Abstract
Background:
The absence of a national register of inflammatory bowel diseases (IBD) hinders effective health care planning in Italy.
Aims:
to investigate prevalence of IBD in the city of Messina, Italy, based on General Practitioner (GP) records, and to establish current treatments prescribed by different health care providers.
Methods:
data were extracted from GP databases with the help of disease-specific healthcare cost exemption codes combined with ICD9 codes for ulcerative colitis (UC) and Crohn’s disease (CD), and prescription for mesalazine. Disease and treatment-related data were collected together with information on employment status and the current healthcare provider.
Results:
Eighty-six GPs participated covering a population of 100,834 people. IBD prevalence (419/105) was 80% higher than estimates of the Regional Health Authorities. Incidence showed a seven-fold increase over the past 30 years. Only 51% of CD and 26% of UC patients were followed by a dedicated IBD centre with more frequent prescriptions of immunomodulators and biologics (p<0.001) compared to GPs.
Conclusions:
Real world data show much higher figures on IBD prevalence than administrative estimates. Differences in therapeutic approaches between IBD-specialists and non-specialists may reflect poor confidence in managing immunosuppressive therapies by the latter, but may lead to inadequate therapy and cancer surveillance.
Keywords: General Practitioner, epidemiology, mesalazine, extraintestinal manifestations
Introduction
Chronic inflammatory bowel diseases (IBD) are complex multifactorial diseases of unknown aetiology with an immune-mediated pathogenesis developing in genetically susceptible subjects. They are characterized by chronic inflammation of the gastrointestinal tract and have a chronic-relapsing course (1,2). General practitioner (GP) activity is essential for early diagnosis and, in collaboration with referral centres, for surveillance of therapies and colorectal cancer (CRC) to control and limit the evolution of disease, which may lead to severe, irreversible complications with a considerable impairment of quality of life.
Knowledge of disease prevalence is fundamental for health care planning and clinical resource management (3). The absence of a national registry in Italy, to date, has hindered a reliable evaluation of the impact of care on ulcerative colitis (UC) and Crohn’s disease (CD) in the Italian population. Even though GPs possess, and possessed, the tools to provide updated data on epidemiology of these diseases thus allowing better territorial and in-hospital care planning, only a few epidemiological studies involving GPs were carried out in Italy, and these more than 20 years ago (4-6), whereas more recent reports have only been based on health care databases, e.g. disease-specific payment exemption codes (DPEC) and/or hospital discharges (7-10).
Finally, most data concerning the clinical course of these diseases come from referral centres, with the risk of being limited to cases with a more severe disease course, however, it has been reported that a consistent number of patients are not followed by referral centres (11,12). This means that, on the one hand, not all patients have access to the newer and more expensive therapies and, on the other hand, the percentage of patients on such newer therapies may be overestimated by referral centres.
In Sicily, known epidemiological data come from the Regional Health Department, which uses administrative health data flows, estimated by indirect methods, only considering the number of exemption code holders for medical assistance costs specific for IBD. It is easy to understand that this evaluation, which takes only administrative data into account, underestimates the real dimension of this issue since other healthcare cost exemption codes are frequently used instead of DPEC for diverse reasons, e.g. for age or economic reasons. Territorial investigation is extremely cumbersome and requires constant checking of data provided.
The present study was carried out to assess the epidemiological impact of IBD within the population of the city of Messina, to estimate the true prevalence of IBD in this area and to calculate, retrospectively, the evolution of incidence by using data from GPs treating individuals affected with IBD. Moreover, clinical presentation of disease, together with data on the current therapies prescribed by the local IBD referral centre or by generic gastroenterologists or other healthcare figures were assessed.
Patients and methods
GPs operating in the city of Messina (northeast Sicily) were invited to participate in the present survey by direct communication and electronic transmission of the study protocol containing participation procedures.
A preliminary evaluation of the prevalence of CD and UC and a characterization of the main clinical variables of affected patients was carried out through data-mining from electronic archives of computerized medical records of GPs participating in the study.
Patients with IBD were identified by physicians using different search strategies and, subsequently, by cross-checking the obtained data: 1. subjects with ICD-9 code 555 and 556 (respectively for CD and UC) recorded in the clinical file, 2. those who presented with the exemption codes specific for CD or UC (code 009), and 3. patients in chronic treatment with drugs indicated exclusively for IBD, such as mesalazine (in any form). This triple approach was chosen in order to overcome the potential bias through different payment exemption codes, e.g. permanent invalidity, and thus to capture the highest possible number of IBD patients.
Each identified case was then verified on the basis of clinical, endoscopic and histological data and subjected to a reliability check (A.B., W.F.), by reassessing the report of the endoscopic examination carried out at the time of diagnosis and the histological examination of intestinal biopsies. Participating GPs assisted by A.B. then collected data of the identified patients affected with IBD through the compilation of a clinical-anamnestic chart, to perform a detailed stratification of the main clinical, epidemiological, and demographic variables of the selected patients. Moreover, data on the current therapy [none, mesalazine (5-ASA), systemic steroids, low bioavailability steroids (LBS – budesonide or beclomethasone), immunomodulators (IMM – azathioprine, 6-mercaptopurine and methotrexate), and biological therapies (BIO- Infliximab, Adalimumab, Golimumab, Vedolizumab)] together with data on the principle professional figure following the patient (IBD specialist alone or jointly with GP, endoscopists, territorial gastroenterologists, or other), and the geographical place where the patients were cured (territorial, regional, or extraregional) were collected. Data on incidence are expressed as incidence rates over 10-year periods. Data collection began in October 2016 and ended in December 2017. The study was approved by the local Ethics Committee (protocol 106/16).
Statistics
Data are presented as absolute numbers or adjusted to 100,000 people for prevalence. Incident cases were calculated retrospectively from electronic archives and were defined as patients first diagnosed as affected by CD and UC in the period from 1979 to December 2017. For the number of cases at risk we accessed the ISTAT website (National Institute of Statistics) (13) and the overall population for each 10-year period was obtained calculating the average of the annual population. Crude incidence per 100,000 inhabitants was estimated for the whole period.
Data on therapies are expressed as crude numbers and percentages and were compared with the chi-square test. A p-value of < 0.05 was considered statistically significant.
Results
In the present study, out of 100 invited GPs, 86 GPs (36% of all GPs working in the city of Messina) participated in the study (Table 1), with a total number of 100,834 patients over 14 years of age recorded in their lists, representing 48.7% of the population aged over 14 years residing in Messina [population of the city of Messina aged over 14 years: 206,176 people (under 14 yrs: 30,786) (males: 97,745, females: 108,431)] (14). Unfortunately, no paediatrician was willing to participate.
Table 1.
population-based data with distribution by gender (adjusted per 100,000 inhabitants), current mean age, median age at diagnosis, current disease extension, and age distribution (numbers are expressed into crude numbers and percentages); calculated on total number of retrieved patients; E1/E2/E3 refers to the Montreal classification for ulcerative colitis (26) indicating rectal disease, left-sided disease, and (sub)total involvement of the colon, respectively; L1/L2/L3 refers to the Montreal classification for Crohn’s disease (26) indicating ileal, colonic, and ileo-colonic involvement of disease, respectively. SD=standard deviation.
| Population-based data | |||
| Participating GPs; n Total number of assisted patients Total IBD Patients excluded Patients recruited per GP (mean ±SD) |
86 100,834 423 11 4.9 ± 2.9 |
||
| Ulcerative colitis | Crohn’s disease | IBDU | |
| M/F | 139/120 | 85/63 | 6/10 |
|
Current mean age ± SD; years Median age at diagnosis (range); years |
55±17 37 (2-84) |
55±17.5 37 (10-74) |
54±18 35.5 (16-84) |
|
Current age distribution age < 40 years; n(%)* age 40 – 65 years; n(%)* age ≥ 65 years ; n(%)* |
129 (50) 109 (42) 21 (8) |
92 (62) 49 (33) 7 (5) |
7 (44) 8 (50) 1 (6) |
|
Montreal classification E1/E2/E3; n(%) L1/L2/L3/p(%) |
56/143/60 (22/55/23) – |
– 72/16/57/33 (50/11/39/23) |
|
Overall, 423 patients with IBD were identified [UC: 259 (139 males), CD: 148 (85 males), IBD undefined (IBDU): 16 (6 males)]. Eleven patients were excluded due to poor details concerning diagnostic criteria (Table 1).
For further statistical analysis, patients with IBDU were included in the UC group, except for age at diagnosis (Figure 1) and incidence calculations (Figure 3) The mean number of IBD patients followed by 1 GP was 4.9 ± 2.9 patients.
Figure 1.

Age distribution at diagnosis in IBD patient cohort.
Figure 3.

Incidence of IBD over the past decades in the province of Messina; Italy.
Thus, total prevalence of IBD was 419 patients/100,000 people (UC: 272/100,000, 95%CI: 269-275; CD: 147/100,000, 95%CI: 145-149), [UC: prevalence for males 148/100,000, for females: 119/100,000, CD: prevalence males 87/100,000, females: 58/100,000] male to female ratios were 1.2:1 and 1:1.6 in UC and CD, respectively. UC showed a higher prevalence rate, representing 65% of the total number of IBD cases, compared to 35% of CD (UC/CD ratio 1.85:1). Patient current average age was 55 years, with a median age at diagnosis of 37 years (Table 1).
In 228 patients (54%), diagnosis was made before the age of 40 years, in 165 patients (39%) between 40 and 65 years, and in 29 patients (7%) over 65 years (Figure 1). Most diagnoses of CD were made before 40 years with 92 cases (62%), followed by 49 (33%) diagnoses between 40 and 65 years, and only 7 patients (5%) were diagnosed over 65 years. In UC, 129 (50%) cases were diagnosed before 40 years, 109 (42%) between 40 – 65 years, and 21 (8%) were diagnosed over 65 years. Only for age calculation at diagnosis did we calculate the data for IBDU separately with 7 cases (44%) diagnosed before 40 years, 8 (50%) in the age group between 40 and 65 years, and 1 (6%) over 65 years. The incidence calculated retrospectively (Table 2, Figure 3) showed a seven fold higher incidence in the most recent decade (2008-2017) compared with that of three decades before (1998-1997).
Table 2.
Incidence rates of IBD cases in the city of Messina calculated in 10-year periods. The overall population for each 10-year period is obtained calculating mean of the annual population on the basis of ISTAT data (13).
| Years | IBD cases over 10-years/population | IBD incidence/100,000 | 95% CI |
| 1978 - 1987 | 28/260118 | 10.8 | 7.15 – 15.6 |
| 1988 - 1997 | 67/251693 | 26.6 | 20.6 – 33.8 |
| 1998 - 2007 | 141/247644 | 56.9 | 48.1 – 67.3 |
| 2008 - 2017 | 185/243208 | 76 | 65.5 - 87.8 |
Family aggregation was present in 64 patients (15%) with at least one first or second degree relative affected with IBD. Regarding surgery, 77 patients (18%) of the whole cohort underwent surgery: 52 (35%) with CD underwent intestinal resections but only 19 (7%) of patients with UC underwent total proctocolectomy. Perianal disease (a history of fistulas, abscesses, fissures) was present in 33 (22%) patients with CD. No data were available on surgical interventions in perianal disease.
Extraintestinal manifestations
One hundred and seven patients (25.4%) presented with extraintestinal manifestations (EIM) (Table 3), with articular involvement as the most frequent EIM (ankylosing spondylitis, entero-related arthritis, and psoriatic arthritis) diagnosed in 76 patients (18%). Dermatological manifestations (pyoderma gangrenosum, erythema nodosum and psoriasis) were present in 21 patients (5%), while hepatic and ocular manifestations were less frequent.
Table 3.
Extraintestinal manifestations (EIM) in IBD patient cohort
| EIM | n. | % |
| Articular (peripheral and axial spondyloarthropathies) | 76 | 18 |
| Psoriasis | 15 | 3.5 |
| Pyoderma gangrenosum | 2 | 0.5 |
| Erythema nodosum | 4 | 1 |
| Primary Sclerosing Cholangitis | 4 | 1 |
| Other liver diseases | 5 | 1.2 |
| Uveitis | 1 | 0.2 |
| Total | 107 | 25.4 |
Social data
Concerning the social employment status of patients affected by IBD, 225 patients (53%) were employed, 109 patients (26%) declared to be unemployed, 33 patients (8%) were students and 56 patients (13%) were retired. Although the unemployment rate was high it does not differ from that of the population of Messina (24.8% in 2017) (source: National Institute of Statistics – ISTAT15).
Management and Therapy
The management of patients affected with IBD was carried out for 147 patients (35%) by their GP in shared management with the reference IBD specialist but 276 patients (65%) were treated by their GPs alone or together with territorial gastroenterologists, endoscopists, or surgeons. When analysing for disease, 75 patients with CD (51%), but only 72 of patients with UC (26%) were followed by a dedicated IBD centre.
Three hundred and eighty-one patients (90%) with IBD were treated in their city of residence.
Taking all patients together, 338 (80%) received 5-ASA, alone or in combination with other therapies. Forty-eight (11%) patients were on systemic steroids at the moment of data extraction, 48 (11%) on low bioavailability steroids, 47 patients (11%) received immunomodulators, and 30 (10%) patients were on biologic therapy. No IBD-specific therapy was registered in 30 patients (7%).
Due to different professional figures caring for IBD patients, current therapies were analysed according to the healthcare providers, dividing them into cohort 1 (GP + non-IBD specialists) and cohort 2 (GP + IBD specialist) (Figure 2).
Figure 2.
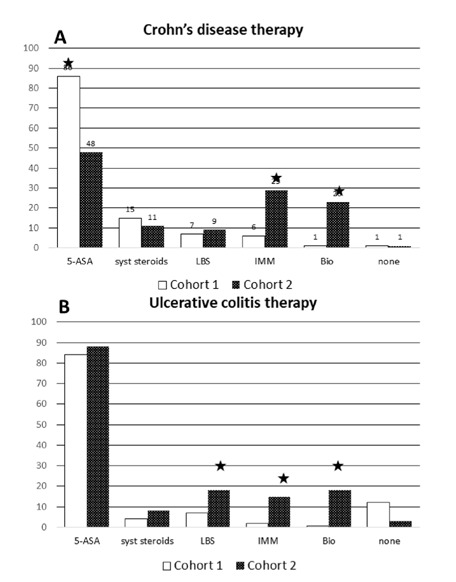
Therapies employed by non IBD-specialists (cohort 1) and IBD specialists (cohort 2) in Crohn’s disease (A) and in ulcerative colitis (B);* p<0.04 or less vs specialist care. 5-ASA: mesalazine; LBS: low bioavailability steroids; IMM: immunomodulators; BIO: biological therapy
Sixty two patients (85%) with CD patients in cohort 1 were treated with mesalazine alone or in association with other drugs compared with 36 patients (48%) in cohort 2 (p=0.017), systemic steroids at the moment of investigation were employed with 11 (15%) and 8 (11%), respectively in cohort 1 and 2, and similar figures were found for low bioavailability steroids (i.e. budesonide) with 5 (7%) and 7 (9%) patients (both not significant). IMM were used with only 4 (6%) CD patients in cohort 1 compared with 22 patients (29%) in cohort 2 (p=0.003) and biologic therapies (i.e. anti-TNF) were administered to 1 patient (1%) in cohort 1 but to 17 (23%) in cohort 2 (p=0.001). The one patient in cohort 1 treated with biologics received treatment from their rheumatologist for spondyloarthritis. One (1%) patient, in each cohort, did not receive any disease specific treatment. Concerning UC, 171 (84%) patients in cohort 1 and 64 (88%) patients in cohort 2 were treated with mesalazine alone or together with other drugs, and systemic steroids were administered to 29 (14%) patients in cohort 1 and to 6 patients (8%) in cohort 2 (both treatments not significant). Low bioavailability steroids (i.e. beclomethasone) were less frequently employed in cohort 1 compared with patients from cohort 2 (cohort 1: 15 (7%); cohort 2: 13 (18%), p=0.040). IMM and BIO were used less frequently in cohort 1 compared with cohort 2 [IMM: cohort 1: 3 patients (2%), cohort 2: 11 patients (15%), p<0.001); BIO: cohort 1: 1 patient (0.5%), cohort 2: 13 patients (18%), p<0.001]. Finally, no specific treatment was received by 26 (12%) patients in cohort 1 and 2 patients (3%) in cohort 2 (p=0.054).
Discussion
At least 3 important findings resulted from the present study: first, the true prevalence exceeded the administrative estimates for the city of Messina; second, only a limited number of IBD patients were followed by a dedicated centre; and third, the effective percentage of IBD treated with high cost therapies, i.e. biologics, was 10% and thus relatively small.
Prevalence
According to the Regional Health Department, the overall prevalence estimate based on exemption codes in the province of Messina for IBD was 232/100,000 in 2013 (10) compared to our population-based data collected in the city of Messina of 419 cases/100,000 people exceeding administrative data by 80% despite the fact that our data concerned only the population over 14 years of age. This marked difference, however, may be due to the fact that our present study was carried out in the city of Messina, whereas administrative data were collected over the whole province. However, our data showed also a 40% higher prevalence compared to the whole region of Sicily (based on payment exemption codes plus hospital discharges) reporting an average prevalence of 300/100,000 in 2013 (10). Interestingly, in the former study, the authors reported a greater prevalence for CD (standardized prevalence 160/100,000) compared with UC (142/100,000). These data are in conflict with former reports on incidence in Palermo and Messina (both provinces in the region of Sicily) (4,5), whereas other contemporary studies carried out in various Italian regions confirmed a higher prevalence for UC as in our study, e.g. in the Lazio (7), Forlì (province Forlì-Cesena; northeast Italy) (8), and San-Marino (9) (cfr table 3) regions. This apparent discordance may imply that unverified administrative data may not necessarily reflect the real situation. A further factor leading potentially to incomplete data capture is represented by the DPEC itself. In an area with an unemployment rate that reaches 25%, DPEC guarantees less coverage of health care costs than other codes, i.e. for age or unemployment, thus DPEC are frequently not used, with other codes being preferred.
Incidence
Our retrospectively estimated incidence data showed a rise by factor seven over the past 3 decades confirming a constant rise of IBD also in the region of Sicily. The highest incidence for IBD was found in the last decade (2008-2017) with 185 incident cases (CD incidence: 28.3/100,000/10-years, UC incidence 42.3/100,000/10-years) (Table 2, Figure 3).
Compared to former research reports from the late 80s, our retrospective calculation of incidence confirmed former data in the same area for CD with 0.8 cases/100,000/year for CD (Figure 3) in the decade from 1988-1997, but not for UC. In fact, our data gave 1.5 cases/100,000/year in the decade from 1988-1997 whereas Tragnone et al. (5) reported an importantly higher incidence with 7.1 cases/100.000/year in the same period. The study by Tragnone was based on multiple sources (hospital discharge data as primary source and GPs, endoscopists, radiologists, and surgeries as secondary source), whereas our study was based exclusively on databases from GPs cross-checking disease specific exemption codes, ICD9 codes, and prescription of mesalazine. A plausible hypothesis may be that since more than 20 years have passed, a certain number of patients may have moved away because of better job opportunities in the Northern regions of Italy or, to a surely lesser extent, they may have died and thus our retrospective incidence calculation missed them. Moreover, the study by Tragnone et al. did not verify every diagnosis so an overestimation is possible. In the same period, data from Palermo reported 8.5 cases/100,000/year for UC and 5.8 cases/100,000/year for CD, i.e. an already higher incidence compared to Messina but still with more UC diagnoses than CD (4).
The age distribution in our patients showed the typical pattern for IBD with a majority of patients diagnosed with IBD before age 40. Patients diagnosed over 65 years were 5% in CD and 8% in UC. Our figures represent approximately half of those reported by Jeuring et al (16). for CD and only a third of those reported for UC (CD 10-11%, UC 18-26%). This difference may be accounted for not only by geographical differences but also the fact that the study of Jeuring et al. included patients over 60 years of age whereas in our study patients over 65 years were considered. However our age distribution with 7% of patients over age 65 years most likely underestimates the real dimension since we expected a 15-20%; this may be due to our search strategy that didn’t caught elderly subjects with different exemption codes who had stopped maintenance therapy.
The frequency of extraintestinal manifestations are in line with former findings, with articular involvement the most frequent form (17); compared to a Swiss cohort (18), in our patients spondiloarthopathies were much less frequent but this difference may be explained since Vawricka et al. included arthralgias in the study whereas in our cohort only definite diagnoses of inflammatory spondyloarthritis were included.
Therapy
In our study, we found that only 26% of patients with UC and 51% of patients with CD were followed by an IBD specialist. This is in line with the findings of Rubin et al. (12) who reported in British IBD patients that only 24.0% of patients with UC and 42.5% of patients with CD continued to be followed by an IBD-specialist. This situation may be explained by the fact that IBD patients may have a mild disease course without the need for major treatments. Our 26% - 51% may reflect the percentage of patients with a more aggressive disease course. In former studies with a prolonged follow-up, 67% of UC patients were asymptomatic at last follow-up, (19) whereas in CD, 44% of patients were in remission with prolonged follow-up (20). Unfortunately, our data did not comprise an evaluation of disease activity at the moment of data collection nor the exact dosing of therapies.
Conventional therapies for CD differed by a more frequent use of mesalazine and a minor use of IMM in patients followed by non-specialists in an era where the role of mesalazine in CD is ever more questioned. This may explain that only 1% of CD patients actually was off every kind of specific therapy. Specialist care includes significantly more IMM and BIO reaching 29% and 23%, respectively, a figure already reported in a recent multicentre study from Italy (21).
Interestingly, there was no major use of systemic steroids in therapies provided by GPs or by other healthcare figures. Immunomodulators were less frequently prescribed by GPs than by IBD specialists and this is consistent with a study from Australia (22) reporting that GPs are frequently uncomfortable with immunosuppressive therapies and with therapy monitoring.
GPs frequently have difficulty in the care management of patients suffering from IBD, often due to the limited skills related to clinical management and the correct application of pharmacological protocols (23).
This finding underlines the need for an adequate education of GPs in terms of surveillance programs for IMM treatment and cancer. Indeed, more information and instruction were requested by GPs in a small study from central Italy (24).
Finally, in our study, only 10% of all IBD patients received or needed biologic therapies. Again, patients followed by IBD-specialist received them significantly more frequently. Presuming that our findings represent the real need for biologics in IBD patients a very small percentage require high-cost therapy. In 2016, similar percentages were reported based on the Truven Health MarketScan database for patients in the USA (25).
Conclusions
Our study provides a detailed real-world picture of IBD. The main findings were a much higher prevalence and a constant increase of IBD over the past 30 years together with a consistent percentage of elderly patients affected with IBD. Moreover, we showed that only a limited number of patients are followed by an IBD-specialist, a fact that may potentially lead to insufficient therapy and cancer surveillance.
Drawbacks of the present study were that no data were available on disease outcome or the actual disease activity and on the daily dosing of therapies. Another limit that underestimated our findings is the exclusion of the paediatric population.
Acknowledgements:
The authors wish to thank the following participating GPs, City of Messina (in alphabetical order): Alecci Umberto, Alibrando Antonino, Alvaro Andrea, Amato Giorgio, Amato Salvatore, Anania Nunziato, Armeli Antonella, Barbaro Luigi, Battiato Salvatore, Bucolo Antonino, Calapristi Irene, Cammera Bruno, Campisi Antonino, Capitò Rosanna, Carella Giuseppina, Caristia Francesco, Cartesio Salvatore, Catania Vincenza, Cincotta Gaetano, Costantino Cosimo, Crescenti Angelo, Crescenti Francesco, Crocitti Emilia, Crupi Domenico, D’Amico Giuseppe, D’Andrea Francesco, De Gaetano Carlo, De Gaetano Carmelo, Di Blasi Aldo, Di Geronimo Luciana, Fava Carmelo, Fazio Anna, Ferraro Tommasa, Flaccomio Teresa, Formica Michele, Gallo Santa, Maria Luisa, Genovese Basilio, Giaco Giovanni, Giorgianni Francesco, Gulletta Antonino, Ilacqua Gaetano, La Malfa Lorenzo, Labate Antonino, Lipari Luigi, Magazzù Giuseppe, Mammola Umberto, Mancini Fiorenzo, Maneri Giandomenico, Manuli Filippo, Marasco Isabella, Marchese Maria, Marino Sebastiano, Merrino Tommaso, Mezzapica Antonino, Micalizzi Carmelo, Migliardi Gregorio, Muscarà Pietro, Pagano Dritto Giuseppe, Pagano Maria Grazia, Panarello Caterina, Panebianco Francesca, Pernice Maurizio, Pizzimenti Concetto, Pollicita Mario, Pulejo Angelina, Ravidà Concetta, Saccà Felice, Saija Giuseppe, Salanitro Luigi, Santoro Beniamino, Scafidi Paolo, Scarso Gaetano, Scavino Francesco, Sferrazza Pietro, Sicilia Vincenza, Sirna Roberto, Sitajolo Nicola Valerio, Stracuzzi Antonino, Tamà Giuseppe, Tamà Sebastiano, Tigani Salvatore, Toscano Antonino, Ungaro Gabriella
Conflict of Interests:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
Funding:
The study was carried out with unrestricted grants from Zambon Italia and Pfizer Italia Srl
References
- Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012;380:1590–605. doi: 10.1016/S0140-6736(12)60026-9. [DOI] [PubMed] [Google Scholar]
- Ordás I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ. Ulcerative colitis. Lancet. 2012;380:1606–19. doi: 10.1016/S0140-6736(12)60150-0. [DOI] [PubMed] [Google Scholar]
- Busch K, Ludvigsson JF, Ekstrom-Smedby K, Ekbom A, Askling J, Neovius M. Nationwide prevalence of inflammatory bowel disease in Sweden: a population-based register study. Aliment Pharmacol Ther. 2014;39:57–68. doi: 10.1111/apt.12528. [DOI] [PubMed] [Google Scholar]
- Shivananda S, Lennard-Jones J, Logan R, et al. Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD). Gut. 1996;39:690–7. doi: 10.1136/gut.39.5.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tragnone A, Corrao G, Miglio F, Caprilli R, Lanfranchi GA. Incidence of inflammatory bowel disease in Italy: a nationwide population-based study. Gruppo Italiano per lo Studio del Colon e del Retto (GISC) Int J Epidemiol. 1996;25:1044–52. doi: 10.1093/ije/25.5.1044. [DOI] [PubMed] [Google Scholar]
- Ranzi T, Bodini P, Zambelli A, et al. Epidemiological aspects of inflammatory bowel disease in a north Italian population: a 4-year prospective study. Eur J Gastroenterol Hepatol. 1996;8:657–61. [PubMed] [Google Scholar]
- Di Domenicantonio R, Cappai G, Arcà M, et al. Occurrence of inflammatory bowel disease in central Italy: a study based on health information systems. Dig Liver Dis. 2014;46:777–82. doi: 10.1016/j.dld.2014.04.014. [DOI] [PubMed] [Google Scholar]
- Valpiani D, Manzi I, Mercuriali M, et al. A model of an inflammatory bowel disease population-based registry: The Forlì experience (1993-2013) Dig Liver Dis. 2018;50:32–36. doi: 10.1016/j.dld.2017.09.120. [DOI] [PubMed] [Google Scholar]
- Piscaglia AC, Lopetuso LR, Laterza L, et al. Epidemiology of inflammatory bowel disease in the Republic of San Marino: The “EPIMICI - San Marino” study. Dig Liver Dis. 2019;51:218–25. doi: 10.1016/j.dld.2018.08.016. [DOI] [PubMed] [Google Scholar]
- Macaluso FS, Mocci G, Orlando A, Scondotto S, Fantaci G, Antonelli A, et al. Prevalence and incidence of inflammatory bowel disease in two Italian islands, Sicily and Sardinia: A report based on health information systems. Dig Liver Dis. 2019;51:1270–4. doi: 10.1016/j.dld.2019.05.017. [DOI] [PubMed] [Google Scholar]
- Stone MA, Mayberry JF, Baker R. Prevalence and management of inflammatory bowel disease: a cross-sectional study from central England. Eur J Gastroenterol Hepatol. 2003;15:1275–80. doi: 10.1097/00042737-200312000-00004. [DOI] [PubMed] [Google Scholar]
- Rubin GP, Hungin AP, Kelly PJ, Ling J. Inflammatory bowel disease: epidemiology and management in an English general practice population. Aliment Pharmacol Ther. 2000;14:1553–9. doi: 10.1046/j.1365-2036.2000.00886.x. [DOI] [PubMed] [Google Scholar]
- https://istat.it (accessed February 26th, 2020) [Google Scholar]
- http://www.comuni-italiani.it/083/statistiche/eta2017.html (accessed June 15th, 2019) [Google Scholar]
- https://dati.istat.it/index.aspx?queryid=20745 (accessed February 26th, 2020) [Google Scholar]
- Jeuring SF, van den Heuvel TR, Zeegers MP, Hameeteman WH, Romberg-Camps MJ, Oostenbrug LE, et al. Epidemiology and Long-term Outcome of Inflammatory Bowel Disease Diagnosed at Elderly Age-An Increasing Distinct Entity? Inflamm Bowel Dis. 2016;22:1425–34. doi: 10.1097/MIB.0000000000000738. [DOI] [PubMed] [Google Scholar]
- Isene R, Bernklev T, Høie O, Munkholm P, Tsianos E, Stockbrügger R. EC-IBD Study Group. Extraintestinal manifestations in Crohn’s disease and ulcerative colitis: results from a prospective, population-based European inception cohort. Scand J Gastroenterol. 50:300–5. doi: 10.3109/00365521.2014.991752. [DOI] [PubMed] [Google Scholar]
- Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:1982–2. doi: 10.1097/MIB.0000000000000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer RG, Easley KA, Rankin GB. Clinical patterns, natural history, and progression of ulcerative colitis. A long-term follow-up of 1116 patients. Dig Dis Sci. 1993;38:1137–46. doi: 10.1007/BF01295733. [DOI] [PubMed] [Google Scholar]
- Solberg IC, Vatn MH, Høie O, Stray N, Sauar J, Jahnsen J, et al. IBSEN Study Group. Clinical course in Crohn’s disease: results of a Norwegian population-based ten-year follow-up study. Clin Gastroenterol Hepatol. 2007;5:1430–8. doi: 10.1016/j.cgh.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Viola A, Monterubbianesi R, Scalisi G, Furfaro F, Rea M, Saibeni S Italian Group for the Study of Inflammatory Bowel Disease (IG-IBD) Late-onset Crohn’s disease: a comparison of disease behaviour and therapy with younger adult patients: the Italian Group for the Study of Inflammatory Bowel Disease ‘AGED’ study. Eur J Gastroenterol Hepatol. 2019;31:1361–9. doi: 10.1097/MEG.0000000000001546. [DOI] [PubMed] [Google Scholar]
- Tan M, Holloway RH, Lange K, Andrews JM. General practitioners’ knowledge of and attitudes to inflammatory bowel disease. Intern Med J. 2012;42:801–7. doi: 10.1111/j.1445-5994.2011.02586.x. [DOI] [PubMed] [Google Scholar]
- Selby L, Hoellein A, Wilson JF. Are primary care providers uncomfortable providing routine preventive care for inflammatory bowel disease patients? Dig Dis Sci. 2011;56:819–24. doi: 10.1007/s10620-010-1329-8. [DOI] [PubMed] [Google Scholar]
- Sossai P, Filippetti F, Muselmani AA, Catalini G. Inflammatory bowel diseases and the general practitioner’s role in a region of Central Italy. Clin Exp Gastroenterol. 2010;3:27–31. doi: 10.2147/ceg.s9334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel CA, Yang F, Eslava S, Cai J. Real-World treatment pathway visualizations show low use of biologic therapies in Crohn’s disease and ulcerative colitis. Gastroenterology. 2017;(152 Suppl 1):S371–2. [Google Scholar]
- Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;(19 Suppl A):5A–36A. doi: 10.1155/2005/269076. [DOI] [PubMed] [Google Scholar]


