Abstract
Background and aim of the work:
Several studies have shown beneficial effects for Platelet-rich plasma (PRP). We aimed to assess the efficacy of pure PRP injection for facial rejuvenation in Iran.
Methods:
30 female consecutive participants were injected with PRP in two sessions with 3 month interval. Evaluations were performed by comparing the pre- and post-improvement measurements of skin scan, before after photography by participants, therapeutic physician and blindly by a second dermatologist.
Results:
In 3 and 6 months follow-ups respectively, moderate to excellent improvement in periorbital dark circles (47.8,60.9%), periorbital wrinkles (73.9%,78.3%), nasolabial fold (52.2%,56.6%) and skin rigidity (52.3%,60.9%) reported by patients, was statistically significant only for dark circle(P value 0.031). Moderate to good improvement in periorbital dark circles (47.9%,74%), periorbital wrinkles (39.1%,43.5%)and nasolabial folds (4.3% ,13.1%) demonstrated by therapeutic physician‘s evaluation, was statistically significant for dark circle (P value 0.008) and nasolabial folds (P value 0.025). Moderate to good improvement in periorbital dark circles (34.8%, 52.2%), periorbital wrinkles (26.1%, 34.8%) and nasolabial folds (4.4%, 13%) by second dermatologist, was statistically significant for dark circle (P value 0.025).
Conclusion:
Face rejuvenation with PRP is a promising and noninvasive technique with best results observed in improving periorbital dark circles and wrinkles. (www.actabiomedica.it)
Keywords: Platelet-rich plasma, Facial skin rejuvenation, Periorbital dark circle
Introduction
Skin aging results from intrinsic process affected by genetic background and extrinsic process influenced by environmental factors such as sun exposure, air pollution, smoking, alcohol abuse, and poor nutrition (1). Physical appearance, not only affects self-respect and personality, but also influences level of acceptance by others (2). Therefore, increasing consideration has focused on facial rejuvenation, with more emphasis on exploring more effective modalities (3). Aesthetic facial rejuvenation, particularly nonoperative procedures are highly in demand.
Platelet-rich plasma (PRP) has been used for accelerating wound healing and tissue regeneration in various fields of medicine over the last several years (4).
Since PRP contains numerous growth factors, it has been studied in skin rejuvenation applications (4). It has been used by different methods such as topical application, direct intradermal injections or adjuvant to other procedures such as laser or microneedling (5).
Several studies have shown beneficial effects for this new treatment modality (4,5). Since there is no study regarding the rejuvenation effects of PRP in different areas of facial skin in Iran, we aimed to assess the efficacy of its injection for treating periorbital dark circles, crow’s feet and nasolabial folds.
Material and methods
In this before after pilot clinical trial, 30 female consecutive participants with Glogau skin score (6) of II to IV, were recruited.
The exclusion criteria were as follows: (1) pregnant or lactating women; (2) patients with severe diabetes, hypertension, or cardiopulmonary insufficiency; (3) patients with a bleeding tendency or coagulation disorders; (4) patients with photosensitization or immunosuppressive diseases; (5) patients whose skin is prone to scar tissue; (6) patients who had received chemical peel, dermabrasion, soft tissue filler, botulinum toxin injection, mesotherapy or other resurfacing surgeries; (7) patients who had taken isotretinoin, vitamin A, vitamin C, or other medications that affect collagen synthesis within 1 year; (8) patients with skin or any other organ cancer (9) patients who have suffered from mental disease, infectious disease, alcoholism, drug abuse or malnutrition (10) patients under corticosteroid treatment.
Autologous Concentrated Platelet Rich Plasma Preparation
The concentrated platelet rich plasma (cPRP) was prepared according to standard procedures (7). 60ml peripheral blood was taken in a sterile syringe containing 600U heparin from each participant in 2 sessions with a 3 month interval and sent to lab at 4 °C. Platelet rich plasma was prepared by first centrifugation at 2000g for 2 min and then cPRP was prepared by second centrifugation at 4000g for 8 min and the supernatant plasma was removed and 5 ml plasma was left and precipitated platelets were resuspended in this volume. 0.5ml of 10% calcium gluconate was added to cPRP for platelet activation.
After collecting photos and writing medical records, the facial treatment areas were coated with anesthetic cream Xyla-P (Tehran chemi) for an hour. Immediately after PRP preparation, it was injected in sterile condition and by an expert physician. A 30 gauge needle was used for superficial micro- injections by the mesotherapy technique ‘point by point’. Injections were spaced about 1 cm apart. The injections were administered into the papillary dermis and were sub-dermal and intra-dermal, 1 cc in periorbital area and crows feet, 1/5 cc in cheek and nasolabial fold each side. Treatments were done in two sessions with 3 month interval. Digital photos of patients were collected 3 and 6 months after the second treatment. Evaluation of wrinkle and darkness improvement was performed on the basis of personal judgment of participants, by comparing the pre- and post improvement measurements of skin scan (Davi &CIA-dermoprime), observation of before and after improvement photography by therapeutic physician and a second dermatologist who was unaware of the order of photos.
All statistical analyses were performed using SPSS software. All data were presented as mean±SD and percentage. Data were assessed for normality by using the Klomogrov–Smirnov test.
Paired sample T-test for normally distributed data and Wilcoxon for non-normally distributed data were used for data analysis. Chi squared test was used to compare the qualitative variables. A p-value<0.05 was considered as statistically significant.
Results
23 out of 30 participants completed the study. Two patients due to pain did not continue the trial and 5 more patients due to loss of follow up were omitted from the study. Mean age of patients was 45.1±6.89 years and in the range of 35 to 55 years .Thirteen patients (56.5%) had glogou score III, 9 patients (39.1%) glogou II and 1 patient (4.3%) glogou IV. The results were evaluated 3 and 6 months after the last session by comparing the pre-and post improvement measurements of skin scan, by the final patients’ satisfaction questionnaire; by the physician’s impressions and double blind evaluation of pre and post treatment photographs by another dermatologist (Figure 1).
Figure 1.
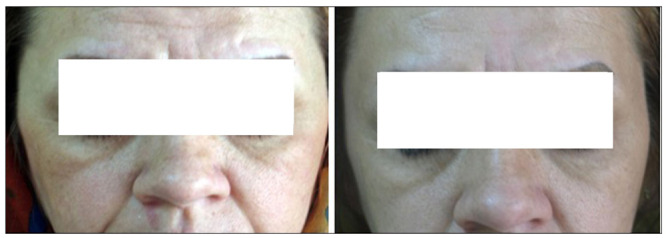
Before and 6 month after last treatment
Skin scan measurements
By using skin scan, variables such as skin wrinkle, moisture, pores, spots and elasticity were evaluated before starting treatment and 6 months after that. The results are showed in Table 1.
Table 1.
Skin scans measurements
| Variable | Index | Mean | SD | Min | Max | P value * |
| Moisture | Before treatment | 28.6 | 6.43 | 7 | 42 | 0.150 |
| After 6 months | 30.2 | 6.64 | 10 | 45 | ||
| Wrinkle | Before treatment | 14.0 | 2.39 | 10 | 19 | 0.007 |
| After 6 months | 12.3 | 2.89 | 6 | 17 | ||
| Pores | Before treatment | 26.1 | 14.68 | 4 | 58 | 0.881 |
| After 6 months | 26.6 | 17.83 | 4 | 66 | ||
| Spot | Before treatment | 14.4 | 9.48 | 2 | 38 | 0.850 |
| After 6 months | 14.9 | 9.25 | 2 | 41 | ||
| Elasticity | Before treatment | 42.7 | 4.88 | 30 | 54 | 0.152 |
| After 6 months | 44.5 | 2.79 | 40 | 50 |
Only skin wrinkle indicated statistically significant difference before and 6 months after treatment (Figure 2).
Figure 2.
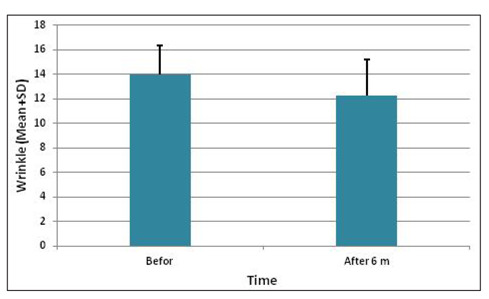
Skin wrinkle before and 6 months after treatment measured by skin scan
Patients’ self-evaluations
Patients’ satisfaction regarding dark circle, eye wrinkle, nasolabial fold and skin stiffness 3 and 6 months after treatment with PRP are shown in Table 2. In overall evaluation, only 13.4% mentioned no improvement 3 and 6 months after treatment.
Table 2.
Patients’ self-evaluations
| Improvement | Dark circle | Eye wrinkles | Nasolabial fold | Skin stiffness | |
| 3 months after treatment | Non | 10(43.5) | 5(21.7) | 9(39.1) | 9(39.1) |
| Poor | 2(8.7) | 1(4.3) | 2(8.7) | 2(8.7) | |
| Moderate | 6(26.1) | 11(47.9) | 7(30.5) | 8(34.8) | |
| Good | 2(8.7) | 3(13) | 5(21.7) | 2(8.7) | |
| Excellent | 3(13) | 3(13) | - | 2(8.7) | |
| 6 months after treatment | Non | 9(39.1) | 4(17.4) | 9(39.1) | 7(30.4) |
| Poor | - | 1(4.3) | 1(4.3) | 2(8.7) | |
| Moderate | 3(13.1) | 8(34.9) | 8(34.9) | 9(39.2) | |
| Good | 7(30.4) | 7(30.4) | 4(17.4) | 4(17.4) | |
| Excellent | 4(17.4) | 3(13) | 1(4.3) | 1(4.3) | |
| P value | 0.031 | 0.096 | 0.414 | 0.19 | |
Objective evaluation of the physician
Results of physician’s impressions regarding eye wrinkle, dark circle, and nasolabial folds at 3 and 6 month follow ups are indicated in Table 3.
Table 3.
Results of physicians’ impressions
| Physician evaluation | Second dermatologist evaluation | ||||||
| Improvement | Dark circle | Eye wrinkles | Nasolabial fold | Dark circle | Eye wrinkles | Nasolabial fold | |
| 3 months after treatment | Non | 3(13.0) | 4(17.4) | 17(73.9) | 6(26.1) | 5(21.7) | 19(82.6) |
| Poor | 9(39.1) | 10(43.5) | 5(21.7) | 9(39.1) | 12(52.2) | 3(13.0) | |
| Moderate | 11(47.9) | 8(34.8) | 1(4.4) | 8(34.8) | 6(26.1) | 1(4.3) | |
| Good | - | 1(4.3) | - | - | - | - | |
| 6 months after treatment | Non | 3(13.0) | 2(8.7) | 15(65.2) | 6(26.1) | 4(17.4) | 17(73.9) |
| Poor | 3(13.0) | 11(47.8) | 5(21.7) | 5(21.7) | 11(47.8) | 3(13.0) | |
| Moderate | 16(69.7) | 9(39.2) | 2(8.8) | 11(47.8) | 7(30.4) | 3(13.0) | |
| Good | 1(4.3) | 1(4.3) | 1(4.3) | 1(4.3) | 1(4.3) | - | |
| P value | 0.008 | 0.08 | 0.025 | 0.025 | 0.05 | 0.10 | |
Double blind evaluation by second dermatologist
Photographs taken before starting treatment and at 3 and 6 month follow ups were compared by a second dermatologist blindly. The results for eye wrinkle, dark circle and nasolabial folds are illustrated in Table 3.
By using spearman’s correlation, evaluations of treating physician and second dermatologist were compared. The results showed correlation regarding all variables including eye wrinkle, dark circle and nasolabial folds (Table 4).
Table 4.
Correlation assessment between treating physician and second dermatologist at 3 and 6 month follow ups
| physician and second dermatologist index | Correlation (r)* | P value |
| Eye wrinkle at 3 month | 0.854 | <0.001 |
| Nasolabial fold at 3 month | 0.796 | <0.001 |
| Dark circle at 3 month | 0.662 | 0.001 |
| Eye wrinkle at 6 month | 0.864 | <0.001 |
| Nasolabial fold at 6 month | 0.866 | <0.001 |
| Dark circle at 6 month | 0.720 | <0.001 |
Side effects
Among 23 participants who finished the study, 16 (69.6%) developed edema or edema and bruise at the site of injection, which lasted 1 to 7 days. One patient fainted at the time of injection.
Discussion
Human skin aging is caused by gradual decrease in its performance over time (intrinsic aging) and cumulative damage caused by environmental factors (external aging) including: smoking, exposure to chemicals and ultraviolet radiation (1). Continuous exposure to UV radiation in the skin, induces the destruction of collagen and elastic tissue changes, leading to disruption of the integrity of the extracellular matrix and finally wrinkles, epidermal and dermal atrophy, dyschromia, telangectasia and decreased skin laxity (3).
As a result, skin rejuvenation has become a hot topic, and applying non invasive procedures with fewer side effects and less down time has become popular (3,4).
PRP plays a vital role in regulating angiogenesis through secreting a large number of growth factors (GF), including platelet-derived GF isoforms (PDGF-aa, PDGF-ab, and PDGF-bb), transforming GF-b isoforms (TGF-b1 and TGF-b2), vascular endothelial GF (VEGF), epithelial GF (EGF), basic fibroblast GF (bFGF), and insulin-like GF (IGF) (3,8). Because of containing these growth factors, it has been studied in skin rejuvenation applications (4). To our knowledge, only TGF-β 1 has been investigated about its relation with melanogenesis. Kim et al investigated the effects of TGF-β1 on melanogenesis by using a spontaneously immortalized mouse melanocyte cell line, and asserted that TGF-β1 significantly inhibits melanin synthesis in a concentration- dependant manner (9). They declared that TGF-β1 decreases melanogenesis via delayed extracellular signal-regulated kinase activation.
This might explain PRP effect on periorbital dark circle.
There are four subtypes of PRP; pure PRP, leukocyte PRP (L-PRP), platelet-rich fibrin matrix (PRFM), and leukocyte and platelet-rich fibrin matrix. Pure PRP is the most commonly used preparation, which is also used in this trial (4).
In a study by Redaelli et al. in 2008, 23 patients received 3 monthly PRP injections for face and neck rejuvenation with no control group. According to spider score, improvements were as follows: nasolabial folds (24%); horizontal neck bands (28%); skin micro-relief (27%); snap test (20%); skin omogeneity and texture (33%); skin tonicity (22.5%) and periocular wrinkles (crow’s feet lines) (30%). Overall, the results were satisfactory. No serious and persistent side effects were reported (10).
In a clinical trial by Mehryan et al. in Iran, the efficacy of PRP on infraorbital dark circles and crow’s feet wrinkles was assessed. The effects on melanin content, color homogeneity of the treated area, epidermal stratum corneum hydration, and wrinkle volume and visibility index were compared 3 months after treatment with baseline. Only significant improvement in infraorbital color homogeneity was detected. No persistent or significant side effect was reported (11).
In a split face study by Kang et al. the effects of three PRP injections on wrinkles and skin tone in asian lower eyelid skin over the course of 12 weeks were assessed. The overall pooled comparison showed that PRP treatment was significantly effective on both wrinkles and skin tone in infraorbital skin (12).
Yuksel et al. applied PRP by dermaroller to 10 healthy volunteer’s forehead and malar area and injected PRP using a 27-gauge injector into the wrinkles of crow’s feet, three times at two-week intervals. Evaluations were done by participants and three dermatologists. There was statistically significant difference regarding the general appearance, skin firmness-sagging and wrinkle state according to the grading scale of the patients before and after three PRP applications. Whereas there was only statistically significant difference for the skin firmness–sagging according to the assessment of the dermatologists (13).
To evaluate the efficacy of a single injection of autologous PRFM for the correction of deep nasolabial folds (NLFs), Sclafani injected PRFM into the dermis and immediate sub dermis below the NLFs in 15 patients. Over 12 weeks, treated patients had statistically significant reductions in wrinkle assessment scores (14).
In several other studies PRP was used in conjunction with other rejuvenating modalities such as lasers or autologous fat transfer with promising results (15,16,17). However in a trial by Rigotti et al, the use of PRP did not show any significant advantage in skin rejuvenation over the use of expanded adipose-derived stem cell or stromal vascular fraction-enriched fat (18).
According to the results of our study, participants’ satisfactions at 3 and 6 month follow-ups respectively showed moderate to excellent improvement for all the parameters as follows; 47.8% and 60.9% for dark circle, 73.9% and 78.3% for periorbital wrinkles, 52.2% and 56.6% for nasolabial folds, 52.3% and 60.9%for skin stiffness, which was statistically significant only for dark circle (P value 0.031). Also, in overall evaluation of patients at 3 and 6 month follow-ups, most patients reported moderate to excellent improvement (82.7%, 82.7%, P value 0.014).
Therapeutic physician‘s evaluation at 3 and 6 month follow-ups showed 47.9%and 74% moderate to good improvement for dark circle, 39.1 and 43.5% for periorbital wrinkles and 4.3% and 13.1% for nasolabial folds, which was statistically significant for dark circle (P value 0.008)and nasolabial folds(P value 0.025).Second dermatologist evolutions at 3 and 6 month follow-ups demonstrated 34.8% and 52.2% moderate to good improvements for dark circle,26.1% and 34.8% for periorbital wrinkles,4.4%and 13.% for nasolabial fold, which was statistically significant only for dark circle (P value 0.025).
No serious or persistent side effects were reported. In this study similar to Redaelli’s study, patient satisfaction score was higher than physician scores which might be due to the fact that patients detected objective improvement at an earlier stage.
The strength of this study was using several ways for evaluating the results. Moreover platelets were counted before injections and in all patients they were 5 times of baseline.
Face rejuvenation with PRP is a promising and noninvasive technique. Best effects of PRP were observed in improving periorbital dark circles and wrinkles. No serious or persistent side effects were reported.
Limitations
We could not prove the changes in collagen and elastic fibers by biopsy technique or special imaging system before and after treatment by PRP. In addition, due to financial limitation, we could not use FDA approved kits of PRP, which might affect the results.
Acknowledgments
The authors would like to thank Miss Akram Momenzadeh for her valuable assistance in preparing and submitting this manuscript. This project was supported by a grant from the Vice Chancellor for Research of Mashhad University of Medical Sciences for a proposal by Dr Solmaz Nakhaizadeh with approval number 901109.
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Puizina-Ivić N, Mirić L, Carija A, Karlica D, Marasović D. Modern approach to topical treatment of aging skin. Coll Antropol. 2010;34:1145–53. [PubMed] [Google Scholar]
- Kohl E, Meierhöfer J, Koller M, Zeman F, Groesser L, Karrer S, et al. Fractional carbon dioxide laser resurfacing of rhytides and photoaged skin-a prospective clinical study on patient expectation and satisfaction. Lasers Surg Med. 2015;47:111–9. doi: 10.1002/lsm.22326. [DOI] [PubMed] [Google Scholar]
- Hui Q, Chang P, Guo B, Zhang Y, Tao K. The Clinical Efficacy of Autologous Platelet-Rich Plasma Combined with Ultra-Pulsed Fractional CO2 Laser Therapy for Facial Rejuvenation. Rejuvenation Res. 2016 Jun 23 doi: 10.1089/rej.2016.1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leo MS, Kumar AS, Kirit R, Konathan R, Sivamani RK. Systematic review of the use of platelet-rich plasma in aesthetic dermatology. J Cosmet Dermatol. 2015;14:315–23. doi: 10.1111/jocd.12167. [DOI] [PubMed] [Google Scholar]
- Arshdeep, Kumaran MS. Platelet-rich plasma in dermatology: boon or a bane? Indian J Dermatol Venereol Leprol. 2014;80:5–14. doi: 10.4103/0378-6323.125467. [DOI] [PubMed] [Google Scholar]
- Rohrer TE, Wesley NO, Glogau R, Dover J. Evaluation of beauty and aging face. In: Bolognia JL, Jorrizo JL, Schaffer JV, Callen PJ, et al., editors. Dermatology. 3ed ed. Vol. 3. UK: Elsevier: 2012. pp. 2474–2475. [Google Scholar]
- Shirvan M K, Alamdari D H, Ghoreifi A. A novel method for iatrogenic vesicovaginal fistula treatment: autologous platelet rich plasma injection and platelet rich fibrin glue interposition. J Urol. 2013;189:2125–2129. doi: 10.1016/j.juro.2012.12.064. [DOI] [PubMed] [Google Scholar]
- Sclafani AP, Azzi J. Platelet Preparations for Use in Facial Rejuvenation and Wound Healing: A Critical Review of Current Literature. Aesthetic Plast Surg. 2015;39:495–505. doi: 10.1007/s00266-015-0504-x. [DOI] [PubMed] [Google Scholar]
- Kim DS, Park SH, Park KC. Transforming growth factor-beta1 decreases melanin synthesis via delayed extracellular signal-regulated kinase activation. Int J Biochem Cell Biol. 2004;36:1482–1491. doi: 10.1016/j.biocel.2003.10.023. [DOI] [PubMed] [Google Scholar]
- Redaelli A, Romano D, Marciano A. Face and neck revitalization with platelet-rich plasma (PRP): clinical outcome in a series of 23 consecutively treated patients. J Drugs Dermatol. 2010;9:466–72. [PubMed] [Google Scholar]
- Mehryan P, Zartab H, Rajabi A, Pazhoohi N, Firooz A. Assessment of efficacy of platelet-rich plasma (PRP) on infraorbital dark circles and crow’s feet wrinkles. J Cosmet Dermatol. 2014;13:72–8. doi: 10.1111/jocd.12072. [DOI] [PubMed] [Google Scholar]
- Kang BK, Shin MK, Lee JH, Kim NI. Effects of platelet-rich plasma on wrinkles and skin tone in Asian lower eyelid skin: preliminary results from a prospective, randomised, split-face trial. Eur J Dermatol. 2014;24:100–1. doi: 10.1684/ejd.2014.2267. [DOI] [PubMed] [Google Scholar]
- Yuksel EP, Sahin G, Aydin F, Senturk N, Turanli AY. Evaluation of effects of platelet-rich plasma on human facial skin. J Cosmet Laser Ther. 2014;16:206–208. doi: 10.3109/14764172.2014.949274. [DOI] [PubMed] [Google Scholar]
- Sclafani AP. Platelet-rich fibrin matrix for improvement of deep nasolabial folds. J Cosmet Dermatol. 2010;9:66–71. doi: 10.1111/j.1473-2165.2010.00486.x. [DOI] [PubMed] [Google Scholar]
- Shin MK, Lee JH, Lee SJ, Kim NI. Platelet-rich plasma combined with fractional laser therapy for skin rejuvenation. Dermatol Surg. 2012;38:623–30. doi: 10.1111/j.1524-4725.2011.02280.x. [DOI] [PubMed] [Google Scholar]
- Park KY, Kim IS, Kim BJ, Kim MN. Letter: autologous fat grafting and platelet-rich plasma for treatment of facial contour defects. Dermatol Surg. 2012;38:1572–4. doi: 10.1111/j.1524-4725.2012.02515.x. [DOI] [PubMed] [Google Scholar]
- Willemsen JC, Lindenblatt N, Stevens HP. Results and long-term patient satisfaction after gluteal augmentation with platelet-rich plasma-enriched autologous fat. Eur J Plast Surg. 2013;36:777–82. doi: 10.1007/s00238-013-0887-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti G, Charles-de-Sá L, Gontijo-de-Amorim NF, Takiya CM, Amable PR, Borojevic R, et al. Expanded Stem Cells, Stromal-Vascular Fraction, and Platelet-Rich Plasma Enriched Fat: Comparing Results of Different Facial Rejuvenation Approaches in a Clinical Trial. Aesthet Surg J. 2016;36:261–70. doi: 10.1093/asj/sjv231. [DOI] [PMC free article] [PubMed] [Google Scholar]


