Abstract
The focus of this study was on the differences between older adults who complied with a clinical recommendation for hearing-aid acquisition (adherents; N = 105) and those who did not (nonadherents; N = 34) among a group of research volunteers from the community. All participants were first-time hearing-aid users. Differences between adherents and nonadherents were examined across several domains, including demographic variables, audiometric measures, measures of affect and personality, cognitive variables, hearing-aid expectations, and the perceived hearing difficulties of the older adults and their adjustments to those difficulties. It was found that the adherents differed significantly (p < .05) from the nonadherents primarily in their perceived difficulties and reactions to them as well as their expectations for hearing aids. Importantly, the pattern of differences between the adherents and nonadherents was primarily confined to measures that could potentially be shaped by appropriate counseling and education of the older adult. In a secondary analysis, among the 105 adherents, a small group (N = 21) returned their hearing aids for credit with 15 of them completing the outcome measures at the end of a 1-month trial period. When comparisons were made between the adherents who kept their hearing aids (N = 84) and those who returned them, the primary differences between these two groups of adherents were in the poorer aided outcomes obtained by those who returned their devices.
Keywords: aging, hearing aids, adherence
The prevalence of hearing loss increases with advancing age (Cruickshanks et al., 2010; Lin et al., 2011) and about 20% of persons age 60 and 50% age 80 years are affected by disabling hearing impairment worldwide (Stevens et al., 2013). These prevalence estimates, defined as disabling hearing impairment by the World Health Organization (Stevens et al., 2013), were based on the pure-tone average for 500, 1000, 2000 and 4000 Hz (PTA4) in the better ear ≥ 35 dB HL. Despite the widespread prevalence of disabling age-related hearing loss, industry surveys and epidemiological studies have consistently documented that only about 15% to 30% of adults with mild-to-moderate hearing loss obtain hearing aids (Bainbridge & Ramachandran, 2014; Bisgaard & Ruf, 2017; Chia et al., 2007; Chien & Lin, 2012; Dalton et al., 2003; Dawes et al., 2014; Kochkin, 1993a, 1993b, 1993c, 2000, 2009; Popelka et al., 1998; Sangster et al., 1991; Smeeth et al., 2002; Ward et al., 1993; Wilson et al., 2010) with even lower rates of hearing-aid uptake among those with Hispanic/Latino backgrounds in the United States (e.g., Arnold et al., 2019).
Factors found to positively influence older adults’ help-seeking and their subsequent decision to at least try hearing aids are perceived hearing difficulties, increasing age, positive attitudes toward hearing aids and support from significant others, with perceived difficulties and need for help being the most impactful factors for uptake (Hickson et al., 2014; Knudsen et al., 2010; Laplante-Levesque et al., 2012; Meyer & Hickson, 2012; Pronk et al., 2017, 2019; Ratanjee-Vanmali et al., 2019; Ridgway et al., 2016; Sawyer, Armitage, et al., 2019; Simpson et al., 2019; Tahden et al., 2018). Stigma associated with hearing impairment and the visibility of hearing aids have also been shown to influence hearing-aid uptake (Southall et al., 2010; Wallhagen, 2010). Of those who do take up hearing aids, about 15% typically return them at the end of the 4-to-6-week trial period in the United States with the remaining 85% reporting current hearing-aid use (e.g., Kochkin, 2000). Of those who self-report current hearing-aid use, however, some may use their hearing aids no more than 1 h per day (Aazh et al., 2015). These findings have been confirmed again recently for the United States in MarkeTrak 10 (Powers & Rogin, 2020). MarkeTrak 10 reported that 23% of prior hearing-aid owners were not current owners with about one third of these individuals rejecting hearing aids after a trial and the balance doing so sometime later after acquisition. In addition, of the 77% who were current hearing-aid owners in MarkeTrak 10, wide ranges of usage were reported. Specifically, 72% of the current hearing-aid owners reported daily usage (with no indication of hours used per day), 17% weekly, declining to 2.7% who reported never using them. Clearly, current hearing-aid ownership does not necessarily equate to daily usage which is often considered another form of adherence to clinical recommendations. This form of adherence differs from the adherence to the recommendation to try hearing aids that is addressed here.
A wide range of factors have been examined to explain the low level of hearing-aid usage by hearing-aid owners. Difficulty handling the devices, perhaps due to dexterity challenges or low self-efficacy, lack of family support, lack of perceived need for hearing assistance, and less-than-desired benefits, especially for speech communication in noisy backgrounds, have often emerged as contributing factors to less than optimal hearing-aid usage by some older adults (Hickson et al., 2014; Humes et al., 2003; Jilla et al., 2020). Of course, as noted in prior discussions of hearing-aid outcome measures (e.g., Humes & Humes, 2004; Humes & Krull, 2012), successful or optimal usage of hearing aids can be challenging to define. Moving forward, as devices become more broadly available to those with milder amounts of hearing impairment, such definitions will likely prove to be even more challenging. Whereas usage for 1 to 2 h/day might be considered suboptimal for those with severe hearing loss, this same amount of usage may be quite appropriate for an older adult with mild impairment.
Due to the poor uptake and usage of hearing aids, millions of older adults with untreated hearing loss continue to suffer broader consequences. It is well known that untreated hearing loss results in reduced speech audibility. This, in turn, causes many difficulties for everyday speech communication, including poor speech perception (e.g., Humes & Dubno, 2010) and increased listening effort (e.g., Pichora-Fuller et al., 2016), among others. Untreated hearing loss can lead to a variety of psychosocial problems, including social isolation (Mick et al., 2018), with most studies focusing on depression associated with hearing loss (e.g., Cosh et al., 2019). There is mounting evidence, moreover, that untreated hearing loss can have a negative impact on cognitive function and that hearing aids may help to reduce that impact (Livingston et al., 2020; Sarant et al., 2020). Amieva and Ouvrard (2020) provide a recent comprehensive review on this topic. In summary, the poor uptake and usage of hearing aids by older adults with mild-to-moderate hearing loss is a serious problem with broad potential consequences on everyday function and well-being.
In most analyses of the impact of hearing aids on function, the starting point is to define the pool of potential hearing-aid candidates using audiometric criteria. It has long been known, however, that older adults with identical audiograms can have markedly different perceived hearing difficulties (e.g., Ventry & Weinstein, 1982, 1983; Weinstein & Ventry, 1983). If one assumes that the primary factor leading an older adult to seek help is perceived hearing loss, as noted earlier, then recent analyses by Edwards (2020) suggest that about 33% of those with measurable audiometric hearing loss also have perceived difficulties and seek clinical assistance. This is consistent with the observation, from analyses of data from over 10,000 older adults, that there is about 36% shared variance between self-report and pure-tone measures of impaired hearing (Humes, 2020, in press; Humes et al., 2020). In other words, among older adults with perceived hearing difficulties there is corroborating evidence from the audiogram to support the presence of a disabling hearing loss in about one third of the individuals. Importantly, the remaining two thirds of those with perceived hearing difficulties but less than disabling hearing loss audiometrically typically were not considered to be viable hearing-aid candidates (Edwards, 2020). It has been suggested that perceived hearing difficulties should determine candidacy for intervention rather than relying on audiometric criteria for candidacy (Humes, 2020, in press), especially for most older adults with milder amounts of audiometrically defined hearing loss. This will take on even more importance in the near future in the United States as a result of the implementation of the Over-The-Counter Hearing Aid Act of 2017 which defines device candidacy based on perceived mild-to-moderate hearing difficulty. Furthermore, as noted earlier, perceived hearing difficulties have repeatedly been identified as the key factor for hearing-aid uptake and use.
Perhaps, the most detailed assessment of perceived hearing difficulties, as well as the individual’s reaction to those difficulties, is provided by the Communication Profile for the Hearing Impaired (CPHI; Demorest & Erdman, 1986, 1987). The full CPHI includes 163 items and 25 scales, which comprise 5 subsets of scales organized around common themes of communication performance (CP), communication importance, communication environment (CE), communication strategies (CS), and personal adjustment (PA) to impaired hearing. Generally, the key factors that influence scores on many of the CPHI scales among older adults are the severity of hearing loss, age, and education level, with mixed findings regarding the influence of gender (Erdman & Demorest, 1998; Garstecki & Erler, 1999).
Two studies have examined differences in CPHI scores between older adults seen at the audiology clinic who were advised to pursue hearing aids and did (adherents) and those who received the same advice but chose not to do so (nonadherents). Garstecki and Erler (1998) obtained CPHI scores from 60 older adults (35 females) who were adherents and 71 older adults (33 females) who were nonadherents. The results were analyzed separately for females and males. Regarding the CPHI scale scores, although there were some significant differences between adherents and nonadherents with the specific pattern varying for each gender, such significant differences were not frequent (two differences among females and one among males). Given the infrequent emergence of significant differences between adherents and nonadherents across the 25 CPHI scales, however, one would have to conclude that differences in perceived hearing difficulties between these two groups were minimal. It should be noted, however, that there were group differences in severity of hearing loss and age between the adherents and nonadherents in the study by Garstecki and Erler (1998) and these were not controlled statistically when examining the differences in CPHI scale scores between adherents and nonadherents.
Humes et al. (2003) examined differences in CPHI scores among three groups of older adults who were matched for average audiograms, age, and gender. Performance of one group of nonadherents (N = 26) was compared with two groups of adherents, one group who had accepted hearing aids after the 30-day trial period and was still using them 6 months later (N = 26) and one group who had discontinued using their hearing aids 6 months later (N = 24), about half of whom returned their hearing aids during the initial 30-day trial. Significant differences in CPHI scale scores were observed for five scales, four of which were PA scales, with the nonadherents differing significantly from the other two groups who had at least tried hearing aids. As noted by Humes et al., the pattern of differences was such that nonadherents had poorer awareness of communication problems (CP-problem awareness), greater denial of communication problems (PA-denial), better self-acceptance of their difficulties (PA-self acceptance), less stress from their communication difficulties (PA-stress), and were less prone to exaggerating the responsibilities for their communication problems (PA-exaggerated responsibility) compared with adherents. It should be kept in mind that, due to the matching of each group for hearing loss, age, and sex, these variables did not contribute to the group differences in CPHI scale scores observed between the nonadherents and adherents.
This study examined differences between adherents and nonadherents for the CPHI as in these prior two studies. The focus here was on older adults who had never worn hearing aids previously, referred to here as new hearing-aid users. A total of 139 older adults participated in this study with 34 not adhering to the recommendation to purchase hearing aids whereas the remaining 105 did so. Differences between these two groups of older adults, adherents and nonadherents, were not confined, however, to the CPHI. As in Garstecki and Erler (1998) and Humes et al. (2003), a much broader range of measures was explored. Here, these additional measures included level of education and socioeconomic status together with standardized measures of affect, personality, cognition, and hearing-aid expectations. Because of group differences in hearing loss between the adherents and nonadherents in these analyses, as well as the known effects of hearing loss on many of these measures, all statistical comparisons between adherents and nonadherents made use of statistical controls for hearing loss. That is, once hearing-loss severity was controlled statistically, remaining differences between the adherents and nonadherents were examined.
At completion of the 1-month hearing-aid trial, the 105 adherents decided whether to keep their hearing aids. A total of 21 participants returned their hearing aids, 6 of whom returned their hearing aids prior to completion of the 1-month trial. The differences between these two subgroups of adherents will also be examined here, as was done in Humes et al. (2003). Because of the relatively small number who had rejected the use of hearing aids after acquiring them, these analyses are secondary to the primary focus on the differences between the 105 adherents and the 34 nonadherents.
Finally, as described in more detail later, the participants in this study were recruited for a study for which they would be asked to purchase hearing aids if they met the study’s eligibility requirements. These volunteers may or may not be representative of the broader population of older adults with untreated hearing loss who have not as yet sought out hearing aids. All participants in this study, however, were recruited identically and volunteered for this research study. The primary focus of these analyses is on the differences between two subgroups of these study volunteers: those who did and did not adhere to the recommendation to acquire hearing aids.
Methods
Participants
The participants were recruited for a study on hearing-aid outcome measures via newspaper ads, flyers posted in the community, printed announcements in church/synagogue bulletins, and word of mouth. The focus of this main study was on individual differences in hearing-aid outcomes and in group differences in outcomes for different technologies. Much of these data were published in a series of prior reports (Humes et al., 2009, 2010). The focus of this study was an analysis of differences between participants who adhered to the recommendation to try hearing aids and those who did not as well as differences between those who kept or returned their hearing aids after agreeing to try them. All participants enrolled met the following inclusion criteria: (a) age between 60 and 89 years; (b) hearing loss that was flat or gently sloping (from 250 to 4000 Hz, no interoctave change in hearing thresholds of more than 20 dB); (c) hearing loss that was of sensorineural origin (normal tympanometry and air-bone gaps no greater than 10 dB at three or more frequencies); (d) hearing loss that was bilaterally symmetrical (interaural difference within 30 dB at all octave and half-octave intervals from 250 to 4000 Hz); (e) pure-tone thresholds within the following ranges at frequencies of 250, 500, 1000, 1500, 2000, 3000, 4000, and 6000 Hz, respectively: 5–85, 5–85, 10–90, 20–95, 25–95, 30–120, 30–120, and 30–120 dB HL (American National Standards Institute, 2004); (f) no known medical or surgically treatable ear-related condition; (g) no known fluctuating or rapidly progressing hearing loss; (h) no cognitive, medical, or language-based conditions that may have limited the participant’s ability to complete the procedures used in the longitudinal study of outcome measures; (i) no use of medications that could affect hearing or cognition; and (j) completion of a signed medical clearance form, or waiver of such by the participant, and a signed informed consent form. The consent form and all procedures used in this study were approved by the Indiana University-Bloomington Institutional Review Board.
From 2004 to 2008, there were a total of 530 individuals who responded to the ads and were screened for study eligibility. Of these, 162 (30.6%) were ineligible. Of the remaining 368 eligible individuals, 154 (42.3%) enrolled and purchased hearing aids. This percentage of adherents to the recommendation to purchase hearing aids appears to be very similar to that of the general clinical population. For example, of the 1,382 older adults recruited from outpatient clinics in Yueh et al. (2010), 15.5% were considered by the audiologist to have aidable hearing loss and uptake was recommended. Of these, 40.2% obtained hearing aids which corresponds closely to the 42.3% who did so here. They paid the full purchase price for the devices at the time of enrollment. Of the 214 eligible candidates who did not enroll, the top four reasons indicated for not doing so were as follows: “considering” hearing aids but still uncertain (43.9%), not interested in hearing aids (35.0%), interested but wants some other style or type of hearing aid (20.6%, a quarter of whom were currently wearing hearing aids and opted to retain them), and cost (7.9%). Of the 214 eligible candidates who opted not to purchase hearing aids and enroll, 36 agreed to return to complete several of the prefit measures completed by the hearing-aid purchasers. The 36 are referred to here as “nonadherents” as they did not adhere to the recommendation to try hearing aids after the initial screening.
There were 154 older adults who met inclusion criteria for this study, enrolled, and purchased hearing aids. When combined with the 36 nonadherents, the total N was 190. Of these, 3 had missing demographic information and were deleted, leaving 187 total. Of these 187, 48 had worn hearing aids previously and were excluded from the present analyses. The remaining 139 participants self-reported no prior hearing-aid use, 105 of whom adhered to the clinician’s recommendation to acquire hearing aids and 34 who did not. The 105 adherents (44 females) had a mean age of 74.7 years (standard deviation [SD] = 7.7 years) and the 34 nonadherents (18 females) had a mean age of 72.7 years (SD = 7.0 years). The group differences in mean age, t(137) = 1.34, p > .10, and gender composition, χ2(1) = 1.27, p > .10, were not significant.
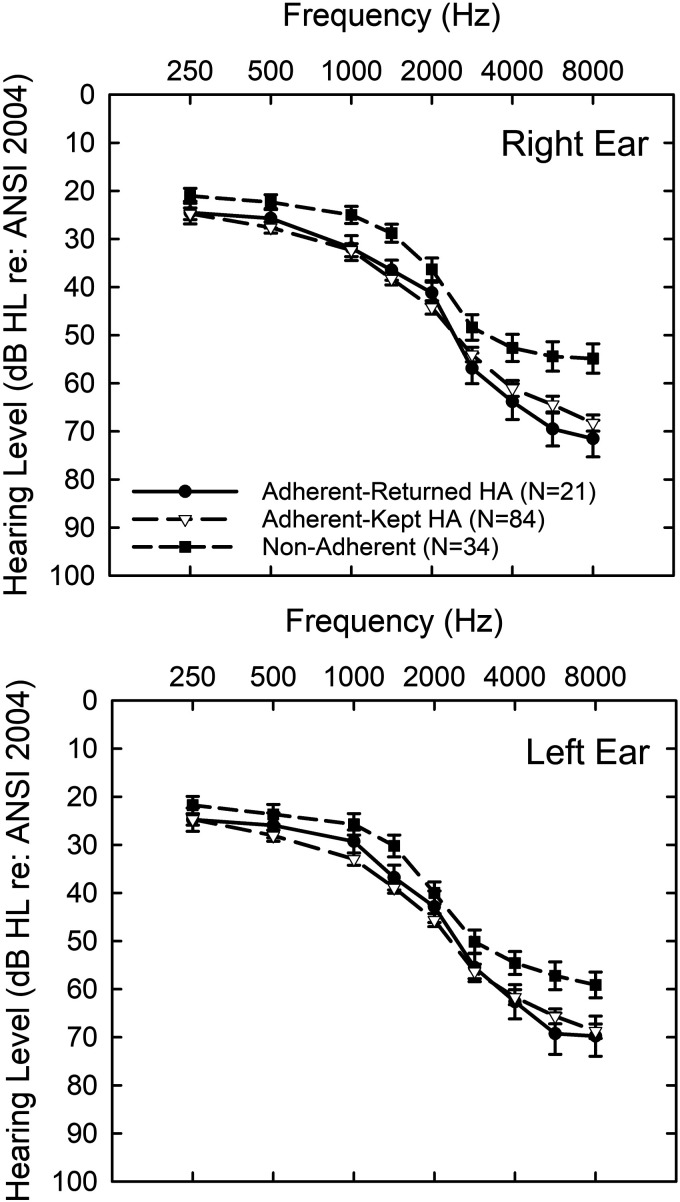
Figure 1 presents the means and standard errors for the air-conduction pure-tone thresholds obtained from the 34 nonadherents (filled squares) and two subgroups of the 105 adherents; those who returned their hearing aids (N = 21; filled circles) and those who kept their hearing aids (N = 84; unfilled triangles). Audiograms for the right ear are shown in the top panel and for the left ear in the bottom panel of Figure 1. A univariate analysis of variance was conducted for each ear and frequency, 18 total analyses of variance, with follow-up t tests for each paired group comparison. The overall effect of group was evaluated using a Bonferroni adjustment for multiple comparisons such that alpha < .05/18 or .0028 was required for significance. Moreover, when those significant analyses of variance were examined using follow-up paired comparisons, the paired comparisons were also Bonferroni adjusted p values < .05. The hearing thresholds for the two subgroups of adherents did not differ significantly (p > .05) in either ear at any frequency. The hearing thresholds of the nonadherents, however, were significantly (p < .05) better than those from both subgroups of adherents at 8000 Hz in the right ear, better than the adherents who returned their hearing aids in the right ear at 6000 Hz, and better than the adherents who kept their hearing aids at 1500 Hz in both ears. When the pure-tone audiometric data were reduced to four-frequency pure-tone averages (mean of 500, 1000, 2000, and 4000 Hz; PTA4) for each ear and general linear model (GLM) analyses were performed with ear and group as factors the main effect of ear was not significant, F(1, 136) = 1.40, p > .1, nor was the interaction between ear and group, F(2, 136) = 0.95, p > .1. There was, however, a significant main effect of group, F(2, 136) = 6.69, p < .01, and follow-up paired-comparison t tests found that the sole significant difference (p < .01) was that the nonadherents had better PTA4 values (M = 32.3; SD = 8.4 dB HL) than those adherents who kept their hearing aids (M = 39.4; SD = 9.2 dB HL). Differences in several additional demographic characteristics among participant groups are reported in “Results”.
Figure 1.
The Means and Standard Errors for the Air-Conduction Pure-Tone Thresholds Obtained From the 34 Nonadherents (Filled Squares) and Two Subgroups of the 105 Adherents; Those Who Returned Their Hearing Aids (N = 24; Filled Circles) and Those Who Kept Their Hearing Aids (N = 81; Unfilled Triangles). Audiograms for the right ear are shown in the top panel and for the left ear in the bottom panel. ANSI = American National Standards Institute.
Procedures
All participants completed a case history and audiological evaluation to determine eligibility for the study during Session 1. The audiological evaluation included immittance measurements, pure-tone audiometry by air and bone conduction, and speech audiometry (speech recognition threshold and suprathreshold word-recognition testing). After completion of this initial 90- to 120-min session, the study of hearing-aid outcomes was explained, which included the purchase of two hearing aids, and they provided their informed consent to participate and purchased the devices. Those who were eligible and declined to participate in the study of hearing-aid outcomes were asked if they would consider participating in an abbreviated study not requiring the purchase of hearing aids. Those who agreed, as well as those who enrolled in the hearing-aid outcomes study, completed the next two sessions, Sessions 2 and 3, each 90 to 120 min in length.
During the next session, a variety of unaided measures were completed, including sound-field speech-in-noise testing, acceptable noise level (ANL; Nabelek et al., 1991, 2006), the Communication Profile of Hearing Impairment (CPHI; Demorest & Erdman, 1986, 1987), the Expected Consequences of Hearing Aid Ownership (ECHO; Cox & Alexander, 2000), and an abbreviated version of the Glasgow Hearing Aid Benefit Profile (GHABP; Gatehouse, 1999). Each of these measures is described in more detail, together with the details of data reduction using principal-components factor analysis (Gorsuch, 1983), in Appendix.
The final prefit 90- to 120-min session, Session 3, included a range of psychological measures. The full third edition of the Wechsler Adult Intelligence Scale (WAIS-III; Wechsler, 1997) was completed to provide a broad assessment of cognitive function. This was followed by three measures of the participant’s affect and a standardized measure of personality. Additional details for each of these measures and the reduction of those data via factor analyses can be found in Appendix.
For those who had enrolled and purchased hearing aids, another three 90- to 120-min sessions were completed. The first of these, Session 4, was devoted to fitting the hearing aids using real-ear insertion gain (REIG) and National Acoustics Laboratory’s Non-Linear 1 (NAL-NL1; Dillon et al., 1998) targets for 65 dB speech input, completing a hearing-aid orientation session with the audiologist, and receiving instructions in the use of the supplied daily log of hearing-aid usage. The technology used varied among one of the three options. One group received four-channel wide-dynamic-range-compression circuits housed in full-concha in-the-ear shells, half with directional microphones and half with omni-directional microphones. The other group received six-channel open-fit mini behind-the-ear devices with directional microphones. The directional microphones were a fixed supercardioid configuration, and its function was verified using Verifit software and hardware (Etymonic Design, Dorchester, Canada).
The same basic protocol was used to set and verify target gain for each participant in each group. First, based on audiological information obtained from each participant (air-conduction and bone-conduction hearing thresholds, as well as loudness discomfort levels), target 2-cm3-coupler gain values were generated at octave intervals from 250 through 4000 Hz, as well as at 1500, 3000, and 6000 Hz. Hearing aids were adjusted in the 2-cm3 coupler for a moderate level input (60–70 dB SPL, across studies) to match target in the coupler and were then fitted to the patient and verified using real-ear probe-tube microphone measurements with adjustments to better match the real-ear targets performed as needed.
The prescriptive procedure used to generate gain targets was NAL-NL1. With each group and technology, software from NAL was used to generate NAL-NL1 targets, rather than the manufacturer’s version of that prescriptive protocol. Within a given group of participants, all were fitted bilaterally with identical make and models of hearing aids. In addition, participants paid the typical clinic price for the devices at the time of delivery and then were paid as research subjects for return visits during which they completed a variety of outcome measures.
After verification of real-ear gain, the participant was counseled about the use, function, and care of the hearing aids. Approximately 2 weeks postfit, the participant returned for a follow-up evaluation of the devices and an unaided speech-recognition measure (Session 5; Online Appendix) and at 1-month postfit, the participant returned to complete several outcome measures (Session 6). The outcome measures completed at Session 6 included the Hearing Aid Performance Inventory (HAPI; Walden et al., 1984), the Satisfaction with Amplification in Daily Life (SADL; Cox & Alexander, 1999), the GHABP, a 42-item hearing-aid satisfaction survey based on the MarkeTrak IV (Humes et al., 2001; Kochkin, 1996), as well as aided (and unaided) Connected Speech Test (CST) scores. As noted, reports for several of the conventional outcomes have been published previously for subsets of the study sample reported here, as well as other samples, with a focus on differences in outcomes for various technologies (Humes et al., 2009, 2010) and individual differences in outcomes (Humes & Krull, 2012).
As noted, 105 eligible individuals who had never worn hearing aids previously purchased hearing aids at the end of Session 1 and paid the full price for the devices at that time. The devices were fitted in Session 4 and participants were paid $150/session for completion of each of the subsequent sessions. By completing Sessions 5 and 6, the participants would have received $300 which represented about 20% of the purchase price of the devices. At the end of the last session (Session 6), participants were asked if they wished to keep their hearing aids or return them for a full refund. Of the 105 individuals who had never worn hearing aids previously, 84 opted to keep their devices and the remaining 21 (20%) returned them. Of these 21, 6 decided to return them prior to completing the outcome measures in the final session after 1 month of usage. Complete outcome measures were available for 98 of the 99 remaining individuals, 84 who kept their hearing aids and 15 who did not.
Results
Comparisons of Adherents to Nonadherents
Demographic Measures
As noted in “Methods”, there were no significant differences in age or the percentage of females between the group of adherents and nonadherents, but there were significant differences in the severity of hearing loss with the nonadherents having milder hearing loss. Nonparametric Mann–Whitney U tests were performed to examine differences in several ordinal demographic measures. There were no significant differences between the adherents and nonadherents for education level, income level, or duration of hearing loss (all Mann–Whitney U > 2,138, p > .05/3 or .0167). The nonadherents had a median self-reported education level corresponding to “a college degree” whereas the median for the adherents was “some graduate school” with both groups exhibiting a wide range from “less than high school education” to “doctorate or medical degree.” For the self-reported annual income, both groups exhibited responses ranging from $5,000–$15,000 to >$45,000 with the median for the adherents being “>$45,000” and the median response for the nonadherents was $35,000. For the duration of hearing loss, an open-response format was used. The adherents self-reported having a hearing loss from 0 to 50 years with a median of 5 years, whereas nonadherents had a range of 0 to 18 years and a median of 3 years.
Affect and Personality Measures
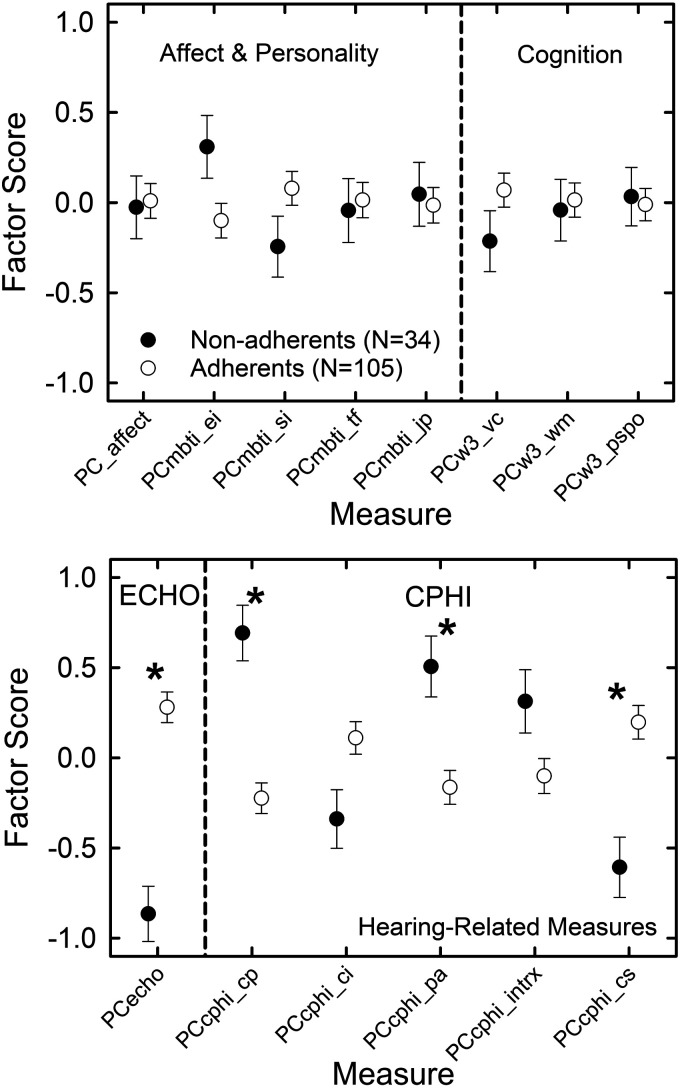
As described in Appendix, given the large number of prefit measures available, several principal-components factor analyses were performed for data reduction. The 13 measures of affect and personality were reduced to 5 principal components (PCs) and the labels for each of these 5 PCs are provided in Table 1. All five measures of affect loaded on the first PC with the remaining four PCs representing each of the four personality dimensions from the Myers-Briggs Type Indicator. GLM analyses were then conducted to examine the effects of group on each of the five PCs for affect and personality with Bonferroni correction for multiple comparisons. Given the difference in hearing loss noted previously between the adherent (N = 105) and nonadherent (N = 34) groups (Figure 1), better-ear PTA4 served as a covariate in all GLM analyses of group effects. No effects of group were significant, all F(1, 136) < 4.07, p > .01. The left-hand portion of the top panel in Figure 2 provides the estimated marginal means and standard errors for each of the five PCs representing affect and personality.
Table 1.
Measures of Affect, Personality, and Various Cognitive Functions With the Labels for the PCs That Emerged From the Factor Analyses Described in Appendix.
| Measure type | Measure | PC label |
|---|---|---|
| Affect | LOT-R, PANAS-positive, PANAS-negative, STAI-state, STAI-trait | PC_affect |
| Personality | MBTI-extraversion, MBTI-introversion | PCmbti_ei |
| MBTI-sensing, MBTI-intuition | PCmbti_si | |
| MBTI-thinking, MBTI-feeling | PCmbti_tf | |
| MBTI-judging, MBTI-perceiving | PCmbti_jp | |
| Verbal comprehension | WAIS-III-vocabulary, WAIS-III-similaritiesWAIS-III-information, WAIS-III-comprehension | PCw3_vc |
| Working memory | WAIS-III-arithmetic, WAIS-III-digit span, WAIS-III-letter number sequence | PCw3_wm |
| Processing speed and perceptual organization | WAIS-III-digit symbol coding, WAIS-III-symbol search, WAIS-III-picture completion, WAIS-III-block design, WAIS-III-matrix reasoning, WAIS-III-picture arrangement | PCw3_pspo |
Note. Details of each measure, including references for each, can also be found in Appendix. PC = principal components; LOT-R = Life Orientation Test-Revised; PANAS = Positive and Negative Affect Scale; STAI = State-Trait Anxiety Inventory; MBTI = Myers-Briggs Type Indicator; WAIS-III = Wechsler Adult Intelligence Scale, 3rd Edition.
Figure 2.
Estimated Marginal Means (Circles) and Standard Errors (Error Bars) for Nonadherents (Filled) and Adherents (Unfilled) From the GLM Analyses with Better-Ear PTA4 as a Covariate. The top panel shows the results for the PCs for affect, personality, and cognition. The bottom panel shows the results for the PCs for two of the hearing-related measures, the ECHO and the CPHI. Asterisks mark significant differences between the two groups. The labels for each of the PCs shown as the measures along the x-axis are provided in Tables 1 and 2. PC = principal component; ECHO = Expected Consequences of Hearing Aid Ownership; CPHI = Communication Profile for the Hearing Impaired.
Cognitive Measures
The factor analysis of the 13 WAIS-III scales (see Appendix) resulted in three PCs, one representing measures of verbal comprehension, one representing working memory, and one including measures of processing speed and perceptual organization. Table 1 shows the labels for each of the three PCs that emerged as well as the WAIS-III scales represented by each PC. GLM analyses of the effects of group, controlling for better-ear PTA4, again found no significant differences (criterion p value = .05/3 or .0167) between adherents and nonadherents, all F(1, 136) < 2.08. This is readily apparent in the plot of estimated marginal means and standard errors from this analysis as shown in the right-hand portion of the top panel of Figure 2.
Hearing-Related Measures
There were several hearing-related measures completed by all participants, including unaided measures of ANL and open-set speech recognition in babble (CST). Separate GLM analyses for each of these dependent measures with better-ear PTA4 as a covariate found no significant differences between the adherents and nonadherents, both F(1, 136) < 3.33, p > . 05.
As noted in Appendix, a single PC emerged from the factor analysis of the four ECHO scales. A very large, partial Eta-squared (ηp2 = .23), and significant, F(1, 136) = 41.3, p < .001, effect of group was observed for the ECHO with nonadherents having lower expectations for hearing aids than adherents. This is revealed in the left-hand portion of the bottom panel of Figure 2. Given this significant difference between adherents and nonadherents on the overall ECHO PC from the factor analysis, group differences were examined separately for each of the four ECHO scales using separate GLM analyses, each with better-ear PTA4 as a covariate. Significant differences based on a Bonferroni adjusted p value of .0125 (.05/4) were observed for three of the four ECHO scales, all three F(1, 136) > 6.48, with the nonadherents having lower expectations than the adherents in all three cases. For the three significant effects of group, one (positive effects) was a large effect (ηp2 = .34) and the other two (service and cost, personal image) were medium effects (ηp2 = .09 and .05, respectively; Cohen, 1988). The effect of group was not significant for the negative effects subscale of the ECHO, F(1, 136) = 5.33.
Table 2 shows the PCs that emerged from the factor analysis of the 23 CPHI scale scores. The factor analysis reduced the 23 scale scores to 5 PCs with Table 2 showing the scales that loaded on each of the PCs together with the label for each of the PCs. The loadings of the scale scores on each PC correspond to measures of communication performance (CP), communication importance, personal adjustment (PA) to hearing impairment, communication strategies (CS), and interactions with others which is captured primarily in the scales assessing communication environment (CE). Significant effects of group were observed for three of the five CPHI PCs based on GLM analysis with better-ear PTA4 as a covariate and a criterion p value of .05/5 = . 01: PCcphi_cp, PCcphi_pa, and PCcphi_cs, all F(1, 136) > 11.6. As shown in the right-hand portion of the bottom panel of Figure 2, based on the estimated marginal means for these three CPHI PCs with significant group effects, adherents had significantly lower factor scores than nonadherents for PCcphi_cp and PCcphi_pa, but this was reversed for PCcphi_cs.
Table 2.
Measures From the CPHI With the Labels for the Five PCs That Emerged From the Factor Analysis Described in Appendix
| Measure type | Measure | PC label |
|---|---|---|
| CP | CPHI-CP-social; CPHI-CP-work, CPHI-CP-home | PCcphi_cp |
| CI | CPHI-CI-social, CPHI-CI-work, CPHI-CI-home, CPHI-CE-need (negative loading) | PCcphi_ci |
| PA | CPHI-PA-self accept, CPHI-PA-accept loss, CPHI-PA-anger, CPHI-PA-displaced responsibility, CPHI-PA-exaggerated responsibility, CPHI-PA-discouragement, CPHI-PA-stress, CPHI-PA-withdrawal, CPHI-PA-denial (negative loading), CPHI-CP-problem awareness | PCcphi_pa |
| Interactions with others | CPHI-CE-physical characteristics, CPHI-CE-attitudes others, CPHI-CE-behavior others; CPHI-CS-maladaptive behaviors | PCcphi_intrx |
| CS | CPHI-CS-verbal strategies, CPHI-CS-nonverbal strategies | PCcphi_cs |
Note. Details can be found in Appendix. CPHI = Communication Profile of the Hearing Impaired; PC = principal components; CP = communication performance; CI = communication importance; PA = personal adjustment; CE = communication environment; CS = communication strategies.
Given the number of significant group differences for the CPHI PCs, differences between groups were examined in more detail using a separate GLM analysis of group for each of the 23 CPHI scale scores. Better-ear PTA4 again served as a covariate in each of these analyses and given 23 analyses an adjusted p value of .05/23 or .0022 was used as the criterion p value for significance. Ten of the 23 analyses showed significant differences between the adherents and nonadherents, all F(1, 136) > 10.1, including all four of the CP scales, two of the three CS scales (CS verbal and CS nonverbal), and four of the nine PA scales (PA self-acceptance, PA exaggerated responsibility of others, PA withdrawal, and PA denial). Partial eta-squared values revealed that half the effect sizes for the significant group differences were large effects and half were medium effects (.07≤ηp2≤.23; Cohen, 1988). For 6 of the 10 significant differences, the adherents had higher scale scores than the nonadherents, whereas the opposit was true for the other 4. In particular, the nonadherents had lower scale scores than the adherents for use of verbal and PA nonverbal CS as well as CP problem awareness and denial.
Comparisons of Adherents Who Kept Hearing Aids to Those Who Did Not
As noted, of the 105 adherents, 84 opted to try hearing aids and kept them, whereas 21 tried hearing aids but returned them. The group of 84 who accepted their hearing aids and the 21 who rejected them completed all the same measures reported earlier including the measures of affect, personality, cognitive function, the ANL, the CST, the ECHO, and the CPHI. Because these two subgroups of adherents, those accepting and those rejecting hearing aids, did not differ significantly in age, t(103) = −0.85, p > .1, or better-ear PTA4, t(103) = −0.54, p > .1, no covariates were used when making the group comparisons. As a result, independent-sample t tests were computed to compare the performance of these two subgroups of adherents on all measures with Bonferroni adjustment of p values as in the foregoing comparisons of adherents to nonadherents. The two subgroups of adherents also did not differ significantly (p > .05) regarding the percentage of females, level of education, annual income, or duration of hearing loss. The t tests for the five affect and personality PCs and three WAIS-III PCs in Table 1, the five CPHI PCs in Table 2, the single PC for the ECHO, as well as the individual ANL and CST scores, all failed to show significant differences between those who kept and those who returned their hearing aids.
Of the 21 adherents who rejected their hearing aids and returned them for a refund, 15 did so at the end of the study after completing a large battery of outcome measures. This included six measures of self-reported hearing-aid satisfaction, five self-report measures of hearing-aid benefit, two measures of hearing-aid usage, and two measures pertaining to aided performance in noise as detailed in “Methods”. Table 3 shows the means and SDs for the 15 outcome measures completed after wearing the hearing aids for 6 weeks. The measures are grouped by the outcome dimension tapped by the measures. The top group, for example, shows six measures of self-reported satisfaction with hearing aids, one from the GHABP, one from the hearing-aid satisfaction survey, and four from the SADL. Four of the six differed significantly, all t(96) > −3.9, p < .05/15 = . 0033, between the two groups of adherents with those rejecting the hearing aids reporting less satisfaction except for the SADL measures of service-and-cost and personal image.
Table 3.
Means (M) and SDs for the 84 Adherents Who Kept Their HAs and the 15 Who Did Not (Rejected HAs) on 15 Outcome Measures Completed at 1-Month Postfit.
| Type of measure | Measure | Reject HA M | Reject HA SD | Kept HA M | Kept HA SD |
|---|---|---|---|---|---|
| Satisfaction | GHABP-sat | 1.8 | 0.8 | 3.1 | 0.8 |
| HASS-global | 3.0 | 0.4 | 3.6 | 0.6 | |
| SADL-pos eff | 2.2 | 1.0 | 4.0 | 1.3 | |
| SADL-serv cost | 4.6 | 0.8 | 4.8 | 0.9 | |
| SADL-neg feat | 3.3 | 1.1 | 4.3 | 0.9 | |
| SADL-pers img | 5.4 | 1.3 | 5.7 | 0.9 | |
| Benefit | GHABP-help | 1.8 | 0.7 | 2.8 | 0.9 |
| HAPI-sp noise | 3.4 | 0.9 | 2.5 | 0.7 | |
| HAPI-sp quiet | 2.7 | 0.9 | 2.2 | 0.7 | |
| HAPI-red cue | 2.9 | 0.7 | 2.2 | 0.6 | |
| HAPI-misc | 3.0 | 1.0 | 2.3 | 0.7 | |
| Use | GHABP-use | 2.5 | 1.1 | 3.7 | 1.1 |
| Daily use (hrs.) | 5.0 | 2.6 | 7.5 | 3.4 | |
| Aided performance | Aided CST (%) | 83.5 | 20.3 | 81.9 | 14.9 |
| Aided ANL (dB) | −2.2 | 5.2 | −0.9 | 6.0 |
Significant differences (p < .05/15 = . 0033) on independent-sample t tests are shown in bold font. Significance was determined with no adjustment to p values for multiple comparisons across dependent measures. HA=hearing aid; SD = standard deviation; GHABP = Glasgow Hearing Aid Benefit Profile; HASS = hearing aid satisfaction survey; SADL = Satisfaction with Amplification in Daily Life; HAPI = Hearing Aid Performance Inventory; CST = Connected Speech Test; ANL = acceptable noise level.
The next section of Table 3 shows five measures of self-reported hearing-aid benefit, one from the GHABP and four from the HAPI. The HAPI is scored such that lower scores reflect more benefit whereas this is not true for the other measures in Table 3. Four of the five measures of self-reported hearing-aid benefit showed significantly less benefit, all t(96) >3.2, adjusted p < .0033, in those who rejected their hearing aids than in those who kept them.
The next set of outcome measures in Table 3 pertains to hearing-aid usage with one coming from the GHABP and the other from daily diaries logging the hours used. Only the GHABP-based measure of usage showed significantly greater hearing-aid usage, t(96) > −3.6, adjusted p < .0033, by those who kept their hearing aids than those who did not, although the diary-based usage measure approached significance, t(96) = −2.7, p = .007.
Finally, two measures of aided performance in noise, the CST and the ANL, are shown at the bottom of Table 3. There were no significant differences, both t(96) < .73, between the two groups of adherents in either aided CST scores in noise or the aided ANL in dB.
Discussion
Adherents and Nonadherents
There were very few significant differences observed between adherents and nonadherents among the large set of demographic, psychological, and cognitive measures examined here. There were four nonauditory demographic measures examined: age, level of education, gender, and annual income level. Adherents did not differ significantly from nonadherents on any of these measures. For two hearing-related demographic measures, duration of hearing loss and better-ear PTA4, the two groups differed only for the latter with adherents having significantly greater hearing loss than nonadherents (Figure 1). As a result, better-ear PTA4 served as a covariate in all subsequent analyses of the differences between adherents and nonadherents. From the 26 psychological measures of affect, personality, and cognition, following data reduction using factor analysis (Table 1; see Online Appendix) there were no significant differences between adherents and nonadherents on any of these measures.
A different picture emerged, however, when examining several self-report measures related to hearing difficulties and hearing aids. Although no differences were observed between adherents and nonadherents for two measures of unaided performance in noise, the ANL and the CST, the nonadherents differed from the adherents on 3 of the 4 measures of hearing-aid expectations (ECHO) and on 10 of the 23 measures of communication difficulties and their reactions to those difficulties (CPHI). For the ECHO, nonadherents revealed lower expectations for hearing aids. For the CPHI, the pattern of differences was such that the nonadherents perceived that they had better communication performance and better adjustment to hearing problems, reflected in 6 of the 10 CPHI scales with significant differences between groups. On the other hand, for the other four CPHI scales with significant differences between adherents and nonadherents, the nonadherents had poorer awareness of communication-performance problems, poorer use of verbal and nonverbal communication strategies, and more denial of communication difficulties than the adherents.
As noted in the introduction, many factors impacting adherence to the recommendation to acquire hearing aids have been explored. Several have been identified as potential contributors to hearing-aid uptake in older adults with mild-to-moderate hearing loss, but measures of perceived hearing difficulties have garnered the greatest support in the literature (e.g., Arnold et al., 2019; Hickson et al., 2014; Knudsen et al., 2010; Laplante-Levesque et al., 2012; Meyer & Hickson, 2012; Pronk et al., 2017, 2019; Ratanjee-Vanmali et al., 2019; Sawyer, Armitage, et al., 2019; Simpson et al., 2019; Tahden et al., 2018). The present results from the CPHI certainly reinforce this finding. The additional finding here is that the two groups differed as well regarding their expectations about hearing aids as measured by the ECHO, also confirming some prior findings (e.g., Hickson et al., 2014).
Overall, this represents potentially good news for shaping the hearing-aid uptake behavior of older adults with mild-to-moderate hearing loss. Had differences been found in personality or cognition, for example, the likelihood of influencing the nonadherents to become adherents would be low. Here, however, it appears that the primary differences between adherents and nonadherents are with the older individual’s perceptions regarding their communication difficulties, or lack thereof, and their expectations about hearing aids. In both cases, these perceptions and expectations are subject to influence through counseling and education of the older adult by the healthcare professional.
Recent studies confirm the important roles that beliefs, expectations, and perceived difficulties play in the acquisition of hearing aids with a focus on self-motivation (Ridgway et al., 2016) and readiness for action (Saunders et al., 2016). In both studies, hearing-aid acquisition is modeled as a desired health behavior and factors that impact the acquisition of hearing aids were identified by comparing groups of older adults who were either adherents or nonadherents regarding the recommendation to seek help with hearing aids. On the other hand, Barker, Mackenzie, Elliott, et al. (2016), based on a systematic review of the literature on the impact of counseling-based approaches to improving use of hearing aids, concluded that programs focused on motivation to acquire hearing aids were generally unsuccessful. More recently, Sawyer, Munro, et al. (2019) suggested from their study of adherents and nonadherents that the most appropriate target for intervention to increase uptake of hearing aids is translating motivation into action. They found both groups to be reasonably motivated to take up hearing aids but those who did so were more ready for action, consistent with the findings of Saunders et al. (2016). Regardless of the health-behavior model employed, the main point here is that the primary determinants of uptake appear to be malleable, whether the focus is on enhancing the older adult’s motivation to acquire the devices or their readiness to do so once motivated.
This assumes that the professional providing the devices is willing and able to provide the needed counseling intervention (Meibos et al., 2017). Something as simple as use of language, written, and oral, that is appropriate for the older adult’s health literacy can have an impact on hearing-aid uptake (Klyn et al., 2020; Sciacca et al., 2017). Yet, even widely available written materials are often presented at a level that is inappropriate for older adults (e.g., Squires & Ou, 2020). The nature of the communication interactions between audiologists and older patients, moreover, is typically not patient-centered (Grenness et al., 2015a, 2015b), although this does not appear to impact hearing-aid uptake per se (Meyer et al., 2017). Hearing-aid fitting appointments rarely make use of behavior change techniques (Barker, Mackenzie, & de Lusignan, 2016) and other counseling skills (Muñoz et al., 2017) by audiologists, often attributed to the lack of adequate training in counseling (Muñoz, 2018). In fact, Amlani (2020) recently demonstrated that the audiologist’s behavior during interactions with the older adult patient may even present a barrier to the patient’s uptake of hearing aids. Clearly, improved uptake of hearing aids by older adults is needed as is more research on the ways in which uptake can be enhanced, including the provision of additional information and counseling online (e.g., Ferguson et al., 2016; Maidment et al., 2020).
It is somewhat difficult to compare the present findings to those from prior studies examining differences between adherents and nonadherents among older adults with mild-to-moderate hearing loss. As noted in the introduction, at least two studies of such groups made use of the CPHI and some of the other measures included here (Garstecki & Erler, 1998; Humes et al., 2003). There are important differences, however, between those studies and this study. Comparisons to Garstecki and Erler (1998) are difficult because the adherents and nonadherents were further divided into two groups based on the participant’s gender. In addition, in Garstecki and Erler it does not appear that adherents were necessarily new hearing-aid users as the authors noted that members of that group “. . . reported regular use of hearing aids” (p. 528). The CPHI measures were obtained from the adherents in that study, it appears, after some unknown period of hearing-aid use. So, these individuals not only adhered to the recommendation to obtain hearing aids but also had become regular users of hearing aids for an unknown duration prior to obtaining the CPHI scores. The nonadherents in Garstecki and Erler (1998), on the other hand, were like those in this study in that they had no prior hearing-aid experience. Likewise, of the 50 adherents in Humes et al. (2003), 2 were current hearing-aid users at the time the various measures were completed and another 10 had tried hearing aids previously but were not wearing them at the time. Thus, 24% of the adherents in Humes et al. (2003) had prior hearing-aid experience of various types and amounts. In this study, none of the 115 participants reported prior hearing-aid use and all measures were obtained prior to trying hearing aids for all participants.
Nonetheless, despite these differences in studies, there is overlap among some of the important variables identified across studies. For the Humes et al.’ (2003) study, the study most like the current one regarding the administration of all tests prior to hearing-aid uptake by most of the participants (100% of the nonadherents and 76% of the adherents), significant differences were observed between adherents and nonadherents for five CPHI scales. The pattern was such that the nonadherents had less problem awareness, greater denial of difficulties, less resulting stress, less exaggeration of the responsibility of others for their difficulties, and better overall self-acceptance compared with adherents. Some of these same differences in CPHI scores were observed here between adherents and nonadherents among the 139 older adults with mild-to-moderate hearing loss, none of whom wore hearing aids previously. Humes et al. (2003) also controlled for group differences in age and hearing loss, although this was accomplished by matching the groups for these two variables (as well as gender) rather than using statistical controls as in this study. Again, in this study, significant differences existed in hearing loss between the adherents and nonadherents, but these differences were controlled statistically by including better-ear PTA4 as a covariate in all the GLM analyses of the differences between adherents and nonadherents. Across the many GLM analyses examining group differences between the adherents and nonadherents, the better-ear PTA4 was a significant covariate in many of those analyses. Had hearing loss not been used as a covariate, many more significant differences between groups would have emerged. Given that the effect of hearing loss was known or could be predicted, that effect was not of interest here. In addition, as noted previously, hearing loss is not a malleable factor. What was of greater interest here was how the adherents and nonadherents differed, if at all, when controlling for differences in hearing loss.
For the significant differences on the ECHO and the CPHI, moreover, all the partial-eta-squared effect sizes for the effect of group in the GLM analyses were at least of medium size and several were large effects (Cohen, 1988). Thus, the differences between the adherents and nonadherents on their perceived communication problems and reactions to them, as well as their expectations about hearing aids, were substantial effects, even after controlling statistically for differences in hearing loss between these two groups.
As noted, in several recent studies of hearing-aid adherents and nonadherents, all involving older adults, perceived need or hearing difficulties consistently emerged as the best predictor of adherence to recommendations for hearing-aid acquisition (Ridgway et al., 2016; Saunders et al., 2016; Tahden et al., 2018). This was true for both paired comparisons of means between each group as well as for logistic regression approaches to the analysis of the individual data in these studies. Moreover, a wide range of other variables were considered in these studies, including a variety of psychosocial and cognitive measures, with the perceived hearing difficulty or need for assistance consistently emerging as the key factor. The present findings are consistent with these findings as well.
Adherents Who Accepted or Rejected Hearing Aids
There were minimal differences, however, between the subgroup of adherents who acquired and kept their hearing aids versus the subgroup who acquired but returned their hearing aids. The only differences between these two subgroups of adherents were found in the outcomes obtained at 1-month postfit. Generally, those who rejected their hearing aids self-reported less benefit, lower satisfaction, and less usage than those who accepted their hearing aids. The lack of significant predictors of the likelihood to accept or reject hearing aids after a trial period was also observed by Pronk et al. (2019). In that study, only differences in high-frequency hearing loss, more severe in those who purchased or kept their hearing aids, proved to distinguish the two groups from one another.
In the present analyses, however, there were only 21 older adults who rejected their hearing aids and only 15 of the 21 completed the outcome measures at 1-month postfit. The percentage who returned their hearing aids, 20%, approximated the return rate for the clinic in which they were seen and for the United States as a whole at that time (Strom, 2007). The observations of differences between these two subgroups of adherents, therefore, must be tempered by the small number of participants who rejected their devices. Furthermore, the outcomes obtained were at 1-month postfit and long-term outcomes were not available from these participants. Our prior work, however, suggests that similar performance on outcome measures would have been observed over a postfit period of up to 2 years (Humes, Wilson, Barlow, & Garner, 2002; Humes, Wilson, Barlow, Garner, & Amos, 2002).
There are several study limitations that should be noted. First, all of those screened for study eligibility in Session 1 were volunteers from the local community. As such, this was a convenience sample rather than a random sample of the community. Among the 139 participants, the focus was on the differences between those who adhered to the clinical recommendation to purchase hearing aids and those who did not. As noted, the percentage who did adhere to the clinical recommendation to purchase hearing aids in this study, 42.3%, is very similar to that reported by Yueh et al. (2010) which included 1,382 older adults recruited from the outpatient clinic of a large Veterans Administration medical center. Aside from the agreement in percentages, however, it is difficult to know how this study’s participants may have differed from “typical” clinic patients who are seeking help for themselves clinically rather than enrolling as a volunteer in a research study directed toward hearing-aid outcomes. Of course, the factors identified here that differed between adherents and nonadherents may or may not generalize to the broader population of older adults with untreated hearing loss depending on the representativeness of the current sample.
Furthermore, of the 368 eligible individuals, 214 (58.1%) did not purchase study hearing aids and the 36 of these 214 who agreed to additional testing are assumed to be representative of this larger group of nonadherents. All that can be said about “nonadherence” to the recommendation to purchase the study hearing aids here is that they did not purchase those devices at that time. As noted earlier in “Methods” section, 64.5% of the 214 indicated that they were either still considering hearing aids as an option at that time or that they were interested in other types of devices than those in the study. It is conceivable that some of these individuals may in fact have opted to purchase hearing aids elsewhere or at some later time. No follow-up information is available from these individuals to document subsequent acquisition of hearing aids.
APPENDIX: Details of measures and data reduction via factor analysis
Hearing-Related Measures from Session 2
For the speech-in-noise measurement, the Connected Speech Test (CST; Cox et al., 1987) was used with the speech at 65 dB SPL, the competing babble at +8 dB signal-to-babble ratio, and the speech and competing babble at 0- and 180-degrees azimuth, respectively. The ECHO, a measure of hearing-aid expectations, includes subscale scores of Positive Effects (PE), Service and Cost (SC), Personal Image (PI), and Negative Features (NF). Hardcopy forms of the ECHO were used, the responses double-entered manually for accuracy, and scored via computer software. The four ECHO subscale scores were subjected to a principal-components factor analysis for data reduction (Gorsuch, 1983) with a single principal component (PC_echo) emerging using an eigenvalue > 1 stopping rule. This solution was reasonably good accounting for 48.9% of the variance [all communalities ≥ 0.3 and the Kaiser-Mayer-Olkin (KMO) measure of sampling adequacy = 0.64].
For the measurement of ANL, we followed the procedures from Nabelek et al. (1991, 2006), but used different speech and noise stimuli. Specifically, we used several tracks from the Speech Intelligibility Rating (SIR; Cox & McDaniel, 1989) corpus as the speech signal and the SIR babble as the competition. All speech and noise stimuli were presented from the same loudspeaker at 0-degree azimuth and elevation. A “comfortable” listening level for the speech was established first using the 7-point loudness rating scale of Hawkins et al. (1987), beginning 15 dB above SRT and bracketing in 5-dB steps for 5 up-down reversals of level. The mean of the last three reversals served as the comfortable listening level for the speech. Next, the competing babble was presented from the same loudspeaker as the speech at a level of 10 dB above SRT. On the first run, this level was increased in 5-dB steps until the listener indicated it was no longer possible to follow the conversation and then decreased from there in 5-dB steps until the passage was heard clearly again. From this latter noise level, the level was increased in 1-dB steps until the participant indicated that he or she was at the maximum noise level that could be “put up with” (defined as the maximum they could tolerate while still hearing the speech signal clearly). This level corresponded to the maximum tolerable noise level and it was measured on three separate ascents with the mean of those three representing the measured background noise level. The ANL was then calculated by subtracting the mean maximum tolerable background noise level from the mean comfortable speech level.
For the CPHI, there are 25 subscale scores organized around the five categories of communication performance (CP), communication importance (CI), communication environment (CE), communication strategies (CS) and personal adjustment (PA). We used the preprinted test booklets and scoring software supplied by the test developers to obtain the 25 subscale scores which were then subjected principal-components factor analysis. Five PCs emerged using an eigenvalue > 1 stopping rule. This solution was excellent accounting for 71.9% of the variance [all communalities ≥ 0.5 and the KMO measure of sampling adequacy = 0.87]. Table 2 presents the CPHI scale scores loading on each of the five CPHI PCs together with the label used for each of the five PCs.
For the GHABP, we used prototypical listening situations described previously (Gatehouse, 1999; Humes et al., 2009). In particular, two of the four items involved communication in noise, one centered on communication with one other person in quiet, and the remaining item involved listening to TV with others.
Measures of Affect, Personality, and Cognition in Session 3
The Life Orientation Test-Revised (LOT-R; Scheier et al., 1994) is a 10-item measure of optimism versus pessimism. Three of the ten items measure either optimism or pessimism with the other four serving as fillers. The participant is presented with a statement and then rates each on a four-point scale of agreement: strongly disagree, disagree, agree, or strongly agree with the three pessimism items reverse scored from the optimism items and the fillers unscored.
The Positive and Negative Affect Scale (PANAS; Watson et al., 1988) is a brief self-report measure of affect. The participant is presented with a list of 20 words in a column and, for each, is asked to indicate whether he or she generally feels this way “very slightly or not at all”, “a little”, “moderately”, “quite a bit” or “extremely”, with points assigned from 1 to 5, respectively. Half of the 20 items convey positive affect, such as “excited”, “strong”, “enthusiastic”, “proud” and “inspired”, whereas the other have convey negative affect, such as “distressed”, “upset”, “scared”, “ashamed” and “nervous”. Two scores emerge: PANAS-positive and PANAS-negative. Each represents the total points for each set of 10 items, scores ranging from 10-50. For the positive scale, higher scores, and, for the negative scale, lower scores, reflect more positive affect.
The State-Trait Anxiety Inventory (STAI; Spielberger et al., 1970; Spielberger, 1983) is a self-report measure of feelings of anxiety, momentary or in current state and long-term or as a trait of the individual. There are forty items with the first 20 assessing situational or state anxiety (STAI-S), with a focus on how the participant “feels right now, at this moment”, and the last 20 measuring underlying trait anxiety (STAI-T), how he or she “generally feels”. For all 40 items, four response choices are provided: “not at all”, “somewhat”, “moderately so” and “very much so” with points of 1, 2, 3 and 4, respectively. Within each scale, several items are reverse scored. Examples from the STAI-S include: “I feel content” and “I am worried”. Examples from the STAI-T are: “I am happy” and “I lack self-confidence.” Total scores, following reversal of some items, range from 20-80 for both the STAI-S and STAI-T with higher scores reflecting less anxiety and more positive affect.
The Myers-Briggs Type Inventory (MBTI) personality scale (Myers et al., 1998), the 126-item Form G, was next completed. This is a widely used measure of personality that can be used to categorize the participant into one of 16 personality types. Here, we used the scores for each of the 8 scales (Extravert, Introvert, Sense, Intuitive, Feeler, Thinker, Judger, Perceiver) in subsequent analyses rather than one of the 16 types derived from these scores. For the MBTI, software supplied by the test publisher was used to score the participant's forms whereas custom software was used to score the responses for the other tests.
The five scores for affect and the eight scores from the MBTI were subjected to a principal-components factor analysis for data reduction. Using an eigenvalue > 1 stopping criterion, five factors emerged, one representing all five measures of affect and four representing each of the personality dimensions from the MBTI. The specific measures loading on each PC and the labels used for that PC are provided in Table 1. The five-factor solution was excellent, accounting for 85.1% of the variance with all communalities > 0.47 and a KMO statistic of 0.58.
For the WAIS-III (Wechsler, 1997), there are thirteen standard scale scores organized into four general types of cognitive processing: verbal comprehension (VC), working memory (WM), processing speed (PS) and perceptual organization (PO). The raw scores for each of the thirteen WAIS-III scales were analyzed using principal-components factor analysis for data reduction. Using the eigenvalue > 1 fitting criterion, three PCs emerged, one for VC, one for WM, and one for the combination of PS and PO. The specific scales loading on each of these three cognitive factors and the labels used for each of these PCs are provided in Table 1. Once again, an excellent fit emerged with the KMO statistic = 0.89, all communalities exceeding 0.54, and 65.5% of the variance explained by these three factors.
In all cases, hardcopy forms were used and responses were recorded on the test forms by the participant using a pen. No assistance was provided to the participant when completing any of the self-report measures.
Footnotes
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported, in part, by research grant R01-AG008293 (L. Humes, PI) from the National Institute on Aging.
ORCID iD: Larry E. Humes https://orcid.org/0000-0002-9668-3744
References
- Aazh H., Prasher D., Nanchahal K., Moore B. C. J. (2015). Hearing-aid use and its determinants in the UK National Health Service: Across-sectional study at the Royal Surrey Country Hospital. International Journal of Audiology, 54, 152–161. 10.3109/14992027.2014.967367 [DOI] [PubMed] [Google Scholar]
- American National Standards Institute. (2004). Specifications for audiometers, ANSI S3.6. [Google Scholar]
- Amieva H., Ouvrard C. (2020). Does treating hearing loss in older adults improve cognitive outcomes? A review. Journal of Clinical Medicine, 9, 805. 10.3390/jcm9030805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlani A. M. (2020). Influence of provider interaction on patient’s readiness toward audiological services and technology. Journal of the American Academy of Audiology, 31, 342–353. 10.3766/jaaa.19051 [DOI] [PubMed] [Google Scholar]
- Arnold M. L., Hyer K., Small B. J., Chisolm T., Saunders G. H., McEvoy C. L., Lee D. J., Dhar S., Bainbridge K. (2019). Hearing aid prevalence and factors related to use among adults from the Hispanic Community Health Study/Study of Latinos. JAMA Otolaryngology Head and Neck Surgery, 145, 501–508. 10.1001/jamaoto.2019.0433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bainbridge K. E., Ramachandran V. (2014). Hearing aid use among older U.S. adults: The National Health and Nutrition Examination Survey, 2005–2006 and 2009–2010. Ear and Hearing, 35, 289–294. 10.1097/01.aud.0000441036.40169.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker F., Mackenzie E., de Lusignan S. (2016). Current process in hearing-aid fitting appointments: An analysis of audiologists’ use of behaviour change techniques using the behaviour change taxonomy. International Journal of Audiology, 55, 643–652. 10.1080/14992027.2016.1197425 [DOI] [PubMed] [Google Scholar]
- Barker F., Mackenzie E., Elliott L., Jones S., de Lusignan S. (2016). Interventions to improve hearing aid use in adult auditory rehabilitation. Cochrane Database of Systematic Reviews, 8, CD010342. 10.1002/14651858.CD010342.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisgaard N., Ruf S. (2017). Findings from the EuroTrak surveys from 2009 to 2015: Hearing loss prevalence, hearing aid adoption, and benefits from hearing aid use. American Journal of Audiology, 26, 451–461. 10.1044/2017_AJA-16-0135 [DOI] [PubMed] [Google Scholar]
- Chia E.-M., Wang J. J., Rochtchina E., Cumming R. R., Newall P., Mitchell P. (2007). Hearing impairment and health-related quality of life: The Blue Mountains Hearing Study. Ear and Hearing, 28, 187–195. 10.1097/AUD.0b013e31803126b6 [DOI] [PubMed] [Google Scholar]
- Chien W., Lin F. R. (2012) Prevalence of hearing-aid use among older adults in the United States. Archives of Internal Medicine, 172, 292–293. 10.1001/archinternmed.2011.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates. 10.4324/9780203771587 [DOI] [Google Scholar]
- Cosh S., Helmer C., Delcourt C., Robins T. G., Tully P. J. (2019). Depression in elderly patients with hearing loss: Current perspectives. Clinical Interventions in Aging, 14, 1471–1480. 10.2147/CIA.S195824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox, R. M., & McDaniel, D. M. (1989). Development of the Speech Intelligibility Rating (SIR) test for hearing aid comparisons. Journal of speech and hearing research, 32(2), 347–352. 10.1044/jshr.3202.347 [DOI] [PubMed]
- Cox R. M., Alexander G. C. (1999). Measuring satisfaction with amplification in daily life: The SADL Scale. Ear and Hearing, 20, 306–320. 10.1097/00003446-199908000-00004 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C. (2000). Expectations about hearing aids and their relationship to fitting outcome. Journal of the American Academy of Audiology, 11, 368–382. [PubMed] [Google Scholar]
- Cruickshanks K. J., Zhan W., Zhong W. (2010). Epidemiology of age-related hearing impairment. In Gordon-Salant S., Frisina R. D., Popper A. N., Fay R. R. (Eds.), Springer handbook of auditory research (SHAR) (pp. 259–274). Springer-Verlag. 10.1007/978-1-4419-0993-0 [DOI] [Google Scholar]
- Dalton D. S., Cruickshanks K. J., Klein B. E., Klein R., Wiley T. L., Nondahl D. M. (2003). The impact of hearing loss on quality of life in older adults. Gerontologist, 43, 661–668. 10.1093/geront/43.5.661 [DOI] [PubMed] [Google Scholar]
- Dawes P., Fortnum H., Moore D., Emsley R., Norman P., Cruickshanks K., Davis A., Edmonson-Jones M., McCormack A., Lutman M., Munro K. (2014) Hearing in middle age: A population snapshot of 40-to-69-year olds in the United Kingdom. Ear and Hearing, 35, e44–e51. 10.1097/AUD.0000000000000010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demorest M. E., Erdman S. A. (1986). Scale composition and item analysis of the Communication Profile for the Hearing Impaired. Journal of Speech & Hearing Research, 29, 515–535. 10.1044/jshr.2904.535 [DOI] [PubMed] [Google Scholar]
- Demorest M. E., Erdman S. A. (1987). Development of the Communication Profile for the Hearing Impaired. Journal of Speech & Hearing Disorders, 52, 129–143. 10.1044/jshd.5202.129 [DOI] [PubMed] [Google Scholar]
- Dillon H., Byrne D., Brewer S., Katsch R., Ching T., Keidser G. (1998). NAL-nonlinear version 1.01 user manual. National Acoustics Laboratories. [Google Scholar]
- Edwards B. (2020). Emerging technologies, market segments, and MarkeTrak 10 insights in hearing health technology. Seminars in Hearing, 41, 37–54. 10.1055/s-0040-1701244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdman S. A., Demorest M. E. (1998). Adjustment to hearing impairment II: Audiological and demographic correlates. Journal of Speech, Language, and Hearing Research, 41, 123–136. 10.1044/jslhr.4101.123 [DOI] [PubMed] [Google Scholar]
- Ferguson M., Brandreth M., Brassington W., Leighton P., Wharrad H. (2016). A randomized controlled trial to evaluate the benefits of a multimedia educational program for first-time hearing aid users. Ear and Hearing, 37, 123–136. 10.1097/AUD.0000000000000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garstecki D. C., Erler S. F. (1998). Hearing loss, control, and demographic factors influencing hearing aid use among older adults. Journal of Speech, Language, Hearing Research, 41, 527–537. 10.1044/jslhr.4103.527 [DOI] [PubMed] [Google Scholar]
- Garstecki D. C., Erler S. F. (1999). Older adult performance on the Communication Profile for the Hearing Impaired: Gender difference. Journal of Speech, Language, Hearing Research, 42, 785–796. 10.1044/jslhr.4204.785 [DOI] [PubMed] [Google Scholar]
- Gatehouse S. (1999). Glasgow Hearing Aid Benefit Profile: Gerivation and validation of a client centered outcome measure for hearing aid services. Journal of the American Academy of Audiology, 10, 80–103. [Google Scholar]
- Gorsuch, R.L. (1983). Factor Analysis, 2nd Edition. NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Grenness C., Hickson L., Laplante-Lévesque A., Meyer C., Davidson B. (2015. a). Communication patterns in audiologic rehabilitation history-taking: Audiologists, patients, and their companions. Ear and Hearing, 36, 191–204. 10.1097/AUD.0000000000000100 [DOI] [PubMed] [Google Scholar]
- Grenness C., Hickson L., Laplante-Lévesque A., Meyer C., Davidson B. (2015. b). The nature of communication throughout diagnosis and management planning in initial audiologic rehabilitation consultations. Journal of the American Academy of Audiology, 26, 36–50. 10.3766/jaaa.26.1.5 [DOI] [PubMed] [Google Scholar]
- Hawkins, D. B., Walden, B. E., Montgomery, A., & Prosek, R. A. (1987). Description and validation of an LDL procedure designed to select SSPL90. Ear and hearing, 8(3), 162–169. 10.1097/00003446-198706000-00006 [DOI] [PubMed]
- Hickson L., Meyer C., Lovelock K., Lampert M., Khan A. (2014). Factors associated with success with hearing aids in older adults. International Journal of Audiology, 53(Suppl 1), S18–S27. 10.3109/14992027.2013.860488 [DOI] [PubMed] [Google Scholar]
- Humes L. E. (2020). What is normal hearing for older adults and can “normal-hearing older adults” benefit from hearing care intervention? Hearing Review, 27(7), 12–18. [Google Scholar]
- Humes, L.E. & Humes, L.E. (2004). Factors affecting “long term” hearing-aid success. Seminars in Hearing, 25, 63–72. 10.1055/s-2004-823048 [DOI] [Google Scholar]
- Humes L. E., Ahlstrom J. B., Bratt G. W., Peek B. F. (2009). Studies of hearing-aid outcome measures in older adults: A comparison of technologies and an examination of individual differences. Seminars in Hearing, 30, 112–128. 10.1055/s-0029-1215439 [DOI] [Google Scholar]
- Humes L. E., Dubno J. R. (2010). Factors affecting speech understanding in older adults. In S. Gordon-Salant, R. D. Frisina, A. N. Popper, & R. R. Fay (Eds.), The aging auditory system: Perceptual characterization and neural bases of presbycusis. Chapter 8. Springer handbook of auditory research (SHAR). Springer-Verlag, pp. 211–258. 10.1007/978-1-4419-0993-0 [DOI]
- Humes L. E., Garner C. B., Wilson D. L., Barlow N. N. (2001). Hearing-aid outcome measures following one month of hearing aid use by the elderly. Journal of Speech, Language, Hearing Research, 44, 469–486. 10.1044/1092-4388(2001/037) [DOI] [PubMed] [Google Scholar]
- Humes L. E., Kinney D. L., Thompson E. (2010). Comparison of benefits provided by various hearing aid technologies in older adults. In Hickson L. (Ed.), Hearing care for adults 2009—The challenge of aging (pp. 131–138). Phonak AG. [Google Scholar]
- Humes L. E., Krull V. (2012). Evidence about the effectiveness of hearing aids in adults. In Wong L., Hickson L. (Eds.), Evidence based practice in audiology. Plural Publishing, pp. 61–92. [Google Scholar]
- Humes L. E., Pichora-Fuller M. K., Hickson L. (2020). Functional consequences of impaired hearing in older adults and implications for intervention. In K. Helfer, E. L. Bartlett, A. N. Popper, & R. R. Fay (Eds.), Aging and hearing. Springer handbook of auditory research (SHAR) (pp. 257–291). Springer-Verlag. 10.1007/978-3-030-49367-7_11 [DOI]
- Humes L. E., Wilson D. L., Barlow N. N., Garner C. B. (2002). Changes in hearing-aid benefit following 1 or 2 years of hearing-aid use by older adults. Journal of Speech, Language, Hearing Research, 45, 772–782. 10.1044/1092-4388(2002/062) [DOI] [PubMed] [Google Scholar]
- Humes L. E., Wilson D. L., Barlow N. N., Garner C. B, Amos N. E. (2002). Longitudinal changes in hearing-aid satisfaction and usage in the elderly over a period of one or two years after hearing delivery. Ear and Hearing, 23, 428–437. 10.1097/00003446-200210000-00005 [DOI] [PubMed] [Google Scholar]
- Humes L. E., Wilson D. L., Humes A. C. (2003) Examination of differences between successful and unsuccessful elderly hearing aid candidates matched for age, hearing loss, and gender. International Journal of Audiology, 42, 432–441. 10.3109/14992020309080053 [DOI] [PubMed] [Google Scholar]
- Jilla A. M., Johnson C. E., Danhauer J. L., Anderson M., Smith J. N., Sullivan J. C., Sanchez K. R. (2020). Predictors of hearing aid use in the advanced digital era: An investigation of benefit, satisfaction, and self-efficacy. Journal of the American Academy of Audiology, 31, 87–95. 10.3766/jaaa.18036 [DOI] [PubMed] [Google Scholar]
- Klyn N. A. M., Shaikh Z. M., Dhar S. (2020). Health literacy and self-reported hearing aid use in the Health and Retirement Study. Ear and Hearing, 41, 386–394. 10.1097/AUD.0000000000000770 [DOI] [PubMed] [Google Scholar]
- Knudsen L. V., Oberg M., Nielsen C., Naylor G., Kramer S. E. (2010). Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends in Amplification, 14, 127–154. 10.1177/1084713810385712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochkin S. (1993. a). MarkeTrak III: Why 20 million in U.S. don’t use hearing aids for their hearing loss. Part I. Hearing Journal, 46(1), 20–27. [Google Scholar]
- Kochkin S. (1993. b). MarkeTrak III: Why 20 million in U.S. don’t use hearing aids for their hearing loss. Part II. Hearing Journal, 46(2), 26–31. [Google Scholar]
- Kochkin S. (1993. c). MarkeTrak III: Why 20 million in U.S. don’t use hearing aids for their hearing loss. Part III. Hearing Journal, 46(4), 36–37. [Google Scholar]
- Kochkin S. (1996). MarkeTrak IV: 10-year trends in the hearing aid market: Has anything changed? Hearing Journal, 48(1), 23–34. [Google Scholar]
- Kochkin S. (2000). MarkeTrak V: Consumer satisfaction revisited. Hearing Journal, 53(1), 38–55. 10.1097/00025572-200001000-00005 [DOI] [Google Scholar]
- Kochkin S. (2009). MarkeTrak VIII: 25-year trends in hearing health market. Hearing Review, 16(11), 12–31. [Google Scholar]
- Laplante-Levesque A., Hickson L., Worrall L. (2012). What makes adults with hearing impairment take up hearing aids or communication programs and achieve successful outcomes. Ear and Hearing, 33, 79–93. 10.1097/AUD.0b013e31822c26dc [DOI] [PubMed] [Google Scholar]
- Lin F. R., Niparko J. K., Ferrucci L. (2011). Hearing loss prevalence in the United States. Archives of Internal Medicine, 171(20), 1851–1853. 10.1001/archinternmed.2011.506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G., Huntley J., Sommerlad A., Ames S., Ballard C., Banerjee S., . . . Mukadam N. (2020). Dementia prevention, intervention, and care: 220 report of the Lancet Commission. Lancet, 396, 413–446. 10.1016/S0140-6736(20)30367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maidment D. W., Coulson N. S., Wharrad H., Taylor M., Ferguson M. A. (2020). The development of an mHealth educational intervention for first-time hearing-aid users: Combining theoretical and ecologically valid approaches. International Journal of Audiology, 59, 492–500. 10.1080/14992027.2020.1755063 [DOI] [PubMed] [Google Scholar]
- Meibos A., Muñoz K., Schultz J., Price T., Whicker J. J., Caballero A., Graham L. (2017). Counselling users of hearing technology: A comprehensive literature review. International Journal of Audiology, 56, 903–908. 10.1080/14992027.2017.1347291 [DOI] [PubMed] [Google Scholar]
- Meyer C., Barr C., Khan A., Hickson L. (2017). Audiologist-patient communication profiles in hearing rehabilitation appointments. Patient Education and Counseling, 100, 1490–1498. 10.1016/j.pec.2017.03.022 [DOI] [PubMed] [Google Scholar]
- Meyer C., Hickson L. (2012). What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? International Journal of Audiology, 51, 66–74. 10.3109/14992027.2011.611178 [DOI] [PubMed] [Google Scholar]
- Mick P., Parfyonov M., Wittich W., Phillips N., Guthrie D., Pichora-Fuller M. K. (2018). Associations between sensory loss and social networks, participation, support, and loneliness: An analysis of the Canadian Longitudinal Study on Aging. Canadian Family Physician Journal, 64, e33–e41. [PMC free article] [PubMed] [Google Scholar]
- Muñoz K. (2018). Counseling skill development in audiology: Clinical instruction considerations. Seminars in Hearing, 39, 9–12. 10.1055/s-0037-1613701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz K., Ong C. W., Borrie S. S. A., Nelson L. H., Twohig M. P. (2017). Audiologists’ communication behaviour during hearing device management appointments. International Journal of Audiology, 56, 1–9. 10.1080/14992027.2017.1282632 [DOI] [PubMed] [Google Scholar]
- Nabelek A. K., Freyaldenhoven M. C., Tampas J. W., Burchfield S. B., Muenchen R. A. (2006). Acceptable noise level as a predictor of hearing aid use. Journal of the American Academy of Audiology, 17, 626–639. 10.3766/jaaa.17.9.2 [DOI] [PubMed] [Google Scholar]
- Nabelek A. K., Tucker F. M., Letowski T. R. (1991). Toleration of background noises: Relationship with patterns of hearing aid use by elderly persons. Journal of Speech Hearing Research, 34, 679–685. 10.1044/jshr.3403.679 [DOI] [PubMed] [Google Scholar]
- Pichora-Fuller M. K., Kramer S. E., Eckert M. A., Edwards B., Hornsby B. W. Y., Humes L. E., . . . Wingfield A. (2016). Hearing impairment and cognitive energy: A framework for understanding effortful listening (FUEL). Ear and Hearing, 37, 5S–27S. 10.1097/AUD.0000000000000312 [DOI] [PubMed] [Google Scholar]
- Popelka M. M., Cruickshanks K. J., Wiley T. L., Tweed T. S., Klein B. E., Klein R. (1998). Low prevalence of hearing aid use among older adults with hearing loss: The Epidemiology of Hearing Loss Study. Journal of the American Geriatric Society, 46, 1075–1078. 10.1111/j.1532-5415.1998.tb06643.x [DOI] [PubMed] [Google Scholar]
- Powers T. A., Rogin C. (2020). MarkeTrak 10: History and methodology. Seminars in Hearing, 41, 3–5. 10.1055/s-0040-1701241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk M., Deeg D. J. H., Versfeld N. J., Heymans M. W., Naylor G., Kramer S. E. (2017). Predictors of entering a hearing aid evaluation period: A prospective study in older hearing-help seekers. Trends in Hearing, 21, 1–20. 10.1177/2331216517744915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk M., Meijerink J. F. J., Kramer S. E., Heymans M. W., Besser J. (2019). Predictors of purchasing a hearing aid after an evaluation period: A prospective study in Dutch older hearing aid candidates. American Journal of Audiology, 28(3S), 802–805. 10.1044/2019_AJA-HEAL18-18-0163 [DOI] [PubMed] [Google Scholar]
- Ratanjee-Vanmali H., Swanepoel D. W., Laplante-Levesque A. (2019). Characteristics, behaviors, and readiness of persons seeking hearing healthcare online. International Journal of Audiology, 58, 107–115. 10.1080/14992027.2018.1516895 [DOI] [PubMed] [Google Scholar]
- Ridgway J., Hickson L., Lind C. (2016). Decision-making and outcomes of hearing help-seekers: A self-determination theory perspective. International Journal of Audiology, 55(Suppl 3), S13–S22. 10.3109/14992027.2015.1120893 [DOI] [PubMed] [Google Scholar]
- Sangster J. F., Gerace T. M., Seewald R. C. (1991). Hearing loss in elderly patients in a family practice. Canadian Medical Association Journal, 144, 981–984. [PMC free article] [PubMed] [Google Scholar]
- Sarant J., Harris D., Busby P., Maruff P., Schembri A., Lemke U., Launer S. (2020). The effect of hearing aid use on cognition in older adults: Can we delay decline or even improve cognition? Journal of Clinical Medicine, 9, 254–277. 10.3390/jcm9010254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders G. H., Frederick M. T., Silverman S. C., Nielsen C., Laplante-Lévesque A. (2016). Health behavior theories as predictors of hearing-aid uptake and outcomes. International Journal of Audiology, 55(Suppl 3), S59–S68. 10.3109/14992027.2016.1144240 [DOI] [PubMed] [Google Scholar]
- Sawyer C., Armitage C., Munro K., Singh G., Dawes P. (2019). Correlates of hearing aid use in UK adults: Self-reported difficulties, social participation, living situation, health, and demographics. Ear and Hearing, 40, 1061–1068. 10.1097/AUD.0000000000000695 [DOI] [PubMed] [Google Scholar]
- Sawyer C., Munro K., Dawes P., O’Driscoll M. P., Armitage C. J. (2019). Beyond motivation: Identifying targets for intervention to increase hearing aids use in adults. International Journal of Audiology, 58, 53–58. 10.1080/14992027.2018.1534007 [DOI] [PubMed] [Google Scholar]
- Sciacca A., Meyer C., Ekberg K., Barr C., Hickson L. (2017). Exploring audiologists’ language and hearing aid uptake in initial rehabilitation appointments. American Journal of Audiology, 26, 110–118. 10.1044/2017_AJA-16-0061 [DOI] [PubMed] [Google Scholar]
- Simpson A., Matthews L., Cassarly C., Dubno J. (2019). Time from hearing aid candidacy to hearing aid adoption: A longitudinal cohort study. Ear and Hearing, 40, 468–476. 10.1097/AUD.0000000000000641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeeth L., Fletcher A., Ng E. S. -W., Stirling S., Nunes M., Breeze E., . . . Tulloch A. (2002). Reduced hearing, ownership, and use of hearing aids in elderly people in the UK—The MRC trial of the assessment and management of older people in the community: A cross-sectional survey. Lancet, 359(9316), 1466–1470. 10.1016/s0140-6736(02)08433-7 [DOI] [PubMed] [Google Scholar]
- Southall K., Gagné J.-P., Jennings M. B. (2010). Stigma: A negative and a positive influence on help-seeking for adults with acquired hearing loss. International Journal of Audiology, 49, 804–814. 10.3109/14992027.2010.498447 [DOI] [PubMed] [Google Scholar]
- Spielberger C. D. (1983). Manual for the State-Trait Anxiety Inventory (Form Y). Consulting Psychologists Press. [Google Scholar]
- Spielberger C. D., Gorsuch R. L., Lushene R. E. (1970). Test manual for the State Trait Anxiety Inventory. Consulting Psychologists Press. [Google Scholar]
- Squires E. A., Ou H. (2020). Do we have effective patient education materials for age-related hearing loss? American Journal of Audiology, 29, 79–87. 10.1044/2019_AJA-19-00063 [DOI] [PubMed] [Google Scholar]
- Stevens G., Flaxman S., Brunskill E., Mascarenhas M., Mathers C. D., Finucane M., & Global Burden of Disease Hearing Loss Expert Group. (2013). Global and regional hearing impairment prevalence: An analysis of 42 studies in 29 countries. European Journal of Public Health, 23, 146–152. 10.1093/eurpub/ckr176 [DOI] [PubMed] [Google Scholar]
- Strom K. (2007). Happier returns? Hearing Journal, 14(5), 5. [Google Scholar]
- Tahden M. A. S., Gieseler A., Meis M., Wagener K. C., Colonius H. (2018). What keeps older adults with hearing impairment from adopting hearing aids? Trends in Hearing, 22, 1–17. 10.1177/2331216518809737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventry I. M., Weinstein B. E. (1982). The Hearing Handicap Inventory for the Elderly: A new tool. Ear and Hearing, 3, 128–134. 10.1097/00003446-198205000-00006 [DOI] [PubMed] [Google Scholar]
- Ventry I. M., Weinstein B. E. (1983). Identification of elderly people with hearing problems. American Speech-Language Hearing Association, 25, 37–42. [PubMed] [Google Scholar]
- Walden B. E., Demorest M. E., Hepler E. L. (1984). Self-report approach to assessing benefit derived from amplification. Journal of Speech and Hearing Research, 27, 49–56. 10.1044/jshr.2701.49 [DOI] [PubMed] [Google Scholar]
- Wallhagen M. I. (2010). The stigma of hearing loss. Gerontologist, 50, 66–75. 10.1093/geront/gnp107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward J. A., Lord S. R., Williams P., Anstey K. (1993). Hearing impairment and hearing aid use in women over 65 years of age. Cross-sectional study of women in a large urban community. The Medical Journal of Australia, 159, 382–384. 10.5694/j.1326-5377.1993.tb137911.x [DOI] [PubMed] [Google Scholar]
- Wechsler D. (1997). Wechsler Adult Intelligence Scale, 3rd Edition (WAIS-III). The Psychological Corporation. [Google Scholar]
- Weinstein B. E., Ventry I. M. (1983). Audiometric correlates of the Hearing Handicap Inventory for the Elderly. Journal of Speech & Hearing Disorders, 48, 379–384. 10.1044/jshd.4804.379 [DOI] [PubMed] [Google Scholar]
- Wilson R. H., Noe C. M., Cruickshanks K. J., Wiley T. L., Nondahl D. M. (2010). Prevalence and degree of hearing loss among males in the Beaver Dam cohort: A comparison of veterans and non-veterans. Journal of Rehabilitative Research & Development, 47, 505–520. 10.1682/jrrd.2009.10.0169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yueh B., Collins P., Souza P. E., Boyko E. J., Loovis C. F., Heagerty P. J., Liu C. -F., Hedrick S. C. (2010). Long-term effectiveness of screening for hearing loss: The screening for auditory impairment-which hearing assessment test (SAI-WHAT) randomized trial. Journal of the American Geriatrics Society, 58, 427–434. 10.1111/j.1532-5415.2010.02738.x [DOI] [PubMed] [Google Scholar]