Introduction
The coronavirus disease 2019 (COVID-19) pandemic has illustrated the advantages of using digital health technologies, such as telemedicine, to improve accessibility to both medical and psychosocial care. The use of such technologies can significantly impact adolescent and young adult (AYA) cancer patients' care by improving adherence, personalizing care, measuring health perception, and improving disparities. The population's perception of the utility of digital technologies is not concordant with that of their health care providers.1 This has created a unique situation in which patients' experiences with a potential class of therapeutic interventions are more comprehensive than that of their providers. Providers are frequently unaware of how digital technology is used by patients, impacts their perceptions of health, and facilitates adherence to therapies.2 Hereunder, we seek to highlight the digital technologies with the most potential to improve AYA supportive care based on initial data. Furthermore, we illustrate the need for further research of these technologies.
Methods
A literature search for existing articles within PubMed, Medline, Google Scholar, Google, Yahoo, and Bing was conducted in April of 2020. Search terms included but were not limited to “digital health,” “digital technology,” “pediatric,” “adolescents,” “young adult,” and “oncology.” Given the increased prevalence of telehealth articles in the setting of the COVID-19 pandemic, an extenuating circumstance, these were excluded from the literature review. The remaining articles pertinent to AYA oncology were classified into the three broad categories explored hereunder, with a summary of the most impactful and AYA-relevant articles described.
Extended reality
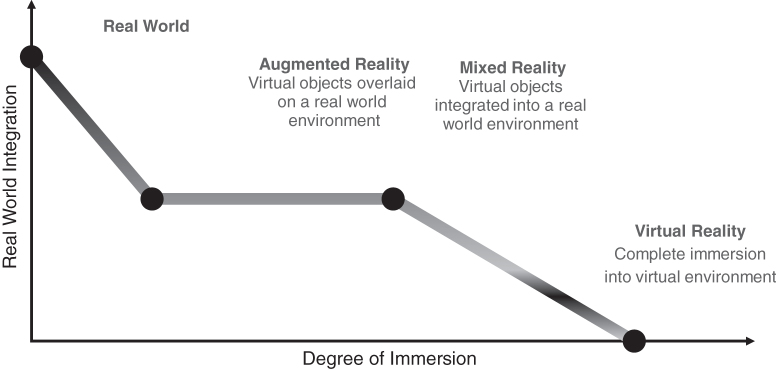
Virtual reality (VR), augmented reality, and mixed reality exist on a continuum of immersion that allows users to be displaced to a completely new digital environment, or to combine components of the real and digital worlds (Fig. 1). This is accomplished by using a heads-up display or mobile device (Fig. 2). Of these, VR has, thus far, been most thoroughly studied in the clinical setting. With ∼171 million users worldwide, VR technology has an adoption rate that outpaces early adoption of personal computers, the internet, and mobile phones.3,4 VR uses a combination of body tracking sensors and display headsets to immerse the user in an artificial environment. It allows for complete immersion, allowing patients to entirely block out the sights and sounds of their external environment.5
FIG. 1.
Comparison of the differences between virtual, augmented, and mixed reality.
FIG. 2.
Heads-up display and handset used in virtual reality.
Clinically, most medical applications of VR focus on decreasing pain or other noxious stimuli.5 Although the true mechanisms by which VR reduces pain perception remain unclear, Hoffman et al. used functional magnetic resonance imaging to show that VR caused a statistically significant reduction in pain-related neural activity in multiple regions of the brain, including the anterior cingulate cortex and the thalamus.6 A pilot study with 59 pediatric oncology patients found that VR reduced pain from subcutaneous venous port access, including decreases in heart rate and pain, as measured by the visual analogue scale.7 Another pilot study looked at the use of VR's distraction potential during chemotherapy infusions. In 11 patients aged 10–17 years, 82% found that VR distracted them from the fact they were receiving chemotherapy.8
VR is being further explored for other health care applications including education, social interaction augmentation, and as an adjunct to cognitive-based therapy and other psychiatric treatments.9,10 For patients with physical disabilities or social anxieties that prevent them from participating in support groups, VR provides the opportunity to connect with others and build strong social support networks.11 During situations requiring quarantine or isolation, such as the COVID-19 pandemic or bone marrow transplant, VR has been seen as a way to cope with the deleterious effects of prolonged isolation.12
Social media
Social media has become an important outlet for AYA patients with cancer to exchange ideas and support.13 Health professionals approach their patients' use of social media for health communication and information with mixed reactions, specifically due to concerns of scientific accuracy and exposure of their clinical decision making to public scrutiny.13 A qualitative study by Gage-Bouchard et al. found that within 15,852 cancer-related posts on various social media platforms, types of information included treatment protocols, health services usage, side effects, and complementary therapies.13 Social media is a particularly appealing communication modality in this population as AYAs do not readily participate in traditional psychosocial interventions.14 In addition to the peer-to-peer use of social media, there are AYA-focused social media accounts specifically aimed at this patient population. One Instagram® account, The Cancer Patient (@thecancerpatient), is a satirical approach to the challenges that come with having cancer and has >52,000 followers as of print.
Formal evaluation of these and similar resources includes a study done by Beaupin et al. investigating the feasibility of a novel concept called “photographs of meaning” within the AYA oncology population. Participants utilized a social media platform called PixStori to anonymously post on weekly themes chosen by the study coordinator. Other users anonymously viewed and commented on these posts. All 13 participants felt they would recommend the intervention to peers.14 Another study involved developing a social media site called LIFECommunity for AYA cancer survivors to create blogs and share information with peers.15 Participants with less of an “in-person” support network and those with strong pre-existing connections with other survivors used this resource most, concluding that LIFECommunity potentially filled a void in the participants' support system.15 Despite these perceived benefits, concerns remain about the impact of social media on children and young adults.16
Compliance enhancement technology
Recently, wearable devices and mobile phone applications promoting health maintenance have surged in popularity.17 A study done by Yurkiewicz et al. provided iPads® and synced Fitbit® fitness trackers to AYA patients at time of diagnosis.18 Seventy-nine percent of participants reported a subjective increase in physical activity and health-related quality of life. Although there were some drawbacks to the study, including patients' use of the iPads for more sedentary activities, the step tracker did give motivation to increase physical activity.18
Oral medication compliance is another field in which technology-driven interventions are being explored through digital health applications and electronic monitoring caps.17 Smart bottles such as Nomi®, SMRxT®, and Adheretech® provide increased reliability of measuring medication adherence.19 Oral medication nonadherence in the AYA population ranges between 27% and 60% and has been attributed to forgetfulness, a state of significant transition, and changing insurance status.20,21 A pilot study done with 23 AYA patients using a smartphone application to improve adherence to oral medications found that >50% of patients took their medications with the reminders.21
A recent study evaluated an application called “Pain Squad”—a mobile health application that “gamified” pain assessment and management in the AYA population. A reward system encouraged management compliance, and found 81% compliance among 18 patients.22 An improved version of the application recommended management techniques based on a standardized algorithm when patients felt pain, with an email alert sent to an oncology trained nurse if an adolescent reported sustained pain.22 The study found statistically significant decreases in pain and improvement in quality-of-life measures.22 These studies show the feasibility of implementing real-time monitoring systems in a remote setting.
Discussion
The AYA population's agility with technology has brought about significant positive change. It has empowered them to find like-minded communities online and new ways to gain knowledge.23 They utilize technology to communicate and are more receptive to the use of technology to improve their health.23 The aforementioned technologies contain a wealth of potential that can and should be utilized by providers and researchers alike to engage AYA patients in their health care.
There are multiple pilot studies in the literature that explore digital technologies with the potential to improve the care of AYA patients. There is, however, an extreme paucity of research beyond the proof-of-concept stage. Roadblocks include providers' general skepticism and difficulties implementing these modalities due to a lack of comfort with the technologies, as well as concerns regarding privacy, confidentiality, and professionalism.16
Digital health is quickly evolving, requiring the academic community to adopt new ways to explore its potential in a timely manner.2 Although the COVID-19 pandemic has accelerated the use of telemedicine, the aforementioned technologies have only been explored in a limited manner and have the potential to be impactfully incorporated with existing digital health platforms.24 Birckhead et al. have proposed a framework to develop and implement large scale clinical trials utilizing VR, but this framework could potentially be broadened to include other technologies.25 Similarly, the Italian Pediatric Hematology and Oncology Association created a multidisciplinary working group to develop guidelines addressing the proper use of social media by health care professionals, particularly when interacting with AYA patients. Significant emphasis was placed on the use of these platforms to supplement in-person interactions while maintaining professional boundaries and awareness of patient confidentiality issues.16
AYAs are keen adopters of new technologies, providing an even greater impetus to explore the impact of digital health on this population. This article explores the three most studied psycho-oncology digital technology categories based on literature review. The care of AYA oncology patients could be improved with further investigation into these modalities on a larger scale with greater provider understanding and incorporation of the AYA perspective.
Authors' Contribution
All authors have contributed to the article in significant ways, have reviewed, and agreed upon the article content.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Abrol E, Groszmann M, Pitman A, et al. Exploring the digital technology preferences of teenagers and young adults (TYA) with cancer and survivors: a cross-sectional service evaluation questionnaire. J Cancer Surviv. 2017;11(6):670–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aldiss S, Baggott C, Gibson F, et al. A critical review of the use of technology to provide psychosocial support for children and young people with long-term conditions. J Pediatr Nurs. 2015;30(1):87–101 [DOI] [PubMed] [Google Scholar]
- 3. Fink C. How are people making money in VR… Or When Will They? 2018. Accessed June24, 2020 from: https://www.forbes.com/sites/charliefink/2018/01/02/how-are-people-making-money-in-vr-or-when-will-they/#1d47311875d7
- 4. Petrov C. 35 virtual reality statistics that will rock the market in 2020. TechJury. 2018. Accessed June25, 2020 from: https://techjury.net/stats-about/virtual-reality/#gref.
- 5. Arane K, Behboudi A, Goldman RD. Virtual reality for pain and anxiety management in children. Can Fam Physician. 2017;63(12):932–4 [PMC free article] [PubMed] [Google Scholar]
- 6. Hoffman HG, Richards TL, Coda B, et al. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport. 2004;15(8):1245–8 [DOI] [PubMed] [Google Scholar]
- 7. Gershon J, Zimand E, Pickering M, et al. A pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatry. 2004;43(10):1243–9 [DOI] [PubMed] [Google Scholar]
- 8. Schneider SM, Workman ML. Virtual reality as a distraction intervention for older children receiving chemotherapy. Pediatr Nurs. 2000;26(6):593–7 [PubMed] [Google Scholar]
- 9. Bourdin P, Barberia I, Oliva R, Slater M. A virtual out-of-body experience reduces fear of death. PLoS One. 2017;12(1):e0169343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Falconer CJ, Rovira A, King JA, et al. Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych Open. 2016;2(1):74–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nathan EP, Winkler SL. Amputees' attitudes toward participation in amputee support groups and the role of virtual technology in supporting amputees: survey study. JMIR Rehabil Assist Technol. 2019;6(2):14887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Riva G, Wiederhold BK. How cyberpsychology and virtual reality can help us to overcome the psychological burden of coronavirus. Cyberpsychol Behav Soc Netw. 2020;23(5):277–9 [DOI] [PubMed] [Google Scholar]
- 13. Gage-Bouchard EA, LaValley S, Warunek M, et al. Is cancer information exchanged on social media scientifically accurate? J Cancer Educ. 2018;33(6):1328–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Beaupin LK, Pailler ME, Brewer-Spritzer E, et al. Photographs of meaning: a novel social media intervention for adolescent and young adult cancer patients. Psychooncology. 2019;28(1):198–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McLaughlin M, Nam Y, Gould J, et al. A videosharing social networking intervention for young adult cancer survivors. Comput Hum Behav. 2012;28(2):631–41 [Google Scholar]
- 16. Clerici CA, Quarello P, Bergadano A, et al. Proper use of social media by health operators in the pediatric oncohematological setting: consensus statement from the Italian Pediatric Hematology and Oncology Association (AIEOP). Pediatr Blood Cancer. 2018;65(5):e26958. [DOI] [PubMed] [Google Scholar]
- 17. Devine KA, Viola AS, Coups EJ, Wu YP. Digital health interventions for adolescent and young adult cancer survivors. JCO Clin Cancer Inform. 2018;2:1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yurkiewicz IR, Simon P, Liedtke M, et al. Effect of fitbit and iPad wearable technology in health-related quality of life in adolescent and young adult cancer patients. J Adolesc Young Adult Oncol. 2018;7(5):579–83 [DOI] [PubMed] [Google Scholar]
- 19. Crowe M. Common features of smart bottles. Pharmacy Times. 2018. Accessed July16, 2020 from: https://www.pharmacytimes.com/contributor/michael-crowe-pharmd-mba-csp-fmpa/2018/06/common-features-of-smart-bottles
- 20. Butow P, Palmer S, Pai A, et al. Review of adherence-related issues in adolescents and young adults with cancer. J Clin Oncol. 2010;28(32):4800–9 [DOI] [PubMed] [Google Scholar]
- 21. Linder LA, Wu YP, Macpherson CF, et al. Oral medication adherence among adolescents and young adults with cancer before and following use of a smartphone-based medication reminder app. J Adolesc Young Adult Oncol. 2019;8(2):122–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jibb LA, Stevens BJ, Nathan PC, et al. Implementation and preliminary effectiveness of a real-time pain management smartphone app for adolescents with cancer: a multicenter pilot clinical study. Pediatr Blood Cancer. 2017;64(10):e26554. [DOI] [PubMed] [Google Scholar]
- 23. Joshi SV, Stubbe D, Li ST, Hilty DM. The use of technology by youth: implications for psychiatric educators. Acad Psychiatry. 2019;43(1):101–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Badawy SM, Radovic A. Digital approaches to remote pediatric health care delivery during the COVID-19 pandemic: existing evidence and a call for further research. JMIR Pediatr Parent. 2020;3(1):e20049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Birckhead B, Khalil C, Liu X, et al. Recommendations for methodology of virtual reality clinical trials in health care by an international working group: iterative study. JMIR Ment Health. 2019;6(1):e11973. [DOI] [PMC free article] [PubMed] [Google Scholar]