Abstract
Background
The authors performed total hip arthroplasty (THA) using a novel hemispherical dual-mobility (DM) acetabular cup without a protrusive cylindro-spherical rim, intended to reduce risks of iliopsoas impingement without requiring changes to conventional intraoperative positioning as with unipolar cups. We aim to determine clinical scores and rates of dislocations, complications, and revisions of this hemispherical DM cup, with the hypothesis that this novel design would result in clinical scores and dislocation rates comparable to other contemporary DM cups with protrusive cylindro-spherical rims.
Methods
We assessed 332 consecutive uncemented THAs performed using a hemispherical DM cup, at a minimum 2-year follow-up, using modified Harris Hip Score (mHHS) and Oxford Hip Score (OHS), and noting complications and revisions. Regression analyses were conducted to determine if mHHS and OHS depended on any independent factors.
Results
At 2.8 ± 0.5 years (range, 2–5), 2 patients (0.6%) had stem and cup revisions, 3 patients (1%) had isolated stem revisions, 13 patients (4%) died, and none were lost to follow-up. No dislocations occurred. For the final cohort of 305 patients (314 hips) with their original implants in place, mHHS was 92 ± 12 (range, 46–100), and OHS was 57 ± 5 (range, 34–60). Multivariable analyses revealed that mHHS and OHS decreased significantly with age (β = -0.35, P < .001, and β = -0.15, P < .001, respectively).
Conclusions
With no dislocations and satisfactory clinical scores, this sizable cohort confirms that the novel hemispherical DM cup studied is effective at preventing dislocations, although longer-term follow-up remains necessary to ascertain the longevity of clinical outcomes and radiographic stability.
Level of Evidence
Level IV, multicentric retrospective case series.
Keywords: Clinical outcome, Dual-mobility cup, Uncemented THA, Dislocations, Survival, Revision
Introduction
Dislocation is a feared and burdensome complication after total hip arthroplasty (THA), reported in up to 7% of primary THAs [1,2]. Over the past decade, dual-mobility (DM) cups demonstrated their efficacy at reducing subluxations and dislocations, as they have greater “jump distance” and higher ratios of head-to-neck diameters [3]. While the original “Bousquet” cup was susceptible to intraprosthetic dislocations and aseptic loosening [2], design enhancements such as tighter press-fit and bioactive coatings, together with more wear-resistant ultra-high-molecular-weight polyethylene liners, helped overcome most of these shortcomings [3].
Contemporary DM cups have proved effective at preventing intraprosthetic dislocation and demonstrated low rates of complications and revisions [3,4]. DM cups were originally designed to prevent dislocations in elderly patients or those with femoral neck fractures [3,5,6] but are increasingly implanted for a broader range of indications [3,7]. Ilio-psoas impingement remains a matter of concern with DM cups because they are more likely to overhang at the anterior margin of the acetabulum, as their design features a protrusive cylindro-spherical rim to increase the jump distance [8].
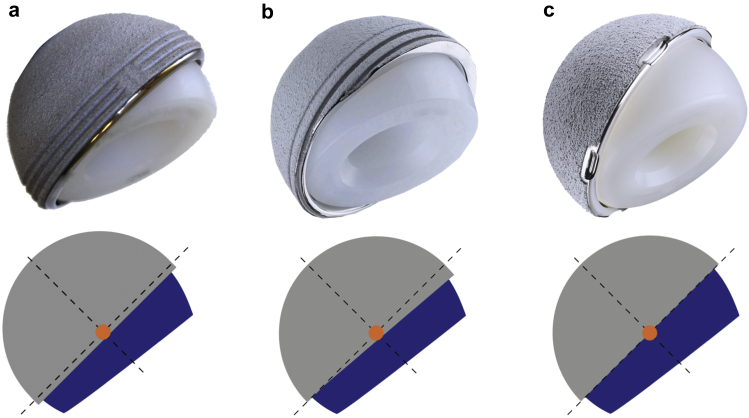
Since 2014, the authors have been using a novel hemispherical DM cup that does not feature a protrusive cylindro-spherical rim (Fig. 1), intended to reduce risks of iliopsoas impingement without requiring changes to conventional intraoperative positioning as with unipolar cups. The purpose of the present study was to determine the rates of dislocations, complications, and revisions, as well as clinical scores of this hemispherical DM cup at a minimum follow-up of 2 years. The hypothesis was that this novel design would result in dislocation rates and clinical scores comparable to those in the recent literature on other contemporary DM cups with protrusive cylindro-spherical rims.
Figure 1.
(a) Original dual-mobility (DM) cup design with a complete cylindro-spherical rim, (b) second generation DM cup with a partial cylindro-spherical rim, and (c) the Symbol hemispherical DM cup without a cylindro-spherical rim.
Material and methods
The authors evaluated a consecutive series of 332 primary THAs (323 patients) performed over 2 consecutive years by 3 surgeons (L.S., G.E., and F.C.) using the same uncemented hemispherical DM cup (Symbol cup DM HA; Dedienne Santé, Mauguio, France). Throughout the inclusion period, the surgeons used this hemispherical DM cup routinely for all primary THAs, without specific inclusion or exclusion criteria (all ages, indications, activity levels, spino-pelvic orientations). Four femoral stem models were used: Hype (Serf, Décines, France), Libra (Serf, Décines, France), Integrale (Amplitude, Valence, France), and Symbol (Dedienne Santé, Mauguio, France); all 4 are straight, titanium-alloy, hydroxyapatite-coated stems, although the first 3 are Corail-like stems (characterized by their long, double-taper geometry to maximize stereo-stability), while the Symbol stem is shorter and metaphyseal-engaging.
The cohort comprised 147 men (147 hips) and 185 women (194 hips), aged 72.3 ± 9.8 years (range, 45–96) and with body mass index of 26.5 ± 4.5 (range, 17–50). The etiology was primary osteoarthritis for 298 hips (90%), avascular necrosis for 17 hips (5%), femoral neck fracture for 12 hips (4%), osteoarthritis secondary to congenital hip dysplasia for 3 hips (1%), posttraumatic osteoarthritis for one hip (0.3%), and rheumatoid arthritis for one hip (0.3%) (Table 1).
Table 1.
Preoperative demographics and morphological data.
| Variable | Original cohort (n = 332 hips) |
|
|---|---|---|
| Mean ± SD |
Range |
|
| N (%) | ||
| Age | 72.3 ± 9.8 | (45-96) |
| BMI | 26.5 ± 4.5 | (17-50) |
| Male gender | 147 (44%) | |
| Etiology | ||
| Primary OA | 298 (90%) | |
| Avascular necrosis | 17 (5%) | |
| Femoral neck fracture | 12 (4%) | |
| Dysplasia | 3 (1%) | |
| Posttraumatic OA | 1 (0%) | |
| RA | 1 (0%) | |
BMI, body mass index; SD, standard deviation; OA, osteoarthritis; RA, rheumatoid arthritis.
The procedures were performed through a posterolateral approach using the same technique for acetabular reaming and cup positioning for all 332 hips (Table 2). The acetabulum was prepared first by removing osteophytes to visualize the acetabular contour, true floor, and transverse acetabular ligament. Then the acetabulum was reamed progressively to expose bleeding subchondral bone and obtain adequate stability of the reamer. A line-to-line trial cup was then inserted to verify primary stability, and the final cup was impacted while adjusting its anteversion to the transverse acetabular ligament [9] and inclination to the acetabular contour (within the range 35°–45°). The smallest possible cup size was used, ensuring no protrusion beyond the anterior acetabular horn to minimize prosthetic overhang.
Table 2.
Intraoperative data.
| Variable | Original cohort (n = 332 hips) |
|---|---|
| N (%) | |
| Surgical approach | |
| Posterolateral | 332 (100) |
| Head diameter | |
| 22 | 138 (42) |
| 28 | 194 (58) |
| Neck length | |
| Short | 119 (36) |
| Medium | 181 (55) |
| Long | 32 (10) |
| Cup diameter | |
| 44 | 6 (2) |
| 46 | 37 (11) |
| 48 | 68 (20) |
| 50 | 64 (19) |
| 52 | 58 (17) |
| 54 | 63 (19) |
| 56 | 25 (8) |
| 58 | 9 (3) |
| 60 | 2 (1) |
| Stem type | |
| Symbol | 135 (41) |
| Hype | 85 (26) |
| Libra | 78 (23) |
| Integrale | 34 (10) |
All patients were recalled for clinical evaluation at a minimum follow-up of 2 years using the modified Harris Hip Score (mHHS) [10] and the Oxford Hip Score (OHS) [11]. Their case notes were used to document implant materials, models, and diameters, as well as postoperative complications or revisions. If patients presented to the clinic with pain, further imaging was performed to inspect for fractures, prosthetic overhang, infection, loosening, and so on. All patients provided written informed consent for the use of their data and images for research and publishing purposes, which had been approved by 'GCS Ramsay Santé pour l’Enseignement et la Recherche' (IRB# COS-RGDS-2019—11-008BONIN-N).
Statistical analysis
The Shapiro-Wilk test was used to assess normality of distributions. Univariable and multivariable analyses were performed after identification of relevant variables (age at surgery, gender, body mass index, cup size, head diameter, head neck, and stem type) to determine their associations with mHHS and OHS. Statistical significance was considered for P values <.05. Statistical analyses were performed using R version 3.5.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
From the cohort of 323 patients (332 hips), there were 6 intraoperative complications, all related to the femoral stem: 4 femoral cracks (1%) treated with cerclage and 2 fractures of the greater trochanter (0.5%, in patients aged 81 and 85 years) treated with trochanteric plate.
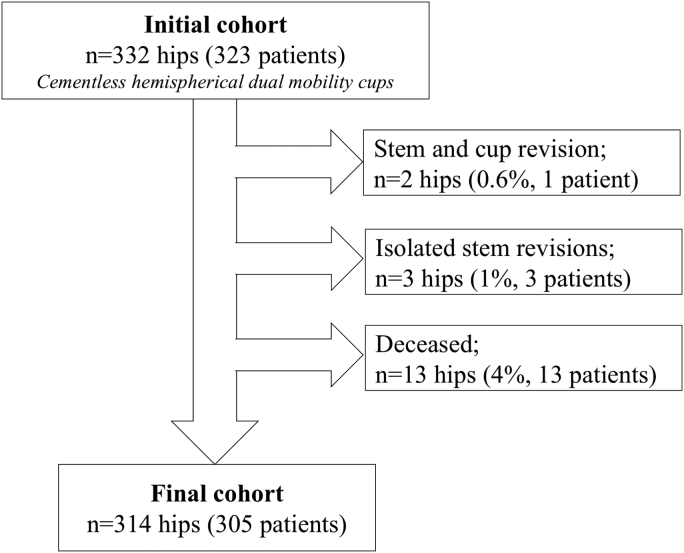
Furthermore, 2 patients (2 hips, 0.6%) had stem and cup revisions, 3 patients (1%) had isolated stem revisions, 13 patients (13 hips, 4%) died, and none were lost to follow-up (Fig. 2). There were no dislocations recorded throughout the follow-up period. The stem and cup revisions were both due to persistent hip pain: one because of excessive mediolateral global offset, and the other because of stem micro-motion with suspected sepsis (ruled out by implant retrieval analysis). The isolated stem revisions were due to traumatic periprosthetic femoral fracture in 2 hips, and, for limb length discrepancy >20 mm, gradual stem subsidence in one hip.
Figure 2.
Flowchart indicating initial cohort, revisions, and deaths.
There were 10 postoperative complications (3%) that did not need implant removal. Three (0.9%) were ilio-psoas impingements (treated by infiltration), one (0.3%) deep infection treated successfully by lavage and polyethylene (PE) liner exchange (patient died thereafter aged 89 years), and one (0.3%) was stem subsidence of >10 mm treated with corrective shoe insole. Five complications were treated conservatively: 2 (0.6%) periprosthetic femoral fractures due to trauma, one (0.3%) traumatic fascia lata tendinitis, one (0.3%) peritrochanteric bursitis, and one (0.3%) edema and blisters.
Clinical outcomes
For the final cohort of 305 patients (314 hips) living with their original cups and stems, evaluated at 2.8 ± 0.5 years (range, 2-5), the mHHS was 92 ± 12 (range, 46–100), and the OHS was 57 ± 5 (range, 34–60). Multivariable analyses revealed that both mHHS and OHS decreased significantly with age (β = −0.35, P < .001, and β = −0.15, P < .001, respectively), while only mHHS increased with cup diameter (β = 1.25, P = .037) (Table 3, Table 4).
Table 3.
Univariable and multivariable regression analysis of modified Harris Hip Score.
| Variable | Univariable |
Multivariable (n = 304) |
||||
|---|---|---|---|---|---|---|
| β | 95% C.I. | P value | β | 95% C.I. | P value | |
| Age at index operation (y) | −0.37 | (−0.51 to −0.24) | <.001 | −0.35 | (−0.50 to −0.21) | <.001 |
| BMI | 0.07 | (−0.24 to 0.39) | .658 | −0.12 | (−0.43 to 0.19) | .448 |
| Male sex | 3.20 | (0.43 to 5.96) | .023 | −1.63 | (−5.35 to 2.09) | .389 |
| Head diameter | ||||||
| 22 | REF | |||||
| 28 | 1.78 | (−1.00 to 4.57) | .209 | −1.50 | (−4.60 to 1.61) | .344 |
| Neck length | ||||||
| Short | −2.72 | (−5.55 to 0.11) | .060 | −2.18 | (−5.13 to 0.76) | .146 |
| Medium | REF | |||||
| Long | 2.19 | (−2.42 to 6.81) | .351 | 3.48 | (−1.23 to 8.18) | .147 |
| Cup diameter (mm) | 1.27 | (0.46 to 2.07) | .002 | 1.25 | (0.08 to 2.41) | .037 |
BMI, body mass index; C.I., confidence interval.
Bold values present statistically significant differences.
Table 4.
Univariable and multivariable regression analysis of Oxford Hip Score.
| Variable | Univariable |
Multivariable (n = 304) |
||||
|---|---|---|---|---|---|---|
| β | 95% C.I. | P value | β | 95% C.I. | P value | |
| Age at index operation (y) | −0.16 | (−0.21 to 0.10) | <.001 | −0.15 | (−0.21 to −0.09) | <.001 |
| BMI | 0.03 | (−0.10 to 0.16) | .663 | −0.05 | (−0.18 to 0.08) | .446 |
| Male sex | 1.46 | (−0.35– 2.58) | .010 | −0.26 | (−1.78 to 1.27) | .741 |
| Head diameter | ||||||
| 22 | REF | |||||
| 28 | 0.68 | (−0.45 to 1.81) | .238 | −0.61 | (−1.88 to 0.66) | .343 |
| Neck length | ||||||
| Short | −1.21 | (−2.40 to 0.03) | .045 | −0.84 | (−2.05 to 0.36) | .169 |
| Medium | REF | |||||
| Long | 2.14 | (−0.48 to 3.27) | .031 | 1.60 | (−0.33 to 3.52) | .104 |
| Cup diameter (mm) | 0.48 | (0.15 to 0.81) | .004 | 0.39 | (0.09 to 0.86) | .113 |
BMI, body mass index; C.I., confidence interval.
Bold values present statistically significant differences.
Discussion
DM cups have gained considerable popularity recently as they grant adequate range of motion while preventing instabilities [1,2]. With no dislocations and satisfactory short-term clinical scores, this sizable cohort confirms that the novel hemispherical DM cup studied is effective at preventing dislocations, although longer term follow-up remains necessary to ascertain the longevity of clinical outcomes and radiographic stability [2,4,6].
This study suggests that hemispherical DM cups could be as effective at preventing dislocations as other contemporary DM cups with protrusive cylindro-spherical rims [1,3,12]. Furthermore, the short-term data regarding the absence of intraprosthetic instabilities at either the liner-cup junction or at the liner-head junction indicate that both 22-mm and 28-mm heads are compatible with this cup design. Nevertheless, the benefits of large femoral heads remain uncertain because they may reduce dislocation rates on one hand but may increase PE wear on the other hand [13,14]. Using large femoral heads (28 mm) could lead to more wear debris and subsequent osteolysis, while using smaller femoral heads (22 mm) could result in intraprosthetic dislocation due to the reduced neck-to-head ratio that leads to earlier impingement between the neck and the retentive portion of the PE liner.
This study demonstrated satisfactory clinical outcomes of uncemented THA using a novel hemispherical DM acetabular cup without a protrusive cylindro-spherical rim, with a cup cumulative revision rate of 0.6%, and a global cumulative revision rate of 1.5%, at a mean follow-up of 2.8 years. While the global cumulative revision rate may seem high at such short follow-up, it is worth noting that some revisions were due to traumatic periprosthetic fractures and that the rate remains within the range reported for other contemporary DM acetabular cups [4,6,7]. Numerous smaller series (<100 hips) had no revisions of any kind at 5 to 10 years of follow-up, but larger cohorts (>150 hips) had overall revision rates between 0.5% and 3.6%, at 5 to 13 years of follow-up.
For this series, the mean mHHS and OHS at 2 to 5 years were 92 and 57 points, respectively, which remain favorable when compared with scores reported for contemporary DM cups [2]. Our multivariable regressions revealed significant associations between age and both mHHS and OHS, which is expected, as function declines in elderly patients. Thus, in the hypothetical case of 2 patients with equal preoperative status but an age difference of 10 years, the expected difference in mHHS and OHS between the 2 patients would be 3.5 points and 1.5 points, respectively.
According to recent literature, sepsis is a common reason for revision of DM cups, and this could be a result of the frailty and comorbidities of the elder population in which they are usually implanted [1,7,15]. The present study recorded no revisions due to infection at 2.8-year follow-up, thus comparing favourably to that reported in the Danish Hip Registry for all THA infections (1.0% at 5 years) [16].
In this study, iliopsoas impingement was diagnosed clinically if a patient exhibited anterior groin pain. Radiographs were then performed in these patients to exclude other causes of pain, and if no other causes of pain were seen, computed tomography scans were performed to quantify cup overhang and anteversion. Psoas impingement due to excessive overhang and inadequate anteversion was found in 3 hips (0.9%), despite the use of hemispherical DM cups, likely due to insufficient cup anteversion or oversizing. Vandenbussche et al. [8] had in fact warned that prosthetic overhang is more likely to occur with DM cups because they have more protrusive rims. Nonetheless, the incidence of ilio-psoas impingement in the present series was considerably lower than rates reported in earlier series (4.3%) [17] as well as recent series of unipolar cups (3.9%) [18].
The limitations of this study include its retrospective design and the lack of radiographic assessment. Moreover, the study is not comparative and did not investigate whether DM cups have relative functional or cost benefits as compared with unipolar cups. Finally, the minimum follow-up duration of 2 years does not enable robust survival analysis but is sufficiently long to detect common cup-related early complications such as instability, dislocation, or ilio-psoas impingement. The main strength of this study is its sample size of 332 hips, which includes patients that are prone to hip instability, for a hemispherical DM cup. Although 4 stem types were used, the same DM cup was implanted in all patients.
Conclusions
With no dislocations and satisfactory clinical scores, this sizable cohort confirms that the novel hemispherical DM cup studied is effective at preventing dislocations, although longer term follow-up remains necessary to ascertain the longevity of clinical outcomes and radiographic stability.
Conflicts of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: L. Schneider receives royalties from Dedienne Santé (France). F. Châtain receives royalties from Dedienne Santé (France). G. Estour receives royalties from Dedienne Santé (France). N. Bonin receives royalties from Dedienne Santé (France) and ConMed (USA); is a paid consultant for Stryker (USA); and is a board member of The International Society of Hip Arthroscopy and is a committee member of the European Society of Sports Traumtology, Knee Surgery and Arthroscopy.
Acknowledgment
The authors are grateful to 'GCS Ramsay Santé pour l’Enseignement et la Recherche' for funding the statistical analysis and manuscript preparation for this study.
Appendix A. Supplementary data
References
- 1.Jonker R.C., van Beers L., van der Wal B.C.H. Can dual mobility cups prevent dislocation without increasing revision rates in primary total hip arthroplasty? A systematic review. Orthop Traumatol Surg Res. 2020;106(3):509. doi: 10.1016/j.otsr.2019.12.019. [DOI] [PubMed] [Google Scholar]
- 2.Reina N., Pareek A., Krych A.J., Pagnano M.W., Berry D.J., Abdel M.P. Dual-mobility constructs in primary and revision total hip arthroplasty: a systematic review of comparative studies. J Arthroplasty. 2019;34(3):594. doi: 10.1016/j.arth.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 3.Batailler C., Fary C., Verdier R., Aslanian T., Caton J., Lustig S. The evolution of outcomes and indications for the dual-mobility cup: a systematic review. Int Orthop. 2017;41(3):645. doi: 10.1007/s00264-016-3377-y. [DOI] [PubMed] [Google Scholar]
- 4.Darrith B., Courtney P.M., Della Valle C.J. Outcomes of dual mobility components in total hip arthroplasty: a systematic review of the literature. Bone Joint J. 2018;100-b(1):11. doi: 10.1302/0301-620X.100B1.BJJ-2017-0462.R1. [DOI] [PubMed] [Google Scholar]
- 5.Kunutsor S.K., Barrett M.C., Beswick A.D. Risk factors for dislocation after primary total hip replacement: a systematic review and meta-analysis of 125 studies involving approximately five million hip replacements. Lancet Rheumatol. 2019;1(2):e111. doi: 10.1016/S2665-9913(19)30045-1. [DOI] [PubMed] [Google Scholar]
- 6.Plummer D.R., Haughom B.D., Della Valle C.J. Dual mobility in total hip arthroplasty. Orthop Clin North Am. 2014;45(1):1. doi: 10.1016/j.ocl.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Chouteau J., Rollier J.C., Bonnin M.P. Absence of instabilities and intra-prosthetic dislocations at 7 to 11 years following THA using a fourth-generation cementless dual mobility acetabular cup. J Exp Orthop. 2020;7(1):51. doi: 10.1186/s40634-020-00265-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vandenbussche E., Saffarini M., Delogé N., Moctezuma J.L., Nogler M. Hemispheric cups do not reproduce acetabular rim morphology. Acta Orthop. 2007;78(3):327. doi: 10.1080/174536707100013870. [DOI] [PubMed] [Google Scholar]
- 9.Archbold H.A., Mockford B., Molloy D., McConway J., Ogonda L., Beverland D. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement: a preliminary study of 1000 cases investigating postoperative stability. J Bone Joint Surg Br. 2006;88(7):883. doi: 10.1302/0301-620X.88B7.17577. [DOI] [PubMed] [Google Scholar]
- 10.Byrd J.W., Jones K.S. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16(6):578. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 11.Delaunay C., Epinette J.A., Dawson J., Murray D., Jolles B.M. Cross-cultural adaptations of the Oxford-12 HIP score to the French speaking population. Orthop Traumatol Surg Res. 2009;95(2):89. doi: 10.1016/j.otsr.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Romagnoli M., Grassi A., Costa G.G., Lazaro L.E., Lo Presti M., Zaffagnini S. The efficacy of dual-mobility cup in preventing dislocation after total hip arthroplasty: a systematic review and meta-analysis of comparative studies. Int Orthop. 2019;43(5):1071. doi: 10.1007/s00264-018-4062-0. [DOI] [PubMed] [Google Scholar]
- 13.Leclercq S., Benoit J.Y., de Rosa J.P., Tallier E., Leteurtre C., Girardin P.H. Evora® chromium-cobalt dual mobility socket: results at a minimum 10 years' follow-up. Orthop Traumatol Surg Res. 2013;99(8):923. doi: 10.1016/j.otsr.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Bunn A., Colwell C.W., Jr., D'Lima D.D. Effect of head diameter on passive and active dynamic hip dislocation. J Orthop Res. 2014;32(11):1525. doi: 10.1002/jor.22659. [DOI] [PubMed] [Google Scholar]
- 15.Kreipke R., Rogmark C., Pedersen A.B. Dual mobility cups: effect on risk of revision of primary total hip arthroplasty due to osteoarthritis: a matched population-based study using the nordic arthroplasty register association database. J Bone Joint Surg Am. 2019;101(2):169. doi: 10.2106/JBJS.17.00841. [DOI] [PubMed] [Google Scholar]
- 16.Gundtoft P.H., Overgaard S., Schonheyder H.C., Moller J.K., Kjaersgaard-Andersen P., Pedersen A.B. The "true" incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties: a prospective cohort study. Acta Orthop. 2015;86(3):326. doi: 10.3109/17453674.2015.1011983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ala Eddine T., Remy F., Chantelot C., Giraud F., Migaud H., Duquennoy A. [Anterior iliopsoas impingement after total hip arthroplasty: diagnosis and conservative treatment in 9 cases] Rev Chir Orthop Reparatrice Appar Mot. 2001;87(8):815. [PubMed] [Google Scholar]
- 18.Ueno T., Kabata T., Kajino Y., Inoue D., Ohmori T., Tsuchiya H. Risk factors and cup protrusion thresholds for symptomatic iliopsoas impingement after total hip arthroplasty: a retrospective case-control study. J Arthroplasty. 2018;33(10):3288. doi: 10.1016/j.arth.2018.05.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.