler L, Machado A, Thorens G, Zullino D, Khazaal Y. Effect of Case Management Interventions for Patients with Substance Use Disorders: A Systematic Review. Front Psychiatry. 2017;8:10.3389/fpsyt.2017.00051. doi: 10.3389/fpsyt.2017.00051 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Powell KG, Treitler P, Peterson NA, Borys S, Hallcom D. Promoting opioid overdose prevention and recovery: An exploratory study of an innovative intervention model to address opioid abuse. Int J Drug Policy. 2019;64:21–29. doi: 10.1016/j.drugpo.2018.12.004 [DOI] [PubMed] [Google Scholar]
- 27.Michigan Department of Health and Human Services. Opioid Overdose Deaths. http://mi-suddr.com/blog/2018/09/26/opioid-heroin-poisonings/. Published 2018. Accessed April 24, 2019.
- 28.Abuse NI of D. Comorbidity: Addiction and Other Mental Illnesses. Vol 10–5771. U.S. Department of Health and Human Services, National Institutes of Health; 2010. [Google Scholar]
- 29.Quality C for BHS and. Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health. Vol HHS Public. Substance Abuse and Mental Health Services Administration (SAMHSA); 2015. http:www.samhsa.gov/data/. [Google Scholar]
- 30.Sue Woods J, Joseph H. Stigma from the Viewpoint of the Patient. J Addict Dis. 2015;34(3):238–247. doi: 10.1080/10550887.2015.1059714 [DOI] [PubMed] [Google Scholar]
- 31.Fanning Madden E. Intervention stigma: How medication-assisted treatment marginalizes patients and providers. 2019. doi: 10.1016/j.socscimed.2019.05.027 [DOI] [PubMed] [Google Scholar]
- 32.Bagley SM, Schoenberger SF, Waye KM, Walley AY. A scoping review of post opioid-overdose interventions. Prev Med (Baltim). August 2019:105813. doi: 10.1016/j.ypmed.2019.105813 [DOI] [PubMed] [Google Scholar]