Abstract
Objectives:
The main aim of this study was to evaluate BMI changes in children and adolescent with obesity or overweight, analyzing the possible risk factors that contributed to weight gain during a pandemic-associated lockdown.
Material and Methods:
The study was conducted at the Pediatric Endocrinology Department of a third-level University Hospital in Rome, including children and adolescents with overweight and obesity. Personal, anthropometrics data and other information about physical activity, eating habits and psychological aspects were collected.
Results:
We included in our study 64 participants, of which 33 (51.6%) were patients with overweight and 31 (48.4%) with obesity. We divided patients in two groups: patients with pre-versus post-lockdown Δ-BMI > 0 (31, 48.4%) and patients with Δ-BMI < 0 (33, 51.6%). Our data showed that patients whose BMI increased were more sedentary (p=0.024 for physical activity and p=0.005 for hours spent with videogames) during the pandemic. As for the eating habits more than half of the subjects (67.2%) had increased the consumption of homemade desserts, bread, pasta and pizza, and a worse diet was found in patients with BMI gain (p=0.000). Regarding the psychic condition the 80% of patients reported psychological discomfort, and patients with an increase in BMI had episodes of emotional feeding more frequently (p=0.016).
Conclusions:
The COVID19 pandemic has had disastrous effects not only directly, but also indirectly through the lockdown especially on some categories, such as adolescents with overweight and obesity. The results indicate that it also causes significant changes in lifestyle, physical inactivity and psychological problems among children and adolescents with obesity/overweight. (www.actabiomedica.it)
Keywords: Children, COVID19, emotional eating, lockdown, obesity, overweight
Introduction
Since December 2019 novel Coronavirus Infection (2019-nCoV) spread in China and subsequently all around the World, becoming a public health emergency. In Italy first cases are reported from February 2020 and since then the virus has spread quickly in all regions.
In order to contain and mitigate the spread of the virus and the large number of infections and deaths, on 9th March 2020, the Italian Government established more stringent containment measures. Due to these measures a sudden and radical change has occurred in the habits and lifestyles of the population, with a drastic reduction of any form of socialization (1). Physical distancing and self-isolation strongly impacted citizens’ lives, affecting in particular eating habits and everyday behaviors (1).
The lockdown has certainly had a strong impact on adults, but even on children and adolescents. Indeed parents had difficulty explaining to their children, especially younger ones, what was happening and why the various social distancing rules to follow. Then for children and adolescents also the psychological impact is not to be underestimated, because hearing continuously on television news about the COVID-19 can be very stressful also for young people. In addition, the schools were closed, the children spent a lot of time at home without being able to see friends or relatives, nor do group sports activities. All this favored sedentary lifestyle, bad eating habits and the use of multimedia devices, such as television, smartphone and videogames.
Children and adolescent with overweight and obesity represented one of the categories most at risk during the lockdown; previous studies highlight that these young people will make lifestyle weight control programs worse at home than when they are engaged in normal daily activities (schools, sports, etc) (2).
Von Hippel et al., reported the effects of school versus non-school environments on overweight in childhood; they found that BMI gain was more rapid during summer vacation than during the in-session school year (3).
The main aim of this study was to evaluate BMI changes in children and adolescent with obesity or overweight, analyzing the possible risk factors that contributed to weight gain during a pandemic-associated lockdown, such as physical activity, diet and use of multimedia devices.
Materials and Methods
Patients selection
A cross-sectional study was carried out by the Pediatric Endocrinology Department of a third-level University Hospital in Rome, from 3rd June 2020 to 28 th June 2020, at the end of the COVID19-associated lockdown. The study was based on a telephone interview, carried out by pediatricians to children and adolescents, aged between 8 and 18, with overweight or obesity in follow up at the Pediatric Endocrinology clinic of our Hospital. The interview was anonymous and participation was voluntary.
According to international guidelines (4), we considered patients with overweight those with BMI at or greater than 85th to less than 95th percentile for age and sex and patients with obesity those with a BMI at or greater than 95th percentile for age and sex. We used Cacciari’s Italian growth charts to attribute the percentile (5). The following were excluded: children under 8 years of age, adults over 18 years of age, subjects suffering from rare disease and/or psychomotor delay, subjects lost to endocrinological follow-up as they had become normal weight.
The study was approved by the Institutional Review Board and Ethic Committee of our institution.
Questionnaires
The questionnaire was developed by the primary investigators following a review of related literature (1,6-7). Furthermore, the questionnaire was experimented as an in-person interview among (n = 10) children admitted to the Pediatric ward to verify their clarity, suitability of the formulation, as well as the average time required for its completion. The questionnaire was later reviewed by the research team and some corrections were made where needed.
The telephone interviews lasted about 20 minutes and the questionnaire consisted of 27 questions.
The first part used 8 questions concerned socio-demographic and anthropometrics data (age, gender, household, weight and height before and after the lockdown. The other questions were divided into 3 categories: Physical activity (physical activity before and during lockdown, time spent playing video games); eating habits (number of meals/day, quantity of food taken, daily consumption of certain foods-for-example junk food consumption, pizza, sweets, red meat, fruits and vegetables); psychological aspect (psychological mood during lockdown, history of contacts with covid-19 patients, sleep behavior, nighttime consumption of food, boredom eating).
To stratify the habits into better and worse, a score was associated with each question. In this way it was possible to assign a total score to each category. A worse diet was considered for a total score <0; a psychological distress for a total score <0. The full version of the questionnaires with score is available as Supplementary Materials.
The primary endpoints were: identify how many children have lost weight at the end of the lockdown and how many gained weight; assess how children’s habits have changed in the three categories analyzed and evaluate the correlation between Δ-BMI and the three categories.
Statistical analyses
Categorical variables were presented as numbers and percentages and were evaluated by Fisher exact test. Continuous variables with normal distribution were summarized as the mean (standard deviation) and the difference between groups were analyzed using Student’s t-test. The Spearman’s correlation coefficient was calculated in order to evaluate the correlation between continuous and categorical variables. Results were significant for p value<0.05. Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.
Results
Patients
We analyzed a cohort of 176 patients with obesity or overweight followed at our Pediatric Endocrinology Clinic. We contacted only the families of patients aged 18 or under on March 9th, 2020, for a total of 149 patients: 69 (46.3%) were unreachable by phone, while 64 (43.0%) responded and agreed to be interviewed and 16 (10.7%) refused. The 64 participants included 26 (40.6%) males and 38 females (59.4%), with a mean baseline age of 13.9 years (SD = 4.2; 95% CI = 12.9-14.9). The mean BMI before the lockdown period was 27.7 kg/m2 (SD = 4.8; 95% CI = 26.5-28.9), while the mean BMI after the lockdown period was 27.6 kg/m2 (SD = 4.0; 95% CI = 26.1-28.1). Moreover, at the beginning of the pandemic 33 (51.6%) patients were overweight (BMI between 85th and 95th percentile), while 31 (48.4%) were obese (BMI>95th percentile).
Then we divided patients in two groups: patients with pre- versus post-lockdown Δ-BMI < 0 (33, 51.6%) and patients with Δ-BMI > 0 (31, 48.4%).
There were no differences in the two groups regarding gender, age, type of home (countryside vs city), taking medications or supplements. The data on the demographic and anthropometric characteristics of the subjects are summarized in Table 1.
Table 1.
Demographic and anthropometric characteristics
| All patients (n=64) | Δ BMI <0 (n=33) | Δ BMI >0 (n=31) | P-value | |
| Gender (male) | 26 (40.6%) | 15 (45.4%) | 11 (35.4%) | 0.45 |
| Age (years) | 13.9 (±2.4) | 14.4 (±2.4) | 13.5 (±2.5) | 0.15 |
| Weight before lockdown (kg) | 71.6 (±19.6) | 76.8 (±21.9) | 66.0 (±15.1) | 0.026 |
| Weight after lockdown (kg) | 72.2 (±17.2) | 74 (±18.4) | 70.3 (±16) | 0.38 |
| Height before lockdown (cm) | 159.6 (±14.6) | 162.3 (±14.5) | 156.8 (±14.3) | 0.14 |
| Height after lockdown (cm) | 161.1 (±14.3) | 163.7 (±14.2) | 158.2 (±14.0) | 0.12 |
| BMI before lockdown (kg/m2) | 27.7 (±4.8) | 28.8 (±5.5) | 26.6 (±3.5) | 0.58 |
| BMI after lockdown (kg/m2) | 27.6 (±4.0) | 27.3 (±4.3) | 27.8 (±3.7) | 0.62 |
| Weight excess before lockdown (kg) | 18.1 (±13.7) | 21.2 (±15.9) | 14.8 (±10.0) | 0.065 |
| Overweight (BMI 85th and 95th pc) | 33 (51.6%) | 16 (48.5%) | 17 (54.8%) | 0.63 |
| Obese (BMI > 95th pc) | 31 (48.4%) | 17 (51.5%) | 14 (45.2%) | 0.62 |
| Area of living (rural vs. urban) | 23 (35.9%) | 13 (39.3%) | 10 (32.2%) | 0.61 |
| Medications or supplements | 17 (26.6%) | 11 (33.3%) | 6 (19.4%) | 0.26 |
| Data are count (%) or mean (± SD). | ||||
Outcomes
Statistically significant data were found about physical activity: patients whose BMI increased were more sedentary (p=0.024 for physical activity and p=0.005 for hours spent with videogames) during the pandemic, but not before it.
As for the eating habits, during the lockdown more than half of the subjects (67.2%) had increased the consumption of bread, pasta and pizza, especially patients with Δ-BMI > 0. Indeed, a significant difference between the groups was found about the consumption of carbohydrates versus fiber, vegetables and fruit or proteins (p=0.002). About a third of patients (31.2%) drank sugary drinks during the pandemic, with no statistically significant differences between the two groups. No statistically significant differences were found even in the number of daily meals, in fact, most patients consumed 4 or 5 meals a day. A worse diet was found in 61.3 % of patients with BMI gain, against 12.1% of those with BMI decrease (p=0.000).
Furthermore 42% of children and adolescent said they had eaten meals other than usual during the pandemic and that they had often prepared dishes following recipes proposed online. Fifty-six percent of them stated that they never prepared meals on their own, as the parent was mainly at home, worked in smart working and had more time to devote to them.
Regarding the mental health, during the lockdown period, the majority of children/adolescents (80%) reported psychological discomfort, although without differences between the two groups. No statistically significant differences were found even in sleep disturbances or having relatives or acquaintances with known SARS-CoV-2 infection. However, patients who presented with an increase in body mass index had more episodes of emotional feeding, such as nighttime food consumption and boring food (48.3 % vs 18.1 %, p=0.016). The most important results about physical activity, eating habits, psychological aspect are described in Table 2.
Table 2.
Physical activity, eating habits, psychological aspect
| All patients (n=64) | Δ BMI <0 (n=33) | Δ BMI >0 (n=31) | P-value | |
| Physical activity before lockdown | 47 (73.4%) | 26 (79%) | 21 (67.7%) | 0.42 |
| Physical activity during lockdown | 33 (51.6%) | 22 (66.7%) | 11(35.5%) | 0.024 |
| Hours spent with videogames (average) | 2.9 (±1.8) | 2.3(±1.5) | 3.5 (±1.9) | 0.005 |
| Food eaten more frequently: -Bread, pasta, pizza -Desserts -Meat -Vegetables and fruit -Fish |
43 (67.2%) 3 (4.7%) 8 (12.5%) 10 (15.6%) 0 (0%) |
18 (55%) 0 (0%) 6 (18%) 9 (27%) 0 (0%) |
25 (80.6%) 3 (9.7%) 2 (6.5%) 1 (3.2%) 0 (0%) |
0.002 |
| Sugary drinks | 20 (31.2%) | 7 (21.2%) | 13 (41.9%) | 0.10 |
| 4 or 5 meals a day | 51 (79.7%) | 27 (81.8%) | 24 (77.4%) | 0.76 |
| Meals prepared by yourself | 28 (43.8%) | 14 (42.4%) | 14 (45.2) | 1 |
| Worse diet (score <0) | 23 (35.9%) | 4 (12.1%) | 19 (61.3%) | 0.000 |
| Emotional eating | 21 (32.8%) | 6 (18.1%) | 15 (48.3%) | 0.016 |
| Sleep disorders | 36 (56.2%) | 19 (57.5%) | 17 (54.8%) | 0.92 |
| Relatives or acquaintances positive at Covid-19 | 12 (18.7%) | 7 (21%) | 5 (16.1%) | 0.75 |
| Psychological discomfort (score<0) | 38 (59.4%) | 19 (58%) | 19(61.3%) | 0.80 |
| Data are count (%) or mean (± SD). | ||||
A weak direct correlation was found between Δ-BMI and the time spent playing video games (R = 0.34, p = 0.006) and the emotional eating episodes (R = 0.3, p = 0.012). While, feeding score, preference to eat fruit and vegetables and physical activity correlate inversely and moderately with Δ-BMI (respectively R = -0.6, p <0.0001, R = -0.5 p <0.0001 and R -0.4, p = 0.003).
No correlation was observed between Δ-BMI and the psychological discomfort (R = 0.11, p = 0.4), however, a correlation was found between the time spent on video games and a worse psychological score (R = -0.3, p = 0.024).
The correlations between qualitative variables are shown in the scatter plots (Figure 1.)
Figure 1.
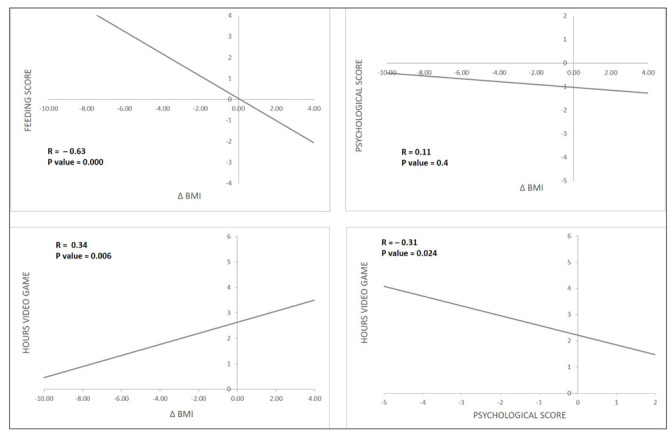
Correlation between qualitative variables
Discussion
This observational study provides a description of the eating habits and lifestyle of Italian children and adolescent with overweight and obesity during the COVID19-lockdown. It was conducted at the end of the lockdown, with the restart of normal daily activities. After the spread of the virus and the large number of infections and deaths, the strategy adopted by many countries, including Italy, has been “social distancing”. The lockdown had the positive effect of flattening the epidemic curve, thanks to the maintenance of the social rules imposed (1). However, the fear of the disease and death, as well as the restrictions of individual freedom, worsened the stress load (1). Indeed we must consider the indirect impacts the pandemic had on changes in eating behaviors, physical activity and psychological aspect.
We included in our study children and adolescents with overweight/obesity and we analyzed their habits during the lockdown and changes in their BMI and weight.
As expected, patients with increased BMI at the end of the lockdown were more sedentary during the pandemic. Children and adolescents who weren’t used to play sports before the COVID-19 lockdown, did not do so even during the pandemic. However, the most interesting fact is that among those who already play sports, training frequency has decreased.
Furthermore, our data showed that the group of patients with an increased BMI was the one who had the worst diet during the quarantine. One of the reasons for a worse diet was the reduction in the consumption of fresh food, accompanied by a deficiency of vitamins and minerals (vitamin C, vitamin E and beta-carotene), due to stringent measures and economic blockade. Deficiency of these micronutrients is associated with both obesity and a reduced immune response, making them more susceptible to viral infections (8-9), and it is therefore an important risk factor for these patients. In fact, obesity is a state of chronic low-grade inflammation dependent on the adipokine secretion of the adipose tissue with immunomodulatory effects (10) that contributes to the onset of several metabolic diseases (including insulin resistance and type 2 diabetes mellitus, dyslipidemia and hypertension). These, due to the downregulation of the innate and adaptive immune responses, make the immune system more vulnerable to infections, resulting in patients being less responsive to vaccinations, antivirals and antimicrobial drugs (11).
Another reason for poor diet was the increased consumption of carbohydrates. Particularly, during the lockdown, more than half of the subjects had increased the consumption of homemade desserts, bread, pasta and pizza, cooked to fill the time. Indeed, the problem of filling time and boredom played a very important role during the pandemic: the subjects with BMI increased woke up at night to look for food, ate out of boredom, and spent more time playing videogames.
To sum up, we can speculate that those who gained BMI had a worse economic condition caused by lockdown, which reduced the purchase of more expensive foods like fruits and vegetables and ate poorer products like pasta and pizza. A tendency to seek comfort in food may also be the cause of weight gain. In fact, it should be noted that most children and adolescents reported sleep disturbances and psychological distress, but those who increased BMI had more episodes of emotional eating, meaning that these patients have sought the answer to their problem in eating. And finally, they were more sedentary.
Although this is a partial snapshot of the current Italian children and adolescents situation, our data seem to confirm the evidence already observed in quarantined individuals (12), showing that people in lockdown are experiencing negative psychosocial changes, which have an impact on well-being (e.g., sleep disturbances, emotional eating, anxiety and use of multimedia devices).
Our study showed that the lockdown worsened the eating habits and physical activity of children and adolescents with overweight and obesity, also having repercussions on the psychological side.
From this emerges the need to improve the preventive measures to be taken against these children and adolescents during lockdown periods. In our survey 94% of patients said they did not feel abandoned by their doctor during this pandemic. In fact, due to the need for social distancing, the COVID-19 pandemic has temporarily reduced in-person visits for clinical care. But in our tertiary-care, interdisciplinary pediatric weight management clinic began the use of telemedicine through telephone (audio-only) visits, without a video component, to the patients to evaluate the diet, the physical activity carried out and encouraging them to measure body weight and height. In fact, a remote follow-up has also proved to be very important especially for patients with obesity and/or the chronic comorbidities of obesity.
Chronic disease requires on-going management; interruption of chronic care visits for obesity delays treatment and can lead to increased disease burden and poor outcomes (13).
Our study has several limitations. Firstly, it is a cross-sectional study and our data was acquired in a small sample through telephone interviews. Secondly, our questionnaire is not sufficiently validated, although we followed the literature to develop it (1,6-7). Finally the measurements of patients (weight and height) used for the analysis were taken and reported by the parents during the lockdown.
In conclusion, the COVID19 pandemic has had disastrous effects not only directly, but also indirectly through the lockdown especially on some categories, such as adolescents with overweight/obesity. Although lockdown is an important saving measure to limit contagion and support the health care system, the results indicate that it also causes significant changes in lifestyle, physical inactivity and psychological problems among children and adolescents with obesity/overweight.
Acknowledgments
C. Cipolla and A.B.De Logu conceived the paper and reviewed and revised the manuscript. A. Curatola, S. Ferretti, C. Condemi and G. Giugno collected data and drafted the initial manuscript. L. Birritella performed statistic analysis and drafted the manuscript. I.Lazzareschi critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Appendix Questionnaire and scores
| QUESTIONNAIRE |
| 1) How many people do you live with at home? |
| -Parents |
| -Parents and brothers/sisters |
| -Others |
| 2) Where do you live? |
| -Town |
| -Country |
| 3) Did your parents work from home? |
| -Yes, both |
| -Yes, only one |
| -No (why? Did they work in their workplace? didn’t they work at all?) |
| 4) Did you attend online lessons? |
| -Yes |
| -No |
| -Other |
| 5) Has any of your relatives or acquaintances been positive at Covid 19? |
| -No |
| -Yes, acquaintance |
| -Yes, relative |
| 6) Did you practice physical activity before the lockdown? |
| -Yes, team sport |
| -Yes, individual sport |
| -No |
| 7) If yes, how many hours a week? |
| - Two hours a week |
| -Three-four hours a week |
| - More than four hours a week |
| 8) Did you practice physical activity during this pandemic period? |
| -No |
| - Less than before |
| -Like before |
| 9) In this period, your diet has been qualitatively in your opinion |
| -Better than before |
| - Worse than before |
| -Like before |
| 10) In this period, your diet has been quantitatively in your opinion |
| -Better than before |
| - Worse than before |
| -Like before |
| 11) Do you know your weight and height before the pandemic? |
| 12) Do you know your current weight and height? |
| 13) How many meals have you eaten per day in these isolation weeks? |
| -Breakfast, snack, lunch, snack and dinner |
| -Breakfast, lunch, dinner and just one snack |
| - Breakfast, lunch, dinner |
| -More than five meals a day |
| 14) Did you have breakfast every morning? |
| -Every morning |
| -Often (at least four times a week) |
| -Sometimes (on average three times a week) |
| - Almost never (twice a week or less) |
| 15) If almost never, why? |
| - I wake up later in the morning |
| - I am not hungry in the morning |
| -Other |
| 16) Did you prepare meals by yourself during this period? |
| -Yes |
| -No |
| 17) In the family during this period |
| - You have eaten different meals than usual |
| - You followed recipes proposed online |
| -You have eaten multiple frozen meals |
| -You have eaten as before |
| 18) What foods did you eat most? |
| -Bread, pasta, pizza |
| - Desserts |
| -Meat |
| -Vegetables and fruit |
| -Fish |
| 19) What drinks did you usually consume? |
| - Fruit juices |
| -Coke |
| -Orange juice |
| -Beer |
| -Alcohol (wine) |
| -Spirits (grappa, sambuca, rhum, tequila, vodka) |
| -none |
| 20) Did you maintain the diet you followed before the pandemic? |
| -Yes |
| -No |
| 21) During this time at home how did you feel compared to before? |
| - More worried |
| -Sadder |
| -More bored |
| -Reassured by the home environment |
| -Like before |
| 22) You think that during this pandemic your parents |
| - Understood you |
| -Encouraged you |
| -Scolded you |
| 23) Since when have pandemic restrictions been in place, how changed your sleep? |
| - I sleep more and better |
| -Worsened, i can’t sleep |
| -I go to bed very late and get up late |
| -Remained the same |
| 24) During the isolation you happened to: |
| - Wake up at night to eat |
| -Eat at night because you didn’t sleep |
| -Do not feel the sense of satiety |
| -Open the fridge because of boredom and eat what you found |
| -Nothing |
| 25) During the pandemic, how many hours did you spend watching TV or playing video games? |
| -Like before |
| -Compared to before: > 2 hours |
| -Compared to before: > 4 hours |
| -Compared to before: > 6 hours |
| 26) During this pandemic period, did you feel abandoned by your doctors? |
| -No |
| -Yes, I couldn’t find them on the phone |
| -Yes, I had to skip the checkups |
| -Yes, they didn’t reply to the emails |
| -Other |
| 27) Are you taking medications or supplements? |
| -Yes (which ones?) |
| -No |
| FEEDING SCORE | |
| QUESTIONS | SCORE |
| In this period, your diet has been qualitatively in your opinion | |
| -Better than before | +1 |
| - Worse than before | -1 |
| -Like before | 0 |
| In this period, your diet has been quantitatively in your opinion | |
| -Better than before | +1 |
| - Worse than before | -1 |
| -Like before | 0 |
| How many meals have you eaten per day in these isolation weeks? | |
| -Breakfast, snack, lunch, snack and dinner | +1 |
| -Breakfast, lunch, dinner and just one snack | 0 |
| - Breakfast, lunch, dinner | -1 |
| -More than five meals a day | -1 |
| What foods did you eat most? | |
| -Bread, pasta, pizza | 0 |
| - Desserts | -1 |
| -Meat | +1 |
| -Vegetables and fruit | +1 |
| -Fish | +1 |
| What drinks did you usually consume? | |
| - Fruit juices | -1 |
| -Coke | -1 |
| -Orange juice | -1 |
| -Beer | -1 |
| -Alcohol (wine) | -1 |
| -Spirits (grappa, sambuca, rhum, tequila, vodka) | -1 |
| -none | 0 |
| PSYCHOLOGICAL SCORE | |
| QUESTIONS | SCORE |
| During this time at home how did you feel compared to before? | |
| - More worried | -2 |
| -Sadder | -1 |
| -More bored | -1 |
| -Reassured by the home environment | +1 |
| -Like before | 0 |
| You think that during this pandemic your parents | |
| - Understood you | 0 |
| -Encouraged you | +1 |
| -Scolded you | -1 |
| Since when have pandemic restrictions been in place, how changed your sleep? | |
| - I sleep more and better | +1 |
| -Worsened, i can’t sleep | -2 |
| -I go to bed very late and get up late | -1 |
| -Remained the same | 0 |
| During the isolation you happened to: | |
| - Wake up at night to eat | -2 |
| -Eat at night because you didn’t sleep | -1 |
| -Do not feel the sense of satiety | -1 |
| -Open the fridge because of boredom and eat what you found | -1 |
| -Nothing | 0 |
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):229. doi: 10.1186/s12967-020-02399-5. Published 2020 Jun 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19 related school closings and risk of weight gain among children. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: Gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007;97(4):696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Kelly AS. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin Proc. 2017;92(2):251–265. doi: 10.1016/j.mayocp.2016.09.017. [DOI] [PubMed] [Google Scholar]
- Cacciari E, Milani S, et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr) Journal of Endocrinological Investigation. 2006;29:581–593. doi: 10.1007/BF03344156. [DOI] [PubMed] [Google Scholar]
- Osler M, Heitmann BL. The validity of a short food frequency questionnaire and its ability to measure changes in food intake: a longitudinal study. Int J Epidemiol. 1996 Oct;25:1023–9. doi: 10.1093/ije/25.5.1023. [DOI] [PubMed] [Google Scholar]
- Husain W, Ashkanani F. Does COVID-19 change dietary habits and lifestyle behaviours in Kuwait: a community-based cross-sectional study. Environ Health Prev Med. 2020 Oct 12;25(1):61. doi: 10.1186/s12199-020-00901-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García OP, Long KZ, Rosado JL. Impact of micronutrient deficiencies on obesity. Nutr Rev. 2009;67:559–72. doi: 10.1111/j.1753-4887.2009.00228.x. [DOI] [PubMed] [Google Scholar]
- Childs CE, Calder PC, Miles EA. Diet and immune function. MDPI AG: Nutrients. 2019 doi: 10.3390/nu11081933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Lorenzo A, Gratteri S, Gualtieri P, Cammarano A, Bertucci P, Di Renzo L. Why primary obesity is a disease? Transl Med. 2019;17:169. doi: 10.1186/s12967-019-1919-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhurandhar NV, Bailey D, Thomas D. Interaction of obesity and infections. Obes Rev. 2015;16:1017–29. doi: 10.1111/obr.12320. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara VM, Johnston SV, Browne NT. The paediatric weight management office visit via telemedicine: pre-to post-COVID-19 pandemic. Pediatr Obes. 2020;15(8):e12694. doi: 10.1111/ijpo.12694. [DOI] [PMC free article] [PubMed] [Google Scholar]


