Abstract
For Chinese community pharmacists, there is a lack of guidance before and after the drug treatment process for community residents. This study aimed to investigate community pharmacists’ role in hypertension management. One hundred ninety-six hypertensive patients were randomly selected from the studied community. For patients in the intervention group, monthly meetings were scheduled with a community pharmacist. Patients in the non-intervention group received standard care from their physicians. In the intervention group, the percentage using information from pharmacists increased significantly, from 54.3% to 94.2% (P < .05). Awareness of self-management was also enhanced, with community self-management group attendance increasing from 53.4% to 77.7% (P < .05), but the non-intervention group did not change significantly. Hypertensive patients’ beliefs about community pharmacists also improved significantly. Hypertension status also showed a significant improvement, whereas for participants without intervention, it worsened over time. In addition to increasing knowledge regarding drug use, care provided by community pharmacists can also significantly improve blood pressure status. For those who did not receive intervention, a disproportionate level of health deterioration could be seen.
Keywords: community pharmacist, hypertension, role recognition
What do we already know about this topic?
Pharmacists play a significant role in chronic diseases management in community, however, the role of pharmacist is often neglected.
How does your research contribute to the field?
The practice in Shanghai showed that pharmacists in primary care institution were helpful in improving general beliefs, health management behaviors, and health indicators for patients with high blood pressure.
What are your research’s implications toward theory, practice, or policy?
It is necessary to strengthen the role of pharmacists in family doctor team in health management for chronic diseases.
Introduction
In 2016, the Global Burden of Disease Study showed that the disability-adjusted life years (DALY) caused by hypertension in the Chinese population were as high as 37.94, accounting for 12.0% of the total DALY and 63.5% of the total DALY caused by cardiovascular diseases; this meant that hypertension ranked first among the examined risk factors in terms of cardiovascular disease burden. 1 Although great progress has been made in the diagnosis and treatment of hypertension in recent years, there are also many problematic aspects of treatment using hypertension drugs that affect patients’ treatment compliance, persistence, and blood pressure (BP) control rate. The Chinese Health and Family Planning Commission has pointed out that problems with the use of drugs by Chinese residents includes overconsumption, the drug-drug interactions, and the use of non-long-acting antihypertensive drugs. Furthermore, the effect of primary medical care on hypertension management services in different parts of China varies substantially. The BP control rate is much higher in economically developed areas than in areas that are less economically developed.2,3
Noncompliance among patient groups has long been a key concern of medical and pharmaceutical professionals. The most significant factors in noncompliance are a lack of knowledge about prescribed drugs and their side effects and a lack of understanding about the consequences of not following a prescribed drug regimen. Offering disease-specific management education programs to patients has been highly effective in improving compliance with drug therapy. Previous studies have demonstrated that clinical pharmacy services have a significant impact on compliance and patient satisfaction, and might be ineffective on therapy outcomes.4,5
The responsibilities of pharmacists in most countries have changed from simple drug dispensing to pharmaceutical care centered on the safety and effectiveness of patients’ medications, and the role of clinical pharmacists has become increasingly prominent.6-11 However, in China, the role of community pharmacists is ambiguous. Since the introduction of medical reform in 2009, the Chinese government has put great efforts toward the improvement of primary medical services, with the aim of achieving the goal of a “Healthy China.” 12 In 2012, Shanghai took the lead in piloting the family doctor system, establishing a management model that centers on family doctors, supplemented by collaboration among health service personnel involved in nursing, public health, and health management. 13 Family doctors provide diagnosis and chronic disease management with the help from family nurses as assistants, public health physicians are responsible for health education, promotion, and major diseases screening, the work of pharmacists include drug distribution, supervision, management, and pharmaceutical consultation. Pharmaceutical care, which is led by community pharmacists, plays an important role in the drug treatment and health management of geriatric and chronic diseases such as hypertension. However, in the current family doctor team advocated by the Chinese government, there is a lack of guidance for pharmacists before and after the drug treatment process for community residents, which results in a complete lack or insufficient level of participation by community pharmacists.14,15 Among community members, there is a public perception of the role of pharmacists as limited to selling drugs in pharmacies.
This study aims to explore the effect of physician in family doctor team in hypertension management in Shanghai which might guide the practice of community pharmacist management in China and lead to the exploration of a new model to improve the community pharmacist system.
Methods
Study Design and Data Collection
This study was conducted in Beiwaitan community of Hongkou District in Shanghai from June 2017 to May 2018, which was selected as a pilot area for the family doctor system in 2016 and implemented the “2.0 Version” of the family doctor system in 2018. We recruited pharmacists as investigators, who have been trained by our research team. Based on previous studies, we calculated the sample size by PASS software (NCSS Statistical Software, 329 North 1000 East Kaysville, Utah 84037 USA), and the results turned out to be at least 66 people for each group. 16 Considering the drop out of the patients and the research funding, we decided to form a 226-peope-sample. We draw all high blood pressure patients from the community’s electronic health profile as a sampling box, in which high blood pressure patients were marked as doctors’ key management objects. Two hundred twenty-six hypertension patients were randomly selected from this sampling box, then 113 patients were selected randomly selected as intervention group while the rest were turned out to be control group automatically. The family doctors of those selected patients help our investigators to contact those patients. Only a small part of patients (about 10%) refused to participate, and we replaced them by similar patient recommended by the responsible family doctor.
The inclusion criteria for the patients were (1) having hypertension, confirmed by the World Health Organization-International Society of Hypertension guidelines for hypertension; (2) being at least 18 years old, without cognitive dysfunctions and with barrier-free communication; and (3) participating in the survey voluntarily and signing the informed consent form. In the process, 196 patients who were tracked successfully and have completed our research, including 103 intervention group members and 93 non-intervention group members.
Interventions
The intervention group received the intervention, which consisted of community pharmacists providing them with pharmaceutical care over 12 months. The non-intervention group received only routine medical services, including issuance of drugs and drug consultations. Referring to previous experience conducted by our team before this study and the literature,17,18 the following pharmacist-led intervention was formulated in this study. First, the pharmacists were required to fill in the BP measurement form for participants in the intervention group. These BP measurements were to be taken at the same time of day. Second, in the intervention group, drug card designed by pharmacists, were used to track the drug name, dose, and method and time of drug, and patients were encouraged to complete record sheets daily, which was thought to be helpful in self-management for patients. Third, pharmacists visited the patients once a month to check the medication type, medicinal dosage, frequency of medication, et al; to correct any errors in a timely fashion; and to provide guidance. Fourth, pharmacists obtained the medication status of patients once a month through phone calls or social software, and they provided patients with personalized suggestions in case of problems. And patients could contact pharmacists with phone calls or social software as well. Fifth, pharmacists invited specialists from tier-2 and tier-3 hospitals to conduct health promotion and education for patients in the intervention group.
Measures
The present study evaluated the recognition and participation of community pharmacists in hypertension management in a community health service center (CHSC) in Hongkou District of Shanghai, China. Patients’ knowledge source and self-management were assessed before and after an intervention by community pharmacists, and changes in hypertension health indicators were also measured.
A questionnaire was designed for this study. The questionnaire was then reviewed by an expert group of family doctors. There were 4 parts to the questionnaire: (1) general information: age, gender, occupation, educational level, individual history of hypertension, and family history of hypertension; (2) health data: BP levels and other health indicators like HbA1C and total cholesterol were tested twice at the beginning and end of the study period; (3) management subject and measures: management subject included family doctor contract management, community self-management group, family members, or not managed at all. Community self-management group is a self-management group set up spontaneously by patients with high blood pressure. Management measures included visit hospital regularly, participate in the hypertensive self-management group, CHSC follow-up, and others; and (4) attitudes toward pharmacists at follow-up.
Statistics and Data Analysis
Community pharmacists conducted 1 baseline visit and 1 post-intervention visit to assess patients’ cognition, attitudes, and health indicators, with monthly follow-up for the intervention group with the aid of family doctors and media channels including social media and telephones. The difference of the sections to determine the patients’ sources about receiving hypertensive knowledge, self-management measures, changes in BP levels, and other health indicators were assessed using Student’s t-test. The internal consistency for the sections to determine the participants’ beliefs about pharmacists was examined by Chi-square test. All data were collected by trained, blinded research assistants during scheduled home visits with EpiData 3.1 software, and Stata 13.0 software was used for the statistical analysis.
Ethics Statement
This study was approved by the Academic Ethics Committee of Shanghai Pudong Institute for Health Development. All of the respondents provided written participant consent to participate in this study.
Results
Characteristics of the Study Population
Table 1 showed the gender distribution of patients was balanced, with women making up a slightly higher percentage than men. The patients were all over 50 years old, and more than half (53.6%) were aged 61 to 70 years. As for educational level, nearly the same percentage of study participants had secondary education or high school/technical school as their highest level of education; together, these 2 categories accounted for more than three-quarters of the participants. Given that the retirement age in China is from 50 to 60, we determined that 95.4% of participants enrolled in this study had already retired. Duration of hypertension ranged from 1 to 10 years (36.2%) to >40 years (5.6%), and nearly all the participants had a family medical history of hypertension (94.4%).
Table 1.
Characteristics of the Respondents (n = 196).
| Frequency | Percentage (%) | Intervention | Non-intervention | P-value | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 86 | 43.9 | 38 | 48 | .51 |
| Female | 110 | 56.1 | 55 | 55 | |
| Age (years) | .01 | ||||
| 51-60 | 19 | 9.7 | 7 | 13 | |
| 61-70 | 105 | 53.6 | 44 | 61 | |
| ≥71 | 72 | 36.7 | 42 | 29 | |
| Degree of education | .01 | ||||
| Primary school or below | 19 | 9.7 | 8 | 11 | |
| Secondary education | 76 | 38.8 | 27 | 49 | |
| High school/technical school | 72 | 36.7 | 40 | 32 | |
| College/university | 27 | 13.8 | 17 | 10 | |
| Postgraduate or above | 2 | 1.0 | 1 | 1 | |
| Working condition | .36 | ||||
| The emeritus and retired | 187 | 95.4 | 90 | 93 | |
| In-service staff | 4 | 2.0 | 3 | 1 | |
| Freelance | 4 | 2.0 | 4 | ||
| Others | 1 | 0.5 | 1 | ||
| Duration of hypertension (years) | .61 | ||||
| 1-10 | 71 | 36.2 | 35 | 37 | |
| 11-20 | 66 | 33.7 | 26 | 40 | |
| 21-30 | 32 | 16.3 | 18 | 14 | |
| 31-40 | 16 | 8.2 | 10 | 6 | |
| >40 | 11 | 5.6 | 4 | 6 | |
| Family medical history of hypertension | .89 | ||||
| Yes | 185 | 94.4 | 88 | 97 | |
| No | 11 | 5.6 | 5 | 6 | |
Sources of Knowledge Regarding Hypertension Medication
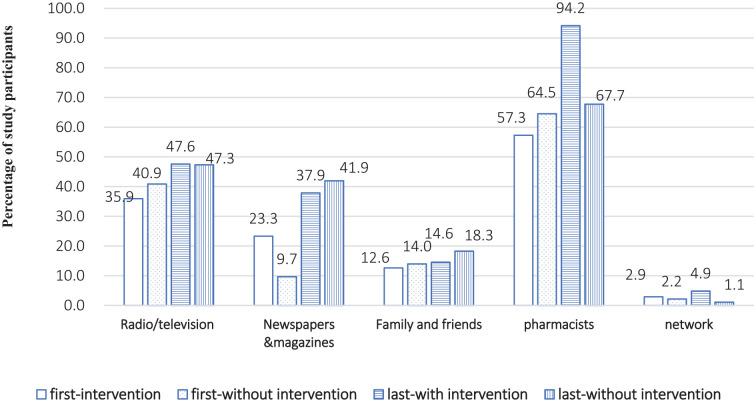
The largest percentages of participants reported that community pharmacists were the most preferred source of knowledge of hypertension and anti-hypertension medication. In the intervention group, nearly 60% used information from community pharmacists at the beginning of the follow-up. After 12-month intervention, this percentage had increased dramatically, reaching 94.2%. For the non-intervention group, the percentage obtaining hypertension knowledge from pharmacists had changed slightly (from 64.5% to 67.7%) (see Figure 1).
Figure 1.
Hypertension and antihypertensive knowledge source.
Note. In the first visit, there is a significant difference between 2 groups in high blood pressure patients obtaining hypertension and antihypertensive knowledge source through newspapers; in the second visit, 2 groups who received knowledge through pharmacists have a significant difference. The rest of the knowledge acquisitions have no significant difference in 2 groups.
Changes in Patients’ Hypertension Management Method and Measures
Study participants were able to provide their own unique responses and even multiple responses regarding their management subject and measures (see Table 2). For both groups, the community self-management group was the most commonly preferred management method at the last visit (77.7% in the intervention group and 63.4% in the non-intervention group, P < .05). The percentage of participants who had signed up with a family doctor team was more than 4 times higher after the intervention than before the intervention. It was inspiring to find that no one in the intervention group was not managing their chronic disease at the last visit, while 1.1% for non-intervention group. Both groups showed a significant difference between the 2 visits in the use of contract management and the community self-management group. However, only for the intervention group, there were significant differences between the 2 visits in the use of family management (family members’ supervision and management of patients).
Table 2.
Self-Management of Hypertension in the Intervention and Non-Intervention Groups at the First and Last Visits.
| Dimension | Way | Survey time | With intervention (%) | Without intervention (%) | t Test |
|---|---|---|---|---|---|
| Management principal | FD contract management | First visit | 11.7 | 15.1 | −0.698 (P = .485) |
| Last visit | 49.5 | 37.6 | 1.688 (P = .091) | ||
| t Test | −6.469 (P < .001) | −3.616 (P < .001) | |||
| Community self-management group | First visit | 53.4 | 36.6 | 2.403 (P = .016) | |
| Last visit | 77.7 | 63.4 | 2.201 (P = .028) | ||
| t Test | −3.791 (P < .001) | −3.806 (P < .001) | |||
| Family management | First visit | 44.7 | 51.6 | −0.975 (P = .330) | |
| Last visit | 59.2 | 39.8 | 2.771 (P = .006) | ||
| t Test | −2.114 (P = .035) | 1.631 (P = .103) | |||
| Do not manage | First visit | 5.8 | 3.2 | 0.882 (P = .378) | |
| Last visit | 0.0 | 1.1 | −1.005 (P = .314) | ||
| t Test | 2.524 (P = .012) | 1.014 (P = .311) | |||
| Management measures | Visit the hospital regularly | First visit | 63.1 | 60.2 | 0.416 (P = .678) |
| Last visit | 95.2 | 76.3 | 3.846 (P < .001) | ||
| t Test | −6.156 (P < .001) | −2.400 (P = .016) | |||
| Participate in the hypertensive self-management group | First visit | 18.5 | 10.8 | 1.541 (P = .123) | |
| Last visit | 38.8 | 36.6 | 0.328 (P = .743) | ||
| t Test | −3.322 (P < .001) | −4.346 (P < .001) | |||
| CHSC follow-up | First visit | 29.1 | 41.9 | −1.884 (P = .060) | |
| Last visit | 68.0 | 45.2 | 3.299 (P = .001) | ||
| t Test | −6.502 (P < .001) | −0.444 (P = .658) | |||
| Others | First visit | 3.9 | 5.4 | −0.495 (P = .619) | |
| Last visit | 1.0 | 0.0 | 1.005 (P = .315) | ||
| t Test | 1.364 (P = .173) | 2.299 (P = .021) |
In terms of the management measures, after 12-month intervention, the proportion for intervention group participating in the hypertension community self-management group doubled, and 95.2% visited hospital regularly (an increase of 32.04%). For the non-intervention group, the percentage in community self-management group also increased significantly (from 10.8% to 36.6%, P < .001), but the percentage regularly visiting the hospital increased less than that in the intervention group (an increase of 16.12%). In the intervention group, after 12-month intervention, there were significant differences in the percentages of participants who used the hypertension community self-management group (P < .001) and CHSC follow-up (P < .001).
General Beliefs about Community Pharmacists
Overall, at the baseline visit, 30.1% of the intervention participants and 54.8% of the non-intervention participants reported negative or neutral general beliefs related to the necessity of community pharmacists participating in drug therapy (see Table 3). More than half of the intervention participants agreed that pharmacists had professional knowledge and skills, whereas 63.4% of the non-intervention participants had a neutral attitude regarding the professional knowledge and skills of community pharmacists. Regarding the comprehensive ability of community pharmacists, 58.3% of the intervention participants and only 35.5% of the non-intervention participants showed positive attitudes. The attitudes of patients in the intervention and non-intervention groups differed significantly on all 5 items (P < .05). In contrast, at the post-intervention visit, beliefs about community pharmacists for both groups had shifted in a positive direction. The percentages of intervention participants who agreed or strongly agreed for all items reached 100% or near 100%.
Table 3.
General Beliefs about Community Pharmacists (n = 196).
| Item | Survey time | Intervention |
Non-intervention |
χ2 test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Disagree (%) | Neutral (%) | Agree (%) | Strongly agree (%) | Disagree (%) | Neutral (%) | Agree (%) | Strongly agree (%) | |||
| It is necessary for community pharmacists to participate in drug therapy | First visit | 5 (4.9) | 26 (25.2) | 47 (45.6) | 25 (24.3) | 5 (5.4) | 46 (49.5) | 23 (24.7) | 19 (20.4) | 14.129 (P = .003) |
| Last visit | 0 (0.0) | 0 (0.0) | 13 (12.6) | 90 (87.4) | 2 (2.2) | 65 (69.9) | 25 (26.9) | 1 (1.1) | 157.734 (P < .001) | |
| χ2 test | 87.006 (P < .001) | 20.821 (P < .001) | ||||||||
| The professional knowledge and skills of community pharmacists can make a significant difference in the treatment of diseases | First visit | 3 (2.9) | 33 (32.0) | 53 (51.5) | 14 (13.6) | 5 (5.4) | 59 (63.4) | 20 (21.5) | 9 (9.7) | 23.403 (P < .001) |
| Last visit | 0 (0.0) | 0 (0.0) | 24 (23.3) | 79 (76.7) | 2 (2.2) | 62 (66.7) | 29 (31.2) | 0 (0.0) | 143.335 (P < .001) | |
| χ2 test | 92.352 (P < .001) | 12.013 (P = .007) | ||||||||
| I am very satisfied with the service attitude of the community pharmacist | First visit | 0 (0.0) | 15 (14.6) | 78 (75.8) | 10 (9.7) | 2 (2.2) | 26 (28.0) | 57 (61.3) | 8 (8.6) | 7.951 (P = .047) |
| Last visit | 0 (0.0) | 1 (1.0) | 16 (15.5) | 86 (83.5) | 0 (0.0) | 42 (45.2) | 51 (54.8) | 0 (0.0) | 143.239 (P < .001) | |
| χ2 test | 113.310 (P < .001) | 14.098 (P = .003) | ||||||||
| I am very satisfied with the medication guidance and education of the community pharmacist | First visit | 3 (2.9) | 36 (35.0) | 54 (52.4) | 10 (9.7) | 4 (4.3) | 58 (62.4) | 22 (23.7) | 9 (9.7) | 18.356 (P < .001) |
| Last visit | 1 (1.0) | 0 (0.0) | 26 (25.2) | 76 (73.8) | 1 (1.1) | 64 (68.8) | 28 (30.1) | 0 (0.0) | 143.928 (P < .001) | |
| χ2 test | 97.451 (P < .001) | 11.815 (P = .008) | ||||||||
| I am very satisfied with the comprehensive ability of the community pharmacist | First visit | 2 (1.9) | 41 (39.8) | 50 (48.5) | 10 (9.7) | 2 (2.2) | 58 (62.4) | 25 (26.9) | 8 (8.6) | 10.993 (P = .012) |
| Last visit | 1 (1.0) | 0 (0.0) | 27 (26.2) | 75 (72.8) | 1 (1.1) | 56 (60.2) | 36 (38.7) | 0 (0.0) | 132.119 (P < .001) | |
| χ2 test | 97.909 (P < .001) | 10.352 (P = .016) | ||||||||
Changes in Health Indicators
Following the 2017 United States hypertension guidelines 2017 Hypertension Clinical Practice Guidelines, we classified the study participants into normal, elevated, Stage 1, and Stage 2 groups (see Figure 2). Overall, in the intervention group, the percentage of people with normal BP was almost 5 times higher after the 12-month intervention, increasing from 8.7% to 43.7%. The percentage of participants categorized as Stage 1 or Stage 2 decreased, especially for the Stage 2 group, which was reduced by more than half. Notably, there was a slight increase in the elevated group (from 8.7% to 23.3%, P = .004). In contrast, in the non-intervention group, there was a slight increase in the percentages of people classified as Stage 1 (from 28% to 32.3%, P = .523) and Stage 2 (from 34.4% to 45.2%, P = .132). However, the percentages of participants classified in the normal and elevated groups decreased.
Figure 2.
Changes in hypertension status in the intervention and non-intervention groups (n1 = 103, n2 = 93).
We also examined 7 other health indicators: HbA1C, total cholesterol, triglycerides, HDL, LDL, uric acid, and creatinine (see Table 4). After the 12-month intervention, there was a slight increase in the percentage of healthy people in the intervention group in terms of 5 indicators, including total cholesterol (from 57.3% to 61.2% classified as healthy, P = .570), triglycerides (from 57.3% to 58.3%, P = .888), HDL (from 91.3% to 93.2%, P = .603), uric acid (from 73.8% to 80.58%, P = .244), and creatinine (from 63.1% to 74.8%, P = .069), although these changes were not statistically significant. In the non-intervention group, only LDL showed a small increase in the percentage of respondents classified as healthy (from 53.8% to 55.9%, P = .768), whereas the percentages classified as healthy for the other 6 factors all decreased-especially HbA1C and creatinine, which decreased by 15.06% and 19.35%, respectively.
Table 4.
Changes in Other Health Indicators (n = 196).
| Item (proportion of healthy population %) | With intervention | Without intervention | t Test |
|---|---|---|---|
| HbA1C | |||
| First visit | 43.7 | 64.5 | −2.991 (P = .003) |
| Last visit | 42.7 | 49.5 | −0.948 (P = .344) |
| t Test | 0.141 (P = .888) | 2.098 (P = .036) | |
| Total cholesterol | |||
| First visit | 57.3 | 64.5 | −1.041 (P = .298) |
| Last visit | 61.2 | 61.3 | −0.017 (P = .986) |
| t Test | −0.569 (P = .570) | 0.456 (P = .648) | |
| Triglyceride | |||
| First visit | 57.3 | 59.2 | −0.264 (P = .792) |
| Last visit | 58.3 | 52.7 | 0.783 (P = .434) |
| t Test | −0.141 (P = .888) | 0.888 (P = .375) | |
| HDL | |||
| First visit | 91.3 | 93.6 | −0.607 (P = .544) |
| Last visit | 93.2 | 83.9 | 2.051 (P = .040) |
| t Test | −0.520 (P = .603) | 2.111 (P = .035) | |
| LDL | |||
| First visit | 51.5 | 53.8 | −0.322 (P = .747) |
| Last visit | 46.6 | 56.1 | −1.308 (P = .191) |
| t Test | 0.698 (P = .485) | −0.295 (P = .768) | |
| Uric acid | |||
| First visit | 73.8 | 75.3 | −0.238 (P = .812) |
| Last visit | 80.6 | 73.1 | 1.238 (P = .216) |
| t Test | −1.165 (P = .244) | 0.335 (P = .738) | |
| Creatinine | |||
| First visit | 63.1 | 74.2 | −1.686 (P = .092) |
| Last visit | 74.8 | 54.8 | 2.971 (P = .003) |
| t Test | −1.281 (P = .069) | 2.816 (P = .005) | |
Discussion
This study aimed to explore the role of community pharmacists in hypertension management from the patient’s perspective and to contribute to improving the community pharmacist system in China. The study suggested that pharmaceutical care led by community pharmacists can play an important role in the drug treatment and health management of geriatric and chronic diseases for hypertensive patients.
Our analysis of the changes in knowledge sources used by the respondents showed that the percentage of respondents acquiring health knowledge from pharmacists increased significantly after the intervention. We found that there were 2 main reasons for this change. First, regular visits by community pharmacists and irregular online medication guidance strengthened the awareness of appropriate medication among patients with hypertension. Second, through various activities such as lectures on medication knowledge, patients were provided with professional medication guidance and counseling services, which increased their medication knowledge. As Xi et al 15 argued, to provide quality pharmaceutical care, pharmacists should be free to go beyond their traditional drug sales activities to solve the actual needs of their patients. In particular, community pharmacists need to transform their role from that of “retailer” to “health care supporter.” 19 The pharmacist-led community health education model has the potential to increase opportunities for hypertensive patients to obtain health education.
During the baseline visit, the patients’ self-management of hypertension was weak, but their awareness of self-management was significantly enhanced after the intervention. The number of patients who managed their disease by signing up with pharmacists was 4 times higher after the intervention, whereas the number of patients who were not managing their illness decreased to 0 in the intervention group. In addition, the number of participants in the self-management group also increased, indicating that, in communities where pharmacists have heavy workloads and are therefore unable to pay close attention to patients with hypertension, self-management groups could be actively promoted as a complementary practice. Other studies have also indicated that self-management of chronic diseases has the potential to improve health status and to reduce hospitalization.20,21 In future practice, hypertension patients’ awareness of disease management should be strengthened, and practical resources—especially social support—should be developed to support communication between pharmacists and patients.
After a 12-month intervention by community pharmacists, hypertensive patients’ satisfaction with community pharmacists’ service attitude, comprehensive ability, and medication guidance and education improved significantly. Perception of professional knowledge and skills of community pharmacists also improved. These findings are consistent with the conclusions of several previous studies.22-24 Most community-dwelling patients with hypertension in China are older adults with poor physical health who lack pharmaceutical knowledge and have weak awareness regarding appropriate and safe drug use. Through pharmaceutical education, mainly in the form of health lectures taught by specialists from tier-2 and tier-3 hospitals, and the regular supervision and management of patients’ use of drugs, community pharmacists have improved the appropriateness and safety of patients’ drug use. Furthermore, by showing a patient-centered service attitude through providing personalized services, as well as taking the initiative to provide door-to-door pharmaceutical care, the intervention examined in the present study narrowed the distance between pharmacists and patients and improved patients’ general beliefs about community pharmacists. A previous study found that, to enhance patients’ recognition of pharmacists, it is crucial for pharmacists to communicate with patients about their use of products other than drugs prescribed to them, and to try to make themselves approachable so that patients find it easy to talk to them. 25
The results of the present study showed that, after a 12-month intervention by community pharmacists, the percentage of patients with normal BP increased significantly, and other relevant health indicators also improved. Other studies have suggested that pharmacist intervention programs result in a significant reduction in BP and an increase in the proportion of patients with controlled hypertension.17,26,27 However, in practice, the role of pharmacists is vague in China, and patients’ participation and recognition are low, which hinders pharmacists from playing their potential role in health management. Under the current policy, the responsibilities and requirements of community pharmacists in China are unclear, and this situation should be improved. To facilitate the transformation of the role of pharmacists, policy makers should recognize the important role of community pharmacists on health management for the patients with non-communicable diseases.
The present study should be considered in light of its limitations. Firstly, we did not consider patients treatment history when including patients as such information were not available. Secondly, this study took place in Shanghai, and, to our knowledge, this type of intervention has not been implemented in other parts of China. Further studies are needed to evaluate this study with larger populations. Thirdly, to be convenient, we replaced the respondents who refused to participate in this study by the patients recommended by the family doctor, which might be the reason for the attitude difference in the baseline. Fourthly, a wider range of factors, such as healthcare access, have not been considered in this study, which might be effective ones. Additionally, the duration of our study was limited, so future interventions should be followed over longer periods of time.
Conclusion
In conclusion, in addition to increasing the knowledge regarding drugs among patients with hypertension, community pharmacists can also significantly improve the BP status and other health indicators of these patients. On the basis of this study’s results, it appears that pharmacists can play an active role in the treatment and management of hypertension. For the study participants who did not receive the intervention, a disproportionate level of health deterioration could clearly be seen at 1-year follow-up.
Supplemental Material
Supplemental material, sj-pdf-1-inq-10.1177_00469580211020874 for Community Pharmacist Services for Hypertensive Patients: A Novel Practice in Shanghai, China by Qian Liu, Xiaoyan Zhu, Mei Shen, Jianping Wu, Shuqin Chen, Zhongzhuang Wang, Wenya Yu, Jianwei Shi, Jiaoling Huang and Zhaoxin Wang in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
The authors would like to acknowledge all the patients and pharmacists who participated in this study.
Footnotes
Author Contributions: JLH and ZXW conceived and designed this study. QL wrote the manuscript. JPW, SQC, and MS managed the data collection. ZZW analyzed the data. WYY and JWS contributed to revisions to the manuscript. XYZ participated in the modification of the manuscript. All authors reviewed and approved the final version.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Natural Science Foundation of China (71904145, 71774116, 71804128), the National Key Research and Development Program of China (SQ2018YFC130057), the Shanghai Municipal Planning Commission of Science and Research Fund (201740202), and the Shanghai Jiao Tong University China Hospital Development Institute 2019 Local High-level University Hospital Management Special Project (CHDI-2019-C-01).
Ethical Approval: This study protocol was approved by the Academic Ethics Committee of Shanghai Pudong Institute for Health Development (Protocol Number PDWSL2013-1). Both verbal and written consent was sought from all study participants before data collection.
ORCID iDs: Qian Liu  https://orcid.org/0000-0003-4082-6176
https://orcid.org/0000-0003-4082-6176
Jiaoling Huang  https://orcid.org/0000-0003-1975-3937
https://orcid.org/0000-0003-1975-3937
Supplemental Material: Supplemental material for this article is available online.
References
- 1. GBD 2016 Mortality Collaborators. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1084-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang JL, Xu XG, Wang JZ, et al. Application analysis of antihypertensive drugs in hypertensive population in a community in Shanghai. Chin J Gen Pract. 2010;9:603-606. [Google Scholar]
- 3. Yu YY, Fan Q, Lian YS, et al. Investigation on hypertension control rate and related factors in urban communities in Jiangsu. Jiangsu Prev Med. 2012;23:46-47. [Google Scholar]
- 4. Lip GY, Beevers DG. Doctors, nurses, pharmacists and patients—the rational evaluation and choice in hypertension (REACH) survey of hypertension care delivery. Blood Press Suppl. 1997;6:6-10. [PubMed] [Google Scholar]
- 5. Alsuwaidan S, Malone DC, Billups SJ, Carter BL, for the IMPROVE Investigators. Characteristics of ambulatory care clinics and pharmacists in veterans affairs medical centers. Am J Health Syst Pharm. 1998;55:68-72. [DOI] [PubMed] [Google Scholar]
- 6. Reeder TA, Mutnick A. Pharmacist versus physician-obtained medication histories. Am J Health Syst Pharm. 2008;65:857-860. [DOI] [PubMed] [Google Scholar]
- 7. Dunn SP, Birtcher KK, Beavers CJ, et al. The role of the clinical pharmacist in the care of patients with cardiovascular disease. J Am Coll Cardiol. 2015;66(21):29-39. [DOI] [PubMed] [Google Scholar]
- 8. American College of Clinical Pharmacy, McBane SE, Dopp AL, Abe A, et al. Collaborative drug therapy management and comprehensive medication management—2015. Pharmacotherapy. 2015;35:e39-e50. [DOI] [PubMed] [Google Scholar]
- 9. Asche SE, O’Connor PJ, Dehmer SP, et al. Patient characteristics associated with greater blood pressure control in a randomized trial of home blood pressure telemonitoring and pharmacist management. J Am Soc Hypertens. 2016;10:873-880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mills KT, Obst KM, Shen W, et al. Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients: a systematic review and meta-analysis. Ann Intern Med. 2018;168:110-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kislan MM, Bernstein AT, Fearrington LR, Ives TJ. Advanced practice pharmacists: a retrospective evaluation of the efficacy and cost of ClinicaL Pharmacist PractitionErs managing ambulatory Medicare patients in North Carolina (APPLE-NC). BMC Health Serv Res. 2016;16:607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tan X, Zhang Y, Shao H. Healthy China 2030, a breakthrough for improving health. Glob Health Promot. 2018;26(4):96-99. [DOI] [PubMed] [Google Scholar]
- 13. Huang JL, Jiang ZY, Zhang T, et al. Which matters more for medication adherence among disabled people in Shanghai, China: family support or primary health care? Inquiry. 2019;56:004695801988317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fang Y, Yang S, Zhou S, Jiang M, Liu J. Community pharmacy practice in China: past, present and future. Int J Clin Pharm. 2013;54:520-528. [DOI] [PubMed] [Google Scholar]
- 15. Xi XY, Huang YK, Lu QN, Ung C, Hu H. Community pharmacists’ opinions and practice of pharmaceutical care at chain pharmacy and independent pharmacy in China. Int J Clin Pharm. 2019;41:478-487. [DOI] [PubMed] [Google Scholar]
- 16. Lei Y. Evaluation of the effect of community health education on patients with hypertension. J Clin Exp Med. 2012;11(15):1234-1236. [Google Scholar]
- 17. Chabot I, Moisan J, Grégoire JP, Milot A. Pharmacist intervention program for control of hypertension. Ann Pharmacother. 2003;37:1186-1193. [DOI] [PubMed] [Google Scholar]
- 18. Di Palo KE, Kish T. The role of the pharmacist in hypertension management. Curr Opin Cardiol. 2018;33:1. [DOI] [PubMed] [Google Scholar]
- 19. Mossialos E, Courtin E, Naci H, et al. From “retailers” to health care providers: transforming the role of community pharmacists in chronic disease management. Health Policy. 2015;119(5):628-639. [DOI] [PubMed] [Google Scholar]
- 20. Warren-Findlow J, Seymour RB, Huber LRB. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37:15-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Perez A. Self-management of hypertension in Hispanic adults. Clin Nurs Res. 2011;20:347-365. [DOI] [PubMed] [Google Scholar]
- 22. Whelton PK, Carey RM, Aronow WS, Casey DE, Wright JT. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2017;71:213-221. [DOI] [PubMed] [Google Scholar]
- 23. Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2003;22:1533-1540. [DOI] [PubMed] [Google Scholar]
- 24. Perrault E, Beal J. Patients’ knowledge about pharmacists, technicians, and physicians. Am J Health Syst Pharm. 2019;79:1420-1425. [DOI] [PubMed] [Google Scholar]
- 25. Oshima S, Senoo K, Negishi A, et al. Identification of the discrepancies between pharmacist and patient perception of the pharmacist’s role as an advisor on drug therapy based on social science theory. Biol Pharm Bull. 2015;39:313-322. [DOI] [PubMed] [Google Scholar]
- 26. Tobari H, Arimoto T, Shimojo N, et al. Physician-pharmacist cooperation program for blood pressure control in patients with hypertension: a randomized-controlled trial. Am J Hypertens. 2010;23:1144-1152. [DOI] [PubMed] [Google Scholar]
- 27. McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN). Arch Intern Med. 2008;168:2355-2361. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-inq-10.1177_00469580211020874 for Community Pharmacist Services for Hypertensive Patients: A Novel Practice in Shanghai, China by Qian Liu, Xiaoyan Zhu, Mei Shen, Jianping Wu, Shuqin Chen, Zhongzhuang Wang, Wenya Yu, Jianwei Shi, Jiaoling Huang and Zhaoxin Wang in INQUIRY: The Journal of Health Care Organization, Provision, and Financing