Abstract
Pancreatic cancer (PC) is one of the deadliest malignancies. The high mortality rate of PC largely results from delayed diagnosis and early metastasis. Therefore, identifying novel treatment targets for patients with PC is urgently required to improve survival rates. A major barrier to successful treatment of PC is the presence of a hypoxic tumor microenvironment, which is associated with poor prognosis, treatment resistance, increased invasion and metastasis. Recent studies have identified a number of novel molecules and pathways in PC cells that promote cancer cells progression under hypoxic conditions, which may provide new therapy strategies to inhibit the development and metastasis of PC. This review summarizes the latest research of hypoxia in PC and provides an overview of how the current therapies have the capacity to overcome hypoxia and improve PC patient treatment. These findings will eventually provide guidance for future PC management and clinical trials and hopefully improve the survival of patients with PC.
Keywords: Pancreatic cancer, hypoxia, tumor microenvironment, novel strategies, survival
Introduction
Pancreatic cancer (PC) is one of the most aggressive and lethal malignancies, with a 5-year survival rate of 9% (1). Pancreatic ductal adenocarcinoma account for 90% of all PC types and is a prototype of a tumor with a pronounced inflammatory microenvironment, in which the majority of the tumor mass consists of nonneoplastic stromal and immune cells (2). The microenvironment of PC is composed of fibroblasts, extracellular matrix, and immune cells, which result in intense stromal desmoplasia and angiogenesis so as to enable invasion, metastasis and resistance to chemotherapy (3). PC is a hypo-vascular malignancy, and the pancreatic tumor microenvironment (TME) is hypoxic (4).
An imbalance between oxygen production and consumption culminates in a hypoxic TME, a unique characteristic of cancer, which plays vital roles in the development of tumors. Researchers have shown that hypoxia-inducible factor (HIF)-1α expression highly correlates to tumor progression and metastasis (5). HIF-1, a key regulator of the response to hypoxia, is overexpressed in PC. Previous studies have shown that cancer cells exhibit increased energetic demands compared with normal cells. Tumors alter their metabolism to adapt to the hypoxia conditions in the TME (6).
HIFs are transcription factors that play a critical role in the cellular response to hypoxia. The HIF-1α transcription factor directly binds to hypoxia-response elements (HREs) in gene promoters, and then activates its downstream target in order to make cells adapt to hypoxia. HIF-1 is a heterodimer composed of an α-subunit and β-subunit. The activity of HIF-1α is controlled by the cellular oxygen concentration; HIF-1α is constitutively degraded by the ubiquitin-proteasome pathway under normoxic conditions but stabilized under hypoxia conditions.
A major barrier to successful treatment of PC is the complex TME with hypoxia, because of rapid development and metastasis of PC. Hence, determining the molecular mechanisms underlying the relationship between metastasis and hypoxia is critical to develop novel strategies to improve PC patients’ outcome. Therefore, revealing the molecular mechanisms underlying PC progression and developing corresponding targeted therapies are essential to improving the outcome of patients with PC. This review summarizes the latest research of hypoxia in PC and provides an overview on the currently developed therapies as well as potential targets for new treatments for hypoxia in metastatic PC.
TME and hypoxia
PC is desmoplastic with highly mesenchymal-like substrates, which favours hypoxia, induces epithelial-to-mesenchymal transition (EMT) and results in tumor cell metastasis (7). PCs are surrounded by a dense fibrotic stroma containing dense masses, pancreatic stellate cells (PSCs) and an extracellular matrix. The stroma creates a hypoxic microenvironment, which plays a significant role in promoting the development of PC cells and inducing metastasis of tumor cells (8). For example, cancer cells adapt to hypoxia by altering the functions of mitochondria for optimal metabolism and energy supply. Low oxygen levels can induce reductive carboxylation in mitochondria and generate reactive oxygen species (ROS) in cancer cells, which induces rapid development of PC (9).
Energy metabolism and hypoxia
The hypoxic environment promotes energy production and mitochondrial biogenesis of PC cells to ensure tumor survival. Targeting mitochondrial energy metabolism has thus increasingly been regarded as a potential strategy for cancer treatment.
Mitochondrial biogenesis is modulated by various transcription factors such as peroxisome proliferator-activated receptor-gamma coactivator-1α (PGC-1α) and mitochondrial transcription factor A (TFAM). PGC-1α enhances TFAM gene expression by activating nuclear respiratory factor (NRF-1) (10). High-mobility group box-1 (HMGB1) is a DNA-binding protein that plays a significant role in protecting against mitochondrial abnormalities by modulating heat shock protein beta-1 (HSPB1) gene expression. In PC patients, low expression of HMGB1 was associated with poor survival (11,12). A recent study showed that HMGB1 serves as a vital mediator of mitochondrial biogenesis through the adenosine 5’-monophosphate-activated protein kinase (AMPK)/PGC-1α pathway in PC (13). HMGB1 upregulates the protein expression of PGC-1α and activates hypoxia-induced phosphorylation of AMPK. AMPK regulates mitochondrial biogenesis by increasing SIRT1 and inducing PGC-1 deacetylation. PGC-1α plays a critical role in cancer energy metabolism in PC by regulating mitochondrial biogenesis and antioxidants detoxification (14). Therefore, HMGB1 is a new modulator of mitochondrial biogenesis via the AMPK/SIRT1/PGC-1α pathway under hypoxia in PC.
PSCs
PSCs are one of the cell types in PC TME and exist in the non-activated and activated state. Activated PSCs show increased expressions of collagen-I and α-smooth muscle actin (α-SMA), which are important for cancer progression and metastasis. Activated PSCs also secrete interleukin (IL)-6, stromal cell-derived factor-1 and transforming growth factor-β, which are associated with tumor progression and metastasis (15). A study demonstrated that HIF-1α increases the secretion of C-C motif chemokine ligand 2 to recruit macrophages, accelerating the activation of PSCs (16). Hypoxia can induce PSCs to secrete IL-6, which in turn promotes the progression of PC through the JAK2/STAT3 and mitogen-activated protein kinase pathways (17,18). In addition, high expression of IL-6 has been related to poor prognosis in PC patients. A recent study showed that the anti-IL-6 antibody tocilizumab reduced tumor weight in an orthotopic model of human Colo357 cells by 2.4 fold compared with controls (19).
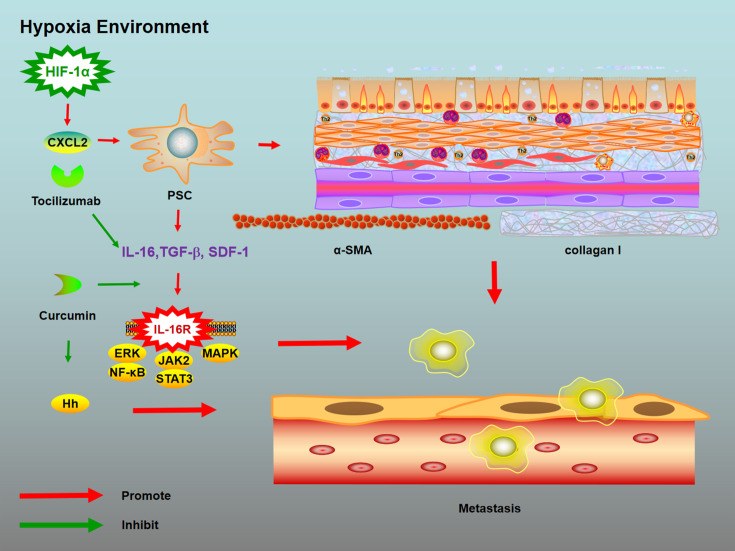
Curcumin (diferuloylmethane), a natural polyphenol derived from turmeric, exhibits significant antitumor effects by influencing a number of signalling pathways (20). Li et al. demonstrated that curcumin inhibits the tumor-stromal crosstalk by inhibiting the IL-6/ERK/NF-κB pathway, and activation of PSCs is inhibited by curcumin under hypoxic conditions (21). Moreover, curcumin has been reported to inhibit EMT and hypoxia-induced proliferation by suppressing Hedgehog (Hh) signalling in PC cells (22). A phase I/II study demonstrated that curcumin increased the median survival time of PC to 161 d vs. gemcitabine alone (70 d) (23). These findings show that curcumin suppresses PC progression by inhibiting the PSC/IL-6/ERK/NF-κB pathway under hypoxic conditions (Figure 1 ).
Figure 1.
Mechanisms of novel strategies targeting PSCs and hypoxia environment. Activated PSCs show increased expressions of collagen-I and α-smooth muscle actin, which are important for cancer progression and metastasis. Activated PSCs also secrete IL-6, stromal cell-derived factor-1 and transforming growth factor-β, which are associated with tumor progression and metastasis. A study demonstrated that HIF-1α increases the secretion of C-C motif chemokine ligand 2 to recruit macrophages, accelerating the activation of PSCs. Hypoxia can induce PSCs to secrete IL-6, which in turn promotes the progression of pancreatic cancer through the JAK2/STAT3 and mitogen-activated protein kinase pathways. Curcumin inhibits the tumor-stromal crosstalk by inhibiting the IL-6/ERK/NF-κB pathway, and activation of PSCs is inhibited by curcumin under hypoxic conditions. PSC, pancreatic stellate cell; IL, interleukin; HIF, hypoxia-inducible factor; CXCL2, chemokine 2; SDF-1, stromal cell derived factor-1.
Cytokines and special factors
IL-37
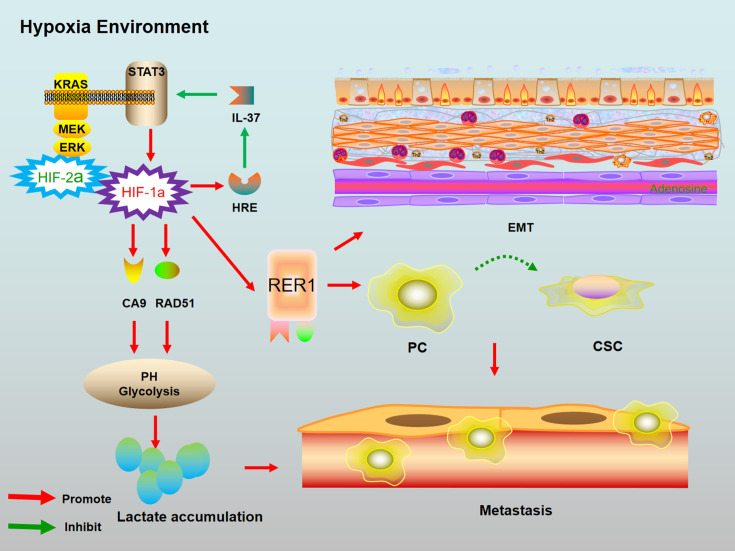
IL-37, an inhibitor of both innate and adaptive immunity, inhibits the production of pro-inflammatory cytokines as well as the maturation of dendritic cells (24). A recent study showed that low expression of IL-37 was positively correlated with PC metastasis. HIF-1α negatively regulates IL-37 gene expression in PC by binding an HRE in the IL-37 gene promoter. Moreover, IL-37 suppresses HIF-1α expression through STAT3 inhibition, and IL-37 sensitizes PC cells to gemcitabine (25) (Figure 2 ).
Figure 2.
Mechanisms of novel strategies targeting IL-37, RER1 and RAD51 under hypoxic environment. 1) HIF-1α directly binds to HREs which as a result reduced IL-37 transcription in PC. Moreover, IL-37 can suppress HIF-1α expression through STAT3 inhibition; 2) RER1 induces the development of PC via enhancing EMT and CSC pathway. RER1 can induce PC cells to convert to CSCs. Moreover, HIF-1α can increase RER1 expression, and hypoxia-induced PC cell progression may be activated by RER1 with the help of HIF-1α; 3) RAD51 positively regulated cell proliferation, decreased intracellular ROS production and increased the HIF-1α protein level. KRAS/MEK/ERK activation increased RAD51 expression; 4) PC modulate the CA9 to regulate pH. CA9 is a down-stream of mutant KRAS. Intra-tumoral hypoxia leads to HIF-1α-mediated metabolic regulation by PC and the production of acidic metabolites. Glycolysis can create an acidic microenvironment via lactate accumulation, resulting in extracellular matrix destruction that favors metastasis. IL, interleukin; RER1, retention in endoplasmic reticulum 1; RAD51, recombination protein A D51; HIF, hypoxia-inducible factor; HRE, hypoxia-response element; PC, pancreatic cancer; CSC, cancer stem cell; ROS, reactive oxygen species; CA 9, carbonic anhydrase 9.
Carbonic anhydrase 9 (CA9)
CA9 is often regarded as a vital marker of hypoxia. A number of researches have proved the positive correlation between CA9 and tumor metastasis (26). Most PC expresses KRAS with hypoxic environment. CA9 and HIF-1 are downstream of mutant KRAS, and HIF-1 is a major driver of CA9 expression in PC. Mutant KRAS regulates HIF1A stability in hypoxia, and the downstream effector CA9 promotes tumor growth and metastases. KRAS signalling regulates HIF1A and HIF2A, which lead to upregulated CA9 expression under hypoxic conditions. For survival in the hypoxic environment, PC modulates CA9 to regulate pH (27). A recent study showed that inhibition of CA9 in PC cells significantly reduced pH under hypoxic conditions, decreased gemcitabine-induced glycolysis and increased cell sensitivity to gemcitabine (28). These studies show that under hypoxia, PC can increase expression of CA9 to regulate pH and glycolysis, leading to decreased sensitivity to chemotherapy.
Retention in endoplasmic reticulum 1 (RER1)
RER1 is an important retention factor in the endoplasmic reticulum. A recent study showed that RER1 is upregulated in PC tissues and its expression is correlated with poor survival outcome, likely from its enhancement of metastasis and stem-cell like behaviour of PC cells. RER1 induces the development of PC cell lines by enhancing EMT and cancer stem cell pathways. RER1 induces PC cells to convert to cancer stem cells, which results in metastasis (29). Moreover, under hypoxic conditions, HIF-1α increases RER1 expression, and hypoxia-induced PC cell progression may be activated by RER1 with the help of HIF-1α. Knockdown of HIF-1α in PC cells leads to decreased RER1 expression and subsequent inhibition of proliferation of PC under hypoxic conditions (30).
Recombination protein A (RA) D51
RAD51, a recombinase and a specific factor in the DNA damage and repair process, plays a significant role in promoting tumor progression. RAD51 is a target of KRAS, and KRAS/MEK/ERK activation increases RAD51 expression. A recent report showed that overexpression of RAD51 was associated with poor survival in PC patients (31). Glycolysis establishes an acidic microenvironment through lactate accumulation, leading to destruction of the extracellular matrix and promoting metastasis (32). RAD51, regulated by oncogenic KRAS, promotes PC progression by modulating aerobic glycolysis via regulating the protein stability of HIF-1α (31).
Nuclear factor of activated T cells 5 (NFAT5)
NFAT5 was first identified as a tonicity-regulated transcription factor (Ton/EBP) that regulates the expression of genes involved in osmotic stress (33). A recent study revealed the potential relationship between NFAT5 and various cancers (34). NFAT5 is highly expressed in PC and its expression is related to poor survival by inducing the Warburg effect and hypoxia. Down-regulation of NFAT5 results in inhibited proliferation of PC cells under hypoxia. Phosphoglycerate kinase 1 (PGK-1), which is the key enzyme that generates ATP in glycolysis, is a direct gene target of NFAT5. Activation of NFAT5 leads to overexpression of PGK1 and promotes PC progression (35).
Non-coding RNA and hypoxia
Long non-coding RNA (lncRNAs)
The involvement of lncRNAs in PC development and metastasis and the regulatory roles of lncRNAs are hot research areas. Deng et al. reported that lncRNA-BX111887 (BX111) was associated with advanced TNM stage and reduced survival rate in PC patients, and down-regulation of BX111 suppressed the proliferation of PC cells (36). BX111 recruits the Y-box protein (YB1) transcription factor to the promoter of ZEB1, a key regulator for EMT. HIF-1α can active ZEB1 and its downstream proteins E-cadherin and matrix metalloprotease 2 under hypoxia condition. Therefore, hypoxia activates the BX111/ZEB1 pathway, which induces EMT and PC progression.
microRNA (miRNA)
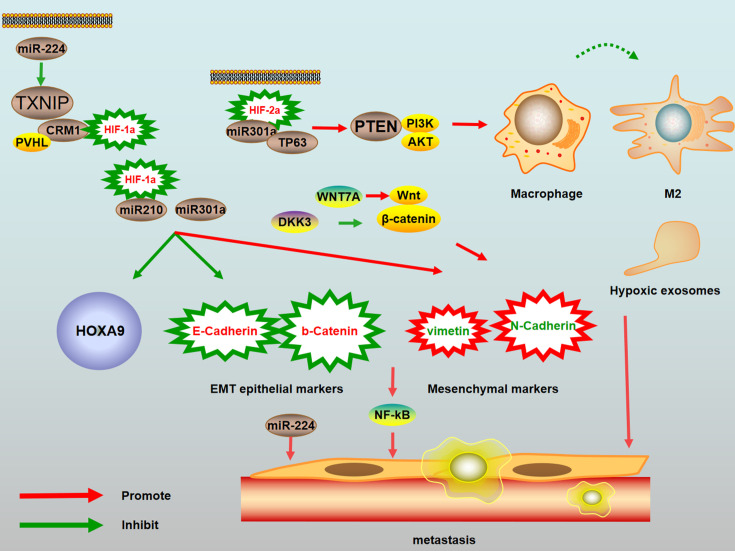
A number of studies have demonstrated that miRNAs are closely involved in PC progression under hypoxic conditions (37-39). Zhu et al. demonstrated that miR-224 is upregulated in PC and stimulates PC cancer cell proliferation. Thioredoxin-interacting protein (TXNIP), which inhibits thioredoxin, is a direct target of miR-224. Since thioredoxin induces tumor progression, TXNIP has a great potential as a tumor suppressor. Several studies have shown that overexpression of TXNIP inhibited HIF-mediated reporter activity in various cancer cell lines (40). Other reports demonstrated that TXNIP regulates the degradation of HIF-1α. TXNIP binds both HIF-1α through the CRM1 region in TXNIP and also binds the ubiquitin ligase pVHL. Formation of the TXNIP-pVHL-HIF-1α complex results in the degradation of HIF-1α. miR-224 negatively regulates TXNIP expression by directly binding to the 3’ untranslated region in its mRNA, activating HIF-1α as a result (39). The miR-224-TXNIP-HIF-1α axis is important for PC cell proliferation and migration and may represent a novel target for cancer therapeutics (Figure 3 ). miR212, located on chromosome 17p13.3, has been reported to be significantly increased in PC tissues and its expression positively correlates with PC metastasis and invasion and poor prognosis of PC patients (41). A recent study reported the positive relationship between the expression of HIF-1α and miR-212 in hypoxic conditions. Mechanistically, HIF-1α binds to an HRE in the miR-212 promoter region, leading to activated miR-212 expression in PC cells, and increased miR-212 was associated with a poor clinical prognosis (38).
Figure 3.
Mechanisms of novel strategies targeting miRNAs and EMT under hypoxia condition. 1) miR-224 inversely regulated TXNIP by binding directly it, activating HIF-1α as a result. The CRM1 region of TXNIP binds the nuclear transcription factor HIF-1α and the ubiquitin ligase pVHL. The TXNIP-pVHL-HIF-1α complex results in the degradation of HIF-1α; 2) TP63 was a direct target of miR-301a and involved in the metastatic process of PC cells via up-regulation of epithelial marker E-cadherin and the down-regulation of mesenchymal marker vimentin; 3) Over-expression of miR-210 can decrease the E-cadherin and b-catenin as well as HOXA9 level and increase vimentin and N-cadherin; 4) WNT7A is a vital ligand to activate the Wnt/β-catenin pathway. WNT7A expression promotes higher expression of N-cadherin and lower expression of E-cadherin; 5) DKK-3 inhibits EMT of PC cells in hypoxic conditions by suppressing the translocation of b-catenin to nucleus, resulting in enhancing of the antitumor effects to PC. EMT, epithelial-to-mesenchymal transition; TXNIP, thioredoxin-interacting protein; HIF, hypoxia-inducible factor; DKK-3, dickkopf-related protein 3.
A recent study showed that miR-301a is a downstream target of HIF-2α and is induced by HIF-2α in response to hypoxia. Moreover, miR-301a enhanced the hypoxia-induced EMT of PC cells through the elevated expression of mesenchymal cell markers and reduced expression of epithelial cell markers. TP63, a member of the tumor suppressor family, plays a negative role in the metastasis of PC cell lines by its up-regulation of the epithelial marker E-cadherin and down-regulation of the mesenchymal marker vimentin (42). TP63 is a key target of miR-301a, and miR-301a inhibits its expression. These findings suggest that the HIF-2α-miR301a-TP63 signalling pathway is involved in hypoxia-induced EMT in PC and may become a new target for PC treatment. Hypoxia induces EMT through multiple signalling pathways (43). Cannito et al. demonstrated that the NF-kB signalling pathway is closely associated with HIF-1α-induced EMT and inhibiting the NF-kB signalling pathway reverses EMT (44).
miR-210 is regulated by HIF-1α under hypoxia and plays a significant role in the cancer EMT process (45). HOXA9 belongs to the homeobox (HOX) family of transcription factors that inhibit EMT in PC. A recent study found that HOXA9 is a target of miR-210. Moreover, miR-210, HIF-1α and NF-kB were increased while HOXA9 was reduced in PC cells under hypoxia. Overexpression of miR-210 decreases E-cadherin and B-catenin expression (EMT epithelial markers) as well as HOXA9 level and increases vimentin and N-cadherin expressions (mesenchymal markers), which as a result decreases NF-kB expression and promotes cell metastasis. miR-210 thus inhibits HOXA9 and activates the NF-kB signalling pathway to promote EMT of PC cells induced by HIF-1α under hypoxia (46).
Gene products
YEATS domain containing 2 (YEATS2)
The YEATS2 gene is a key hypoxia-associated gene (47). A recent study showed that YEATS2 is highly expressed in PC cells under hypoxia and its high expression predicts poor outcome (48). Moreover, the authors found that down-regulation of YEATS2 inhibits the development and migration of PC cells under hypoxia. YEATS2 is a transcriptional target of HIF-1α; HIF-1α regulates the gene expression of YEATS2 by binding to the HRE in the promoter of YEATS2. Inhibition of HIF-1α decreased the proliferation ability and migration of PC cells under hypoxia, but overexpression of YEATS2 reversed this effect. Hence, YEATS2 is regulated by HIF-1α and promotes PC cell proliferation as well as metastasis under hypoxic conditions.
Human family with sequence similarity 115, member C (FAM115C)
FAM115C, also known as TCAF2, is a novel gene that is overexpressed in PC cells. FAM115C binds to and interacts with transient receptor potential 8 (TRPM8), which promotes the trafficking of FAM115C to the cell surface. Saeki et al. reported increased levels of FAM115C under hypoxia compared with normoxia in PC and demonstrated that inhibitors of FAM115C could promote the progression of PC (49). The authors examined whether FAM115C mRNA was associated with the survival of patients with PC. Surprisingly, patients with high FAM115C expression showed significantly better overall survival (P=0.0463) and disease-free survival (P=0.029) compared with patients with low FAM115C expression. These findings demonstrated that high expression of FAM115C was associated with better prognosis in patients with PC. Furthermore, knockdown of HIF-1α in all of the PC cell lines examined in the study decreased the expression of FAM115C, which suggested that HIF-1α might be a modulator of FAM115C expression in PC cells induced by hypoxia.
Insulin-induced gene 2 (Insig2)
Insig2 is a tumor-related protein that regulates the proteolytic activation of sterol regulatory element-binding proteins (50). Overexpression of Insig2 has been reported to alter the mitochondrial gene expressions of several apoptosis-related factors and regulate mitochondria-mediated apoptosis in cancer cells (51). A recent study showed that Insig2 mRNA expression levels were significantly higher in PC cells than in non-tumor pancreatic cells especially under hypoxic conditions. In addition, inhibition of Insig2 decreased the invasion ability of PC, suggesting that Insig2 has a functional role in proliferation and invasion of PC cells (52).
Metastasis-associated gene 1 (MTA1)
MTA1, a member of the nucleosome remodelling and histone deacetylation complex, has been associated with the progression and metastasis of cancers (53).
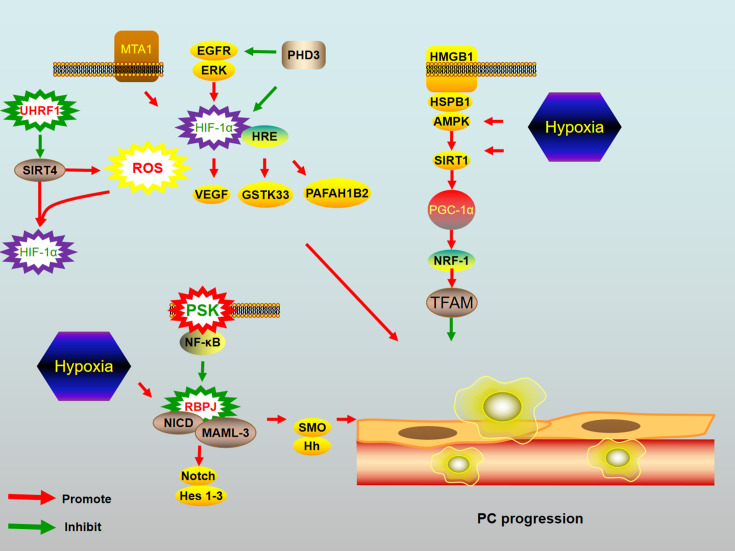
Vascular endothelial growth factor (VEGF) is vital for tumor angiogenesis and progression. VEGF is a downstream target of HIF-1α and is regulated by HIF-1α under hypoxia conditions (54). A recent study showed that MTA1 induces PC metastasis via the HIF-1α/VEGF pathway (55). In response to hypoxia, MTA1 increases the expressions of HIF-1α and VEGF proteins. Moreover, HIF-1α aggregation regulates the expression level of VEGF and its receptors in cancer and may accelerate metastasis. These findings suggest a novel MTA1/HIF-α/VEGF pathway and indicate that MTA1 may be a potential target for PC treatment.
Enzymes and hypoxia
Proline hydroxylase domains 3 (PHD3)
Abnormal expression of epidermal growth factor receptor (EGFR) can accelerate the development of PC (56). HIF-1α is an important factor in the EGFR-mediated pathway, and HIF-1α and EGFR signalling form a positive feedback loop. Decreasing HIF-1α can inhibit activation of the EGFR/ERK/HIF-1α loop (57).
PHD3 is a rate-limiting enzyme that degrades HIF-1α in the hypoxic microenvironment of PC (58). HIF-1α is degraded by PHD under hypoxic conditions to help PC tolerate hypoxic conditions (59). A previous study reported that PHD3 suppresses EGFR during tumorigenesis (60). In response to irradiation under hypoxia, overexpression of PHD3 not only reduced HIF-1α protein expression but also reduced EGFR phosphorylation and inhibited the growth of PC by inducing cell cycle arrest at G2/M phase (61). These findings indicate that PHD3 inhibits PC proliferation under the hypoxic environment (Figure 4 ).
Figure 4.
Mechanisms of novel strategies targeting signaling pathway and mitochondrial abnormalities under hypoxia condition. (1) Under hypoxia, MTA1 increased the expression of HIF-α and VEGF proteins; (2) EGFR/ERK/HIF-1α can be activated by hypoxic conditions. PHD3 can degrade HIF-1α in the hypoxic microenvironment of PC; (3) Hypoxia induced STK33 expression in PC cells. HIF-1α regulated STK33 via direct binding to a hypoxia response element in its promoter; (4) HIF-1α directly increased the expression of PAFAH1B2 by binding to an HRE on PAFAH1B2 promoter in PC cells; (5) PGC-1α activates NRF-1 and then up-regulates TFAM expression. HMGB1 can up-regulate the protein expression of PGC-1α, and then activate AMPK. AMPK can regulate mitochondrial biogenesis by increasing SIRT1 and inducing PGC-1 deacetylation; (6) SIRT4 is a downstream target of Ubiquitin like with plant homeodomain and ring finger domains 1 (UHRF1) and negatively correlated with UHRF1, which can suppress HIF-1α; (7) PSK can not only inhibit SMO but also reduce mastermind-like 3 and recombination signal binding protein for immunoglobulin-kappa-J region (RBPJ) expression in PC cells under hypoxia. Hh signaling can be activated by increasing the transcription of SMO gene under hypoxia. Another mechanism is that RBPJ forms a complex with the NICD that is stabilized by MAML3, and Notch signaling is activated by binding of the RBPJ/NICD/MAML3 complex to DNA in the nucleus. Hes1-3, a target gene of Notch signaling, can be decreased by RBPJ and MAML3 inhibition. RBPJ and MAML3 inhibition under hypoxia led to decreased SMO. MTA1, metastasis-associated gene 1; HIF, hypoxia-inducible factor; VEGF, vascular endothelial growth factor; EGFR, epidermal growth factor receptor; PC, pancreatic cancer; STK 33, serine/threonine kinase 33; PAFAH1B2, platelet-activating factor acetylhydrolase IB subunit beta; NRF, nuclear respiratory factor; TFAM, mitochondrial transcription factor A; HMGB1, High-mobility group box-1; AMPK, AMP-activated protein kinase; SMO, smoothened; Hh, Hedgehog; MAML3, mastermind-like 3.
Heme oxygenase-1 (HO-1)
HO-1, one of the stress-associated enzymes whose expression is stimulated by hypoxia, plays antioxidant roles and is upregulated in response to hypoxia and ROS (62). A previous study demonstrated that HO-1 is upregulated in PC, and treatment of PC cells with HO-1 inhibitors leads to increased sensitivity to chemotherapy (63). Recent results showed that increased HO-1 expression in response to hypoxia led to PC cell proliferation. Under hypoxic conditions, PC cells treated with HO-1 inhibitors are more sensitive to gemcitabine than cells treated with gemcitabine alone. Inhibition of HO-1 increases the production of ROS and disrupts glutathione, and inhibitors of HO-1 reduce the expression of stemness markers in PC cell lines, which in turn inhibit PC tumor growth and metastasis (64).
Endoplasmic reticulum oxidoreductin 1-α (ERO1α)
The oxidoreductase enzyme ERO1α has been reported to play a significant role in cancer cell invasion of healthy tissues and promotion of angiogenesis in various malignancies (65,66). ERO1α is highly expressed in PC and activated by hypoxia stress in PC, and its high expression is correlated with poor prognosis in PC patients. ERO1α enzyme activity leads to generation of ROS, which directly regulates the hypoxia response through HIF-1α transcription factor. Genetic deletion of ERO1α in mice resulted in inhibited ROS production, decreased PC cells growth and suppressed tumorigenicity (67).
Serine/threonine kinase 33 (STK33)
STK33 belongs to a family of calcium/calmodulin-dependent kinases. A recent study demonstrated that STK33 is highly expressed in PC and its high expression is closely related to poor prognosis (68). Mechanically, the STK33 gene is a direct target of HIF-1α and is transcriptionally regulated by HIF-1α. HIF-1α/STK33 signaling promotes PC growth and proliferation.
Proteins and hypoxia
Mucins (MUC)20
Mucins are heavily glycosylated proteins that can promote cancer development. PC is characterized by the abnormal expression of both secretory and transmembrane mucins. A recent study demonstrated that overexpression of MUC20 is closely associated with poor survival of PC patients (69). Moreover, hypoxia can induce the expression of MUC20 in PC cells, while MUC20 knockdown inhibits PC cells proliferation by suppressing the HGF/MET pathway.
LIM and senescent cell antigen-like-containing domain protein 1 (LIMS1)
LIMS1, also known as PINCH1, is a marker for senescent erythrocytes. LIMS1 consists of five LIM domains and tandem nuclear localization signals. LIMS1 binds to integrin-linked kinase as well as parvin to form a ternary protein complex, which plays a significant role in cell-extracellular matrix adhesion-mediated cell behaviour (70). LIMS1 directly inhibits phosphatase 1α to activate Akt1 phosphorylation (71). A recent study showed that LIMS1 promotes PC cell survival under hypoxia by activating AKT/mTOR signalling, which enables PC adaptation to the hypoxia stress. LIMS1 enhances GLUT1 expression via HIF-1α, while HIF-1α enhances glucose influx by activating GLUT1 and promoting LIMS1 transcription, thus forming a LIMS1-HIF-1 positive loop in PC cell adaptation to hypoxia (72). Inhibition of LIMS1 significantly suppressed PC mouse models. Hence, LIMS1 is a key factor in the interaction between hypoxia and PC survival.
Polypyrimidine tract-binding protein 3 (PTBP3)
The cellular response to hypoxia is primarily regulated through post-transcriptional mechanisms involving RNA-binding proteins. Certain RNA-binding proteins bind to hypoxia-related transcripts to affect the expression of hypoxic genes.
The RNA splicing protein PTBP3, which is also known as ROD1, functions as a splicing repressor. PTBP3 regulates hypoxic gene expression by selectively binding to hypoxia-regulated transcripts. Hypoxia accelerates the accumulation of autophagosomes by increasing the expression of autophagy-related genes, such as the gene encoding ATG12, which modulates autophagy and endolysosomal transport. Cancer cells protect against the stressful conditions of TME and adapt to hypoxia through autophagy (73).
A recent study showed that hypoxia significantly increased the expression of PTBP3 in PC, and PTBP3 overexpression promoted PC proliferation under hypoxia and rendered PC cells more resistance to gemcitabine (74). In addition, down-regulation of PTBP3 not only inhibited PC growth and metastasis but also decreased resistance to gemcitabine. PTBP3 binds to a PTBP3 binding motif in the 3’-untranslated region of ATG12 mRNA to increase ATG12 expression in response to hypoxic stress, leading to increased cancer cell proliferation and autophagic flux as well as gemcitabine resistance.
Novel candidate treatments
β-elemene
Late-stage PC patients with peritoneum effusion generally report a poor life quality. A recent study showed that HIF-1α can promote peritoneum effusion by activating its target VEGFA, and the HIF-1α/VEGFA pathway is closely associated with peritoneum effusion (75).
β-elemene is an extract from Curcuma wenyujin, which is a traditional Chinese medicinal herb (76). Notably, β-elemene has been reported to inhibit the expression of HIF-1α in cancer (77). Previous studies showed that β-elemene can reverse chemoresistance, suppress cancer progression, reduce tumor angiogenesis and even treat malignant pleural effusion (78,79). Mechanistically, β-elemene decreases HIF-1α and its downstream target VEGFA to inhibit the proliferation of PC cells from peritoneum effusion (80).
Ubiquitin like with plant homeodomain and ring finger domains 1 (UHRF1)
UHRF1 is a chromatin modifier that is overexpressed in PC and is associated with DNA methylation and heterochromatin formation that leads to tumor suppressor gene silencing (81). Hu et al. recently reported that high UHRF1 expression predicted worse prognosis of PC. Furthermore, high UHRF1 expression enhanced PC cell proliferation by inducing aerobic glycolysis, while down-regulation of UHRF1 inhibited HIF-1α and suppressed aerobic glycolysis in PC cells. SIRT4, a tumor suppressor as well as mitochondrial negative regulator of aerobic glycolysis, is a downstream target of UHRF1 and negatively correlated with UHRF1 in PC. SIRT4 inhibits aerobic glycolysis, cell proliferation and tumor growth by suppressing HIF-1α. One study showed that UHRF1 might promote aerobic glycolysis via suppression of SIRT4 (82). Moreover, SIRT4 has been reported to be associated with ROS production. Increased ROS production inhibits the catalytic activity of prolyl hydroxylase, which is a negative regulator of HIF-1α (83). Hence, SIRT4 can inhibit HIF-1α production.
Propofol
Previous studies showed that ADAM metallopeptidase domain 8 (ADAM8) is significantly induced by hypoxia and its expression is associated with progression, metastasis and poor prognosis of PC (84). A recent report showed that propofol suppressed the progression of PC by inhibiting ADAM8 under hypoxia, and subcutaneous injection of propofol decreased tumor progression in PC mouse model (85).
PAFAH1B2
Platelet-activating factor (PAF) is an inflammatory mediator that plays a significant role in various physiological processes. PAF is deacetylated by PAF acetylhydrolase (PAFAH). Platelet-activating factor acetylhydrolase IB subunit beta (PAFAH1B2) is the catalytic subunit of PAFAH. A recent study demonstrated that PAFAH1B2 is overexpressed in PC, and HIF-1α increases the expression of PAFAH1B2 by binding to an HRE in the PAFAH1B2 promoter in PC cells. Moreover, activation of PAFAH1B2 by HIF-1α promotes EMT and metastasis of PC (86).
Resveratrol
The Hh signalling pathway has been shown to be very active in PC (87). The Hh signalling pathway is activated by binding of Hh to the membrane receptor Patched 1, which results in smoothened (SMO) dissociation and up-regulation of the GLI transcription factor.
Resveratrol is a natural polyphenolic phytoalexin that is extracted from plants. Recent studies have shown that resveratrol can restrict cell proliferation and increase cell apoptosis via inhibition of the Hh signalling pathway (88). The hypoxic environment shows significantly increased expression levels of Hh pathway-related factors such as SHH, SMO and GLI1 in PC cells, and resveratrol inhibits the induction of these factors (89). Hypoxia-induced ROS is closely associated with PC metastasis. Increasing evidence has shown that resveratrol inhibits the hypoxia-induced production of ROS (90). These findings indicate that resveratrol plays a significant role in reducing hypoxia-driven ROS-induced PC progression by suppressing the Hh signalling pathway.
Signaling regulators
Protein-bound polysaccharide-K (PSK)
The expressions of SMO, mastermind-like 3 (MAML3) and recombination signal binding protein for immunoglobulin-kappa-J region (RBPJ) are increased under hypoxia in PC. A recent study showed that hypoxia promotes SMO transcription through up-regulation of MAML3 and RBPJ to induce proliferation and metastasis in PC (91). Hh signalling can be activated by increased transcription of the SMO gene under hypoxia, which can lead to PC progression (92). Notch signalling is associated with cancer progression and hypoxia. RBPJ forms a complex with the Notch intracellular domain (NICD) that is stabilized by MAML3, and Notch signalling is activated by binding of the RBPJ/NICD/MAML3 complex to nuclear DNA. Hes1-3, a target gene of Notch signalling, is decreased by RBPJ and MAML3 inhibition, suggesting that RBPJ and MAML3 are involved in Notch signalling activation (93).
PSK, a protein-bound polysaccharide, can inhibit PC cell invasiveness (94). A previous study showed that RBPJ and MAML3 both function in the up-regulation of SMO transcription (95). However, PSK not only inhibits SMO but also reduces MAML3 and RBPJ expression in PC cells under hypoxia. Given that SMO is the key activator of the Hh signalling pathway, these findings suggest that PSK can inhibit SMO/Hh signalling through down-regulation of MAML3 and RBPJ transcription under hypoxia, which as a result improve the treatment of PC (96).
Apatinib
VEGF and its receptors play an essential role in carcinogenesis. HIF-1α not only helps PC cells adapt to hypoxia but also promotes PC progression by modulating expression of its downstream VEGF gene (97). Apatinib is a novel drug that selectively inhibits VEGFR (98). A recent study showed that apatinib suppresses the progression of PC by reducing HIF-1α and VEGF and inhibiting the PI3K/Akt/mTOR signalling pathway (99). Moreover, positive outcomes have been reported in patients with PC treated with apatinib (100).
Transcription factor 7-like2 (TCF7L2)
Activation of the Wnt/β-catenin signalling culminates in the progression of PC. TCF7L2, a β-catenin transcriptional partner, plays a vital role in the Wnt/β-catenin signalling pathway and is a key activator of Wnt target genes (101,102). A recent study reported that high TCF7L2 expression predicted worse prognosis in PC patients. TCF7L2 upregulates aerobic glycolysis by inhibiting Egl-9 family hypoxia inducible factor 2 (EGLN2), resulting in increased HIF-1α, which then promotes the proliferation of PC. The EGLN2 enzymes activate HIF hydroxylases in response to hypoxia. Moreover, EGLN2 is downstream of TCF7L2 in PC and inhibits proliferation and development in PC (103). Therefore, TCF7L2 regulates aerobic glycolysis to promote the progression of PC by targeting the EGLN2/HIF-1α axis.
Dickkopf-related protein 3 (DKK-3)
The Wnt/b-catenin signalling pathway can activate PC progression. DKK3 is a member of the human Dickkopf family secreted proteins and an antagonist of Wnt ligand activity. A recent study showed that DKK3 expression was significantly lower in PC tissues compared with non-tumor tissues and that DKK3 inhibits nuclear translocation of β-catenin induced by hypoxia in PC. DKK3 reduced migration and the stem cell-like phenotype of PC cells in hypoxic conditions by suppressing EMT. These results indicate that DKK3 inhibits EMT of PC cells in hypoxic conditions by suppressing the translocation of β-catenin to the nucleus, resulting in anti-tumor effects in PC (104). Therefore, DKK3 is a tumor suppressor and improves gemcitabine therapeutic effect through inducing apoptosis and regulating β-catenin/EMT signalling in PC.
Problems and future direction
Hypoxia is a key determinant amongst the TME driving pancreatic tumor malignancy. Current strategies have shown success in the treatment of PC but relatively few clinical studies have been done. Extensive researches have identified hypoxia to drive a number of pathways in PC that lead to invasiveness, induction of EMT, metastasis. However, all these findings point to hypoxia as an important therapeutic target in PC have to be proved by future exploration. Hopefully, we reviewed those novel strategies that can increase the efficacy and reduce toxicity of chemotherapeutic agents in order to provide a direction for future researches and explorations. For example, the novel antihypoxic molecule Evofosfamide and myo-inositoltrispyrophosphate (ITPP, OXY111A) target tumor hypoxia and are used to target PC cells under hypoxic conditions (105,106).
Conclusions
Current research has established that hypoxia plays a significant role in the biological function of PC. Here, we provided new insights into potential novel strategies targeting hypoxia in PC and the regulatory molecular mechanisms, with the aim of improving treatment outcome in PC. Obstacles of PC treatment field in general with respect to targeting hypoxia are lacking of enough practice. Future research should focus on combinations of novel drugs.
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (No. 81772639 and No.81972258), Natural Science Foundation of Beijing (No. 7192157), National Fundamental Research Program of China (No. 2018YFE0118600), and Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (No. 2019XK320001).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Siegel RL, Miller KD, Jemal A Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.National Health Commission of the People’s Republic of China Chinese guidelines for diagnosis and treatment of pancreatic cancer 2018 (English version) Chin J Cancer Res. 2019;31:278–94. doi: 10.21147/j.issn.1000-9604.2019.02.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dougan SK The pancreatic cancer microenvironment. Cancer J. 2017;23:321–5. doi: 10.1097/ppo.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 4.Erkan M, Kurtoglu M, Kleeff J The role of hypoxia in pancreatic cancer: a potential therapeutic target? Expert Rev Gastroenterol Hepatol. 2016;10:301–16. doi: 10.1586/17474124.2016.1117386. [DOI] [PubMed] [Google Scholar]
- 5.Zimna A, Kurpisz M Hypoxia-inducible factor-1 in physiological and pathophysiological angiogenesis: Applications and therapies. Biomed Res Int. 2015;2015:549412. doi: 10.1155/2015/549412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hwang HK, Wada K, Kim HY, et al A nomogram to preoperatively predict 1-year disease-specific survival in resected pancreatic cancer following neoadjuvant chemoradiation therapy. Chin J Cancer Res. 2020;32:105–14. doi: 10.21147/j.issn.1000-9604.2020.01.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Li Y, Yan K, et al Clinical study of ultrasound and microbubbles for enhancing chemotherapeutic sensitivity of malignant tumors in digestive system. Chin J Cancer Res. 2018;30:553–63. doi: 10.21147/j.issn.1000-9604.2018.05.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li H, Wang X, Wen C, et al Long noncoding RNA NORAD, a novel competing endogenous RNA, enhances the hypoxia-induced epithelial-mesenchymal transition to promote metastasis in pancreatic cancer. Mol Cancer. 2017;16:169. doi: 10.1186/s12943-017-0738-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fuhrmann DC, Brüne B Mitochondrial composition and function under the control of hypoxia. Redox Biol. 2017;12:208–15. doi: 10.1016/j.redox.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo A, Li K, Xiao Q Fibroblast growth factor 19 alleviates palmitic acid-induced mitochondrial dysfunction and oxidative stress via the AMPK/PGC-1α pathway in skeletal muscle. Biochem Biophys Res Commun. 2020;526:1069–76. doi: 10.1016/j.bbrc.2020.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Kang R, Xie Y, Zhang Q, et al Intracellular HMGB1 as a novel tumor suppressor of pancreatic cancer. Cell Res. 2017;27:916–32. doi: 10.1038/cr.2017.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tohme S, Yazdani HO, Liu Y, et al Hypoxia mediates mitochondrial biogenesis in hepatocellular carcinoma to promote tumor growth through HMGB1 and TLR9 interaction. Hepatology. 2017;66:182–97. doi: 10.1002/hep.29184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang L, Ye F, Zeng L, et al Knockdown of HMGB1 suppresses hypoxia-induced mitochondrial biogenesis in pancreatic cancer cells. Onco Targets Ther. 2020;13:1187–98. doi: 10.2147/ott.S234530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sancho P, Burgos-Ramos E, Tavera A, et al MYC/PGC-1α balance determines the metabolic phenotype and plasticity of pancreatic cancer stem cells. Cell Metab. 2015;22:590–605. doi: 10.1016/j.cmet.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 15.Wu Q, Tian Y, Zhang J, et al Functions of pancreatic stellate cell-derived soluble factors in the microenvironment of pancreatic ductal carcinoma. Oncotarget. 2017;8:102721–38. doi: 10.18632/oncotarget.21970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li N, Li Y, Li Z, et al Hypoxia inducible factor 1 (HIF-1) recruits macrophage to activate pancreatic stellate cells in pancreatic ductal adenocarcinoma. Int J Mol Sci. 2016;17:799. doi: 10.3390/ijms17060799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vainer N, Dehlendorff C, Johansen JS Systematic literature review of IL-6 as a biomarker or treatment target in patients with gastric, bile duct, pancreatic and colorectal cancer. Oncotarget. 2018;9:29820–41. doi: 10.18632/oncotarget.25661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pop VV, Seicean A, Lupan I, et al IL-6 roles — molecular pathway and clinical implication in pancreatic cancer - A systemic review. Immunol Lett. 2017;181:45–50. doi: 10.1016/j.imlet.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Goumas FA, Holmer R, Egberts JH, et al Inhibition of IL-6 signaling significantly reduces primary tumor growth and recurrencies in orthotopic xenograft models of pancreatic cancer. Int J Cancer. 2015;137:1035–46. doi: 10.1002/ijc.29445. [DOI] [PubMed] [Google Scholar]
- 20.Allegra A, Innao V, Russo S, et al Anticancer activity of curcumin and its analogues: Preclinical and clinical studies. Cancer Invest. 2017;35:1–22. doi: 10.1080/07357907.2016.1247166. [DOI] [PubMed] [Google Scholar]
- 21.Li W, Sun L, Lei J, et al Curcumin inhibits pancreatic cancer cell invasion and EMT by interfering with tumor stromal crosstalk under hypoxic conditions via the IL 6/ERK/NF κB axis. Oncol Rep. 2020;44:382–92. doi: 10.3892/or.2020.7600. [DOI] [PubMed] [Google Scholar]
- 22.Cao L, Xiao X, Lei J, et al Curcumin inhibits hypoxia-induced epithelial mesenchymal transition in pancreatic cancer cells via suppression of the hedgehog signaling pathway. Oncol Rep. 2016;35:3728–34. doi: 10.3892/or.2016.4709. [DOI] [PubMed] [Google Scholar]
- 23.Kanai M, Yoshimura K, Asada M, et al A phase I/II study of gemcitabine-based chemotherapy plus curcumin for patients with gemcitabine-resistant pancreatic cancer. Cancer Chemother Pharmacol. 2011;68:157–64. doi: 10.1007/s00280-010-1470-2. [DOI] [PubMed] [Google Scholar]
- 24.Wu W, Wang W, Wang Y, et al IL-37b suppresses T cell priming by modulating dendritic cell maturation and cytokine production via dampening ERK/NF-κB/S6K signalings. Acta Biochim Biophys Sin (Shanghai) 2015;47:597–603. doi: 10.1093/abbs/gmv058. [DOI] [PubMed] [Google Scholar]
- 25.Zhao T, Jin F, Xiao D, et al IL-37/ STAT3/ HIF-1α negative feedback signaling drives gemcitabine resistance in pancreatic cancer. Theranostics. 2020;10:4088–100. doi: 10.7150/thno.42416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chiche J, Ilc K, Laferrière J, et al Hypoxia-inducible carbonic anhydrase IX and XII promote tumor cell growth by counteracting acidosis through the regulation of the intracellular pH. Cancer Res. 2009;69:358–68. doi: 10.1158/0008-5472.Can-08-2470. [DOI] [PubMed] [Google Scholar]
- 27.Corbet C, Feron O Tumour acidosis: from the passenger to the driver’s seat. Nat Rev Cancer. 2017;17:577–93. doi: 10.1038/nrc.2017.77. [DOI] [PubMed] [Google Scholar]
- 28.McDonald PC, Chafe SC, Brown WS, et al Regulation of pH by carbonic anhydrase 9 mediates survival of pancreatic cancer cells with activated KRAS in response to hypoxia. Gastroenterology. 2019;157:823–37. doi: 10.1053/j.gastro.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 29.Shiozawa Y, Nie B, Pienta KJ, et al Cancer stem cells and their role in metastasis. Pharmacol Ther. 2013;138:285–93. doi: 10.1016/j.pharmthera.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen S, Zhang J, Chen J, et al RER1 enhances carcinogenesis and stemness of pancreatic cancer under hypoxic environment. J Exp Clin Cancer Res. 2019;38:15. doi: 10.1186/s13046-018-0986-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang X, Ma N, Yao W, et al RAD51 is a potential marker for prognosis and regulates cell proliferation in pancreatic cancer. Cancer Cell Int. 2019;19:356. doi: 10.1186/s12935-019-1077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brahimi-Horn MC, Pouysségur J Hypoxia in cancer cell metabolism and pH regulation. Essays Biochem. 2007;43:165–78. doi: 10.1042/bse0430165. [DOI] [PubMed] [Google Scholar]
- 33.Lee JH, Kim M, Im YS, et al NFAT5 induction and its role in hyperosmolar stressed human limbal epithelial cells. Invest Ophthalmol Vis Sci. 2008;49:1827–35. doi: 10.1167/iovs.07-1142. [DOI] [PubMed] [Google Scholar]
- 34.Kim DH, Kim KS, Ramakrishna S NFAT5 promotes in vivo development of murine melanoma metastasis . Biochem Biophys Res Commun. 2018;505:748–54. doi: 10.1016/j.bbrc.2018.09.171. [DOI] [PubMed] [Google Scholar]
- 35.Jiang Y, He R, Jiang Y, et al Transcription factor NFAT5 contributes to the glycolytic phenotype rewiring and pancreatic cancer progression via transcription of PGK1. Cell Death Dis. 2019;10:948. doi: 10.1038/s41419-019-2072-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deng SJ, Chen HY, Ye Z, et al Hypoxia-induced LncRNA-BX111 promotes metastasis and progression of pancreatic cancer through regulating ZEB1 transcription. Oncogene. 2018;37:5811–28. doi: 10.1038/s41388-018-0382-1. [DOI] [PubMed] [Google Scholar]
- 37.Mace TA, Collins AL, Wojcik SE, et al Hypoxia induces the overexpression of microRNA-21 in pancreatic cancer cells. J Surg Res. 2013;184:855–60. doi: 10.1016/j.jss.2013.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yue H, Liu L, Song Z miR-212 regulated by HIF-1α promotes the progression of pancreatic cancer. Exp Ther Med. 2019;17:2359–65. doi: 10.3892/etm.2019.7213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu G, Zhou L, Liu H, et al MicroRNA-224 promotes pancreatic cancer cell proliferation and migration by targeting the TXNIP-mediated HIF1α pathway. Cell Physiol Biochem. 2018;48:1735–46. doi: 10.1159/000492309. [DOI] [PubMed] [Google Scholar]
- 40.Wong RW, Hagen T Mechanistic target of rapamycin (mTOR) dependent regulation of thioredoxin interacting protein (TXNIP) transcription in hypoxia. Biochem Biophys Res Commun. 2013;433:40–6. doi: 10.1016/j.bbrc.2013.02.070. [DOI] [PubMed] [Google Scholar]
- 41.Wu Z, Zhou L, Ding G, et al Overexpressions of miR-212 are associated with poor prognosis of patients with pancreatic ductal adenocarcinoma. Cancer Biomark. 2017;18:35–9. doi: 10.3233/cbm-160671. [DOI] [PubMed] [Google Scholar]
- 42.Zhang KD, Hu B, Cen G, et al MiR-301a transcriptionally activated by HIF-2α promotes hypoxia-induced epithelial-mesenchymal transition by targeting TP63 in pancreatic cancer. World J Gastroenterol. 2020;26:2349–73. doi: 10.3748/wjg.v26.i19.2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jiang J, Tang YL, Liang XH EMT: a new vision of hypoxia promoting cancer progression. Cancer Biol Ther. 2011;11:714–23. doi: 10.4161/cbt.11.8.15274. [DOI] [PubMed] [Google Scholar]
- 44.Cannito S, Novo E, Compagnone A, et al Redox mechanisms switch on hypoxia-dependent epithelial-mesenchymal transition in cancer cells. Carcinogenesis. 2008;29:2267–78. doi: 10.1093/carcin/bgn216. [DOI] [PubMed] [Google Scholar]
- 45.Devlin C, Greco S, Martelli F, et al miR-210: More than a silent player in hypoxia. IUBMB Life. 2011;63:94–100. doi: 10.1002/iub.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ni J, Zhou S, Yuan W, et al Mechanism of miR-210 involved in epithelial-mesenchymal transition of pancreatic cancer cells under hypoxia. J Recept Signal Transduct Res. 2019;39:399–406. doi: 10.1080/10799893.2019.1683863. [DOI] [PubMed] [Google Scholar]
- 47.Wang YL, Faiola F, Xu M, et al Human ATAC is a GCN5/PCAF-containing acetylase complex with a novel NC2-like histone fold module that interacts with the TATA-binding protein. J Biol Chem. 2008;283:33808–15. doi: 10.1074/jbc.M806936200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zeng Z, Lei S, He Z, et al YEATS2 is a target of HIF1α and promotes pancreatic cancer cell proliferation and migration. J Cell Physiol. 2021;236:2087–98. doi: 10.1002/jcp.29995. [DOI] [PubMed] [Google Scholar]
- 49.Saeki K, Onishi H, Koga S, et al FAM115C could be a novel tumor suppressor associated with prolonged survival in pancreatic cancer patients. J Cancer. 2020;11:2289–302. doi: 10.7150/jca.38399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yabe D, Brown MS, Goldstein JL Insig-2, a second endoplasmic reticulum protein that binds SCAP and blocks export of sterol regulatory element-binding proteins. Proc Natl Acad Sci U S A. 2002;99:12753–8. doi: 10.1073/pnas.162488899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li CG, Gruidl M, Eschrich S, et al Insig2 is associated with colon tumorigenesis and inhibits Bax-mediated apoptosis. Int J Cancer. 2008;123:273–82. doi: 10.1002/ijc.23510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kayashima T, Nakata K, Ohuchida K, et al Insig2 is overexpressed in pancreatic cancer and its expression is induced by hypoxia. Cancer Sci. 2011;102:1137–43. doi: 10.1111/j.1349-7006.2011.01936.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sen N, Gui B, Kumar R Role of MTA1 in cancer progression and metastasis. Cancer Metastasis Rev. 2014;33:879–89. doi: 10.1007/s10555-014-9515-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahluwalia A, Tarnawski AS Critical role of hypoxia sensor — HIF-1α in VEGF gene activation. Implications for angiogenesis and tissue injury healing. Curr Med Chem. 2012;19:90–7. doi: 10.2174/092986712803413944. [DOI] [PubMed] [Google Scholar]
- 55.Sun X, Zhang Y, Li B, et al MTA1 promotes the invasion and migration of pancreatic cancer cells potentially through the HIF-α/VEGF pathway. J Recept Signal Transduct Res. 2018;38:352–8. doi: 10.1080/10799893.2018.1531887. [DOI] [PubMed] [Google Scholar]
- 56.Ardito CM, Grüner BM, Takeuchi KK, et al EGF receptor is required for KRAS-induced pancreatic tumorigenesis. Cancer Cell. 2012;22:304–17. doi: 10.1016/j.ccr.2012.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang G, Li Y, Yang Z, et al ROS mediated EGFR/MEK/ERK/HIF-1α loop regulates glucose metabolism in pancreatic cancer. Biochem Biophys Res Commun. 2018;500:873–8. doi: 10.1016/j.bbrc.2018.04.177. [DOI] [PubMed] [Google Scholar]
- 58.Bruick RK, McKnight SL A conserved family of prolyl-4-hydroxylases that modify HIF. Science. 2001;294:1337–40. doi: 10.1126/science.1066373. [DOI] [PubMed] [Google Scholar]
- 59.Kim SY, Yang EG Recent advances in developing inhibitors for hypoxia-inducible factor prolyl hydroxylases and their therapeutic implications. Molecules. 2015;20:20551–68. doi: 10.3390/molecules201119717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dopeso H, Jiao HK, Cuesta AM, et al PHD3 controls lung cancer metastasis and resistance to egfr inhibitors through TGFα. Cancer Res. 2018;78:1805–19. doi: 10.1158/0008-5472.Can-17-1346. [DOI] [PubMed] [Google Scholar]
- 61.Tang LR, Wu JX, Cai SL, et al Prolyl hydroxylase domain 3 influences the radiotherapy efficacy of pancreatic cancer cells by targeting hypoxia-inducible factor-1α. Onco Targets Ther. 2018;11:8507–15. doi: 10.2147/ott.S187615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Abdalla MY, Ahmad IM, Spitz DR, et al Hepatitis C virus-core and non structural proteins lead to different effects on cellular antioxidant defenses. J Med Virol. 2005;76:489–97. doi: 10.1002/jmv.20388. [DOI] [PubMed] [Google Scholar]
- 63.Nuhn P, Künzli BM, Hennig R, et al Heme oxygenase-1 and its metabolites affect pancreatic tumor growth in vivo . Mol Cancer. 2009;8:37. doi: 10.1186/1476-4598-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abdalla MY, Ahmad IM, Rachagani S, et al Enhancing responsiveness of pancreatic cancer cells to gemcitabine treatment under hypoxia by heme oxygenase-1 inhibition. Transl Res. 2019;207:56–69. doi: 10.1016/j.trsl.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 65.Seol SY, Kim C, Lim JY, et al Overexpression of endoplasmic reticulum oxidoreductin 1-α (ERO1L) is associated with poor prognosis of gastric cancer. Cancer Res Treat. 2016;48:1196–209. doi: 10.4143/crt.2015.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tanaka T, Kajiwara T, Torigoe T, et al Cancer-associated oxidoreductase ERO1-α drives the production of tumor-promoting myeloid-derived suppressor cells via oxidative protein folding. J Immunol. 2015;194:2004–10. doi: 10.4049/jimmunol.1402538. [DOI] [PubMed] [Google Scholar]
- 67.Gupta N, Park JE, Tse W, et al ERO1α promotes hypoxic tumor progression and is associated with poor prognosis in pancreatic cancer. Oncotarget. 2019;10:5970–82. doi: 10.18632/oncotarget.27235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kong F, Kong X, Du Y, et al STK33 promotes growth and progression of pancreatic cancer as a critical downstream mediator of HIF1α. Cancer Res. 2017;77:6851–62. doi: 10.1158/0008-5472.Can-17-0067. [DOI] [PubMed] [Google Scholar]
- 69.Chen ST, Kuo TC, Liao YY, et al Silencing of MUC20 suppresses the malignant character of pancreatic ductal adenocarcinoma cells through inhibition of the HGF/MET pathway. Oncogene. 2018;37:6041–53. doi: 10.1038/s41388-018-0403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ito S, Takahara Y, Hyodo T, et al The roles of two distinct regions of PINCH-1 in the regulation of cell attachment and spreading. Mol Biol Cell. 2010;21:4120–9. doi: 10.1091/mbc.E10-05-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eke I, Koch U, Hehlgans S, et al PINCH1 regulates Akt1 activation and enhances radioresistance by inhibiting PP1alpha. J Clin Invest. 2010;120:2516–27. doi: 10.1172/jci41078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huang C, Li Y, Li Z, et al LIMS1 promotes pancreatic cancer cell survival under oxygen-glucose deprivation conditions by enhancing HIF1A protein translation. Clin Cancer Res. 2019;25:4091–103. doi: 10.1158/1078-0432.Ccr-18-3533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen Y, Henson ES, Xiao W, et al Tyrosine kinase receptor EGFR regulates the switch in cancer cells between cell survival and cell death induced by autophagy in hypoxia. Autophagy. 2016;12:1029–46. doi: 10.1080/15548627.2016.1164357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ma J, Weng L, Jia Y, et al PTBP3 promotes malignancy and hypoxia-induced chemoresistance in pancreatic cancer cells by ATG12 up-regulation. J Cell Mol Med. 2020;24:2917–30. doi: 10.1111/jcmm.14896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pérez S, Pereda J, Sabater L, et al Pancreatic ascites hemoglobin contributes to the systemic response in acute pancreatitis. Free Radic Biol Med. 2015;81:145–55. doi: 10.1016/j.freeradbiomed.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 76.Chang Z, Gao M, Zhang W, et al Beta-elemene treatment is associated with improved outcomes of patients with esophageal squamous cell carcinoma. Surg Oncol. 2017;26:333–7. doi: 10.1016/j.suronc.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 77.Zou K, Tong E, Xu Y, et al Down regulation of mammalian target of rapamycin decreases HIF-1α and survivin expression in anoxic lung adenocarcinoma A549 cell to elemene and/or irradiation. Tumour Biol. 2014;35:9735–41. doi: 10.1007/s13277-014-2226-0. [DOI] [PubMed] [Google Scholar]
- 78.Jiang Z, Jacob JA, Loganathachetti DS, et al β-Elemene: Mechanistic studies on cancer cell interaction and its chemosensitization effect. Front Pharmacol. 2017;8:105. doi: 10.3389/fphar.2017.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liu Y, Jiang ZY, Zhou YL, et al β-elemene regulates endoplasmic reticulum stress to induce the apoptosis of NSCLC cells through PERK/IRE1α/ATF6 pathway. Biomed Pharmacother. 2017;93:490–7. doi: 10.1016/j.biopha.2017.06.073. [DOI] [PubMed] [Google Scholar]
- 80.Zhu J, Li B, Ji Y, et al β elemene inhibits the generation of peritoneum effusion in pancreatic cancer via suppression of the HIF1A VEGFA pathway based on network pharmacology. Oncol Rep. 2019;42:2561–71. doi: 10.3892/or.2019.7360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bronner C, Krifa M, Mousli M Increasing role of UHRF1 in the reading and inheritance of the epigenetic code as well as in tumorogenesis. Biochem Pharmacol. 2013;86:1643–9. doi: 10.1016/j.bcp.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 82.Hu Q, Qin Y, Ji S, et al UHRF1 promotes aerobic glycolysis and proliferation via suppression of SIRT4 in pancreatic cancer. Cancer Lett. 2019;452:226–36. doi: 10.1016/j.canlet.2019.03.024. [DOI] [PubMed] [Google Scholar]
- 83.Lang A, Grether-Beck S, Singh M, et al MicroRNA-15b regulates mitochondrial ROS production and the senescence-associated secretory phenotype through sirtuin 4/SIRT4. Aging (Albany NY) 2016;8:484–505. doi: 10.18632/aging.100905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Valkovskaya N, Kayed H, Felix K, et al ADAM8 expression is associated with increased invasiveness and reduced patient survival in pancreatic cancer. J Cell Mol Med. 2007;11:1162–74. doi: 10.1111/j.1582-4934.2007.00082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gao Y, Yu X, Zhang F, et al Propofol inhibits pancreatic cancer progress under hypoxia via ADAM8. J Hepatobiliary Pancreat Sci. 2019;26:219–26. doi: 10.1002/jhbp.624. [DOI] [PubMed] [Google Scholar]
- 86.Ma C, Guo Y, Zhang Y, et al PAFAH1B2 is a HIF1a target gene and promotes metastasis in pancreatic cancer. Biochem Biophys Res Commun. 2018;501:654–60. doi: 10.1016/j.bbrc.2018.05.039. [DOI] [PubMed] [Google Scholar]
- 87.Lei J, Ma J, Ma Q, et al Hedgehog signaling regulates hypoxia induced epithelial to mesenchymal transition and invasion in pancreatic cancer cells via a ligand-independent manner. Mol Cancer. 2013;12:66. doi: 10.1186/1476-4598-12-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Qin Y, Ma Z, Dang X, et al Effect of resveratrol on proliferation and apoptosis of human pancreatic cancer MIA PaCa-2 cells may involve inhibition of the Hedgehog signaling pathway. Mol Med Rep. 2014;10:2563–7. doi: 10.3892/mmr.2014.2511. [DOI] [PubMed] [Google Scholar]
- 89.Li W, Cao L, Chen X, et al Resveratrol inhibits hypoxia-driven ROS-induced invasive and migratory ability of pancreatic cancer cells via suppression of the Hedgehog signaling pathway. Oncol Rep. 2016;35:1718–26. doi: 10.3892/or.2015.4504. [DOI] [PubMed] [Google Scholar]
- 90.Lei J, Huo X, Duan W, et al α-Mangostin inhibits hypoxia-driven ROS-induced PSC activation and pancreatic cancer cell invasion. Cancer Lett. 2014;347:129–38. doi: 10.1016/j.canlet.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Onishi H, Yamasaki A, Kawamoto M, et al Hypoxia but not normoxia promotes Smoothened transcription through upregulation of RBPJ and Mastermind-like 3 in pancreatic cancer. Cancer Lett. 2016;371:143–50. doi: 10.1016/j.canlet.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 92.Onishi H, Morifuji Y, Kai M, et al Hedgehog inhibitor decreases chemosensitivity to 5-fluorouracil and gemcitabine under hypoxic conditions in pancreatic cancer. Cancer Sci. 2012;103:1272–9. doi: 10.1111/j.1349-7006.2012.02297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ables JL, Breunig JJ, Eisch AJ, et al Not(ch) just development: Notch signalling in the adult brain. Nat Rev Neurosci. 2011;12:269–83. doi: 10.1038/nrn3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhang H, Morisaki T, Nakahara C, et al PSK-mediated NF-kappaB inhibition augments docetaxel-induced apoptosis in human pancreatic cancer cells NOR-P1. Oncogene. 2003;22:2088–96. doi: 10.1038/sj.onc.1206310. [DOI] [PubMed] [Google Scholar]
- 95.Yamasaki A, Kameda C, Xu R, et al Nuclear factor kappaB-activated monocytes contribute to pancreatic cancer progression through the production of Shh. Cancer Immunol Immunother. 2010;59:675–86. doi: 10.1007/s00262-009-0783-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yamasaki A, Onishi H, Imaizumi A, et al Protein-bound polysaccharide-K inhibits hedgehog signaling through down-regulation of MAML3 and RBPJ transcription under hypoxia, suppressing the malignant phenotype in pancreatic cancer. Anticancer Res. 2016;36:3945–52. [PubMed] [Google Scholar]
- 97.Zhang J, Xu J, Dong Y, et al Down-regulation of HIF-1α inhibits the proliferation, migration, and invasion of gastric cancer by inhibiting PI3K/AKT pathway and VEGF expression. Biosci Rep. 2018;38:BSR20180741. doi: 10.1042/bsr20180741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Roviello G, Ravelli A, Polom K, et al Apatinib: A novel receptor tyrosine kinase inhibitor for the treatment of gastric cancer. Cancer Lett. 2016;372:187–91. doi: 10.1016/j.canlet.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 99.He K, Wu L, Ding Q, et al Apatinib promotes apoptosis of pancreatic cancer cells through downregulation of hypoxia-inducible factor-1α and increased levels of reactive oxygen species. Oxid Med Cell Longev. 2019;2019:5152072. doi: 10.1155/2019/5152072. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 100.Li CM, Liu ZC, Bao YT, et al Extraordinary response of metastatic pancreatic cancer to apatinib after failed chemotherapy: A case report and literature review. World J Gastroenterol. 2017;23:7478–88. doi: 10.3748/wjg.v23.i41.7478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fancy SP, Kotter MR, Harrington EP, et al Overcoming remyelination failure in multiple sclerosis and other myelin disorders. Exp Neurol. 2010;225:18–23. doi: 10.1016/j.expneurol.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 102.Freese JL, Pino D, Pleasure SJ Wnt signaling in development and disease. Neurobiol Dis. 2010;38:148–53. doi: 10.1016/j.nbd.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xiang J, Hu Q, Qin Y, et al TCF7L2 positively regulates aerobic glycolysis via the EGLN2/HIF-1α axis and indicates prognosis in pancreatic cancer. Cell Death Dis. 2018;9:321. doi: 10.1038/s41419-018-0367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Guo Q, Qin W DKK3 blocked translocation of β-catenin/EMT induced by hypoxia and improved gemcitabine therapeutic effect in pancreatic cancer Bxpc-3 cell. J Cell Mol Med. 2015;19:2832–41. doi: 10.1111/jcmm.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pourmorteza M, Rahman ZU, Young M Evofosfamide, a new horizon in the treatment of pancreatic cancer. Anticancer Drugs. 2016;27:723–5. doi: 10.1097/cad.0000000000000386. [DOI] [PubMed] [Google Scholar]
- 106.Limani P, Linecker M, Kron P, et al Development of OXY111A, a novel hypoxia-modifier as a potential antitumor agent in patients with hepato-pancreato-biliary neoplasms — Protocol of a first Ib/IIa clinical trial. BMC Cancer. 2016;16:812. doi: 10.1186/s12885-016-2855-3. [DOI] [PMC free article] [PubMed] [Google Scholar]