Abstract
Status migrainosus (SM) is a subtype of migraine defined by migraine lasting >72 hours and is difficult to treat in clinical practice. Magnesium is commonly used in the treatment of migraine. We conducted a retrospective cohort study to determine if length of admission was associated with IV magnesium therapy in patients with SM. We reviewed the charts of all patients admitted to a large military treatment facility from October 2013 to December 2018 with the admission diagnosis of migraine. There were 333 patients that were reviewed and 141 met the inclusion criteria. Nearly half of patients received IV magnesium therapy with routine care (46.8%, n = 66). IV magnesium therapy was not associated with length of admission (58 hours (IQR 25.5, 86) compared to 42 hours (IQR 25.5, 80.5) respectively, p = 0.47). Of the cases without Neurology consultation, patients who received magnesium therapy (n = 5) had numerically shorter admission but this difference did not meet statistical significance (n = 12) (17 hours (IQR 13.75, 31.25) versus 24.5 hours (IQR 15.25, 58.75), p = 0.0534). This study contributes to the limited pool of available data on the treatment of SM. Prospective research is needed to study magnesium therapy in patients with prolonged migraine.
Keywords: status migrainosus, magnesium, healthcare costs, prolonged migraine
Introduction
Migraine headache is a common clinical condition affecting 12% of the global population and is among the world’s leading cause of disability. 1 Status migrainosus (SM) is a subtype of migraine defined by the International Headache Society (IHS) as a migraine lasting >72 hours. 1 Status migrainosus is sparsely referenced in the medical literature and the prevalence is not well established. Abortive migraine treatments are most efficacious if used at the first sign of impending migraine, making SM particularly difficult to treat. 2 One retrospective review in a French tertiary-care center showed status migrainosus was encountered in only 3% of patients and is thought to be a rare complication of migraine associated with stress, sleep deprivation, and menstruation. 3 -5 Unfortunately, relapse is common, and many go on to develop chronic migraine. 4,5 The clinical heterogeneity and lack of universally effective treatment makes this entity particularly difficult to treat.
Magnesium is a therapy commonly used in the treatment of migraine and supplementation has been shown to be safe in adults. 6 -12 A variety of mechanisms have been proposed to account for the benefit of magnesium supplementation in migraine. Some theories suggest that low levels of magnesium may propagate the migraine cascade including the release of substance P, cerebral vasospasm, and mitochondrial dysfunction. 6,10 -13 Several studies have demonstrated the benefit of magnesium supplementation in the preventive treatment of migraine. A study of 81 patients with migraine demonstrated a significant decrease in the duration and frequency of migraines after prophylactic magnesium supplementation compared to controls (p = 0.03). 10-11 A follow on study of 69 patients showed no significant difference in migraine duration between patients treated with magnesium supplement or placebo (20% versus 23.5%, respectively). 12 The Canadian Headache Society recommends 600 mg of elemental magnesium daily for migraine prophylaxis, but recommends against its use for the acute treatment of migraine due to lack of evidence to support its efficacy. 14 The American Academy of Neurology (AAN) gives a level B recommendation (probably effective) for its use as a preventative therapy. 15 The AAN does note evidence to support the use of IV magnesium therapy in the acute treatment of migraine with aura. 16 Magnesium is often used as an adjuvant migraine treatment combined with other acute (triptans, etc) and preventive therapies (beta blockers, anti-epileptics, etc). 16 Though quality randomized controlled studies are lacking, the limited data available supports the use of IV magnesium therapy in the treatment of SM. 17,18 A retrospective analysis of patients with SM who were administered IV magnesium therapy in an outpatient infusion center were found to have a statistically significant decrease in reported pain score after treatment. 18 Given the paucity of evidence to guide treatment of status migrainosus, we set out to determine if the use of IV magnesium therapy in patients with status migrainosus was associated with length of hospital admission. We selected this as our study end point because (1) it is an objective data point that can be used to compare patients and (2) it serves as a surrogate for clinical improvement such that patients can further manage their attack at home.
Methods
Study Design
We performed a retrospective cohort study by chart review of all patients admitted to a large military treatment facility from October 2013 to December 2018 with the admission diagnosis of migraine or status migrainosus. The initial list of patients was generated by searching for all patients admitted during the indicated time frame with an admission diagnosis of migraine or status migrainosus which later corresponded with the following ICD10 codes: G43.0, G43.1, G43.4, G43.5, G43.7, G43.8, G43.9. All records were manually reviewed by at least 1 author to determine if the inclusion/exclusion criteria were met. Duration of headache in hours at time of presentation was based on documentation in the admission history and physical. Age, gender, length of admission, and whether the Neurology service was consulted during the patient’s admission was recorded for each case. The total dose of IV and oral magnesium administered during hospitalization was calculated for each patient given therapy. Pain Severity Scale (VAS) rating (using a 1-10 scale, where 1 was the least severe and 10 was the most severe) was recorded (1) on admission, (2) after magnesium therapy, and (3) at discharge when it was in the medical record. Only a small proportion of patients had this data point recorded in their medical record, so it was ultimately not used in our analysis. We instead used hours of hospital duration as a surrogate for clinical improvement such that patients were able to further manage their attack at home. Whether aura was or was not present was also recorded, but this too was documented in a minority of charts and not included in our analysis.
Study Definitions
Status migrainosus was defined by the most recent guidelines provided by the International Headache Society Classification (ICHD-3) as an unremitting, debilitating migraine attack lasting longer than 72 hours with or without aura. We also followed the definition of migraine with and without aura per ICHD-3 guidelines. 1 Routine care was defined by the primary team as the medication(s) selected with the indication of migraine. Length of admission was measured in hours and calculated based on the bedside nurse’s documentation in the electronic medical record. Time in the emergency department was not included in the length of admission.
Inclusion and Exclusion Criteria
Patients 18 to 65 years old with an admission diagnosis of migraine or status migrainosus were included in the chart review. If the patient met the above definition of SM at time of admission, they were included in the analysis. Patients (1) given magnesium for another indication (i.e. hypomagnesemia, i.e. serum concentration <1.6 mg/dL) (2) diagnosed with another headache subtype, (3) diagnosed with a headache secondary to another etiology (i.e subdural hematoma), or (4) admitted to the hospital for a primary diagnosis other than migraine were excluded from the study. Patients seen and discharged from the emergency department were not included in the study.
Oversight
Brooke Army Medical Center Institutional Review Board granted the study exempt status because it was less than minimal risk. IRB Number C.20-19126e.
Statistical Methods
Categorical Data were summarized using percentages and analyzed using Chi Squared Test. Medians and Inter-quartile Range (IQR) as well as 95% confidence intervals were used as summary statistics for continuous variables (length of admission and age) and were analyzed using the nonparametric Wilcoxon’s Test due to low sample size and observed skewness of the data. Significance for results was established when p-values were less than 0.05. Due to the degree of heterogeneity in magnesium dosing, both in amount and frequency, we did not complete a dose response analysis as it was felt to be underpowered. In attempt to remain consistent with testing and given the low sample size, nonparametric testing was used for age rather than t tests. All statistical analysis was performed using JMP v13.2 (SAS Corp, Cary NC).
Results
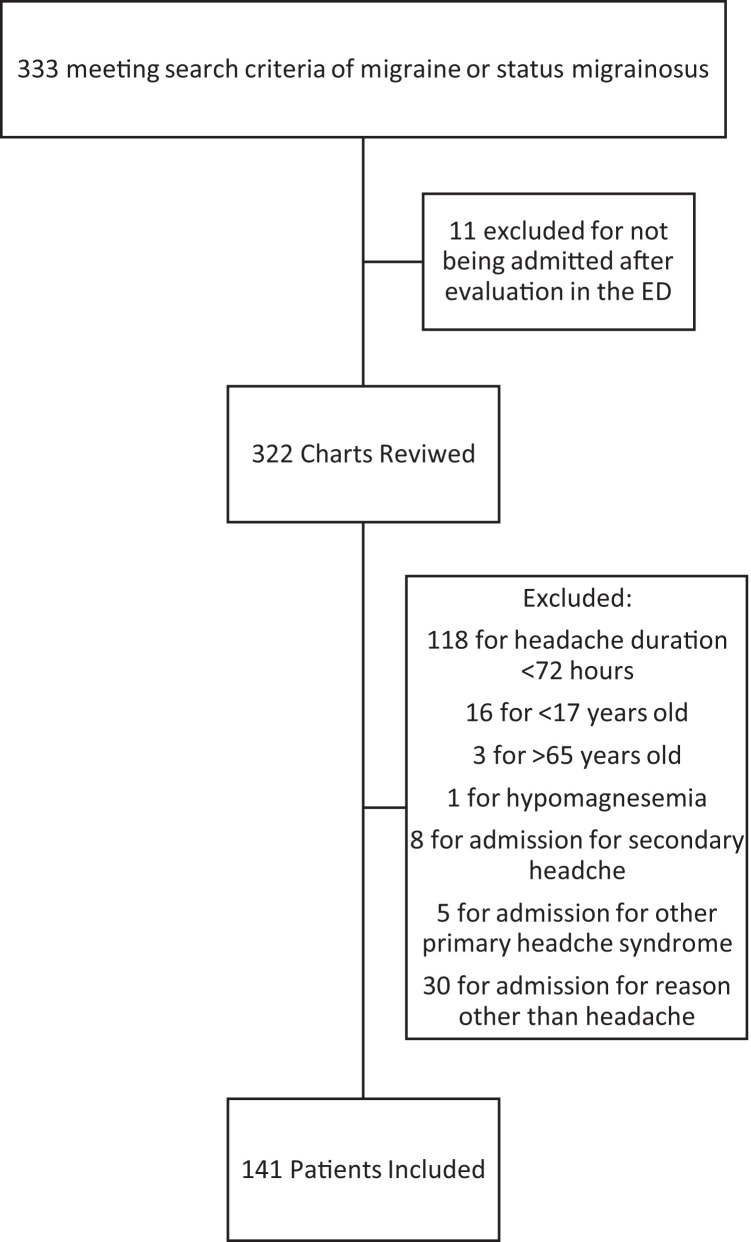
There were 333 patients admitted with the diagnosis of migraine and 141 met both inclusion and exclusion criteria (Figure 1). Our cohort was primarily female (88.7%, n = 125/141) and the median age was 39 years old (IQR 30, 47). There was no significant difference in median age between patients not treated (40 years old, IQR 30, 48) and treated (38 years old, IQR 31, 47) with magnesium. The median duration of migraine prior to admission in all patients was 168 hours (IQR 96, 336) and length of admission was 45.5 hours (IQR 25.5, 83.5). In our cohort, 44% (n = 66) presented with an attack longer than a week prior to admission. There was no significant difference in length of migraine prior to admission between patients treated and not treated with magnesium (p = 0.26). Of those who were not treated with magnesium, 84% (n = 63) had Neurology consultation compared to 91% of treated patients (n = 60) (p = 0.22). Nearly half of all patients (46.8%, n = 66) were treated with magnesium. Of those treated, the median magnesium dose was 2000 mg (IQR 2000, 4000), with 57.6% (n = 38) receiving 2 grams or less and one patient receiving greater than 10 grams (1.5%, n = 1). Table 1 shows the characteristics of the cohort.
Figure 1.
Flow diagram of patient inclusion and exclusion.
Table 1.
Patient Characteristics.
| Inclusion Criteria Met | 141 | ||
| Total Patients with Neurology Consultation | 123 (87.2% (80.7%, 91.8%)) | ||
| Total Patients Treated with Magnesium | 66 (46.8% (38.8%, 55.0%)) | ||
| Magnesium Administered | |||
| No | Yes | p-val | |
| All (n) | 75 (53.2%) | 66 (46.8%) | |
| Male (n) | 5 (6.7%) | 11 (16.7%) | 0.06 |
| 95% CI | (3%, 15%) | (10%, 27%) | |
| Median Age (years) (IQR) | 40 (30, 48) | 38 (31, 47) | 0.76 |
| 95% CI | (36.9, 42.2) | (36.3, 41,3) | |
| Median Hosp LOS (hours) (IQR) | 58 (25.5, 86) | 42 (25.5, 80.5) | 0.47 |
| 95% CI | (52.8, 72.8) | (48.3, 74.9) | |
| Neurology Consult (n) | 63 (84%) | 60 (91%) | 0.22 |
| 95% CI | (74%, 91%) | (82%, 96%) | |
| Duration of Migraine Prior to Admission (hours) (n) | |||
| <96 | 36 (48%) | 26 (39%) | 0.26 |
| 95% CI | (37%, 59%) | (29%, 51%) | |
| 97 to 168 | 25 (33%) | 20 (30%) | |
| 95% CI | (24%, 45%) | (21%, 42%) | |
| >168 | 14 (19%) | 20 (30%) | |
| 95% CI | (11%, 29%) | (21%, 42%)) | |
There was no significant difference in length of stay (LOS) in patients not treated and treated with magnesium (58 hours (IQR 25.5, 86) compared to 42 hours (IQR 25.5, 80.5) respectively, p = 0.47). Length of stay was shorter among those who received IV magnesium for both patients with neurology consultation and those without neurology consultation, but neither comparison met statistical significance. Cases with Neurology consultation had a significantly longer median length of admission compared to cases without consultation (55 hours (IQR 62) versus 23 hours (IQR 35.6) respectively, p ≤ 0.0001). Length of stay was further stratified by whether or not the Neurology service consulted on the case. Of the cases without Neurology consultation, patients who received magnesium therapy (n = 5/18) had a shorter mean length of admission compared to those who did not, though this did not meet statistical significance (n = 12/18) (17 hours (IQR 17.75) versus 24.5 hours (IQR 43.5) respectively, p = 0.0534). Length of admission was not associated with magnesium treatment in patients with Neurology consultation who did (n = 60/123) and did not (n = 63/123) receive IV magnesium (42.25 hours (IQR 30, 86) versus 60 hours (IQR 27.75, 89.5) respectively, p = 0.37). Nearly half of patients with Neurology consultation were given IV magnesium (48.78%, n = 60/123), while only a third of patients without Neurology consultation were given IV magnesium (33.33%, n = 6/18). In all patients, magnesium was used as an adjuvant therapy combined with routine treatment directed by the primary general internal medicine or Neurology team. Figure 2 demonstrates the study results.
Figure 2.
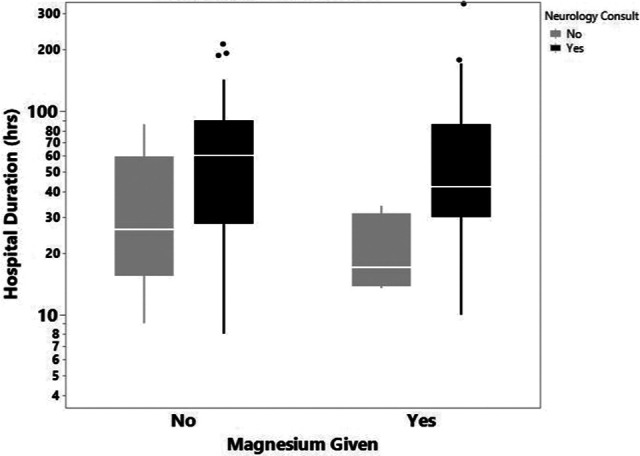
Hospital duration based on magnesium treatment in patients with and without neurology consultation.
It should be noted that some patients in our cohort received magnesium at scheduled intervals (for example, they received 2 grams of IV magnesium daily) while others had a single treatment. The most common dose was 2 grams IV magnesium given a single time (34.8%, n = 23/66), though there was significant variability between patients. Interestingly, magnesium therapy was administered more commonly in the second half of the study than the first. Between October 2013 and May 2016, 34.5% (29/84) of patients received magnesium compared to 64.9% (37/57) of patients between June 2016 and December 2018.
Discussion
We conducted a retrospective cohort study to determine if IV magnesium was associated with length of admission in patients admitted for SM. If a correlation were found, it could support the routine use of magnesium in patients hospitalized for SM. The majority of our patients were female, the median age was 39 years old, and all had access to primary and emergency medical care through the military medical system. We feel this sample is a reasonable representation of migraine sufferers in a specialty clinic. 3,18 Consistent with a previous study that demonstrated SM often persists far longer than the 72 hours, 44% (n = 66) of our cohort presented with an attack longer than a week prior to admission. 3 The length of hospital admission in our study was similar to a previous retrospective review of patients admitted with SM, where the median length of stay was 3 days (IQR 2, 4) and 9.3% (n = 402) had a stay 6 days of longer. 19 We found no statistical difference in duration of admission in SM patients treated and not treated with IV magnesium (42 hours (IQR 25.5, 80.5) compared to 58 hours (IQR 25.5, 86) respectively, p = 0.47). Subgroup analysis based on Neurology consultation demonstrated that treatment with IV magnesium in patients without Neurology consultation trended toward shorter hospital length of stay, though not statistically significant (p = 0.0534). The majority of patients in the early years of the study did not receive magnesium therapy, while those in the later years nearly universally received therapy. This difference reflects the growing understanding and utilization of magnesium supplementation in the treatment of migraine.
Though our results did not show a significant reduction in admission length, we feel the use of IV magnesium may be still reasonable in certain patients given the low risk profile and benefit in certain patients. 14,18 It is possible SM severe enough to warrant inpatient admission may be refractory to magnesium therapy and that length of admission is not sensitive to detect subtle changes in the clinical improvement. The medical literature on SM is sparse and limited data is available to guide treatment. Beyond the primary objectives, our study also contributes to the available data regarding patient demographics and clinical course of SM. Prospective research is needed to determine the most effective total dose, frequency and overall efficacy of magnesium in patients with SM.
Our study was not without limitations. IV magnesium was used as an adjunct to other first line migraine therapies (anti-epileptics, anti-emetics, etc) in our study, making it difficult to determine the contribution of magnesium alone. First line therapies were selected by the patient’s primary team and drug selection was highly heterogeneous between patients. Unfortunately, we were not able to determine the rational for drug selection due to limitations of the medical record and were unable to control for differences. Further, conclusions about our observations were complicated by the heterogeneity of patient presentation and the variation in total magnesium administered. These variables reflect the lack of singular approach or definitive algorithm to treat SM and speaks to the complexity of managing patients with prolonged migraine. Length of admission is an imperfect measure of therapy effectiveness and ultimately complicates retrospective review. There are multiple unrelated factors such as co-occurring medical conditions and logistics related to patient discharge that could confound this measure, which may have falsely prolonged admission. Whether or not a patient was on prophylactic magnesium therapy prior to admission was another confounder we were not able to address. Patients on prophylactic magnesium therapy may respond differently than patients not on therapy, and we were unable to compare these two subgroups. Incorrect coding of the admission diagnosis, which we used to generate our cohort, is a possible source of bias to note. We could have potentially missed a small group of eligible patients and ultimately altered our results. Neurology consultation itself may have prolonged length of admission and falsely altered the results. Further, standard of care may have changed over the course of our review (for example, more patients receiving magnesium in the second half of the study compared to the first), which may have changed the results.
There are limitations to the generalizability of our study. A higher proportion of our cohort was on active military duty or had history of acute military duty compared to the general population. Our cohort was more likely to have a history of traumatic brain injury, which suggests our cohort may have a less heterogeneous etiology of migraine compared to the general population (i.e. post traumatic). 20 The etiology of migraine may change the overall clinical course of the attack and ultimately change the response to treatment. 21 It is also possible that a higher proportion of our cohort was on prophylactic magnesium therapy compared to a cohort with limited healthcare access, which could have altered the results compared to a more heterogeneous population. These factors combined with the fact that this review was conducted at a single hospital should bring caution when considering the generalizability of these data.
Conclusions
IV magnesium supplementation was not found to be associated with length of admission in patients admitted with SM. Treatment with IV magnesium trended toward shorter length of admission in patients that did not require Neurology consultation, though not statistically significant. This study contributes to the limited pool of data available on patients with SM and demonstrates the evolution of magnesium therapy in migraine. Prospective research is needed to further study the efficacy of magnesium therapy in patients with prolonged migraine.
Footnotes
Authors’ Note: The view(s) expressed herein are those of the authors and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force and Department of Defense of the U.S. Government. Dr. Hoffman contributed to data collection, analysis, and interpretation and wrote and edited the majority of the manuscript. Dr. Aden conducted biostatistical analysis, data interpretation, and manuscript editing. Dr. Luster contributed to data collection, analysis, and interpretation. Dr. Bossler contributed to study design, data interpretation, manuscript editing, and faculty mentorship. Dr. Jordan designed the study, completed the Institutional Review Board review, contributed to data collection, analysis, and interpretation, and contributed to manuscript writing and editing. Research data can be requested by contacting the corresponding author via email or mail.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: William Hoffman  https://orcid.org/0000-0002-4131-1169
https://orcid.org/0000-0002-4131-1169
References
- 1. International Headache Society Classification ICHD-3, Status migrainosus. Accessed December 10, 2019. https://ichd-3.org/1-migraine/1-4-complications-of-migraine/1-4-1-status-migrainosus/
- 2. Silberstein S. Preventive migraine treatment. Continuum. 2015;21(4):973–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beltramone M, Donnet A. Status migrainosus and migraine aura status in a French tertiary-care center: An 11-year retrospective analysis. Cephalalgia. 2014;34:633–637. [DOI] [PubMed] [Google Scholar]
- 4. Couch J, Diamond S. Status migrainosus: causative and therapeutic aspects. Headache. 1983;23:94–101. [DOI] [PubMed] [Google Scholar]
- 5. Tarun S, Cutrer M, Smith J. Episodic status migrainosus: a novel migraine subtype. Cephalalgia. 2017;38(2):304–311. [DOI] [PubMed] [Google Scholar]
- 6. Kupetsky E. Chapter 4: migraine and magnesium. In: Sunderkrishnan R, Cantarin M. Magnesium: Application in Clinical Medicine. 1st ed. CRC Press. 2019:39–46. [Google Scholar]
- 7. Bigal M, Bordini C, Tepper S, Speciali J. Intravenous magnesium sulphate in the acute treatment of migraine without aura and migraine with aura. A randomized, double-blind, placebo-controlled study. Cephalalgia. 2002;22(5):345–353. [DOI] [PubMed] [Google Scholar]
- 8. Rozen TD. Emergency department and inpatient management of status migrainosus and intractable headache. Continuum. 2015;21(4):1004–1017. [DOI] [PubMed] [Google Scholar]
- 9. Cete Y, Dora B, Ertan C, et al. A randomized prospective placebo-controlled study of intravenous magnesium sulphate vs metoclopramide in the management of acute migraine attacks in the emergency department. Cephalalgia. 2005;25(3):199–204. [DOI] [PubMed] [Google Scholar]
- 10. Teigen L, Boes C. An evidence-based review of oral magnesium supplementation in the preventive treatment of migraine. Cephalalgia. 2014;35(10):912–922. [DOI] [PubMed] [Google Scholar]
- 11. Peikert A, Wilimzig C, Kohne-Volland R. Prophylaxis of migraine with oral magnesium: results from a prospective, multi-center, placebo-controlled and double-blind randomized study. Cephalalgia. 1996;16:257–263. [DOI] [PubMed] [Google Scholar]
- 12. Pfaffenrath V, Wessely P, Meyer C. Magnesium in the prophylaxis of migraine—a double-blind placebo-controlled study. Cephalalgia. 1996;16(6):436–440. [DOI] [PubMed] [Google Scholar]
- 13. Assarzadegan F, Asgarzadeh H, Hatamabadi A, et al. Serum concentration of magnesium as an independent risk factor in migraine attack. Int Clin Psychopharmacol. 2016;31(5):287–292. [DOI] [PubMed] [Google Scholar]
- 14. Orr S, Aube M, Becker W, et al. Canadian headache society systemic review and recommendations on the treatment of migraine pain in emergency settings. Cephalalgia. 2014;35(3):271–284. [DOI] [PubMed] [Google Scholar]
- 15. Schwedt T. Preventive therapy of Migraine. Continuum (Minneap Minn). 2018; 24(4 Headache):1052–1065. [DOI] [PubMed] [Google Scholar]
- 16. Vargas B. Acute treatment of migraine. Continuum (Minneap Minn). 2018;24(4):1032–1051. [DOI] [PubMed] [Google Scholar]
- 17. Schwedt T. Preventive therapy of migraine. Continuum (Minneap Minn). 2018;24(4):1052–1065. [DOI] [PubMed] [Google Scholar]
- 18. Xu F, Arakelyan A, Spitzberg A, et al. Experiences of an outpatient infusion center with intravenous magnesium therapy for status migrainosus. Clin Neurol Neurosurg. 2019;178:31–35. [DOI] [PubMed] [Google Scholar]
- 19. Modi S, Dharaiya D, Katramados A, Mitsias P. Predictors of prolonged hospital stay in status Migrainosus. Neurohospitalist. 2016;6(4):141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Whiteneck G, Cuthbert J, Mellick D. VA Traumatic brain injury. Veterans Health Registry Report. Department of Veterans Affairs. 2015. https://www.publichealth.va.gov/docs/epidemiology/TBI-report-fy2013-qtr4.pdf [Google Scholar]
- 21. Bennett-Brown C, Ostrowski-Delahanty S, Johnson TL, Victorio MC, Klein SK. Migraine phenotype prolongs recovery time in traumatic brain injury (TBI). Neurology. 2018;91(23 Supple 1):S17–S18. [Google Scholar]