Abstract
Gastric cancer has a high rate of metastasis, during which pre-metastatic niches (PMN) provide a supportive environment for the upcoming tumor cells. Exosomes are bilayer vesicles secreted by cells containing biological information that mediates communication between cells. Using exosomes, gastric cancer cells establish PMN remotely in multifarious perspectives, including immunosuppression, stroma remodeling, angiogenesis, mesothelial mesenchymal transformation, and organotropism. In turn, the cell components in PMN secrete exosomes that interact with each other and provide onco-promoting signals. In this review, we highlight the role of exosomes in PMN formation in gastric cancer and discuss their potential values in gastric cancer metastasis diagnosis, prevention, and treatment.
Keywords: exosome, gastric cancer, pre-metastatic niche, metastasis, tumor microenvironment
Introduction
Gastric cancer (GC) is one of the most common cancers globally, ranking the fifth in cancer incidence and the third in cancer-related death (1). Despite that surgery and perioperative radiotherapy or chemotherapy are the primary treatments for early-stage gastric cancer, more than half of patients with radical resection suffered local recurrence or distant metastasis (2). Moreover, many patients were initially diagnosed with metastatic gastric cancer that is unresectable (3). Due to high heterogeneity and drug resistance, the median survival rate of metastatic gastric cancer rarely exceeds one year, and the 5-year survival rate is less than 10% (4). In particular, peritoneal metastasis is the most common metastatic pattern of gastric cancer and has several negative features, including high incidence, high mortality, difficult diagnosis, and poor prognosis (5). It occurs in 55%-60% of advanced gastric cancers (6) and has a 5-year survival rate of only 2% (7).
One of the crucial steps during metastases is the formation of a pre-metastatic niche (PMN), which provides a receptive and supportive environment in terms of nutrients, extracellular matrix (ECM), stromal cell, and immune cells for cancer cells to seed in distant organs (8–11). The PMN is initiated and educated by PMN-promoting molecules secreted by the primary tumors, tumor-mobilized myeloid cells, and local stromal cells of the host. These niche-promoting molecules include tumor-secreted factors, cytokines, chemokines, inflammatory factors, microvesicles, oncosomes, and exosomes (11).
Recently, studies revealed that exosomes play essential roles in PMN formation (12). Ranging from 40 to 150 nm in size and enveloped by lipid bilayers, exosomes are a class of extracellular vesicles released by various cells (13). They contain a variety of cell components, including DNA, RNA, lipids, and proteins, that can be transported to and can regulate recipient cells (13). Importantly, they carry a variety of cytokines, such as TGF-β, TNF-α, IL-6, IL-8, and IL-10, to maintain their stability and transfer to distant recipient cells (14). In particular, tumor-derived exosomes (TDEs) travel from their original site to distant potential metastatic sites and educate the PMN components with their cargo, thereby facilitating tumor cell arrival and colonization (15). In addition, exosomes from non-tumor cells may also participate in this process (15–18). In this review, we summarize the roles of exosomes in PMN formation in gastric cancer, as well as their implications in gastric cancer metastasis, prevention, and treatment.
Roles of Exosomes in Gastric Cancer Malignity
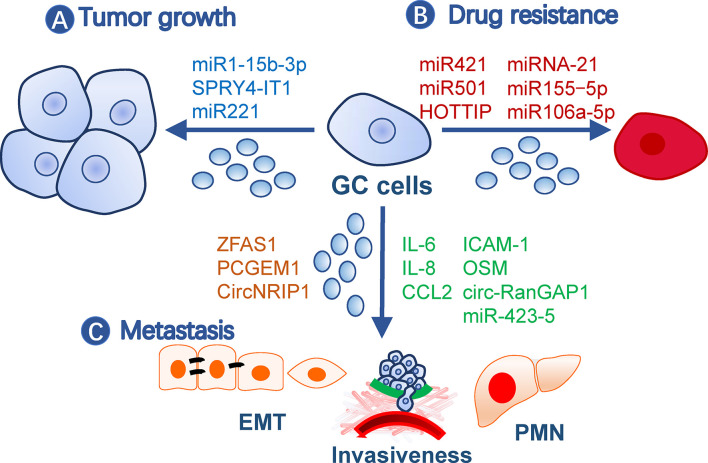
Exosomes contribute to malignity through their roles in gastric cancer growth, drug resistance, and metastasis ( Figure 1 ).
Figure 1.
Roles of exosomes in gastric cancer malignity. Exosomes from gastric cancer cells or other cells contribute to malignity in (A) tumor growth, (B) drug resistance, and (C) metastasis. Exosomes may affect all processes of metastasis, such as EMT, invasiveness, and pre-metastatic niche formation. The small circles represent exosomes, and effective molecules were listed by the arrows. EMT, Epithelial-mesenchymal transition; GC, gastric cancer; PMN, pre-metastatic niche.
Promotion of Gastric Cancer Growth
Gastric cancer TDE contents, including proteins and nucleic acids, have a broad impact on tumor growth. For example, TDEs secreted by BGC-823 cells can transfer miR-15b-3p to SGC-7901 or GES-1 cells to enhance their development by inhibiting the DYNLT1/Caspase-3/Caspase-9 signaling pathway (19). SPRY4-IT1, a long noncoding RNA (lncRNA), promotes gastric cancer proliferation and migration by sponging miR-101-3p, is upregulated in serum exosomes of gastric cancer patients, and is correlated with patient outcomes (20). In addition, exosomes from non-tumor cells may also impact tumor growth. For example, exosomes from gastric cancer tissue-derived mesenchymal stem cells (MSCs) are onco-promoting by transmitting miR-221 (21), while gastric mucosal epithelial cells induce apoptosis of gastric cancer cells through exosomal proteins (22).
Induction of Drug Resistance
Gastric cancer cells may transmit drug resistance to other sensitive clones by communication with exosomes. For instance, doxorubicin-resistant SGC7901 cells conferred the same drug resistance in drug-sensitive cells via exosomal miR-501 that targets BLID (23). Cisplatin resistance was transmitted by exosomal lncRNA HOTTIP, which targets the miR-218/HMGA1 axis in cisplatin-sensitive cells (24). M2 macrophage-derived exosomes also transferred cisplatin-resistance through miRNA-21 targeting PETN in recipient cells (25). A paclitaxel-resistant gastric cancer cell line, MGC803R, can induce chemoresistance in paclitaxel−sensitive cells, MGC803S, by exosomal delivery of miR−155−5p, which further suppresses GATA3 and TP53INP1 in the latter (26). In addition, TFAP2E hypermethylation facilitates packaging of miR-106a-5p and miR-421 into gastric cancer exosomes, which subsequently induce 5−fluorouracil resistance in tumor cells (27).
Facilitation of Gastric Cancer Metastasis
Metastasis is a multistep process including cancer cell motility, local infiltration, intravasation, transit in the blood or lymph, extravasation, and proliferation in competent organs (28). Epithelial-mesenchymal transition (EMT) is a biological process associated with increased cell motility, resistance to apoptosis and senescence, and suppressed immune reaction during the initial step of metastasis (29) and is closely regulated by TDEs (30). LncRNA ZFAS1 and PCGEM1 are highly enriched in gastric cancer TDEs and are capable of inducing EMT phenotypes among cancer cells during metastasis, in which PCGEM1 stabilizes SNAI1 (31, 32). CircNRIP1, a circular RNA, can also be transmitted among gastric cancer cells through exosomes and regulate EMT through a circNRIP1-miR-149-5p-AKT1/mTOR axis (33). In addition, exosomal TRIM3 was found to be an anti-EMT factor, and its levels were downregulated in gastric cancer TDEs (34). Besides TDEs, malignant ascites-derived exosomes also played essential roles in enhancing the EMT signaling in gastric cancer cells during peritoneal metastasis (35). Invasiveness is also critical during the initial and terminal processes of tumor metastasis and is easy to be quantified by in vitro and in vivo methods. This ability of gastric cancer cells can be elevated by exosomal miR-423-5p, which is remarkably correlated with lymph node metastasis (36). In SGC cells, CD97 facilitated cell invasions through packaging miRNAs into exosomes, which mediated the MAPK signaling pathway (37). circ-RanGAP1 is elevated in plasma exosomes from gastric cancer patients and facilitates gastric cancer invasiveness by upregulating VEGFA expression (38). Besides, omentum may play an active role in enhancing gastric cancer cell invasiveness by exosomal proteins (i.e., IL-6, IL-8, ICAM-1, CCl2, and OSM) (39).
Besides these processes, PMN formation is also indispensable for distant metastasis and is closely regulated by exosomes. Next, we will focus on the roles of exosomes in gastric cancer PMN formation.
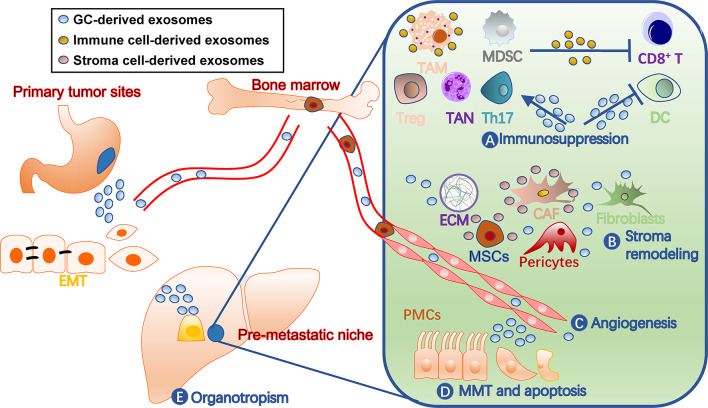
Roles of Exosomes in Gastric Cancer PMN Formation
A PMN has distinct characters from normal tissue environments, such as immunosuppression, angiogenesis, and organotropism (11). Cells involved in shaping these features are fine-tuned by tumor-secreted factors, including TDEs ( Figure 2 ). They not only act on various immune cells for immunosuppression, but also remodel stromal components into tumor-supporting types in PMN. Additionally, exosomes target endothelial cells for angiogenesis and organ-specific cells, such as peritoneal mesothelial cells (PMCs), for organotropism. In turn, the immune and stromal cells secrete exosomes that benefit tumor cells and communicate among different cells (40).
Figure 2.
Roles of exosomes in gastric cancer pre-metastatic niches. Exosomes contribute to pre-metastatic niche formation through multiple mechanisms, including (A) immunosuppression by facilitating TAM and TAN polarization, inhibiting dendritic cell maturation and T cell activation, and inducing MDSCs, (B) stroma remodeling by acting on stromal cells such as CAF and MSCs and ECM balance, (C) angiogenesis, (D) MMT and apoptosis of tissue-specific cells, such as PMCs, and (E) organotropisms. The liver is drawn to represent a metastatic target. CAF, cancer-associated fibroblast; DC, dendritic cell; ECM, extracellular matrix; EMT, epithelial-mesenchymal transition; GC, gastric cancer; MDSCs, myeloid-derived suppressor cells; MMT, mesothelial-mesenchymal transition; MSC, mesenchymal stem cell; PMC, peritoneal mesothelial cell; TAM, tumor-associated macrophage; TAN, tumor-associated neutrophil; Th17, T-helper 17 cell; Treg, regulatory T cell.
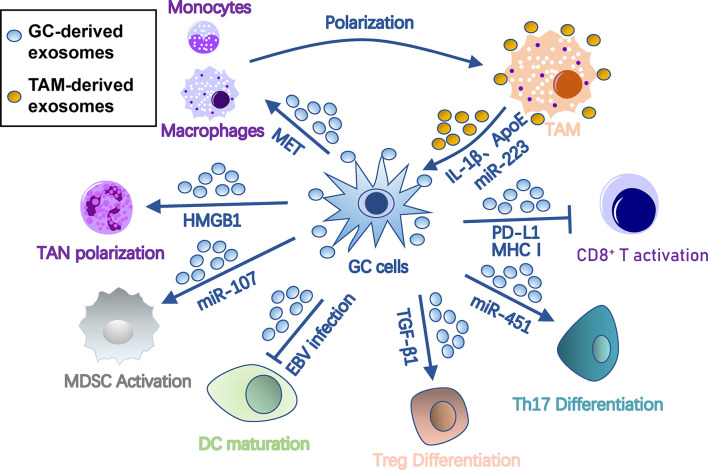
Immunosuppression
To metastasize, tumor cells must evade immune surveillance and killing in the seeding organ. Thus, the PMN must orchestrate immunosuppression of all types of immune cells to protect colonizing tumor cells from immune attack. Exosomes are one of key factors that orchestrate this process among cancer cells, PMN, and immune cells ( Figure 3 ). Specifically, exosomes polarize tumor-associated macrophages (TAMs), induce tumor-associated neutrophils (TANs), inhibit dendritic cell maturation, regulate T cell differentiation and function, and induce myeloid-derived suppressor cells (MDSCs).
Figure 3.
Roles of exosomes in immunosuppression in gastric cancer pre-metastatic niches. Gastric cancer-derived exosomes cause immunosuppression by suppressing DC/CD8+ T cell activation and DC maturation and inducing differentiation of TAM, TAN, MDSC, Treg, and Th17 cells. In turn, TAM provides onco-promoting signals to tumors and stromal cells through its exosomes. Arrows represent activation, whereas bar-headed arrows represent inhibition. CAF, cancer-associated fibroblast; DC, dendritic cells; ECM, extracellular matrix; EMT, epithelial-mesenchymal transition; MDSC, myeloid-derived suppressor cell; MMT, mesothelial-mesenchymal transition; MSC, mesenchymal stem cell; PMC, peritoneal mesothelial cell; TAM, tumor-associated macrophage; TAN, tumor-associated neutrophil; Th17, T-helper 17 cell; Treg, regulatory T cell.
Polarization of TAMs
Macrophages are the most abundant immune cells with two types of polarized cells, the tumor-suppressing M1 and tumor-promoting M2 (41). TAMs are primarily M2 polarized, capable of promoting tumors by regulating tumor malignancy, angiogenesis, and anti-tumor immunity (42). In gastric cancer, TDEs promote M2 transformation and facilitate production of pro-inflammatory factors by stimulating NF-κB pathways in macrophages (43). Gastric cancer TDEs also induce monocytes to differentiate into PD-1+ macrophages, which exhibit an M2-like surface profile and impair CD8+ T cell function (44). In Helicobacter pylori-infected gastric cancer, TDEs are enriched with activated MET, which educates the macrophages towards an M2 phenotype with high IL-1β expression (45).
In turn, TAM-derived exosomes may act on gastric cancer cells. ApoE is a highly specific protein in TAM-derived exosomes that can activate the PI3K-Akt signaling pathway in gastric cancer cells to rebuild the cytoskeleton for migration (46). Exosomal miR-223 derived from macrophages can provide proliferation/EMT signals for metastasis via the PTEN-PI3K/AKT pathway (47). Interestingly, during peritoneal PMN formation, TAM can transfer TDEs from gastric cancer cells to surrounding stromal cells, including peritoneal mesothelial cells, fibroblasts, and endothelial cells, and induce their conversion into cancer-associated fibroblasts (CAF)-like cells (48).
Induction of TANs
Like macrophages, neutrophils can also polarize into N1 or N2 phenotypes. N1 cells possess anti-tumor activity due to their immune-activating cytokines/chemokines that recruit and activate CD8+ T cells (49), while most TANs appear to have “pro-tumorigenic” N2 phenotypes (50). TANs release multifarious pro-PMN substrates, including reactive oxygen species and reactive nitrogen species that cause genetic instability and carcinogenesis (51), elastase that degrades tumor-suppressing proteins (52), prostaglandin E2 that drives wound inflammation-mediated pre-neoplastic cell proliferation (53), VEGF and MMP9 that facilitate angiogenesis (54), and CCL2/17 that recruits other immunosuppression cells (55, 56). In gastric cancer, membrane HMGB1 on TDEs interacts with TLR4 on neutrophils, which induces TAN polarization through NF-κB and an autophagic response to reshape the metastatic niche (57).
Inhibition of Dendritic Cell Maturation
Dendritic cells are the central antigen-presenting cells in anti-tumor immunity. Epstein-Barr virus (EBV)-positive gastric cancer is characterized by an abundance of infiltrated-immune cells, including dendritic cells, but with suppressed anti-tumor immunity. Hinata et al. revealed that EBV-positive gastric cancer has more TDE secretion than EBV-negative gastric cancer (58). These TDEs suppress dendritic cell maturation, represented with low CD86 expression, and inhibit activation of other immune cells (58).
Regulation of T Cell Differentiation and Function
Anti-tumor immunity is largely imposed by T cells, which are potential targets of TDEs for immunosuppression. Gastric cancer TDEs can induce T cell apoptosis by mediating PI3K proteasome degradation and caspases 3, 8, and 9 activation (59). TDE-bound PD-L1 is an immune response “brake” that is more stable than soluble PD-L1 and is co-expressed with MHC-I. Thus, TDE-bound PD-L1 is able to lead to much stronger T cell dysfunction than soluble PD-L1 in gastric cancer (60).
A group of immunomodulatory T cells, such as regulatory T (Treg) cells, are essential in coordinating distinct immunoregulatory programs and creating an immunologically permissive environment for tumor metastasis (61). Gastric cancer TDEs also induce FOXP3+ Treg cell differentiation from naive T cells through exosomal TGF-β1 (62). In addition, glucose deprivation can induce an exosome-mediated miR-451 redistribution from tumor to T cells, resulting in T-helper 17 cell differentiation in gastric cancer (63). A lncRNA, RP11-323N12.5, is found upregulated in gastric cancer cells as well as tumor-infiltrated lymphocytes (64). Upregulated RP11-323N12.5 in tumor-infiltrated lymphocytes is derived from TDEs and contributes to Treg differentiation by upregulating the Hippo pathway effector, YAP1 (64).
In gastric cancer, TDEs may also regulate T cell functions indirectly by a third cell. They can regulate immunomodulation function of MSCs through the NF-κB signaling pathway, which further activates CD69 and CD25 on the surface of T cells (65). Furthermore, gastric cancer TDEs also have immunogenicity to induce dendritic cell maturation for tumor-specific T cell responses (66).
Recruitment of MDSCs
MDSCs are a heterogeneous population of immature myeloid cells that suppress immunity during tumor progression, inflammation, or infection (67). They are indispensable for PMN formation due to their roles in immunosuppression, vascular permeability, and collagen remodeling (68). Many immune cells in PMNs, including cytotoxic T cells, Treg cells, NKT cells, dendritic cells, and macrophages, are regulated by MDSCs during tumor metastasis (69). TDEs have been shown to transform bone marrow myeloid cells into MDSCs (70). In gastric cancer, TDEs also help MDSC expansion by delivering miRNA-107 targeting DICER1 and PTEN-PI3K signaling in the recipient MDSC (71).
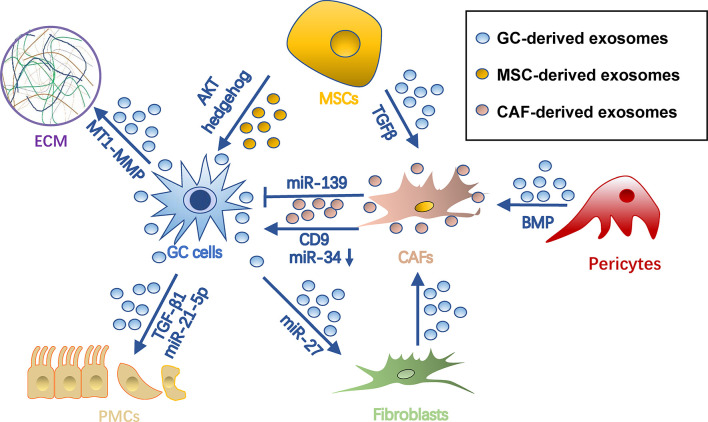
Stroma Remodeling
The survival of cancer cells in the metastatic site highly depends on the stromal microenvironment, which is composed of fibroblasts, pericytes, MSC, endothelial cells, ECM, and vasculature (72). TDEs have been shown to remodel stroma by reprograming these stromal cells and ECMs for tumor colonization ( Figure 4 ).
Figure 4.
Roles of exosomes in stroma remodeling in gastric cancer pre-metastatic niches. Gastric cancer cell-derived exosomes can convert pericytes, fibroblasts, and MSCs into CAFs. Also, they remodel ECM and induce MMT and apoptosis of PMCs through different cargo during PMN formation. Meanwhile, exosomes from MSCs and CAFs can in turn promote tumor cell progression. Arrows represent activation, whereas bar-headed arrows represent inhibition. CAF, cancer-associated fibroblast; ECM extracellular matrix; MSC, mesenchymal stem cell; PMN, pre-metastatic niche.
Regulation of CAF Reprogramming
CAFs are a group of heterogeneous cells that may differentiate from multiple origins (73) and are potent regulators of tumors and tumor microenvironments (74, 75). Exosomes are important for inducing pro-tumorigenic/metastatic CAFs. For example, gastric cancer TDEs contain high levels of miRNA-27a and can deliver them into fibroblasts for CAF reprogramming in a CSRP2-dependent manner (76). Conversely, CAFs with miRNA-27a provide a favorable environment pleiotropically for malignant behavior of gastric cancer cells (76). TGF-β on gastric cancer TDEs triggers differentiation of umbilical cord-derived MSC into CAF by activating the Smad pathway (77). In addition, gastric cancer TDEs induce transition of pericytes into CAFs by exosome-mediated BMP transfer and PI3K/AKT and MEK/ERK pathway activation (78).
Exosomes from CAF in turn impact gastric cancer cells. CAF-derived CD9+ exosomes potently stimulate MMP2 expression and migration in scirrhous-type gastric cancer cells (OCUM-12 and NUGC-3 cells) (79). This process was hindered by adding CD9 neutralizing antibodies or siRNAs targeting CD9 (79). In addition, CAF-derived exosomes are internalized by gastric cancer cells and facilitate gastric cancer proliferation and invasion (80). This process was mediated by exosomal miRNA-34, which targets 16 onco-promoting molecules in gastric cancer (80). Notably, not all CAF-derived exosomes are onco-promoting. For instance, the exosomal miR-139 derived from gastric cancer CAFs is anti-metastatic, decreasing MMP11 in tumor microenvironments (81).
Onco-Promoting Exosomes Derived from MSCs
MSCs are another origin of tumor stromal cells, which are able to differentiate into several types of mesenchymal cells, including adipocytes, CAFs, pericytes, and endothelial-like cells (82). They orchestrate an environment associated with tumor survival, angiogenesis, and immunosuppression, which all contribute to tumor growth and metastasis (83). MSC-derived exosomes have been proven indispensable during this process. In GC, they promote tumor growth and migrations via activation of the AKT (84) or hedgehog pathway (85). Besides, bone marrow-derived MSC exosomes are able to activate the ERK1/2 pathway in gastric cancer cells to upregulate VEGF expression, promoting angiogenesis (86). In a gastric cancer precancerous model, p53 deficient bone marrow-MSCs could secrete UBR2-rich exosomes, which activate the Wnt/catenin pathway in tumor cells and result in tumor growth, motility, and stemness (87). MSC exosomes could also induce chemoresistance in gastric cancer cells by antagonizing 5-fluorouracil-induced apoptosis and enhancing expression of multidrug resistance-associated proteins (88). This process is mediated by the calcium/calmodulin-dependent protein kinases and Raf/MEK/ERK kinase cascades (88).
Alternation of ECM Dynamics
ECM is a dynamic extracellular environment with continuous degradation, deposition, and modification and functions to fine-tune the elasticity and compressive or tensile strength of tissues (89). Dysregulated ECM remodeling includes irreversible proteolysis and crosslinking, which in turn influences microenvironmental cues, angiogenesis, and tissue biomechanics, being crucial for PMN formation (90). As far as we know, exosomes not only influence ECM dynamics directly, but also induce imbalances of metalloproteinases (MMPs) and tissue inhibitors of MMPs (TIMPs) released by tumor or stromal cells. Being rich in stable MMPs, TDEs help degrade collagen, laminin, and fibronectin to reshape ECM (91, 92). mRNA of membrane type 1-MMP is contained in and protected by gastric cancer TDEs and is highly associated with lymphatic metastasis (93). CD63 is an exosome marker as well as a receptor for TIMP1 (94). CD63 positivity in gastric cancer cells or gastric cancer stromal cells is significantly correlated with lymph node metastasis, so it is inferred that CD63-positive exosomes of gastric cancer might also be associated with metastatic niche formation (95), probably by binding with and inhibiting TIMP1. CD9+ exosomes derived from CAF also potently stimulate MMP expression in tumor environments (79).
Inducing PMC Mesothelial-Mesenchymal Transition
The peritoneum is composed of a layer of PMCs and connective tissues and is the first barrier to tumor attachment and invasion in peritoneal metastasis (96, 97). Mesothelial-mesenchymal transition (MMT) has been observed to occur early in intraperitoneal dissemination, thus being an important process of peritoneal PMN formation (98, 99). Through MMT, mesothelial cells acquire a migratory phenotype expressing pro-inflammatory cytokines, angiogenetic factors, and a specialized ECM to disintegrate the peritoneum (100). Gastric cancer TDEs are able to induce MMT of PMCs (35, 101–103). For example, TDE-derived miR-21-5p can promote MMT of PMCs by suppressing SMAD7 (101). In addition, internalization of gastric cancer TDEs upregulates expression of adhesion-related molecules, including fibronectin-1 and laminin-γ1, in PMCs and promotes PMC-gastric cancer cell adhesion, which favors tumor settlement (102). Additionally, gastric cancer TDEs also elicit mesothelial barrier disruption and fibrosis by inducing concurrent apoptosis and MMT (103). Ascites-derived exosomes also potently facilitated TGF-β1-induced MMT of PMCs during gastric cancer peritoneal metastasis (104).
Angiogenesis
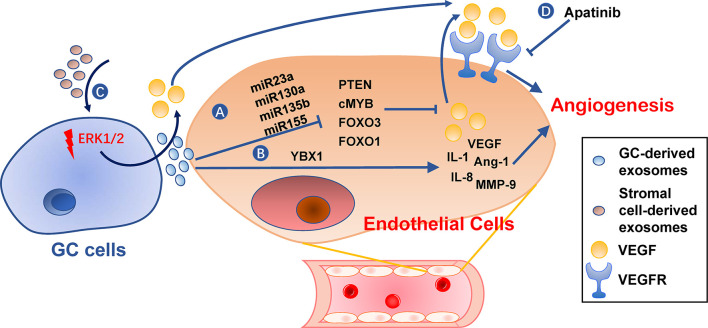
Angiogenesis is an essential step in the establishment of PMN by providing oxygen and nutrients for tumor growth and allowing circulating tumor cells to arrive (105). Furthermore, angiogenic factor VEGF has an immunosuppressive effect during PMN establishment (106, 107). Gastric cancer TDEs can activate angiogenesis by delivering several types of miRNAs to vascular endothelial cells, including miR-130a targeting c-MYB (108), miR-135b targeting FOXO1 (109), miR-155 targeting FOXO3 (110) and c-MYB (111), miR-23a targeting PTEN (112) ( Figure 5 ). Transmembrane protein Tetraspanin 8 on gastric cancer TDEs can also activate vascular endothelial cells by stimulating its ERK/MAPK pathway (113). Exosomal YB-1 from gastric cancer also promotes angiogenesis from endothelial cells by upregulating specific angiogenic factors (114). Irradiation-treated gastric cancer can produce TDEs with enhanced ability to induce angiogenesis of vascular endothelial cells (115). Consequently, VEGFR inhibitor, Apatinib, inhibits this process and could be used in combination with radiotherapy for better results (115). In addition, exosomes derived from non-tumor cells, such as MSCs, may also be angiogenic (86).
Figure 5.
Roles of exosomes in angiogenesis. (A, B) Gastric cancer cell-derived exosomes can induce expression of pro-angiogenesis molecules, such as VEGF, IL-1, IL-8, Ang-1, and MMP-9, in endothelial cells by delivering miRNAs (A) or YBX1 (B). (C) Stromal cell-derived exosomes or tumor-derived exosomes also promote VEGF expression in gastric cancer cells. (D) VEGFR inhibitors, such as Apatinib, can hinder angiogenesis caused by these exosomes. GC, gastric cancer.
Organotropism
Metastatic organotropism is one of the characteristics of PMN (11). Organotropism results from an active selection and education by the primary gastric cancer cells of a specific distant microenvironment into a PMN (116). As reported by Hoshino and colleagues, integrin patterns in TDEs determine the organotropic metastases through an integrin-dependent uptake of exosomes by different organs (117). For example, exosomal integrins α6β4 and α6β1 are lung-tropic, while exosomal integrin αvβ5 was liver-tropic (117). The uptake of exosomal integrin by local cells activates Src phosphorylation and pro-inflammatory factors to allow PMN establishment (117).
In gastric cancer liver metastasis, TDEs deliver membrane EGFR to liver stromal cells prior to liver metastasis (118). Recipient cells then activate hepatocyte growth factor paracrine, which provides a favorable environment for tumor landing by binding to their c-MET receptor (118). The lymphotropic gastric cancer cells produce CD97-enriched TDEs, which effectively aid gastric cancer metastasis by creating distant lymphatic PMN (119). Additionally, PMCs are peritoneum-specific cells and, therefore, the PMC-targeting exosomes mentioned above are considered peritoneum-tropic (101–103). Before gastric cancer peritoneal metastasis, Wnt3a-containing TDEs induce PMC infiltration into the gastric wall to create PMN in these sites, which in turn promoted subserosal invasions of gastric cancer cells and further dissemination (120). In addition, three miRNAs, namely miR-10b-5p, miR-101-3p, and miR-143-5p, are proposed biomarkers for gastric cancer lymph node, ovarian, and liver metastasis, respectively (121).
Implications and Perspectives
Biomarkers and Liquid Biopsy
The lipid bilayer membrane structure of the exosome maintains the stability of its cargo well, so exosomes have great potential as non-invasive biopsy specimens for cancer detection and prognosis (122, 123). So far, we may see potential roles of exosomes as biomarkers in gastric cancer metastasis prediction, prevention, and treatment. Some studies have shown evidence of clinical relevance between exosome and gastric cancer metastasis (summarized in Table 1 ). For example, exosomal PSMA3 and PSMA6 are explicitly enriched in serum during metastatic gastric cancer, but not primary gastric cancer, thus being a potential biomarker for gastric cancer metastasis (124). Further, exosomal miR-10b-5p, miR-101-3p, and miR-143-5p were proposed biomarkers for gastric cancer lymph node, ovarian, and liver metastasis, respectively, helping distinguish gastric cancer patients with various types of metastasis (121). Exosomal miRNAs from peritoneum lavage fluid, including miR-21 and miR-1225-5p, are specifically elevated in gastric cancer peritoneal metastasis after curative gastric cancer resection, thus providing a novel approach to early diagnosis of peritoneal dissemination of gastric cancer (125). However, evidence is limited up to date.
Table 1.
Evidence of clinical relevance between exosomal contents and metastatic sites in gastric cancer.
| Exosomal contents | Origin | Associated metastatic sites | Citation |
|---|---|---|---|
| miR-10b-5p | Plasma | Lymph node | (121) |
| miR-101-3p | Plasma | Ovary | (121) |
| miR-143-5p | Plasma | Liver | (121) |
| miR-21 | Peritoneum lavage fluid | Peritoneum | (124) |
| miR-320c | |||
| miR-1225-5p | |||
| let-7g-5p | Serum | Nerve infiltration | (123) |
| miR-146b-5p | |||
| PSMA3 | Serum | Distant metastasis | (125) |
| PSMA6 | |||
| EGFR | Serum | Liver | (118) |
| MT1-MMP mRNA | Serum | Lymph node | (93) |
Cancer Prevention and Treatment
The characteristics of exosomes, including high biocompatibility, safety, and nano-sized diameters, allow effective drug-loading capacity and long blood circulation half-life. Thus, they serve as an ideal system to deliver cytokines, DNA, RNA, adjuvants, and even vaccines for treatment (126, 127). For example, HGF siRNA packed in exosomes can be transported into gastric cancer cells, where it decreases tumor growth rates and blood vessels in vivo (128). Exosomes from heat-treated gastric cancer malignant ascites have improved immunogenicity, being able to promote dendritic cell maturation and induce a tumor-specific cytotoxic T cell response (66). The organotropic factors, such as integrins on the exosome surface, could be used to improve targeting specificity and deliver drugs to specific tissues (129). However, it remains unknown whether exosome-based drug delivery could be used to prevent or treat gastric cancer metastasis to a specific organ.
Perspectives
Despite immature clinical usage of exosomes in cancer, we believe it will be an important utility in metastasis assessment, prevention, and treatment in the future. First, methods such as nano-plasmonic sensors (14), microfluidic exosome analysis (130), and surface plasmon resonance imaging (131) were developed for exosome analysis with a small amount of sample, compared with routine methods. These techniques will allow exosomes to be a good tool for liquid biopsy. Second, because cancer cells, immune cells, and stromal cells all produce exosomes into the circulation, they will provide comprehensive information from tumor environments and PMN, as long as we have effective ways of exosome classification (132). An interesting technique utilizes a proximity barcoding method to profile surface proteins on individual exosomes, which allows both tissue origination and quantification of exosomes in mixed samples (133). Further classification based on exosome function, organophilicity, biological distribution, and immunogenicity, at single exosome levels, may be considered (134). Third, besides exosome-based drug delivery, another direction is to target PMN-promoting exosomes, based on their essential role in coordinating PMN formation. Although not feasible currently, targeting exosomes may come true in the future with fine characterizations of specific cell-derived exosomes and membrane markers for targeting. Fourth, some chemotherapeutics can induce certain exosome secretions and alters exosome composition, which degrades ECM and activates macrophage to release TNF-α (135). Therefore, whether these “chemo-exosomes” are PMN-promoting may be taken into consideration when choosing therapeutic regimens. Last but not least, despite of insufficient evidence, some studies have reported how oncogenes, cytokines, and exosomes interacted with each other in cancer, as reported in a squamous cancer cell line that cortactin promotes exosome secretion (136). Targeting genes or cytokines that regulate exosome packaging and secretion would be another way for exosome elimination and PMN inhibition.
Conclusion
Exosomes play a vital role in establishing PMN formation by immunosuppression, angiogenesis, stroma remodeling, PMC MMT, and organotropism and have great potential in metastasis prediction, prevention, and treatment. Yet, their clinical usage is limited, and further studies are needed to validate the translational value of exosomes in PMNs of gastric cancer.
Author Contributions
JG searched databases and collected studies. JG and SL summarized the contents, wrote the manuscript, and drew the figures. QX, XZ, MH, and XD helped in data collection and figure design. LL designed this review, edited the article, and supervised the work. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (81172487 to LL and 81500092 to SL) and Natural Science Foundation of Shandong Province (ZR201702180008 to LL).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The manuscript was edited by Alexandra H. Marshall (Marshall Medical Communications).
References
- 1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin (2018) 68:394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2. Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric Cancer. Lancet (2020) 396:635–48. 10.1016/S0140-6736(20)31288-5 [DOI] [PubMed] [Google Scholar]
- 3. Digklia A, Wagner AD. Advanced Gastric Cancer: Current Treatment Landscape and Future Perspectives. World J Gastroenterol (2016) 22:2403–14. 10.3748/wjg.v22.i8.2403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Orditura M, Galizia G, Sforza V, Gambardella V, Fabozzi A, Laterza MM, et al. Treatment of Gastric Cancer. World J Gastroenterol (2014) 20:1635–49. 10.3748/wjg.v20.i7.1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thomassen I, van Gestel YR, van Ramshorst B, Luyer MD, Bosscha K, Nienhuijs SW, et al. Peritoneal Carcinomatosis of Gastric Origin: A Population-Based Study on Incidence, Survival and Risk Factors. Int J Cancer (2014) 134:622–8. 10.1002/ijc.28373 [DOI] [PubMed] [Google Scholar]
- 6. Kanda M, Kobayashi D, Tanaka C, Iwata N, Yamada S, Fujii T, et al. Adverse Prognostic Impact of Perioperative Allogeneic Transfusion on Patients With Stage II/III Gastric Cancer. Gastri Cancer (2016) 19:255–63. 10.1007/s10120-014-0456-x [DOI] [PubMed] [Google Scholar]
- 7. Kanda M, Kodera Y. Molecular Mechanisms of Peritoneal Dissemination in Gastric Cancer. World J Gastroenterol (2016) 22:6829–40. 10.3748/wjg.v22.i30.6829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kaplan RN, Rafii S, Lyden D. Preparing the “Soil”: The Premetastatic Niche. Cancer Res (2006) 66:11089–93. 10.1158/0008-5472.CAN-06-2407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chin AR, Wang SE. Cancer Tills the Premetastatic Field: Mechanistic Basis and Clinical Implications. Clin Cancer Res (2016) 22:3725–33. 10.1158/1078-0432.CCR-16-0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, et al. VEGFR1-Positive Haematopoietic Bone Marrow Progenitors Initiate the Pre-Metastatic Niche. Nature (2005) 438:820–7. 10.1038/nature04186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu Y, Cao X. Characteristics and Significance of the Pre-metastatic Niche. Cancer Cell (2016) 30:668–81. 10.1016/j.ccell.2016.09.011 [DOI] [PubMed] [Google Scholar]
- 12. Meehan K, Vella LJ. The Contribution of Tumour-Derived Exosomes to the Hallmarks of Cancer. Crit Rev Clin Lab Sci (2016) 53:121–31. 10.3109/10408363.2015.1092496 [DOI] [PubMed] [Google Scholar]
- 13. Kalluri R. The Biology and Function of Exosomes in Cancer. J Clin Invest (2016) 126:1208–15. 10.1172/JCI81135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Im H, Shao H, Park YI, Peterson VM, Castro CM, Weissleder R, et al. Label-Free Detection and Molecular Profiling of Exosomes With a Nano-Plasmonic Sensor. Nat Biotechnol (2014) 32:490–5. 10.1038/nbt.2886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wortzel I, Dror S, Kenific CM, Lyden D. Exosome-Mediated Metastasis: Communication From a Distance. Dev Cell (2019) 49:347–60. 10.1016/j.devcel.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 16. Ingenito F, Roscigno G, Affinito A, Nuzzo S, Scognamiglio I, Quintavalle C, et al. The Role of Exo-miRNAs in Cancer: A Focus on Therapeutic and Diagnostic Applications. Int J Mol Sci (2019) 20:4687. 10.3390/ijms20194687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Li Y, Zheng Q, Bao C, Li S, Guo W, Zhao J, et al. Circular RNA is Enriched and Stable in Exosomes: A Promising Biomarker for Cancer Diagnosis. Cell Res (2015) 25:981–4. 10.1038/cr.2015.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Théry C, Ostrowski M, Segura E. Membrane Vesicles as Conveyors of Immune Responses. Nat Rev Immunol (2009) 9:581–93. 10.1038/nri2567 [DOI] [PubMed] [Google Scholar]
- 19. Shuchun W, Lei P, Jiajia Y, Huaiming S, Duochen J, Xuan L, et al. Exosomal Transfer of miR-15b-3p Enhances Tumorigenesis and Malignant Transformation Through the DYNLT1/Caspase-3/Caspase-9 Signaling Pathway in Gastric Cancer. J Exp Clin Cancer Res (2020) 39:32. 10.1186/s13046-019-1511-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cao S, Lin L, Xia X, Wu H. Lncrna SPRY4-IT1 Regulates Cell Proliferation and Migration by Sponging miR-101-3p and Regulating Ampk Expression in Gastric Cancer. Mol Ther Nucleic Acids (2019) 17:455–64. 10.1016/j.omtn.2019.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 21. Wang M, Zhao C, Shi H, Zhang B, Zhang L, Zhang X, et al. Deregulated microRNAs in Gastric Cancer Tissue-Derived Mesenchymal Stem Cells: Novel Biomarkers and a Mechanism for Gastric Cancer. Br J Cancer (2014) 110:1199–210. 10.1038/bjc.2014.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yoon JH, Ham IH, Kim O, Ashktorab H, Smoot DT, Nam SW, et al. Gastrokine 1 Protein is a Potential Theragnostic Target for Gastric Cancer. Gastri Cancer (2018) 21:956–67. 10.1007/s10120-018-0828-8 [DOI] [PubMed] [Google Scholar]
- 23. Liu X, Lu Y, Xu Y, Hou S, Huang J, Wang B, et al. Exosomal Transfer of miR-501 Confers Doxorubicin Resistance and Tumorigenesis Via Targeting of BLID in Gastric Cancer. Cancer Lett (2019) 459:122–34. 10.1016/j.canlet.2019.05.035 [DOI] [PubMed] [Google Scholar]
- 24. Wang J, Lv B, Su Y, Wang X, Bu J, Yao L. Exosome-Mediated Transfer of Lncrna HOTTIP Promotes Cisplatin Resistance in Gastric Cancer Cells by Regulating Hmga1/miR-218 Axis. Onco Targets Ther (2019) 12:11325–38. 10.2147/OTT.S231846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zheng P, Chen L, Yuan X, Luo Q, Liu Y, Xie G, et al. Exosomal Transfer of Tumor-Associated Macrophage-Derived miR-21 Confers Cisplatin Resistance in Gastric Cancer Cells. J Exp Clin Cancer Res (2017) 36:53. 10.1186/s13046-017-0528-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang M, Qiu R, Yu S, Xu X, Li G, Gu R, et al. Paclitaxel−Resistant Gastric Cancer MGC−803 Cells Promote Epithelial−to−Mesenchymal Transition and Chemoresistance in Paclitaxel−Sensitive Cells Via Exosomal Delivery of Mir−155−5p. Int J Oncol (2019) 54:326–38. 10.3892/ijo.2018.4601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jingyue S, Xiao W, Juanmin Z, Wei L, Daoming L, Hong X. TFAP2E Methylation Promotes 5−Fluorouracil Resistance Via Exosomal miR−106a−5p and miR−421 in Gastric Cancer MGC−803 Cells. Mol Med Rep (2019) 20:323–31. 10.3892/mmr.2019.10237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sahai E. Illuminating the Metastatic Process. Nat Rev Cancer (2007) 7:737–49. 10.1038/nrc2229 [DOI] [PubMed] [Google Scholar]
- 29. Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-Mesenchymal Transitions in Development and Disease. Cell (2009) 139:871–90. 10.1016/j.cell.2009.11.007 [DOI] [PubMed] [Google Scholar]
- 30. Syn N, Wang L, Sethi G, Thiery JP, Goh BC. Exosome-Mediated Metastasis: From Epithelial-Mesenchymal Transition to Escape From Immunosurveillance. Trends Pharmacol Sci (2016) 37:606–17. 10.1016/j.tips.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 31. Pan L, Liang W, Fu M, Huang ZH, Li X, Zhang W, et al. Exosomes-Mediated Transfer of Long Noncoding RNA ZFAS1 Promotes Gastric Cancer Progression. J Cancer Res Clin Oncol (2017) 143:991–1004. 10.1007/s00432-017-2361-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Piao HY, Guo S, Wang Y, Zhang J. Exosome-Transmitted Lncrna PCGEM1 Promotes Invasive and Metastasis in Gastric Cancer by Maintaining the Stability of SNAI1. Clin Transl Oncol (2021) 23:246–56. 10.1007/s12094-020-02412-9 [DOI] [PubMed] [Google Scholar]
- 33. Xing Z, Sen W, Haixiao W, Jiacheng C, Xiaoxu H, Zheng C, et al. Circular RNA circNRIP1 Acts as a microRNA-149-5p Sponge to Promote Gastric Cancer Progression Via the AKT1/mTOR Pathway. Mol Cancer (2019) 18:20. 10.1186/s12943-018-0935-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fu H, Yang H, Zhang X, Wang B, Mao J, Li X, et al. Exosomal TRIM3 is a Novel Marker and Therapy Target for Gastric Cancer. J Exp Clin Cancer Res (2018) 37:162. 10.1186/s13046-018-0825-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hu Y, Qi C, Liu X, Zhang C, Gao J, Wu Y, et al. Malignant Ascites-Derived Exosomes Promote Peritoneal Tumor Cell Dissemination and Reveal a Distinct miRNA Signature in Advanced Gastric Cancer. Cancer Lett (2019) 457:142–50. 10.1016/j.canlet.2019.04.034 [DOI] [PubMed] [Google Scholar]
- 36. Yang H, Fu H, Wang B, Zhang X, Mao J, Li X, et al. Exosomal miR-423-5p Targets SUFU to Promote Cancer Growth and Metastasis and Serves as a Novel Marker for Gastric Cancer. Mol Carcinog (2018) 57:1223–36. 10.1002/mc.22838 [DOI] [PubMed] [Google Scholar]
- 37. Li C, Liu DR, Li GG, Wang HH, Li XW, Zhang W, et al. CD97 Promotes Gastric Cancer Cell Proliferation and Invasion Through Exosome-Mediated MAPK Signaling Pathway. World J Gastroenterol (2015) 21:6215–28. 10.3748/wjg.v21.i20.6215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lu J, Wang YH, Yoon C, Huang XY, Xu Y, Xie JW, et al. Circular RNA circ-RanGAP1 Regulates VEGFA Expression by Targeting miR-877-3p to Facilitate Gastric Cancer Invasion and Metastasis. Cancer Lett (2020) 471:38–48. 10.1016/j.canlet.2019.11.038 [DOI] [PubMed] [Google Scholar]
- 39. Kersy O, Loewenstein S, Lubezky N, Sher O, Simon NB, Klausner JM, et al. Omental Tissue-Mediated Tumorigenesis of Gastric Cancer Peritoneal Metastases. Front Oncol (2019) 9:1267. 10.3389/fonc.2019.01267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Whiteside TL. Tumor-Derived Exosomes and Their Role in Cancer Progression. Adv Clin Chem (2016) 74:103–41. 10.1016/bs.acc.2015.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zheng X, Turkowski K, Mora J, Brüne B, Seeger W, Weigert A, et al. Redirecting Tumor-Associated Macrophages to Become Tumoricidal Effectors as a Novel Strategy for Cancer Therapy. Oncotarget (2017) 8:48436–52. 10.18632/oncotarget.17061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Qian BZ, Pollard JW. Macrophage Diversity Enhances Tumor Progression and Metastasis. Cell (2010) 141:39–51. 10.1016/j.cell.2010.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wu L, Zhang X, Zhang B, Shi H, Yuan X, Sun Y, et al. Exosomes Derived From Gastric Cancer Cells Activate NF-kappaB Pathway in Macrophages to Promote Cancer Progression. Tumor Biol (2016) 37:12169–80. 10.1007/s13277-016-5071-5 [DOI] [PubMed] [Google Scholar]
- 44. Wang F, Li B, Wei Y, Zhao Y, Wang L, Zhang P, et al. Tumor-Derived Exosomes Induce PD1(+) Macrophage Population in Human Gastric Cancer That Promotes Disease Progression. Oncogenesis (2018) 7:41. 10.1038/s41389-018-0049-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Che Y, Geng B, Xu Y, Miao X, Chen L, Mu X, et al. Helicobacter Pylori-Induced Exosomal MET Educates Tumour-Associated Macrophages to Promote Gastric Cancer Progression. J Cell Mol Med (2018) 22:5708–19. 10.1111/jcmm.13847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zheng P, Luo Q, Wang W, Li J, Wang T, Wang P, et al. Tumor-Associated Macrophages-Derived Exosomes Promote the Migration of Gastric Cancer Cells by Transfer of Functional Apolipoprotein E. Cell Death Dis (2018) 9:434. 10.1038/s41419-018-0465-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zheng PM, Gao HJ, Li JM, Zhang P, Li G. Effect of Exosome-Derived miR-223 From Macrophages on the Metastasis of Gastric Cancer Cells. Zhonghua Yi Xue Za Zhi (2020) 100:1750–5. 10.3760/cma.j.cn112137-20200425-01309 [DOI] [PubMed] [Google Scholar]
- 48. Umakoshi M, Takahashi S, Itoh G, Kuriyama S, Sasaki Y, Yanagihara K, et al. Macrophage-Mediated Transfer of Cancer-Derived Components to Stromal Cells Contributes to Establishment of a Pro-Tumor Microenvironment. Oncogene (2019) 38:2162–76. 10.1038/s41388-018-0564-x [DOI] [PubMed] [Google Scholar]
- 49. Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, et al. Polarization of Tumor-Associated Neutrophil Phenotype by TGF-beta: “N1” Versus “N2Tan” Cancer Cell (2009) 16:183–94. 10.1016/j.ccr.2009.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hurt B, Schulick R, Edil B, El Kasmi KC, Barnett C., Jr. Cancer-Promoting Mechanisms of Tumor-Associated Neutrophils. Am J Surg (2017) 214:938–44. 10.1016/j.amjsurg.2017.08.003 [DOI] [PubMed] [Google Scholar]
- 51. Wu L, Saxena S, Singh RK. Neutrophils in the Tumor Microenvironment. Adv Exp Med Biol (2020) 1224:1–20. 10.1007/978-3-030-35723-8_1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Houghton AM, Rzymkiewicz DM, Ji H, Gregory AD, Egea EE, Metz HE, et al. Neutrophil Elastase-Mediated Degradation of IRS-1 Accelerates Lung Tumor Growth. Nat Med (2010) 16:219–23. 10.1038/nm.2084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Antonio N, Bønnelykke-Behrndtz ML, Ward LC, Collin J, Christensen IJ, Steiniche T, et al. The Wound Inflammatory Response Exacerbates Growth of Pre-Neoplastic Cells and Progression To Cancer. EMBO J (2015) 34:2219–36. 10.15252/embj.201490147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kuang DM, Zhao Q, Wu Y, Peng C, Wang J, Xu Z, et al. Peritumoral Neutrophils Link Inflammatory Response to Disease Progression by Fostering Angiogenesis in Hepatocellular Carcinoma. J Hepatol (2011) 54:948–55. 10.1016/j.jhep.2010.08.041 [DOI] [PubMed] [Google Scholar]
- 55. Zhou SL, Zhou ZJ, Hu ZQ, Huang XW, Wang Z, Chen EB, et al. Tumor-Associated Neutrophils Recruit Macrophages and T-Regulatory Cells to Promote Progression of Hepatocellular Carcinoma and Resistance to Sorafenib. Gastroenterology (2016) 150:1646–58.e17. 10.1053/j.gastro.2016.02.040 [DOI] [PubMed] [Google Scholar]
- 56. Mishalian I, Bayuh R, Eruslanov E, Michaeli J, Levy L, Zolotarov L, et al. Neutrophils Recruit Regulatory T-cells Into Tumors Via Secretion of CCL17–a New Mechanism of Impaired Antitumor Immunity. Int J Cancer (2014) 135:1178–86. 10.1002/ijc.28770 [DOI] [PubMed] [Google Scholar]
- 57. Zhang X, Shi H, Yuan X, Jiang P, Qian H, Xu W. Tumor-Derived Exosomes Induce N2 Polarization of Neutrophils to Promote Gastric Cancer Cell Migration. Mol Cancer (2018) 17:146. 10.1186/s12943-018-0898-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hinata M, Kunita A, Abe H, Morishita Y, Sakuma K, Yamashita H, et al. Exosomes of Epstein-Barr Virus-Associated Gastric Carcinoma Suppress Dendritic Cell Maturation. Microorganisms (2020) 8:1776. 10.3390/microorganisms8111776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Qu JL, Qu XJ, Qu JL, Qu XJ, Zhao MF, Teng YE, et al. The Role of Cbl Family of Ubiquitin Ligases in Gastric Cancer Exosome-Induced Apoptosis of Jurkat T Cells. Acta Oncol (2009) 48:1173–80. 10.3109/02841860903032817 [DOI] [PubMed] [Google Scholar]
- 60. Fan Y, Che X, Qu J, Hou K, Wen T, Li Z, et al. Exosomal PD-L1 Retains Immunosuppressive Activity and is Associated With Gastric Cancer Prognosis. Ann Surg Oncol (2019) 26:3745–55. 10.1245/s10434-019-07431-7 [DOI] [PubMed] [Google Scholar]
- 61. Clever D, Roychoudhuri R, Constantinides MG, Askenase MH, Sukumar M, Klebanoff CA, et al. Oxygen Sensing by T Cells Establishes an Immunologically Tolerant Metastatic Niche. Cell (2016) 166:1117–31.e14. 10.1016/j.cell.2016.07.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Yen EY, Miaw SC, Yu JS, Lai IR. Exosomal TGF-β1 is Correlated With Lymphatic Metastasis of Gastric Cancers. Am J Cancer Res (2017) 7:2199–208. [PMC free article] [PubMed] [Google Scholar]
- 63. Liu F, Bu Z, Zhao F, Xiao D. Increased T-helper 17 Cell Differentiation Mediated by Exosome-Mediated microRNA-451 Redistribution in Gastric Cancer Infiltrated T Cells. Cancer Sci (2018) 109:65–73. 10.1111/cas.13429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Wang J, Huang F, Shi Y, Zhang Q, Xu S, Yao Y, et al. Rp11-323N12.5 Promotes the Malignancy and Immunosuppression of Human Gastric Cancer by Increasing YAP1 Transcription. Gastri Cancer (2021) 24:85–102. 10.1007/s10120-020-01099-9 [DOI] [PubMed] [Google Scholar]
- 65. Shen Y, Xue C, Li X, Ba L, Gu J, Sun Z, et al. Effects of Gastric Cancer Cell-Derived Exosomes on the Immune Regulation of Mesenchymal Stem Cells by the NF-kB Signaling Pathway. Stem Cells Dev (2019) 28:464–76. 10.1089/scd.2018.0125 [DOI] [PubMed] [Google Scholar]
- 66. Zhong H, Yang Y, Ma S, Xiu F, Cai Z, Zhao H, et al. Induction of a Tumour-Specific CTL Response by Exosomes Isolated From Heat-Treated Malignant Ascites of Gastric Cancer Patients. Int J Hyperther (2011) 27:604–11. 10.3109/02656736.2011.564598 [DOI] [PubMed] [Google Scholar]
- 67. Talmadge JE, Gabrilovich DI. History of Myeloid-Derived Suppressor Cells. Nat Rev Cancer (2013) 13:739–52. 10.1038/nrc3581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wang Y, Ding Y, Guo N, Wang S. Mdscs: Key Criminals of Tumor Pre-Metastatic Niche Formation. Front Immunol (2019) 10:172. 10.3389/fimmu.2019.00172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Motallebnezhad M, Jadidi-Niaragh F, Qamsari ES, Bagheri S, Gharibi T, Yousefi M. The Immunobiology of Myeloid-Derived Suppressor Cells in Cancer. Tumour Biol (2016) 37:1387–406. 10.1007/s13277-015-4477-9 [DOI] [PubMed] [Google Scholar]
- 70. Xiang X, Poliakov A, Liu C, Liu Y, Deng ZB, Wang J, et al. Induction of Myeloid-Derived Suppressor Cells by Tumor Exosomes. Int J Cancer (2009) 124:2621–33. 10.1002/ijc.24249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ren W, Zhang X, Li W, Feng Q, Feng H, Tong Y, et al. Exosomal miRNA-107 Induces Myeloid-Derived Suppressor Cell Expansion in Gastric Cancer. Cancer Manag Res (2019) 11:4023–40. 10.2147/CMAR.S198886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Guo Y, Ji X, Liu J, Fan D, Zhou Q, Chen C, et al. Effects of Exosomes on Pre-Metastatic Niche Formation in Tumors. Mol Cancer (2019) 18:39. 10.1186/s12943-019-0995-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Tao L, Huang G, Song H, Chen Y, Chen L. Cancer Associated Fibroblasts: An Essential Role in the Tumor Microenvironment. Oncol Lett (2017) 14:2611–20. 10.3892/ol.2017.6497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Micke P, Ostman A. Tumour-Stroma Interaction: Cancer-Associated Fibroblasts as Novel Targets in Anti-Cancer Therapy. Lung Cancer (2004) 45 Suppl 2:S163–75. 10.1016/j.lungcan.2004.07.977 [DOI] [PubMed] [Google Scholar]
- 75. Ma Z, Chen M, Yang X, Xu B, Song Z, Zhou B, et al. The Role of Cancer-associated Fibroblasts in Tumorigenesis of Gastric Cancer. Curr Pharm Des (2018) 24:3297–302. 10.2174/1381612824666180601094056 [DOI] [PubMed] [Google Scholar]
- 76. Wang J, Guan X, Zhang Y, Ge S, Zhang L, Li H, et al. Exosomal Mir-27a Derived From Gastric Cancer Cells Regulates the Transformation of Fibroblasts Into Cancer-Associated Fibroblasts. Cell Physiol Biochem (2018) 49:869–83. 10.1159/000493218 [DOI] [PubMed] [Google Scholar]
- 77. Gu J, Qian H, Shen L, Zhang X, Zhu W, Huang L, et al. Gastric Cancer Exosomes Trigger Differentiation of Umbilical Cord Derived Mesenchymal Stem Cells to Carcinoma-Associated Fibroblasts Through TGF-β/Smad Pathway. PloS One (2012) 7:e52465. 10.1371/journal.pone.0052465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ning X, Zhang H, Wang C, Song X. Exosomes Released by Gastric Cancer Cells Induce Transition of Pericytes Into Cancer-Associated Fibroblasts. Med Sci Monit (2018) 24:2350–9. 10.12659/msm.906641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Miki Y, Yashiro M, Okuno T, Kitayama K, Masuda G, Hirakawa K, et al. CD9-Positive Exosomes From Cancer-Associated Fibroblasts Stimulate the Migration Ability of Scirrhous-Type Gastric Cancer Cells. Br J Cancer (2018) 118:867–77. 10.1038/bjc.2017.487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Shi L, Wang Z, Geng X, Zhang Y, Xue Z. Exosomal miRNA-34 From Cancer-Associated Fibroblasts Inhibits Growth and Invasion of Gastric Cancer Cells In Vitro and In Vivo. Aging (Albany NY) (2020) 12:8549–64. 10.18632/aging.103157 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 81. Xu G, Zhang B, Ye J, Cao S, Shi J, Zhao Y, et al. Exosomal miRNA-139 in Cancer-Associated Fibroblasts Inhibits Gastric Cancer Progression by Repressing MMP11 Expression. Int J Biol Sci (2019) 15:2320–9. 10.7150/ijbs.33750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Roorda BD, ter Elst A, Kamps WA, de Bont ES. Bone Marrow-Derived Cells and Tumor Growth: Contribution of Bone Marrow-Derived Cells to Tumor Micro-Environments With Special Focus on Mesenchymal Stem Cells. Crit Rev Oncol Hematol (2009) 69:187–98. 10.1016/j.critrevonc.2008.06.004 [DOI] [PubMed] [Google Scholar]
- 83. Yang X, Hou J, Han Z, Wang Y, Hao C, Wei L, et al. One Cell, Multiple Roles: Contribution of Mesenchymal Stem Cells to Tumor Development in Tumor Microenvironment. Cell Biosci (2013) 3:5. 10.1186/2045-3701-3-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Gu H, Ji R, Zhang X, Wang M, Zhu W, Qian H, et al. Exosomes Derived From Human Mesenchymal Stem Cells Promote Gastric Cancer Cell Growth and Migration Via the Activation of the Akt Pathway. Mol Med Rep (2016) 14:3452–8. 10.3892/mmr.2016.5625 [DOI] [PubMed] [Google Scholar]
- 85. Qi J, Zhou Y, Jiao Z, Wang X, Zhao Y, Li Y, et al. Exosomes Derived From Human Bone Marrow Mesenchymal Stem Cells Promote Tumor Growth Through Hedgehog Signaling Pathway. Cell Physiol Biochem (2017) 42:2242–54. 10.1159/000479998 [DOI] [PubMed] [Google Scholar]
- 86. Zhu W, Huang L, Li Y, Zhang X, Gu J, Yan Y, et al. Exosomes Derived From Human Bone Marrow Mesenchymal Stem Cells Promote Tumor Growth In Vivo. Cancer Lett (2012) 315:28–37. 10.1016/j.canlet.2011.10.002 [DOI] [PubMed] [Google Scholar]
- 87. Mao J, Liang Z, Zhang B, Yang H, Li X, Fu H, et al. Ubr2 Enriched in P53 Deficient Mouse Bone Marrow Mesenchymal Stem Cell-Exosome Promoted Gastric Cancer Progression Via Wnt/β-Catenin Pathway. Stem Cells (2017) 35:2267–79. 10.1002/stem.2702 [DOI] [PubMed] [Google Scholar]
- 88. Ji R, Zhang B, Zhang X, Xue J, Yuan X, Yan Y, et al. Exosomes Derived From Human Mesenchymal Stem Cells Confer Drug Resistance in Gastric Cancer. Cell Cycle (2015) 14:2473–83. 10.1080/15384101.2015.1005530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Lu P, Takai K, Weaver VM, Werb Z. Extracellular Matrix Degradation and Remodeling in Development and Disease. Cold Spring Harb Perspect Biol (2011) 3:a005058. 10.1101/cshperspect.a005058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Mohan V, Das A, Sagi I. Emerging Roles of ECM Remodeling Processes in Cancer. Semin Cancer Biol (2020) 62:192–200. 10.1016/j.semcancer.2019.09.004 [DOI] [PubMed] [Google Scholar]
- 91. Łukaszewicz-Zając M, Szmitkowski M, Litman-Zawadzka A, Mroczko B. Matrix Metalloproteinases and Their Tissue Inhibitors in Comparison to Other Inflammatory Proteins in Gastric Cancer (Gc). Cancer Invest (2016) 34:305–12. 10.1080/07357907.2016.1197237 [DOI] [PubMed] [Google Scholar]
- 92. Mu W, Rana S, Zöller M. Host Matrix Modulation by Tumor Exosomes Promotes Motility and Invasiveness. Neoplasia (2013) 15:875–87. 10.1593/neo.13786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Dong Z, Sun X, Xu J, Han X, Xing Z, Wang D, et al. Serum Membrane Type 1-Matrix Metalloproteinase (Mt1-MMP) Mrna Protected by Exosomes as a Potential Biomarker for Gastric Cancer. Med Sci Monit (2019) 25:7770–83. 10.12659/MSM.918486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Grünwald B, Harant V, Schaten S, Frühschütz M, Spallek R, Höchst B, et al. Pancreatic Premalignant Lesions Secrete Tissue Inhibitor of Metalloproteinases-1, Which Activates Hepatic Stellate Cells Via CD63 Signaling to Create a Premetastatic Niche in the Liver. Gastroenterology (2016) 151:1011–24.e7. 10.1053/j.gastro.2016.07.043 [DOI] [PubMed] [Google Scholar]
- 95. Miki Y, Yashiro M, Okuno T, Kuroda K, Togano S, Hirakawa K, et al. Clinico-Pathological Significance of Exosome Marker CD63 Expression on Cancer Cells and Stromal Cells in Gastric Cancer. PloS One (2018) 13:e0202956. 10.1371/journal.pone.0202956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Chen KB, Chen J, Jin XL, Huang Y, Su QM, Chen L. Exosome-Mediated Peritoneal Dissemination in Gastric Cancer and its Clinical Applications. BioMed Rep (2018) 8:503–9. 10.3892/br.2018.1088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Yeung TL, Leung CS, Yip KP, Au Yeung CL, Wong ST, Mok SC. Cellular and Molecular Processes in Ovarian Cancer Metastasis. A Review in the Theme: Cell and Molecular Processes in Cancer Metastasis. Am J Physiol Cell Physiol (2015) 309:C444–56. 10.1152/ajpcell.00188.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Sandoval P, Jiménez-Heffernan JA, Rynne-Vidal Á, Pérez-Lozano ML, Gilsanz Á, Ruiz-Carpio V, et al. Carcinoma-Associated Fibroblasts Derive From Mesothelial Cells Via Mesothelial-to-Mesenchymal Transition in Peritoneal Metastasis. J Pathol (2013) 231:517–31. 10.1002/path.4281 [DOI] [PubMed] [Google Scholar]
- 99. Nakamura M, Ono YJ, Kanemura M, Tanaka T, Hayashi M, Terai Y, et al. Hepatocyte Growth Factor Secreted by Ovarian Cancer Cells Stimulates Peritoneal Implantation Via the Mesothelial-Mesenchymal Transition of the Peritoneum. Gynecol Oncol (2015) 139:345–54. 10.1016/j.ygyno.2015.08.010 [DOI] [PubMed] [Google Scholar]
- 100. Yáñez-Mó M, Lara-Pezzi E, Selgas R, Ramírez-Huesca M, Domínguez-Jiménez C, Jiménez-Heffernan JA, et al. Peritoneal Dialysis and Epithelial-to-Mesenchymal Transition of Mesothelial Cells. N Engl J Med (2003) 348:403–13. 10.1056/NEJMoa020809 [DOI] [PubMed] [Google Scholar]
- 101. Li Q, Li B, Li Q, Wei S, He Z, Huang X, et al. Exosomal miR-21-5p Derived From Gastric Cancer Promotes Peritoneal Metastasis Via Mesothelial-to-Mesenchymal Transition. Cell Death Dis (2018) 9:854. 10.1038/s41419-018-0928-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Arita T, Ichikawa D, Konishi H, Komatsu S, Shiozaki A, Ogino S, et al. Tumor Exosome-Mediated Promotion of Adhesion to Mesothelial Cells in Gastric Cancer Cells. Oncotarget (2016) 7:56855–63. 10.18632/oncotarget.10869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Deng G, Qu J, Zhang Y, Che X, Cheng Y, Fan Y, et al. Gastric Cancer-Derived Exosomes Promote Peritoneal Metastasis by Destroying the Mesothelial Barrier. FEBS Lett (2017) 591:2167–79. 10.1002/1873-3468.12722 [DOI] [PubMed] [Google Scholar]
- 104. Wei M, Yang T, Chen X, Wu Y, Deng X, He W, et al. Malignant Ascites-Derived Exosomes Promote Proliferation and Induce Carcinoma-Associated Fibroblasts Transition in Peritoneal Mesothelial Cells. Oncotarget (2017) 8:42262–71. 10.18632/oncotarget.15040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Aslan C, Maralbashi S, Salari F, Kahroba H, Sigaroodi F, Kazemi T, et al. Tumor-Derived Exosomes: Implication in Angiogenesis and Antiangiogenesis Cancer Therapy. J Cell Physiol (2019) 234:16885–903. 10.1002/jcp.28374 [DOI] [PubMed] [Google Scholar]
- 106. Tamura R, Tanaka T, Akasaki Y, Murayama Y, Yoshida K, Sasaki H. The Role of Vascular Endothelial Growth Factor in the Hypoxic and Immunosuppressive Tumor Microenvironment: Perspectives for Therapeutic Implications. Med Oncol (2019) 37:2. 10.1007/s12032-019-1329-2 [DOI] [PubMed] [Google Scholar]
- 107. Hegde PS, Wallin JJ, Mancao C. Predictive Markers of anti-VEGF and Emerging Role of Angiogenesis Inhibitors as Immunotherapeutics. Semin Cancer Biol (2018) 52:117–24. 10.1016/j.semcancer.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 108. Yang H, Zhang H, Ge S, Ning T, Bai M, Li J, et al. Exosome-Derived Mir-130a Activates Angiogenesis in Gastric Cancer by Targeting C-MYB in Vascular Endothelial Cells. Mol Ther (2018) 26:2466–75. 10.1016/j.ymthe.2018.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 109. Bai M, Li J, Yang H, Zhang H, Zhou Z, Deng T, et al. Mir-135b Delivered by Gastric Tumor Exosomes Inhibits FOXO1 Expression in Endothelial Cells and Promotes Angiogenesis. Mol Ther (2019) 27:1772–83. 10.1016/j.ymthe.2019.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 110. Zhou Z, Zhang H, Deng T, Ning T, Liu R, Liu D, et al. Exosomes Carrying Microrna-155 Target Forkhead Box O3 of Endothelial Cells and Promote Angiogenesis in Gastric Cancer. Mol Ther Oncol (2019) 15:223–33. 10.1016/j.omto.2019.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 111. Deng T, Zhang H, Yang H, Wang H, Bai M, Sun W, et al. Exosome Mir-155 Derived From Gastric Carcinoma Promotes Angiogenesis by Targeting the C-MYB/VEGF Axis of Endothelial Cells. Mol Ther Nucleic Acids (2020) 19:1449–59. 10.1016/j.omtn.2020.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 112. Du J, Liang Y, Li J, Zhao JM, Wang ZN, Lin XY. Gastric Cancer Cell-Derived Exosomal Microrna-23a Promotes Angiogenesis by Targeting Pten. Front Oncol (2020) 10:326. 10.3389/fonc.2020.00326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Anami K, Oue N, Noguchi T, Sakamoto N, Sentani K, Hayashi T, et al. TSPAN8, Identified by Escherichia Coli Ampicillin Secretion Trap, is Associated With Cell Growth and Invasion in Gastric Cancer. Gastri Cancer (2016) 19:370–80. 10.1007/s10120-015-0478-z [DOI] [PubMed] [Google Scholar]
- 114. Xue X, Huang J, Yu K, Chen X, He Y, Qi D, et al. YB-1 Transferred by Gastric Cancer Exosomes Promotes Angiogenesis Via Enhancing the Expression of Angiogenic Factors in Vascular Endothelial Cells. BMC Cancer (2020) 20:996. 10.1186/s12885-020-07509-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Li G, Lin H, Tian R, Zhao P, Huang Y, Pang X, et al. Vegfr-2 Inhibitor Apatinib Hinders Endothelial Cells Progression Triggered by Irradiated Gastric Cancer Cells-Derived Exosomes. J Cancer (2018) 9:4049–57. 10.7150/jca.25370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Peinado H, Zhang H, Matei IR, Costa-Silva B, Hoshino A, Rodrigues G, et al. Pre-Metastatic Niches: Organ-Specific Homes for Metastases. Nat Rev Cancer (2017) 17:302–17. 10.1038/nrc.2017.6 [DOI] [PubMed] [Google Scholar]
- 117. Hoshino A, Costa-Silva B, Shen TL, Rodrigues G, Hashimoto A, Tesic Mark M, et al. Tumour Exosome Integrins Determine Organotropic Metastasis. Nature (2015) 527:329–35. 10.1038/nature15756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Zhang H, Deng T, Liu R, Bai M, Zhou L, Wang X, et al. Exosome-Delivered EGFR Regulates Liver Microenvironment to Promote Gastric Cancer Liver Metastasis. Nat Commun (2017) 8:15016. 10.1038/ncomms15016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Liu D, Li C, Trojanowicz B, Li X, Shi D, Zhan C, et al. CD97 Promotion of Gastric Carcinoma Lymphatic Metastasis is Exosome Dependent. Gastri Cancer (2016) 19:754–66. 10.1007/s10120-015-0523-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Tanaka M, Kuriyama S, Itoh G, Maeda D, Goto A, Tamiya Y, et al. Mesothelial Cells Create a Novel Tissue Niche That Facilitates Gastric Cancer Invasion. Cancer Res (2017) 77:684–95. 10.1158/0008-5472.CAN-16-0964 [DOI] [PubMed] [Google Scholar]
- 121. Zhang Y, Han T, Feng D, Li J, Wu M, Peng X, et al. Screening of non-Invasive miRNA Biomarker Candidates for Metastasis of Gastric Cancer by Small RNA Sequencing of Plasma Exosomes. Carcinogenesis (2020) 41:582–90. 10.1093/carcin/bgz186 [DOI] [PubMed] [Google Scholar]
- 122. Wang J, Liu Y, Sun W, Zhang Q, Gu T, Li G. Plasma Exosomes as Novel Biomarker for the Early Diagnosis of Gastric Cancer. Cancer Biomark (2018) 21:805–12. 10.3233/CBM-170738 [DOI] [PubMed] [Google Scholar]
- 123. Tang S, Cheng J, Yao Y, Lou C, Wang L, Huang X, et al. Combination of Four Serum Exosomal MiRNAs as Novel Diagnostic Biomarkers for Early-Stage Gastric Cancer. Front Genet (2020) 11:237. 10.3389/fgene.2020.00237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Ding XQ, Wang ZY, Xia D, Wang RX, Pan XR, Tong JH. Proteomic Profiling of Serum Exosomes From Patients With Metastatic Gastric Cancer. Front Oncol (2020) 10:1113. 10.3389/fonc.2020.01113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Tokuhisa M, Ichikawa Y, Kosaka N, Ochiya T, Yashiro M, Hirakawa K, et al. Exosomal miRNAs From Peritoneum Lavage Fluid as Potential Prognostic Biomarkers of Peritoneal Metastasis in Gastric Cancer. PLoS One (2015) 10:e0130472. 10.1371/journal.pone.0130472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Kim OY, Lee J, Gho YS. Extracellular Vesicle Mimetics: Novel Alternatives to Extracellular Vesicle-Based Theranostics, Drug Delivery, and Vaccines. Semin Cell Dev Biol (2017) 67:74–82. 10.1016/j.semcdb.2016.12.001 [DOI] [PubMed] [Google Scholar]
- 127. Tan A, De La Peña H, Seifalian AM. The Application of Exosomes as a Nanoscale Cancer Vaccine. Int J Nanomed (2010) 5:889–900. 10.2147/IJN.S13402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Zhang H, Wang Y, Bai M, Wang J, Zhu K, Liu R, et al. Exosomes Serve as Nanoparticles to Suppress Tumor Growth and Angiogenesis in Gastric Cancer by Delivering Hepatocyte Growth Factor Sirna. Cancer Sci (2018) 109:629–41. 10.1111/cas.13488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Jiang K, Dong C, Yin Z, Li R, Wang Q, Wang L. The Critical Role of Exosomes in Tumor Biology. J Cell Biochem (2019) 120:6820–32. 10.1002/jcb.27813 [DOI] [PubMed] [Google Scholar]
- 130. He M, Crow J, Roth M, Zeng Y, Godwin AK. Integrated Immunoisolation and Protein Analysis of Circulating Exosomes Using Microfluidic Technology. Lab Chip (2014) 14:3773–80. 10.1039/c4lc00662c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Zhu L, Wang K, Cui J, Liu H, Bu X, Ma H, et al. Label-Free Quantitative Detection of Tumor-Derived Exosomes Through Surface Plasmon Resonance Imaging. Anal Chem (2014) 86:8857–64. 10.1021/ac5023056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Mathai RA, Vidya R, Reddy BS, Thomas L, Udupa K, Kolesar J, et al. Potential Utility of Liquid Biopsy as a Diagnostic and Prognostic Tool for the Assessment of Solid Tumors: Implications in the Precision Oncology. J Clin Med (2019) 8:373. 10.3390/jcm8030373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Wu D, Yan J, Shen X, Sun Y, Thulin M, Cai Y, et al. Profiling Surface Proteins on Individual Exosomes Using a Proximity Barcoding Assay. Nat Commun (2019) 10:3854. 10.1038/s41467-019-11486-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Zhang Y, Bi J, Huang J, Tang Y, Du S, Li P. Exosome: A Review of Its Classification, Isolation Techniques, Storage, Diagnostic and Targeted Therapy Applications. Int J Nanomed (2020) 15:6917–34. 10.2147/IJN.S264498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Bandari SK, Purushothaman A, Ramani VC, Brinkley GJ, Chandrashekar DS, Varambally S, et al. Chemotherapy Induces Secretion of Exosomes Loaded With Heparanase That Degrades Extracellular Matrix and Impacts Tumor and Host Cell Behavior. Matrix Biol (2018) 65:104–18. 10.1016/j.matbio.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Sinha S, Hoshino D, Hong NH, Kirkbride KC, Grega-Larson NE, Seiki M, et al. Cortactin Promotes Exosome Secretion by Controlling Branched Actin Dynamics. J Cell Biol (2016) 214:197–213. 10.1083/jcb.201601025 [DOI] [PMC free article] [PubMed] [Google Scholar]