Abstract
A 63-year-old right-handed man was admitted to our hospital after sustaining a traumatic right-sided subdural hematoma, subarachnoid hemorrhage, and temporal lobe hemorrhagic contusion. He was managed non-operatively and discharged without any neurologic deficits. Two weeks later he presented with worsening headaches and altered sensorium. Imaging studies showed that the patient had developed a cerebral abscess at the site of his intracerebral hemorrhage. The abscess was surgically resected, and the patient was treated with antibiotics with complete resolution of symptoms. This case illustrates the importance of timely recognition of a rare complication of intracranial hemorrhage, and the utility of MR spectroscopy.
Keywords: brain abscess, central nervous system infections, trauma, nervous system, imaging, techniques
Introduction
Cerebral abscess is a well-known complication of a surgically-managed intracerebral hemorrhage (ICH); however, it is exceptionally rare to develop an abscess after a non-operated ICH. Here we present a case of a patient who developed a cerebral abscess at the site of his non-operated traumatic ICH.
Case Description
A 63-year-old right-handed Caucasian male sustained a right-sided subdural hematoma, subarachnoid hemorrhage, and temporal lobe hemorrhagic contusion after a fall from his bicycle with head strike. Initial unenhanced CT of the head showed a multi-compartmental hemorrhage with mild edema surrounding the ICH (Figure 1A and B). No skull fractures were visualized. The patient was managed non-operatively and completed 7 days of levetiracetam for seizure prophylaxis. He was discharged home with no neurological deficits 2 days after presentation.
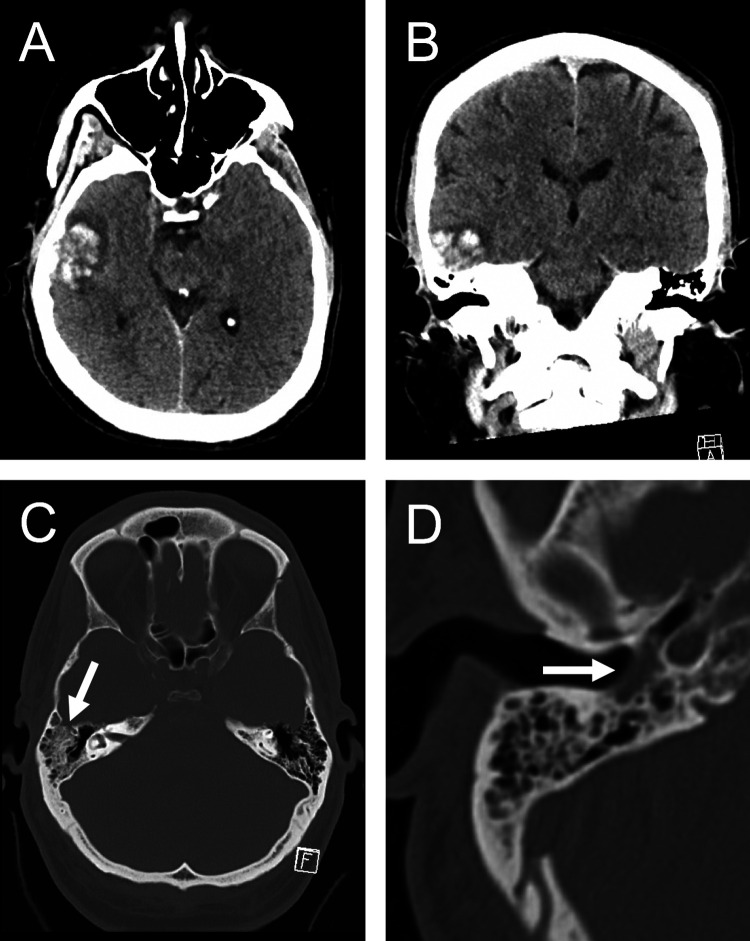
Figure 1.
Axial (A) and coronal (B) unenhanced CT of the head showing an acute right lateral temporal hemorrhagic contusion. Though no skull fracture was visualized, partial opacification of the right mastoid air cells (C, arrow) and right tympanic cavity (D, arrow) by fluid suggests possible injury to adjacent bone.
The patient was seen in clinic a week after discharge and complained of intermittent headaches. Two weeks later he presented to the emergency department with worsening headaches and altered sensorium. Unenhanced CT of the head at this time showed markedly increased edema in the right temporal lobe. MRI of the brain demonstrated a rim-enhancing lesion with internal diffusion restriction in the location of the prior hemorrhagic contusion (Figure 2). MR perfusion showed no associated elevation in blood volume, and MR spectroscopy of the lesion showed reduced N-acetyl aspartate and elevated lipid and lactate peaks within the fluid collection, a pattern consistent with intracerebral abscess. The patient underwent surgical resection of the abscess and Fusobacterium nucleatum, an oropharyngeal commensal organism, was isolated. The patient was treated with ceftriaxone and metronidazole for 8 weeks followed by amoxicillin-clavulanic acid and had complete resolution of headaches and altered sensorium.
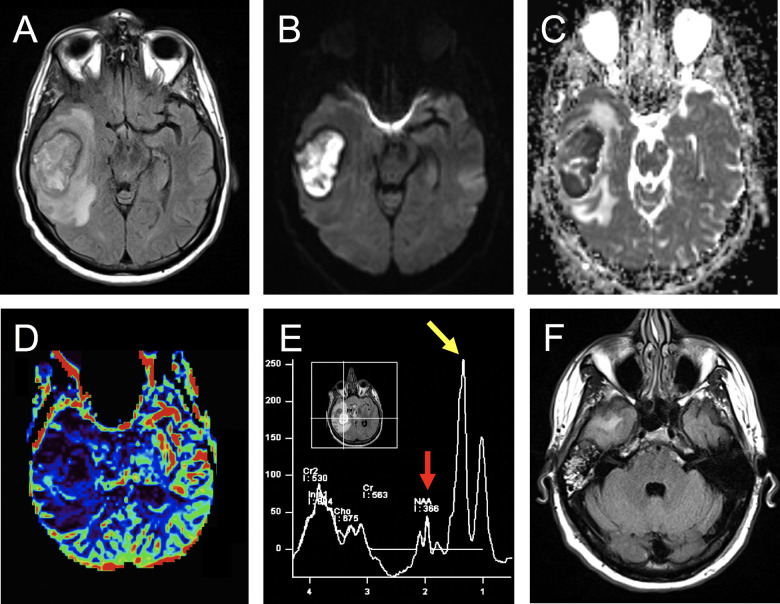
Figure 2.
Brain MRI. Axial T2-FLAIR image (A) shows interval development of a large and well-circumscribed heterogeneous iso-to-hyperintense mass in the location of the recent hemorrhagic contusion, with a rim of T2 hypointensity (hemosiderin) and a larger surrounding area of T2 hyperintensity representing vasogenic edema. This edema produces sulcal effacement laterally and medialization of the right uncus. DWI (B) and ADC (C) images show restricted diffusion within the mass. Axial MR perfusion (D) shows no elevation in cerebral blood volume associated with the right temporal mass (red/yellow = high blood volume, blue = low blood volume). Single-voxel spectroscopy of the right temporal lesion (E) shows reduction in N-acetyl aspartate (red arrow, resonance at 2.0 ppm chemical shift) and a highly elevated lactate peak (yellow arrow, resonance at 1.3 ppm chemical shift). Axial T2 FLAIR image (F) shows persistent partial opacification of the right mastoid air cells.
Discussion
It is very rare for a cerebral abscess to develop spontaneously at the site of a non-surgical ICH. When it does occur, it is usually the result of spread of either contiguous or distant foci of infection. 1 In retrospect, the patient’s initial CT showed partial opacification of the right mastoid air cells and tympanic cavity (Figure 1C and D). It should be assumed that all trauma patients with opacified mastoid air cells have a temporal bone fracture until proven otherwise. 2 We suspect this patient may have had contiguous spread of infection related to an occult temporal bone fracture. Review of the literature shows abscess formation beginning 0 to 20 weeks after initial ICH. Patients usually present with a fever, headache, and other signs of systemic infection (e.g., leukocytosis, elevated inflammatory markers). 1,3- 8 This patient developed a fever after an acute exam decline on the second day of his second hospital admission (16 days post-trauma).
This case highlights the importance of early identification of cerebral abscess as a potential early or late complication of non-surgical ICH. The mortality rate of cerebral abscess is not well documented but is likely declining as more sophisticated diagnostic imaging modalities become routinely available. 9,10 This patient’s MRI showed a contrast-enhancing lesion with internal diffusion restriction and surrounding edema. Given the late-subacute age of the hematoma, these findings could have represented the expected evolution of his ICH, however, the patient’s clinical course and the degree of edema were concerning for a progressive process such as an abscess or necrotic tumor. MR spectroscopy was utilized and displayed lesion markers that were more suggestive of an abscess, with reduced N-acetyl aspartate and elevated lipid and lactate peaks within the fluid collection. After the cerebral abscess was identified in our patient, he was immediately taken for surgical resection of the abscess and antibiotics were initiated. The patient had complete resolution of headaches and altered sensorium.
The patient provided informed consent to allow details of hospital stays and treatments to be used in this case report.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Joshua P. Klein  https://orcid.org/0000-0001-7685-2523
https://orcid.org/0000-0001-7685-2523
References
- 1. Liu K, Yang C, Zhang Y, Yuan X, Xiao H, Xi B. Brain abscess following intracerebral hemorrhage in a patient with pneumonia. J Craniofac Surg. 2016;27(8):e773–e775. [DOI] [PubMed] [Google Scholar]
- 2. Zayas JO, Feliciano YZ, Hadley CR, Gomez AA, Vidal JA. Temporal bone trauma and the role of multidetector CT in the emergency department. Radiographics. 2011;31(6):1741–1755. [DOI] [PubMed] [Google Scholar]
- 3. Nakai K, Yamamoto T, Yasuda S, Matsumura A. Brain abscess following intracerebral haemorrhage. J Clin Neurosci. 2006;13(10):1047–1051. [DOI] [PubMed] [Google Scholar]
- 4. Inamasu J, Kagami H, Nakamura Y, Saito R, Niimi M, Ichikizaki K. Brain abscess developing at the site of preceding intracerebral hemorrhage. J Neurol. 2002;249(2):221–223. [DOI] [PubMed] [Google Scholar]
- 5. Muzumdar D, Jhawar S, Goel A. Brain abscess: an overview. Int J Surg. 2011;9(2), 136–144. [DOI] [PubMed] [Google Scholar]
- 6. Thomas SG, Moorthy RK, Rajshekhar V. Brain abscess in a non-penetrating traumatic intracerebral hematoma: case report and review of literature. Neurol India. 2009;57(1):73–75. [DOI] [PubMed] [Google Scholar]
- 7. Siatouni A, Mpouras T, Boviatsis EJ, Gatzonis S, Stefanatou M, Sakas D. Brain abscess following intracerebral haemorrhage. J Clin Neurosci. 2007;14(10):986–989. [DOI] [PubMed] [Google Scholar]
- 8. Seydoux CH, Francioli P. Bacterial brain abscesses: factors influencing mortality and sequelae. Clin Infect Dis. 1992;15(3):394–401. [DOI] [PubMed] [Google Scholar]
- 9. Rosenblum ML, Hoff JT, Norman D, Weinstein PR, Pitts L. Decreased mortality from brain abscesses since advent of computerized tomography. J Neurosurg. 1978;49(5):658–668. [DOI] [PubMed] [Google Scholar]
- 10. Tseng JH, Tseng MY. Brain abscess in 142 patients: factors influencing outcome and mortality. Surg Neurol. 2006;65(6):557–562. [DOI] [PubMed] [Google Scholar]