To the Editor:
We would like to describe a study that illustrates the ability of aerosol and droplets to be generated in intraocular surgery. This is pertinent for the current pandemic where the pathogen has been reported to be transmissible by aerosol [1]. It is also important in designing measures to reduce exposure for theatre staff and risk stratification of ophthalmic procedures.
We used the Bausch and Lomb Stellaris PC machine to model aerosol generation in intraocular surgery. Fluorescein dye was added to saline. Using a black background and dark room, a blue light was used to allow better visualisation of aerosol and droplet formation. To test both instruments, an ultrasound phacoemulsification hand piece and then a 25 gauge vitrector was applied to the solution with the tip fully submerged and then lifted towards the surface of the solution. A video was taken of the turbulence caused within the solution and the aerosol/droplet generated above [2].
Phacoemulsification generated aerosol that floated away from the phaco tip with droplets travelling beyond the wrist of the hand holding the hand piece (Fig. 1a). The vitrector at both 2000 and 5000 cuts per minute caused minimal turbulence when submerged in the solution or at the surface (Fig. 1b). No aerosol or droplets were detected at any point.
Fig. 1. Aerosol and droplet generation in phacoemulsfication and vitrectomy (in vitro).
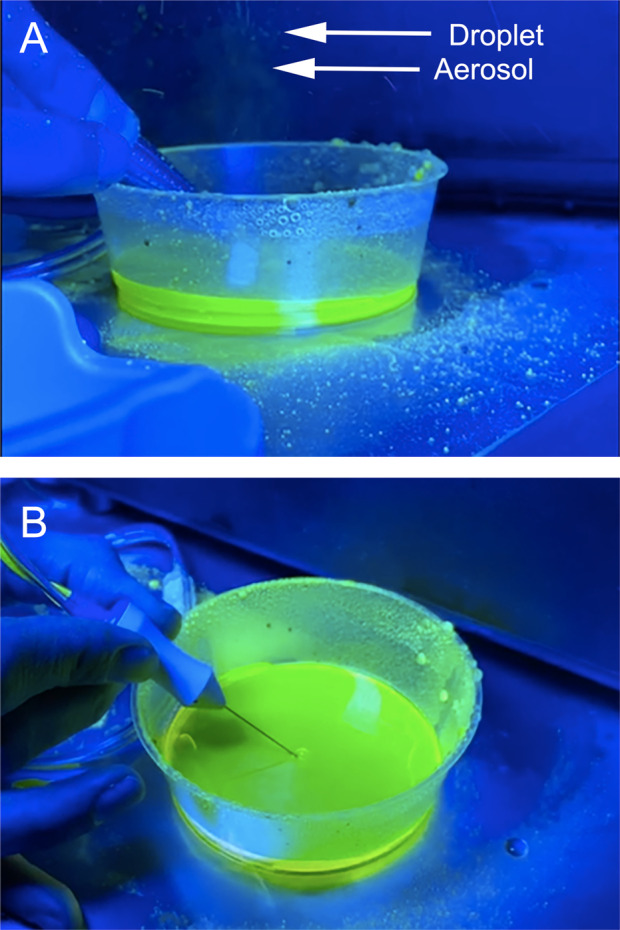
a Aerosol and droplet generation with phacoemulsification hand piece; Arrows points to aerosol and droplet. b No aerosol or droplet formation with 25 gauge vitrector.
NHS England has deemed procedures that involve the airway and high speed instruments to be aerosol generating. This has been shown in high speed saws for post mortem autopsy [3]. Vitrectors, which cut at high cut rates (10,000 cuts per minute) and phacoemulsification hand pieces (25–100 kHz), would naturally fall into this category of high speed instruments. Although we have demonstrated clearly that significant amounts of aerosol can be generated by phacoemulsification and not the vitrector, our study is dependent on visualisation of a significant amount of aerosol and limited to the sensitivity of the camera. Smaller amounts of bioaerosols that can be less than 10 μm require sophisticated instrumentation to detect [4]. Therefore, small quantities of aerosol that were not detected using our methodology may still be present.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Tamin A, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong R, Bannerjee P, Kumaran N. Aerosol generated procedures in intraocular surgery. 2020. https://youtu.be/0pjkNFwIHCA. [DOI] [PMC free article] [PubMed]
- 3.Green FHY, Yoshida K. Characteristics of aerosols generated during autopsy procedures and their potential role as carriers of infectious agents. Appl Occup Environ Hyg. 1990;5:853–8. doi: 10.1080/1047322X.1990.10387806. [DOI] [Google Scholar]
- 4.Pan YL. Detection and characterization of biological and other organic-carbon aerosol particles in atmosphere using fluorescence. J Quant Spectroc Radiat. 2015;150:12–35. doi: 10.1016/j.jqsrt.2014.06.007. [DOI] [Google Scholar]


