Abstract
A 70-year-old man presented to our vein clinic with intermittent and recurrent left testicular and groin pain, clinically resembling epididymo-orchitis. He had never had any genitourinary problems until contracting a severe flu-like illness in January 2020, strongly suspected to have been Covid-19. He had failed to respond on four separate occasions to antibiotics prescribed by his GP and had only responded on these occasions to aspirin. Duplex ultrasonography at our clinic showed thrombosis of the left testicular vein with venous collateral formation. The testicle itself showed mild oedema, but a reduced arterial flow supporting the pain to be secondary to thrombosis. Covid-19 is known to be associated with venous thromboembolic disease, but usually in patients sick enough to be hospitalised and particularly in those requiring intensive care. This man appears to have had a left testicular vein thrombosis secondary to relatively mild Covid-19 infection, as he did not require hospitalisation.
Keywords: Covid-19, thrombosis, gonadal vein, testicular vein, spermatic vein
Case
A 70-year-old man presented to our vein clinic in November 2020 with a history of intermittent and recurrent bouts of pain associated with his left testicle and groin. In January 2020, he had a severe febrile illness that started following a visit to Australia that had the clinical presentation of Covid-19. At that time, he had no access to a test for the virus to confirm the diagnosis and this was thought to be a severe influenza type illness. However, his wife and the two younger friends whom they were staying with, all developed a similar illness.
Generally, he was very fit and well. He had a body mass index (BMI) of 25.4, was a non-smoker and had no history of any venous thromboembolic disease, heart attack, stroke or diabetes. He was not on any regular medication.
The patient recovered from that acute illness without problems and shortly afterwards, developed a tender painful left testicle and epididymis, with pain extending into the left inguinal canal area. He had never had any previous episode of similar symptoms and had never had any previous genitourinary problems.
His General Practitioner diagnosed epididymo-orchitis and he was given a course of antibiotics that had no effect. However, starting regular aspirin reduced pain and discomfort.
Over the subsequent 9 months, he had intermittent recurrences of these symptoms. On three further occasions, he had courses of antibiotics for suspected epididymo-orchitis, none of which gave any improvement. The only symptomatic relief he got during an attack was by taking aspirin regularly, 600 mg qds for as long as the pain lasted.
In view of this atypical history, it was suggested he come to a venous clinic for duplex ultrasonography of his left testicle, scrotum, and testicular vein and artery.
On examination, the testicle had the normal lie with no ‘bell-clapper’ abnormality that might suggest intermittent torsion.
Duplex ultrasound of the left testicle showed mild oedema when compared to the right (Figure 1) but reduced arterial flow within the testicle itself. Duplex of the testicular vein showed thrombosis distally (Figure 2) with complete occlusion and minor venous collateral formation. The arterial inflow was present but reduced compared to the right side.
Figure 1.

Duplex ultrasound of the hilum of each testicle – right normal and left showing some local oedema (white arrows).
Figure 2.
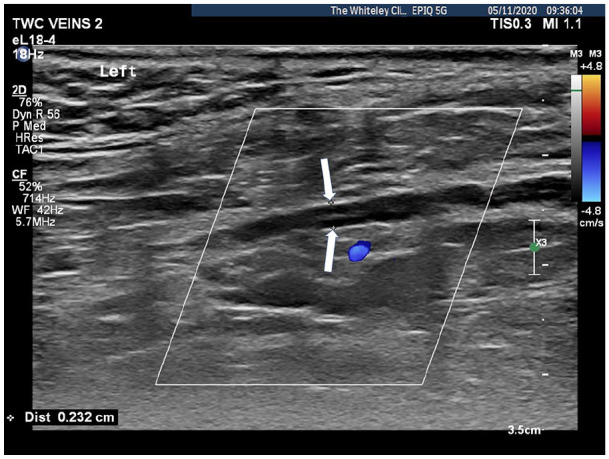
Duplex ultrasound showing thrombosed and left testicular vein with no flow (cursors showing reduced diameter of thrombosed vein shown by white arrows).
A diagnosis was made of testicular vein thrombosis, probably secondary to Covid-19 and he was referred to urology. He has subsequently undergone investigations for occult malignancy and none has been found.
His care under urological advice has been conservative. Six months after presentation, his testicular vein was still thrombosed and any discomfort relieved by aspirin.
Discussion
Testicular vein thrombosis is a very rare condition that was first described in 1903 (see Table 1). A literature search has identified 41 cases of assorted thromboses of the pampiniform plexus, spermatic vein and/or testicular vein. Five were in children, most were on the left and only two bilateral. It can be seen from Table 1 that before non-invasive imaging was widely available, surgical exploration and intervention was the norm. However, with the advent of non-invasive imaging, such thromboses are more often managed non-operatively mainly by anticoagulation or anti-inflammatory medication.
Table 1.
Table listing 41 reports cases of thromboses of the pampiniform plexus, spermatic vein and/or testicular vein.
| Age | Side | Symptom duration | Presenting symptoms | Associated factors | Investigations | Treatment | Outcome | Vein(s) involved | First author and journal |
|---|---|---|---|---|---|---|---|---|---|
| N/A | Left | N/A | Acute pain in scrotum | N/A | None | N/A | N/A | Spermatic vein | Senn NA. Surgical clinic. Clin Rev 1903;4:241–245 |
| N/A | N/A | ‘Sudden’ | Acute pain in Scrotum | N/A | None | “Excision” | N/A | Spermatic vein | Senn NA. Int Clin 1904;4:148–160 |
| 33 | Right | 3 weeks | Pain in testicle | Amoebic Dysentery | None | Conservative Management | Resolution | Pampiniform plexus | J.W. Tomb. Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 20, Issue 4, 25 November 1926, Pages 288–289 |
| 41 | Left | 5 weeks | Pain in testicle and swelling | None | None | Orchidectomy | N/A | Pampiniform plexus | McGavin D. The Lancet 1935; 226 (5842): 368–369 |
| 57 | Left | 4 weeks | Pain in testicle | 1 Stone weight loss | None | Orchidectomy | N/A | Pampiniform plexus | |
| 27 | Left | 16 h | Dull pain in testicle and inguinal region | Testicle Horizontal Lie | None | Exploration and biopsy of vein | N/A | Pampiniform plexus | Anseline P. Aust N Z J Surg. 1977 Dec;47(6):801–802 |
| 7 | Left | N/A | Pain groin, swollen cord, oedema scrotum | None | None before op | Exploration – Anti-inflammatory medication | Resolution | Pampiniform plexus | Coolsaet B. J Urol. 1980 Aug;124(2):290–291 |
| 10 | Left | N/A | Pain and oedema of scrotum | Previous testicular fixation | Venogram | Anti-inflammatory medication | Resolution | Pampiniform plexus | |
| 15 | Left | 11 days | Painful scrotal swelling | None | None | Excision of veins to external ring | N/A | Pampiniform plexus | |
| 44 | Right | Several hours | Tender swelling mid-scrotum | Playing baseball and tennis | None – Observed for 4 days | Excision thrombosed vein to internal ring | N/A | Pampiniform plexus | Rothman D. J Med Soc N J. 1981 Sep;78(10):681 |
| 33 | Left | 10 days | Inguinal pain | None | None | Excision thrombosed vein to internal ring | N/A | Spermatic vein | Vincent MP. Urology. 1981 Feb;17(2):175–176 |
| 33 | Left | Recent | Inguinal tenderness and mass | Varicocele | None – Observed for 1 week | Excision thrombosed varicocele and ligation | Resolution | Thrombosed varicocele | Roach R. J Urol. 1985 Aug;134(2):369–370 |
| 42 | Left | 1 week | Groin lump tender | None | Excretory urography (IVP) | Excision thrombosed veins | Left ischaemic testicle – Orchidectomy, then right spermatic vein thrombosis treated with anticoagulants | Spermatic vein | |
| 19 | Left | Hours | Groin pain | Vigorous exercise – rowing sit-ups | None | Excision thrombosed veins | Resolution | Spermatic vein | Isenberg JS. J Urol. 1990 Jul;144(1):138 |
| 23 | Left | 1 day | Painful bulging in left inguinal region | Heavy lifting boxes | Ultrasound | Excision thrombosed varicocele and ligation | Resolution | Thrombosed varicocele | Gleeson MJ. Br J Urol. 1992 Nov;70(5):567 |
| 43 | Left | During hospitalisation | Acute scrotal pain | Ischemic colitis and antiphospholipid syndrome | Doppler Ultrasound | Orchidectomy | N/A | Testicular vein and pampiniform plexus | Wu VH. J Ultrasound Med. 1995 Jan;14(1):57–59 |
| 6 | Right | 3 months | Swelling of testicle | None | Ultrasound | Exploration and biopsy of vein | 6 months later further episode | Pampiniform plexus | Campagnola S. Minerva Urol Nefrol. 1999 Sep;51(3):163–165. |
| 8 | Left | 24 h | Pain in abdomen and testicle | Henoch-Schoenlein purpura | Ultrasound | Steroids – Exploration at 2 weeks | Resolution | Spermatic veins | Diana A. J Pediatr Surg. 2000 Dec;35(12):1843. |
| N/A | N/A | N/A | N/A | Varicocele | None | Conservative Management | Resolution | Varicocele | Kleinclauss F. Prog Urol. 2001 Feb;11(1):95–96. |
| 28 | Left | 3 days | Pain in scrotum and inguinal region | None | Doppler Ultrasound | Oxerutin medication + rest – delayed varicocele ligation and vein excision | Resolution | Spermatic veins | Martino G. Chirurgia 2005 December;18(6):501–506. |
| 27 | Left | 2–3 h | Painful mass inguinal area | Lifting a patient | None | Exploration | Resolution | Pampiniform plexus | Hashimoto L. J Urol Nephrol. 2006;40(3):252–254. |
| 42 | Left | 7 days | Pleuritic chest pain – Pulmonary embolism | Contusion left inguinal regions 2 weeks before. Left cryptorchidism treated as infant | CT scan | Oral anticoagulation | Resolution | Spermatic vein | Castillo OA. Urol Int. 2008;80(2):217–218. |
| 40 | Right | 4 days | Abdominal pain | Terminal ileitis and thrombophilia | CT scan | Anti-inflammatory medication | Resolution | Testicular vein | Schwartz JH. J Urol. 2008 Sep;180(3):1124. |
| 33 | Left | 3 days | Acute pain in scrotum | Cycling | Duplex ultrasound | Conservative management | Resolution | Pampiniform plexus | Doerfler A. Prog Urol. 2009 May;19(5):351–352. |
| 21 | Left | Hours | Acute pain in scrotum | High intensity exercise in combat attire – Horizontal lie of testis | None | Exploration and biopsy of vein | 1 month later right pampiniform plexus thrombosis after exercise | Pampiniform plexus | Kayes O. Ann R Coll Surg Engl. 2010 Oct;92(7): W22–W23. |
| 28 | Left | 14 days | Left inguinal induration + abdominal pain + testicular pain | Intermittent left loin pain and Haematuria for years | Duplex ultrasound + CT scan | Excision of spermatic vein from renal vein caudally | Resolution | Thrombosed varicocele + spermatic vein secondary to nutcracker | Mallat F. Int J Case Rep Images 2014;5(7):519–523. |
| 43 | Right | 2 days | Scrotal pain and swelling | Absent Inferior Vena Cava and heterozygous factor V Leiden mutation | Ultrasound and venogram | Anticoagulation | Resolution | Thrombosed testicular vein | Chi AC. Urology. 2015 May;85(5): e39–e40. |
| 35 | Right | N/A | Testicular pain and swelling | Varicocele + heterozygous factor V Leiden mutation | Duplex ultrasound + MRI | Anticoagulation | Resolution | Thrombosed testicular vein + spermatic vein | Bolat D. Can Urol Assoc J. 2016 Sep-Oct;10(9–10): E324–E327. |
| 23 | Left | 2 days | Left testicular and groin pain – radiating to left flank | None | Ultrasound | Anti-inflammatory medication | Resolution | Pampiniform plexus | Tanner R. Ir Med J. 2016 Jan;109(1):347–348. |
| 29 | Right | 4 h | Testicular pain, low grade temperature and sweating | Possible trauma 2 days before. Age 8 left torsion and orchidopexy | Ultrasound | Anticoagulation + anti-inflammatory medication + antibiotics | Resolution | Pampiniform plexus | Caño-Velasco J, RRev Int Androl. 2018 Jan-Mar;16(1):38–41. |
| 39 | Bilat | 2 days | Scrotal pain and swelling | Protein C deficiency | Ultrasound + CT | Anticoagulation + antibiotics | 6 days later right gonadal vein thrombosis – Then resolution | Left varicocele and right testicular vein | Kamel K. African J Uro 2018, Vol 24 (1), 14–18. |
| 31 | Left | 20 days | Dull ache inguinal and scrotal areas | 8-h drive | Ultrasound + contrast enhanced ultrasound + CT | Excision of thrombosed vein | Resolution | Spermatic vein | Liu M. Am J Emerg Med. 2018 Dec;36(12):2339.e1–2339.e3. |
| 36 | Right | 24 h | Right flank pain then acute right inguinal and scrotal pain | Housework; ulcerative colitis; left orchidectomy 6 months earlier | Duplex ultrasound + CT | Exploration | Resolution | Spermatic vein | Murthy PB. Urology. 2018 Sep;119:32–34. |
| 54 | Left | 2 days | Left inguinal pain | None | Ultrasound | Anticoagulation + anti-inflammatory medication and venotonics | Resolution | Pampiniform plexus | Ouanes Y. Urol Case Rep. 2018 Jun 7;20:28–29. |
| 68 | Left | 1 week | Left scrotal pain | None | Duplex ultrasound | Exploration and removal of varicocele | Resolution | Varicocele | Raghavendran M. BMC Urol. 2018 May 8;18(1):34. |
| 40 | Left | 2 h acute – 6 months previous intermittent pain | Acute pain left scrotum | None | Duplex ultrasound | Exploration and removal of varicocele | Resolution | Varicocele | Robayna A. Urol Int. 2018;101(1):117–120. |
| 14 | Right | 4 days | Swelling and dull pain right inguinal and scrotal pain + fever | None | Duplex ultrasound | Right orchidectomy | Resolution | Testicular vein | Hussain JM. Urology. 2019 Aug;130:144–147. |
| 65 | Bilat | 1.5 months – severe 4 days | Swelling inguinal region bilaterally then upper scrotum | Labourer | Ultrasound | Left inguinal exploration | Resolution | Pampiniform plexus | Bakshi S. Surg Case Rep. 2020 Mar 5;6(1):47. |
| 50 | Left | Scrotal pain and swelling | None | Duplex ultrasound | Anticoagulation + antibiotics | Resolution | Pampiniform plexus | Lay Keat WO. Urol Case Rep. 2019 Sep 5;28:101000. | |
| 12 | Left | 3 days | Left testicular pain | Factor V Leiden heterozygous mutation; Nut-cracker syndrome suggested on ultrasound | Duplex ultrasound | Exploration then anticoagulation and antibiotics | Resolution | Pampiniform plexus | Pérez-Ardavín J. Cir Pediatr. 2020 Apr 1;33(2):99–101. |
| 55 | Left | 2 weeks | Scrotal induration and pain | None | Duplex ultrasound + CT | Exploration and excision of vein | Resolution | Spermatic vein | Petca RC. Chirurgia (Bucur). 2020 Jul-Aug;115(4):505–510. |
CT: computed tomography; MRI: magnetic resonance imaging; IVP: intravenous pyelogram. Please see text for other reports of less significance.
The presentation varied considerably but appears to be mainly acute testicular pain and swelling if the pampiniform plexus was involved (including varicocele), inguinal mass and pain if the spermatic vein in the cord was thrombosed, and flank pain with testicular pain without scrotal swelling if the testicular vein was thrombosed. However, this is a generalisation from reading the cases and making the table, but it is complicated by the terminology used by some authors. Some speak of the spermatic vein meaning the veins in the scrotum, some in the inguinal canal and at least one using the term to mean the vein connecting to the left renal vein.
As can also be seen in the table, most of the case reports show no obvious underlying cause, or simple causes such as exercise, exertion or local trauma. Some patients showed underling thrombophilic tendencies and three had intra-abdominal inflammatory conditions – amoebic dysentery, ischaemic colitis and ulcerative colitis. However, none mentioned intra-abdominal malignancy.
Interestingly, a study by Lenz and colleagues 1 comparing a series of 39 patients in their institution with reported testicular vein thrombosis between 1995 and 2015 with a selection of patients with deep vein thrombosis (DVT) reported 59% were associated with malignancy. However, in many of these cases, the testicular vein thrombosis was found as an incidental finding during staging of the malignancy, and once in the follow-up of an abdominal aortic aneurysm, and the thrombosis was not the presenting problem. There is little information as to the few who might have presented with the symptoms and signs of testicular vein thrombosis.
Previous reports of this condition have also often included testicular vein thrombosis in neonates secondary to renal vein or more extensive thromboses, which is clearly a completely different condition,2 –4 as is a reported case of a left renal vein thrombosis with retrograde flow down the testicular vein. 5
An increased incidence of venous thromboembolism has been reported in patients infected with Covid-19, secondary to thromboinflammation. 6 However, a published registry of 1114 patients with Covid-19 infection found increased thromboembolism in patients in intensive care and treated as inpatients, but no increased incidence of thromboembolism in those treated as outpatients. 7
The commonest site of venous thrombosis in Covid-19 patients appears to be in-situ thrombosis of the lungs 8 with DVT and superficial venous thrombosis being less common. 9 There have now been three cases reported of ovarian vein thrombosis secondary to Covid-19,10 –12 but we have not been able to find a report of testicular vein thrombosis yet.
Conclusion
We have reported a case of left testicular vein thrombosis causing intermittent attacks of pain and discomfort mimicking epididymo-orchitis following a febrile illness presumed to be Covid-19 in a 70-year-old man with no other underlying medical condition. Venous thromboembolism is known to be associated with Covid-19 infection, although usually in patients who are sick enough to be hospitalised and particularly those ill enough to be admitted to intensive care. In this case, this rare venous thrombosis has occurred in a man who did not require hospitalisation and who recovered from the acute illness without any other complication. The persistent, intermittent and recurrent pain he is getting from his left testicular vein thrombosis was the only sequela of the viral infection.
Footnotes
Author contributions: The study’s conception and design was done by O.A.B. and J.M.H.; analysis and interpretation by M.S.W., O.A.B. and J.M.H.; data collection by O.A.B. and J.M.H.; writing the manuscript by M.S.W.; and critical revision of the manuscript by M.S.W., O.A.B. and J.M.H.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iD: Mark S Whiteley  https://orcid.org/0000-0001-6727-6245
https://orcid.org/0000-0001-6727-6245
References
- 1. Lenz CJ, McBane RD, Cohoon KP, et al. Testicular vein thrombosis: incidence of recurrent venous thromboembolism and survival. Eur J Haematol 2018; 100(1): 83–87. [DOI] [PubMed] [Google Scholar]
- 2. Chapman S. The acute scrotum: a complication of cardiac catheterization. Br J Radiol 1988; 61(722): 162–164. [DOI] [PubMed] [Google Scholar]
- 3. Hagstrom JN, Walter J, Bluebond-Langner R, et al. Prevalence of the factor V Leiden mutation in children and neonates with thromboembolic disease. J Pediatr 1998; 133(6): 777–781. [DOI] [PubMed] [Google Scholar]
- 4. Maas C, Müller-Hansen I, Flechsig H, et al. Acute scrotum in a neonate caused by renal vein thrombosis. Arch Dis Child Fetal Neonatal Ed 2011; 96(2): F149–F150. [DOI] [PubMed] [Google Scholar]
- 5. Nana GR, Basra M, Maudgil DD, et al. Left renal vein thrombosis: a rare cause of acute scrotal pain. BMJ Case Rep 2014; 2014: bcr2013202237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schulman S, Hu Y, Konstantinides S. Venous thromboembolism in COVID-19. Thromb Haemost 2020; 120: 1642–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Piazza G, Campia U, Hurwitz S, et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19. J Am Coll Cardiol 2020; 76(18): 2060–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang L, Chen F, Bai L, et al. In situ pulmonary thrombosis in patients with COVID-19 pneumonia: different phenotypes may exist. Thromb Res 2020; 196: 541–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marone EM, Bonalumi G, Curci R, et al. Characteristics of venous thromboembolism in COVID-19 patients: a multicenter experience from Northern Italy. Ann Vasc Surg 2020; 68: 83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. DeBoer RE, Oladunjoye OO, Herb R. Right ovarian vein thrombosis in the setting of COVID-19 infection. Cureus 2021; 13(1): e12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Veyseh M, Pophali P, Jayarangaiah A, et al. Left gonadal vein thrombosis in a patient with COVID-19-associated coagulopathy. BMJ Case Rep 2020; 13(9): e236786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mohammadi S, Abouzaripour M, Hesam Shariati N, et al. Ovarian vein thrombosis after coronavirus disease (COVID-19) infection in a pregnant woman: case report. J Thromb Thrombolysis 2020; 50(3): 604–607. [DOI] [PMC free article] [PubMed] [Google Scholar]


