Capsule Summary:
Greater child daily global stress was associated with increased likelihood of awakening from asthma that night. Asthma awakenings were followed by greater morbidity the next day.
Keywords: asthma, nocturnal awakening, children, stress
To the Editor:
Asthma guidelines use nocturnal awakenings to categorize asthma impairment. Even with daily controller therapy in a clinical trial, nocturnal asthma symptoms occurred in the absence of exacerbations and in up to 26% of children at least monthly1. Since psychological stress is associated with the risk of asthma exacerbations in children2 and affects sleep quality,3 stress is a potential modifiable predisposing factor for nocturnal asthma symptoms. We hypothesized that acute child and caregiver stress would be associated with increased likelihood of nocturnal asthma symptom occurrence in school-age children.
Nocturnal awakenings and measures of parental and child stress were assessed by daily diary card. After development, pilot study and revision, the diary card included 42 self-administered items (17 child, 9 caregiver, 16 caregiver with child input). Questions addressed nocturnal awakenings attributed to asthma and to other reasons. The perception of the child’s daily global stress was indicated by response to the question “How was your day today?” [question 6 Daily Diary Card (DDC), see table S1, online supplement]. Possible responses included very bad, bad, good or very good and represent decreasing levels of daily global stress. The child circled facial representations of his/her emotions that day (questions 18–22 DDC) and of how specified daily events made him/her feel4 (questions 7–17 DDC). Morbidity measures, including albuterol use, school absence, doctor contacts and prednisone use (questions 25–28 DDC), were recorded. Daily caregiver stress was assessed by questions about family, home, job/school, and financial demands5 (questions 36–39 DDC). Child worry and anxiety was assessed at baseline with the T score from the Revised Child Manifest Anxiety Scale-26. (See the online supplement for instruments and questions used).
Diary cards were completed daily by 46 caregiver-child pairs for a median of 12 weeks (range 1–12). Children were 6–11 years old, had a physician diagnosis of persistent asthma for ≥ 1 year, reported ≥ 1 nocturnal asthma symptom in the past 6 months, and slept in the same residence as their caregiver on 7 nights in a usual week. Exclusion criteria included other chronic lung disease, prematurity (<34 weeks gestation), obstructive sleep apnea or sleep-disordered breathing, GERD diagnosis or treatment, ADHD or other psychiatric disorder, and psychostimulant or anticonvulsant medication use. This study was conducted in accordance with the institutional review board with written informed consent and assent.
Descriptive statistics were performed for baseline characteristics. Comparisons of categorical variables employed Chi-Square tests and continuous variables employed Spearman correlation tests. Logistic regressions were also performed. All analyses were performed with SAS version 9.3.
At enrollment, children were 8.9 ± 1.7 years old, with 52% male, 61% Caucasian, and 28% Medicaid (see Table S2 for baseline characteristics). 66% had baseline C-ACT score of ≥ 20. During the 12 weeks, 59% of children had ≥1 awakening from asthma. 80% of children had ≥1 awakening for another reason besides asthma. Children who had ≥1 awakening at night from asthma were younger (p=0.028) and reported more frequent controller use (p=0.038) than children with no asthma awakenings. There were no significant associations between nocturnal asthma awakenings and gender, insurance, step therapy, baseline C-ACT, allergic rhinitis diagnosis or season of enrollment.
Daily global stress was rated as very bad 1.4%, bad 4.2%, good 46.3%, and very good 48.1% of days. 39.1% of children had ≥1 very bad day, 63.0% had ≥1 bad day, 97.8% had ≥1 good day, and 93.5% had ≥1 very good day. Awakening from asthma that night was similarly frequent after days rated as very bad, bad or good, but awakening was significantly more likely after days rated as very bad, bad or good compared to days rated as very good (OR 2.2, 95% CI 1.5–3.1) (Figure 1). This association remained significant when controlling for prednisone use that day (OR 2.1, 95% CI 1.5–3.1) or for albuterol use that day (OR 1.8, 95% CI 1.19–2.6). There was no association between child daily global stress and awakening for reasons besides asthma that night (p=0.69).
Figure 1.
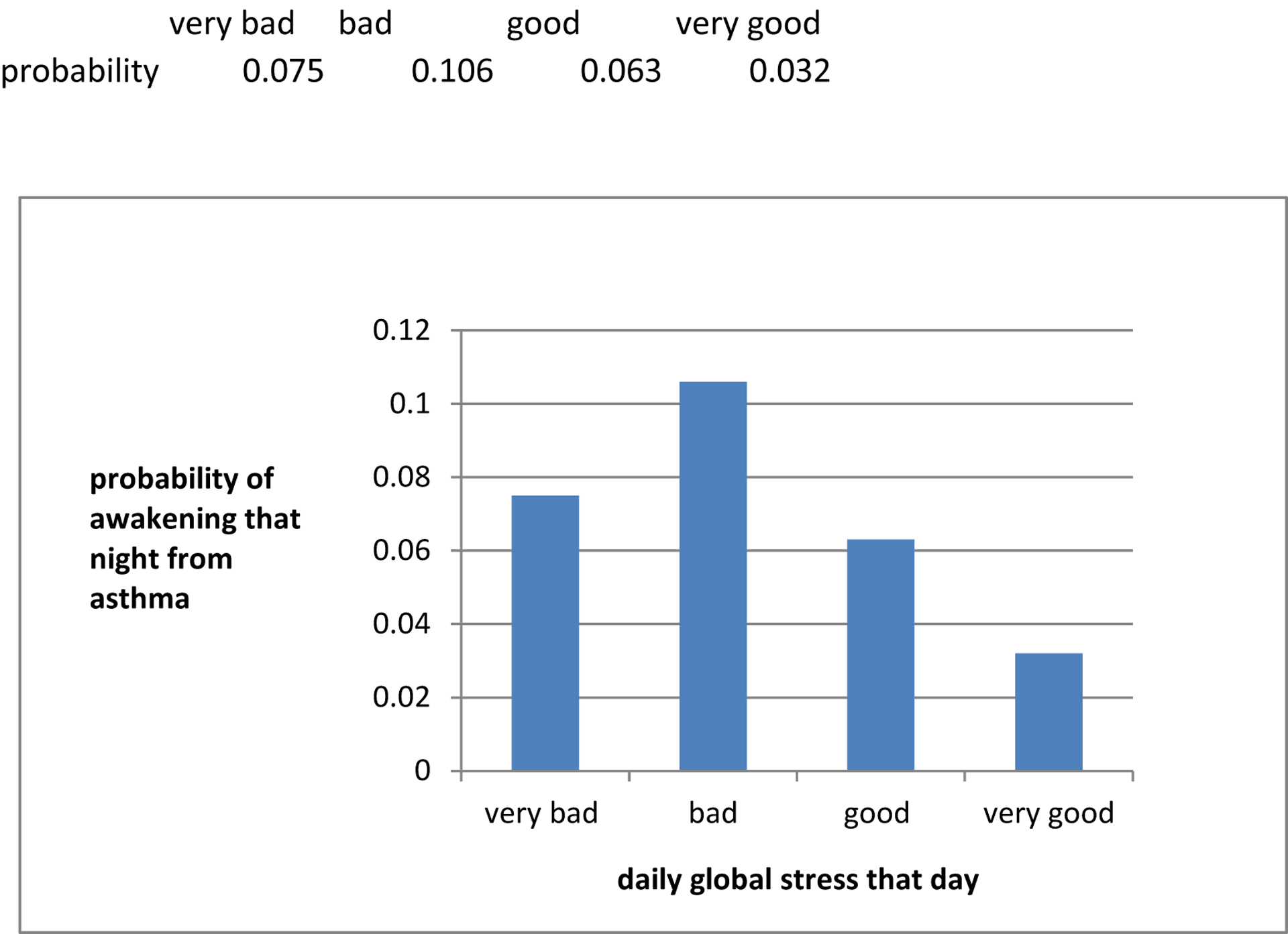
Probability of awakening that night from asthma is related to child daily global stress that day. * denotes that days with daily global stress of very bad, bad or good have significantly greater frequency of nocturnal awakenings from asthma that night than days with daily global stress of very good (OR 2.2, 95% CI 1.5–3.1).
Greater child-reported worry and anxiety was associated with higher percentages of days rated very bad (Spearman correlation=0.48, p=0.0025), days the child experienced negative emotions “a lot” (Spearman correlation=0.61, p=0.0011), and days that events made the child feel “very bad” (Spearman correlation=0.83, p=0.011). Although there was no daily measure that included all facets of anxiety, when children responded “today I was worried a lot”, they had greater likelihood of rating their day as very bad (p<0.0001). When children responded “today I was worried not at all”, they had lower likelihood of rating their day as very good (p<0.0001). Children were also more likely to report daily global stress as very bad when they experienced negative emotions “a lot” that day (p<0.0001). There was no association between caregiver-reported stressful demands that day with child daily global stress that day (p=0.47) or with child awakening from asthma that night (p=0.63).
Days following awakenings from asthma contained more morbidity events, including daytime albuterol use, doctor contact, missed school day, and prednisone use (all p<0.0001). There were no ED visits. The one child with hospitalization did not have asthma awakening the prior nights.
The main study finding is that greater child-perceived daily global stress significantly increases the odds of an asthma awakening that night, but not of awakening for other reasons. Nights following days rated other than “very good” are more than twice as likely to have awakenings from asthma. This association persists when adjusting for daytime asthma symptom activity reflected by albuterol and prednisone use. Although prior studies have linked chronic stress and negative life events to subsequent asthma symptoms,2, 7 this study demonstrates a relationship between acute daily stress with proximate nocturnal awakenings. It is possible that Corticotropin Releasing Hormone (CRH) is released in response to acute stress. CRH outside the brain activates lung mast cells and causes mediator release and other pro-inflammatory effects8. This mast cell activation in combination with the circadian variation with lower lung function at night could lead to bronchoconstriction and obstruction that triggers awakening from asthma. CRH also activates the HPA axis and stimulates cortisol release. Children with altered glucocorticoid receptors and inflammatory cells from chronic stress9 may have a heightened inflammatory response with acute stress as described. Surprisingly, our measures of caregiver stress were not associated with child daily global stress. It is unclear whether caregiver stressors in general do not influence children or whether other unmeasured stressors are more influential. Our baseline anxiety measure was associated with increased daily stress measures and indicates the possibility of identifying candidate children for stress-reduction intervention with a screening measure rather than daily diaries. The associated morbidity after asthma awakenings confirms our previous findings1 and provides additional clinical utility for addressing nocturnal awakenings outside of exacerbations.
The limited observational design with a lack of control participants is appropriate for our proof-of-concept study. The lack of a gold standard by which to measure daily stressors necessitated our utilization of a newly developed instrument. We used the child rating of his/her day as a surrogate measure of child daily global stress and a general measure of psychological perception of relative daily stress. We cannot specifically state what stressors contributed to or did not contribute to the formation of this perception. This measure correlated with the related measures of anxiety and negative emotions as a rough measure of construct-related validity. An additional limitation is that a child’s understanding of questions about stress and anxiety may vary with the age of the child. The main statistical limitation was lack of adjustment for repeated measures based on small sample size. Replication in a larger prospective study is merited. Shortening the diary card to make it less labor-intensive, while maintaining the focus on daily global stress and asthma symptoms, might be more acceptable for use by families in a clinical setting.
In conclusion, child-reported greater daily global stress was associated with increased likelihood of awakening from asthma that night but was not associated with awakening for a reason other than asthma. Further investigation is warranted into screening tools that can be used in clinical practice to identify children experiencing or being at risk for stressors related to nocturnal asthma symptoms. These data support the utility of developing and studying interventions that address reduction in acute stress to ultimately decrease nocturnal asthma symptoms and their associated morbidity.
Supplementary Material
Figure 2.
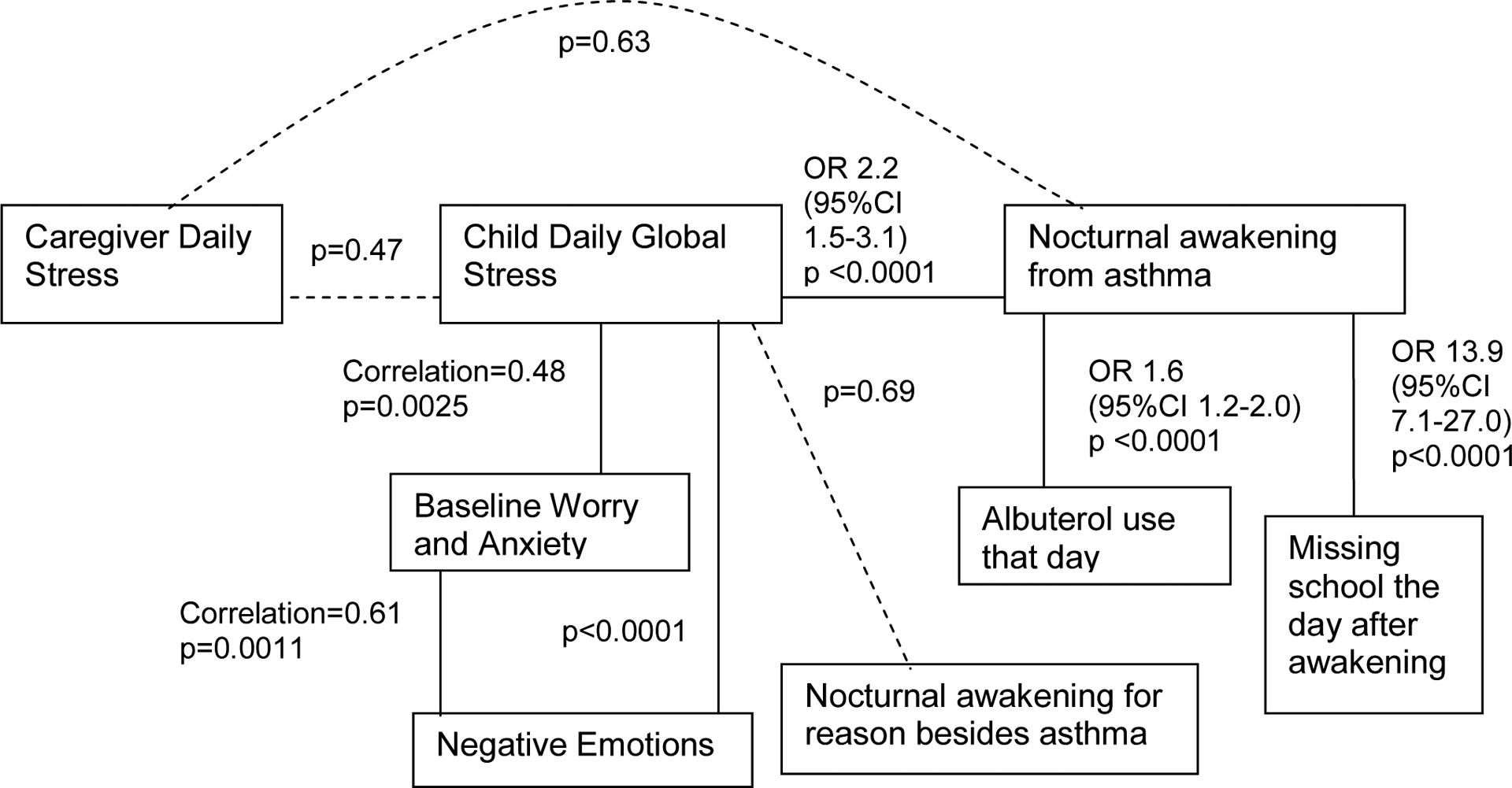
Inter-relationships between hypothesized associations; p values are shown for statistical associations between 2 measures connected by a line, e.g., child daily global stress was significantly associated with nocturnal awakening from asthma, baseline worry and anxiety and negative emotions that day. *p values without other accompanying values are for Chi Square tests. Solid lines represent associations with significant p values. Dotted lines represent associations with p values that are not significant.
Supported by:
Grant UL1 RR024992 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research and the Gail G. Shapiro Clinical Faculty Award.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Horner CC, Mauger D, Strunk RC, Graber NJ, Lemanske RF Jr., Sorkness CA, et al. Most nocturnal asthma symptoms occur outside of exacerbations and associate with morbidity. J Allergy Clin Immunol 2011; 128:977–82 e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sandberg S, Paton JY, Ahola S, McCann DC, McGuinness D, Hillary CR, et al. The role of acute and chronic stress in asthma attacks in children. Lancet 2000; 356:982–7. [DOI] [PubMed] [Google Scholar]
- 3.Mezick EJ, Matthews KA, Hall M, Kamarck TW, Buysse DJ, Owens JF, et al. Intra-individual variability in sleep duration and fragmentation: associations with stress. Psychoneuroendocrinology 2009; 34:1346–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varni JW, Rapoff MA, Waldron SA, Gragg RA, Bernstein BH, Lindsley CB. Effects of perceived stress on pediatric chronic pain. J Behav Med 1996; 19:515–28. [DOI] [PubMed] [Google Scholar]
- 5.Bolger N, DeLongis A, Kessler RC, Schilling EA. Effects of daily stress on negative mood. J Pers Soc Psychol 1989; 57:808–18. [DOI] [PubMed] [Google Scholar]
- 6.Reynolds C, Richmond B. Revised Children’s Manifest Anxiety Scale, Second Edition (RCMAS-2). 2008. [Google Scholar]
- 7.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health 2004; 94:625–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Theoharides TC, Enakuaa S, Sismanopoulos N, Asadi S, Papadimas EC, Angelidou A, et al. Contribution of stress to asthma worsening through mast cell activation. Ann Allergy Asthma Immunol 2012; 109(1):14–9. [DOI] [PubMed] [Google Scholar]
- 9.Busse WW. The brain and asthma: what are the linkages? Chem Immunol Allergy 2012; 98:1431. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


