Abstract
Background.
A series of research reports has indicated that the use of substances such as cannabis, alcohol and tobacco are higher in youth at clinical high risk (CHR) of developing psychosis than in controls. Little is known about the longitudinal trajectory of substance use, and findings on the relationship between substance use and later transition to psychosis in CHR individuals are mixed.
Method.
At baseline and 6- and 12-month follow-ups, 735 CHR and 278 control participants completed the Alcohol and Drug Use Scale and a cannabis use questionnaire. The longitudinal trajectory of substance use was evaluated with linear mixed models.
Results.
CHR participants endorsed significantly higher cannabis and tobacco use severity, and lower alcohol use severity, at baseline and over a 1-year period compared with controls. CHR youth had higher lifetime prevalence and frequency of cannabis, and were significantly younger upon first use, and were more likely to use alone and during the day. Baseline substance use did not differentiate participants who later transitioned to psychosis (n = 90) from those who did not transition (n = 272). Controls had lower tobacco use than CHR participants with a prodromal progression clinical outcome and lower cannabis use than those with a psychotic clinical outcome at the 2-year assessment.
Conclusions.
In CHR individuals cannabis and tobacco use is higher than in controls and this pattern persists across 1 year. Evaluation of clinical outcome may provide additional information on the longitudinal impact of substance use that cannot be detected through evaluation of transition/non-transition to psychosis alone.
Keywords: Alcohol, cannabis, prodrome, substance use, tobacco
Introduction
Recent research has begun to explore substance use in those who are at risk of developing psychosis. These young people have been described as being at clinical high risk (CHR) or ultra high risk of psychosis. The CHR state is characterized by the presence of subthreshold psychotic symptoms, brief intermittent psychotic symptoms, or family history of psychosis and recent decline in functioning (McGlashan et al. 2010). Interest in substance use in this population has developed, first, because it is well established that people with schizophrenia and other psychotic disorders have increased rates of substance use relative to the general population (Regier et al. 1990), and second, there has been an increase in epidemiological studies suggesting a role for cannabis in the onset of psychosis (Caspi et al. 2005; Moore et al. 2007; Kuepper et al. 2011; Fusar-Poli et al. 2012).
A recent review of the literature (Addington et al. 2014) reported on 10 studies evaluating substance use in CHR samples. Cannabis, alcohol and tobacco were consistently reported as the most commonly used substances. The use of other substances including hallucinogens, opioids, sedatives, stimulants, amphetamines, ecstasy and solvents was either negligible or absent. Cannabis and tobacco use was reportedly higher than in healthy controls (Auther et al. 2012), with similar rates observed amongst those experiencing a first episode of psychosis (Addington & Addington, 2007; Barnett et al. 2007; Cooper et al. 2012). Interestingly, only two of the CHR studies reported a relationship between substance use and transition to psychosis (Kristensen & Cadenhead, 2007; Cannon et al. 2008) whereas others reported no significant relationships between use severity and later transition to psychosis (Phillips et al. 2002; Ruhrmann et al. 2010; Thompson et al. 2011; Auther et al. 2012). These results were supported in a newly published study (Buchy et al. 2014) that demonstrated that substance abuse did not contribute to the transition to psychosis in CHR youth.
There are several limitations with current studies examining substance use in those at CHR of psychosis (Addington et al. 2014). First, the majority of studies lack details on the severity and frequency of substance use. Second, only one study included a healthy comparison group (Auther et al. 2012), leaving unclear the prevalence of substance use in CHR youth relative to youth in the general population. Third, little is known about the change in substance use over time in this population. Fourth, in studies examining the substance use-transition to psychosis link, some recorded patterns of cannabis use only (Korver et al. 2010) whereas other studies grouped the use of any substance into one variable (Cannon et al. 2008; Thompson et al. 2011). Fifth, studies that reported on smaller sample sizes may be underpowered to detect an effect of substance use on transition to psychosis. Further details on cannabis use in particular also deserve further evaluation as there are some results suggesting that cannabis use may be related to severity of attenuated psychotic symptoms (Corcoran et al. 2008; Korver et al. 2010).
The aim of the present study was to evaluate in a large sample of CHR youth: (1) the prevalence, severity and frequency of substance use, as well as a more detailed assessment of cannabis use, relative to a healthy control group; (2) the relationship between substance use and participant demographics as well as severity of attenuated psychotic symptoms and negative symptoms; (3) change in substance use over a 1-year period; (4) substance use between those who made the transition to psychosis and those who did not; and (5) substance use amongst different groups defined by their clinical outcome after 2 years in the study, i.e. those who made the transition to psychosis, with those who did not but still have attenuated psychotic symptoms and with those whose attenuated psychotic symptoms are in remission.
Method
Participants
All participants were recruited as part of the eight-site North American Prodrome Longitudinal Study 2 (NAPLS-2) (Addington et al. 2012) which was established to investigate predictors and mechanisms of transition to psychosis. As described in Addington et al. (2012) all participants are help-seekers and are responding to similar recruitment strategies across sites. The final NAPLS-2 sample consists of 765 CHR participants and 280 healthy controls. This paper reports on the 735 CHR participants (423 male, 312 female) and 278 healthy controls (140 male, 138 female) who completed baseline substance use assessments. All CHR participants were required to meet the Criteria of Prodromal Syndromes (COPS) using the Structured Interview for Prodromal Syndromes (SIPS) (McGlashan et al. 2010). Participants were excluded if they met criteria for any current or lifetime Axis I psychotic disorder, intelligence quotient <70 based on the Wechsler Abbreviated Scale of Intelligence (Wechsler, 1999), past or current history of central nervous system disorder or Diagnostic and Statistical Manual of Mental Disorder, 4th edition (DSM-IV) criteria for current substance dependence disorder. Control participants were also excluded if they had a first-degree relative with a current or past psychotic disorder or any other disorder involving psychotic symptoms, could not meet criteria for any prodromal syndrome, any current or past psychotic disorder or a cluster A personality disorder diagnosis, and could not be currently using psychotropic medication. A more detailed description of participant details is provided elsewhere (Addington et al. 2012).
A proportion of those individuals (362 CHR participants, 142 healthy controls) who had completed the final 2-year assessment of the NAPLS-2 project and provided Alcohol and Drug Use Scale (AUS/DUS; Drake et al. 1996) ratings were included in order to examine the association of baseline substance use to later clinical outcome, i.e. clinical status at the 2-year follow-up. This smaller sample included 90 participants (58 male, 32 female) who had made the transition to psychosis.
Informed consent was obtained from those who met criteria and were judged fully competent to give consent. Parental consent was obtained from parents/guardians of participants who were under the age of 16 years. The study was approved by the institutional review boards of all eight NAPLS-2 sites.
Measures
The SIPS and the Scale for Assessment of Prodromal Symptoms (SOPS) (McGlashan et al. 2010) were used to assess criteria for a prodromal syndrome and severity of attenuated positive symptoms and negative symptoms. The Structured Clinical Interview for DSM-IV (SCID; First et al. 1998) was used to assess for current and lifetime substance abuse and dependence.
Alcohol and drug use was rated using the AUS/DUS (Drake et al. 1996) which records severity (1 = abstinent, 2 = use without impairment, 3 = abuse, 4 = dependence) and frequency of use (0 = no use, 1 = once or twice per month, 2 = 3–4 times per month, 3 = 1–2 times per week, 4 = 3–4 times per week, 5 = almost daily) in the last month. Frequency of tobacco use was the only item rated differently (0 = no use, 1 = occasionally, 2 = less than 10 per day, 3 = 11–25 per day, 4 = more than 25 per day). Ratings were collected for tobacco, alcohol, marijuana, cocaine, opiates, phencyclidine (PCP), amphetamines, methylenedioxy-methylamphetamine (MDMA), γ-hydroxybutyric acid (GHB), huffing (inhaling glue, other volatiles), hallucinogens, and other drugs. Based on commonly used measures and interview questions in the literature (Arseneault et al. 2002; Caspi et al. 2005; Henquet et al. 2005) we also enquired if cannabis had ever been used, how many times it had been used across one’s lifetime, whether use was current and/or past, age at first use, frequency and pattern of use, environment of use (socially or alone), and time of day most frequently used (morning, evening, both).
Clinical status at the 2-year follow-up was determined in the following way: (1) healthy control (has never met criteria for a prodromal risk syndrome); (2) remission (scores of 2 or less on the five positive symptoms on the SOPS scale); (3) symptomatic (not currently meeting criteria for a prodromal risk syndrome but having ratings of 3–5 on any one of the five positive symptoms on the SOPS); (4) prodromal progression [currently meeting criteria for one of the at-risk syndromes; Attenuated Positive Symptom State (APSS), Genetic Risk and Deterioration (GRD), Brief Intermittent Psychotic State (BIPS)]; and (5) psychotic (currently meeting criteria for a psychotic disorder or evidencing scores of 6 on one or more positive symptoms of the SOPS).
Statistical analysis
We used χ2 or Fisher’s exact analyses for categorical variables and t tests for continuous variables to compare CHR and control groups on demographics variables. The use of substances other than alcohol, tobacco or cannabis was either minimal or absent; therefore the use of these substances was not considered further in statistical analyses. Spearman’s correlations were used to measure associations of cannabis use with demographics and symptom severity. Linear regression was used to determine predictors of continuous dependent variables. To account for any missing data and intra-participant correlation over time, mixed modeling was used to examine the group and time effects on AUS/DUS tobacco, alcohol and cannabis scores at baseline. In our sample of 362 CHR and 142 control participants who had been followed for 24 months, the Kruskal–Wallis test was used to compare the five groups based on 2-year clinical status (1 = healthy control; 2 = remission; 3 = symptomatic; 4 = prodromal progression; 5 = psychotic) on baseline substance use. We also compared those who had made the transition to psychosis with those who had not on baseline substance use using the Mann–Whitney test. The critical p value for the AUS/DUS analyses was set to p = 0.017 following Bonferroni correction for multiple comparisons of the three substances. Statistical analyses were conducted using SPSS 20.0 (USA).
Procedures
All eight sites (Emory University, Harvard University, University of Calgary, University of California at Los Angeles, University of California at San Diego, University of North Carolina at Chapel Hill, Yale University, and Zucker Hillside Hospital) recruited CHR individuals and controls. Raters were experienced research clinicians who demonstrated adequate reliability at routine reliability checks. ‘Gold standard’ post-training agreement on the critical threshold for determining initial eligibility and subsequent transition status based on the SIPS was excellent (k = 0.90). The principal investigator, clinical psychiatrist or psychologist at each site conducted a comprehensive clinical assessment to determine if entry criteria were met. J.A. chaired weekly conference calls to review criteria for all individuals admitted to the study. Clinical assessments that included the AUS/DUS and the SOPS were conducted at baseline, and at 6 and 12 months. The study protocols and informed consents were reviewed and approved by the ethical review boards of all eight study sites.
Results
Demographics
As summarized in Table 1, control participants were older, had more males and more years of education than those of the CHR group.
Table 1.
Demographic and clinical characteristics of the groups
| CHR (n = 735) | Controls (n = 278) | Statistics | p | |
|---|---|---|---|---|
| Sex | ||||
| Male | 424 (57.6) | 140 (50.4) | χ2 = 4.23 | 0.04 |
| Female | 311 (42.4) | 138 (49.6) | ||
| Race | ||||
| First Nations | 14 (1.9) | 4 (1.4) | χ2 = 6.69 | 0.67 |
| Asian | 55 (7.4) | 30 (10.8) | ||
| Black | 109 (14.8) | 48 (17.3) | ||
| Latin America/Middle East/White | 461 (62.7) | 166 (59.7) | ||
| Native Hawaiian/Pacific Islander | 3 (0.4) | 1 (0.4) | ||
| Inter-racial | 92 (12.5) | 29 (10.4) | ||
| Mean age, years (s.d.) | 18.5 (4.2) | 19.6 (4.7) | t = 3.89 | <0.001 |
| Mean duration of education, years (s.d.) | 11.3 (2.8) | 12.7 (3.6) | t = 6.43 | <0.001 |
Data are given as number of participants (percentage) unless otherwise indicated.
CHR, Clinical high risk; s.d., standard deviation.
SCID diagnoses
Of the participants, 55 (7.5%) CHR and two (0.8%) control participants met DSM-IV criteria for a current substance use disorder (χ2 = 17.04, p < 0.001, φ = 0.13). Cannabis abuse (0.4%) and dependence in remission (0.4%) were the only current diagnoses in the control group. Current diagnoses in CHR participants included cannabis (abuse, 3.3%; dependence in remission, 1.8%), alcohol (abuse, 2.0%; dependence in remission, 1.1%), amphetamine (abuse, 0.1%; dependence in remission, 0.1%), cocaine dependence in remission (0.1%), hallucinogen abuse (0.1%), other (0.4%) and polysubstance dependence in remission (0.1%).
For these individuals, it appeared at initial screening that they did not have a substance use problem; however, at the later baseline assessment when rated with the SCID it became apparent that they met criteria for a diagnosable substance use disorder. As the total n’s for alcohol and cannabis dependence were relatively small these participants were included in statistical analyses.
AUS/DUS ratings at baseline
The use of substances other than alcohol, tobacco or cannabis was either minimal or absent; therefore the use of these substances was not considered further in relation to demographics, SOPS positive symptoms, transition to psychosis or clinical outcome. However, rates of use of all substances are presented in Table 2. When considering substance use severity as determined by the AUS/DUS, in the entire sample, males had significantly higher baseline tobacco (p < 0.01) and cannabis use (p < 0.01), but not alcohol use (p = 0.82). Being older significantly correlated with increased tobacco (r = 0.14, p < 0.001, r2 = 0.02), alcohol (r = 0.39, p < 0.001, r2 = 0.15) and cannabis use at baseline (r = 0.07, p < 0.05, r2 = 0.004).
Table 2.
Severity of substance use as measured with the AUS/DUS at baseline in CHR participants and controlsa
| Baseline AUS/DUS assessment |
CHR (n = 735) |
Controls (n = 278) |
|---|---|---|
| Alcoholb | ||
| Abstinent | 441 (60.0) | 136 (49.1) |
| Use without impairment | 273 (37.1) | 141 (50.9) |
| Abuse | 16 (2.2) | 0 (0.0) |
| Dependence | 5 (0.7) | 0 (0.0) |
| Tobaccoc | ||
| Abstinent | 560 (76.2) | 256 (92.1) |
| Use without impairment | 163 (22.2) | 20 (7.2) |
| Abuse | 5 (0.7) | 0 (0.0) |
| Dependence | 7 (1.0) | 0 (0.0) |
| Cannabis | ||
| Abstinent | 563 (76.6) | 252 (90.6) |
| Use without impairment | 144 (19.6) | 26 (9.4) |
| Abuse | 26 (3.5) | 0 (0.0) |
| Dependence | 2 (0.3) | 0 (0.0) |
| Cocaine | ||
| Abstinent | 727 (98.9) | 278 (100.0) |
| Use without impairment | 8 (1.1) | 0 (0.0) |
| Opiates | ||
| Abstinent | 732 (99.6) | 278 (100.0) |
| Use without impairment | 2 (0.3) | 0 (0.0) |
| Abuse | 1 (0.1) | 0 (0.0) |
| PCP | ||
| Abstinent | 734 (99.9) | 278 (100.0) |
| Use without impairment | 1 (0.1) | 0 (0.0) |
| Amphetamines | ||
| Abstinent | 732 (99.6) | 278 (100.0) |
| Use without impairment | 3 (0.4) | 0 (0.0) |
| MDMA | ||
| Abstinent | 726 (98.8) | 278 (100.0) |
| Use without impairment | 9 (1.2) | 0 (0.0) |
| GHBb | ||
| Abstinent | 735 (100.0) | 278 (100.0) |
| Huffing | ||
| Abstinent | 735 (100.0) | 278 (100.0) |
| Hallucinogens | ||
| Abstinent | 724 (98.5) | 276 (99.3) |
| Use without impairment | 11 (1.5) | 2 (0.7) |
| Other substances | ||
| Abstinent | 724 (98.5) | 278 (100.0) |
| Use without impairment | 11 (1.5) | 0 (0.0) |
Data are given as number of participants (percentage).
AUS/DUS, Alcohol and Drug Use Scale; CHR, clinical high risk; PCP, phencyclidine; MDMA, methylenedioxy-methylamphetamine; GHB, γ-hydroxybutyric acid.
Only ratings that were endorsed have been included in this table.
Data were missing for one participant in the control group.
Data were missing for two participants in the control group.
Alcohol use at baseline did not differ between males and females in either the CHR or control group (CHR, χ2 = 0.80, p = 0.85; controls, χ2 = 1.91, p = 0.17). Significant correlations were observed between participants’ age and alcohol use in both the CHR and control groups (CHR, r = 0.36, p < 0.001; controls, r = 0.48, p < 0.001).
For the CHR group, SOPS total attenuated positive symptom score significantly correlated with baseline tobacco use (r = 0.08, p < 0.05, r2 = 0.006) and cannabis use (r = 0.12, p < 0.01, r2 = 0.01), but not alcohol use (r = −0.07, p = 0.07). Cannabis use did not significantly correlate with SOPS total negative symptoms, (r = −0.007, p = 0.85). The correlation between tobacco use and SOPS total attenuated positive symptom score was non-significant when controlling statistically for cannabis use (r = 0.03, p = 0.38). The correlation between cannabis and SOPS total attenuated positive symptom score remained significant when entering tobacco use as a covariate (r = 0.10, p = 0.009, r2 = 0.01).
Alcohol was the most frequently reported substance consumed by both CHR and control participants. Cannabis was reported as the most widely used illicit drug in both groups.
Course of substance use in the control and CHR groups based on AUS/DUS ratings
AUS/DUS ratings were available for 188 controls and 502 CHR participants at the 6-month assessment, and 197 controls and 393 CHR participants at the 12-month assessment.
Mixed modeling of tobacco scores showed that the CHR group had higher tobacco use severity compared with controls as revealed by a significant main effect of group [F = 39.2, degrees of freedom (df) = 1, 966.6; p < 0.001] (Fig. 1). The effect of time was non-significant (F = 0.04, df = 2, 1126.8; p = 0.96). No significant changes in tobacco use were observed over any time points in either group. Adding cannabis use as a covariate did not change interpretation of results.
Fig. 1.
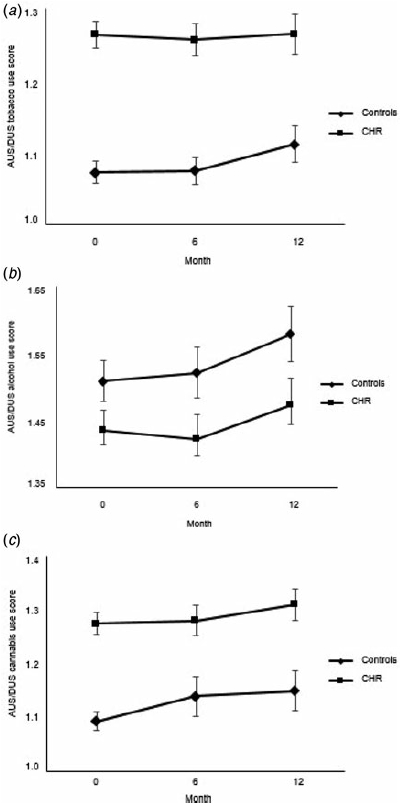
Substance use ratings for the clinical high risk (CHR) and healthy control groups for (a) tobacco, (b) alcohol and (c) cannabis. Values are means, with standard errors represented by vertical bars. AUS/DUS, Alcohol and Drug Use Scale.
Results of mixed modeling of alcohol use indicated that the control group had higher alcohol use compared with the CHR group as indicated by a significant group effect (F = 5.5, df = 1, 970.8; p = 0.02) (Fig. 1). The main effect of time was non-significant (F = 1.9, df= 2, 1216.9; p = 0.15). Over the follow-up period, controls had significantly higher alcohol use at the 12-month assessment compared with baseline p < 0.01). No significant changes in alcohol use were observed over any time points in the CHR group.
Finally, mixed modeling showed that cannabis use was significantly higher in the CHR group compared with controls (F = 27.9, df = 1, 970.5; p < 0.001) (Fig. 1). The main effect of time did not achieve significance (F = 0.53, df = 2, 1202.1; p = 0.59). No significant changes in cannabis use were observed over any time point in either group. Adding tobacco use as a covariate did not change interpretation of results. As a further test, we conducted linear mixed models to explore whether any of the attenuated psychotic symptoms covaried with substance use over the three time points. However, because use of these substances did not change over time, whereas there was significant improvement in attenuated positive symptoms (typically in the first 6 months), there was no covariation between substance use and individual attenuated psychotic symptoms.
Cannabis use questionnaire
Cannabis use data were missing for two controls and three CHR participants. As presented in Table 3, the CHR group was significantly younger than controls when participants first tried cannabis. The mean number of times that individuals had used cannabis across their lifetime was higher in the CHR group relative to the control group, as was the number of people who had ever smoked or used cannabis. The CHR group was more likely to currently use alone and during the day than controls. Groups did not differ on use frequency.
Table 3.
Rates and patterns of cannabis use over lifetime by group
| Cannabis scale | CHR (n = 732) | Controls (n = 276) | Statistics | p |
|---|---|---|---|---|
| Mean age first tried, years (s.d)a | 15.7 (2.82) | 16.6 (2.71) | t = 2.86 | 0.004 |
| Mean number of times used in lifetime (s.d.)b | 125.5 (124.90) | 63.0 (100.15) | t = 4.82 | <0.001 |
| Ever smoked/used, yes | 404 (55.2) | 110 (39.9) | χ2 = 18.98 | <0.001 |
| Currently using | 238 (32.4) | 81 (29.1) | χ2 = 9.29 | <0.01 |
| Past use only | 164 (22.3) | 27 (9.7) | ||
| Missing | 333 (45.3) | 170 (61.2) | ||
| Use frequency for current users | ||||
| Every day | 21 (2.9) | 2 (0.7) | χ2 = 9.50 | 0.22 |
| Once/twice per week | 78 (10.6) | 10 (3.6) | ||
| Once/twice per month to once/twice per year | 79 (10.7) | 23 (8.3) | ||
| Not applicable | 126 (17.1) | 35 (12.6) | ||
| Missing | 431 (58.7) | 208 (74.8) | ||
| Environment for current users | ||||
| Socially | 324 (44.1) | 100 (36.0) | χ2 = 11.01 | 0.001 |
| Alone | 64 (8.7) | 4 (1.4) | ||
| Missing | 347 (47.2) | 174 (62.6) | ||
| Time of use for current users | ||||
| During the day | 48 (6.5) | 4 (1.4) | χ2 = 19.21 | <0.001 |
| During the evening | 212 (28.8) | 80 (28.8) | ||
| Frequently during the day and evening | 141 (19.2) | 21 (7.6) | ||
| Missing | 334 (45.4) | 173 (62.2) |
Data are given as number of participants (percentage) unless otherwise indicated.
CHR, Clinical high risk; s.d., standard deviation.
Excludes participants who had never used cannabis.
Excludes never-users.
Use of multiple substances
AUS/DUS substances reported to be most commonly used together were cannabis, alcohol and tobacco. In the CHR group, of those participants who used cannabis within the past month (n = 172), 130 (75.6%) also reported using alcohol, and 95 (55.2%) reported using tobacco. Of CHR participants who used alcohol in the past month (n = 294), 122 (41.5%) also reported using tobacco and 130 (44.2%) also reported using cannabis. Co-morbid use of other substances was either negligible or absent.
Relationship between substance use and clinical status at end of study
The sample of 504 participants who had completed the 24-month end-of-study assessment and had provided AUS/DUS ratings at baseline consisted of 142 healthy controls, 109 CHR participants in remission, 92 symptomatic CHR participants, 71 CHR participants who met criteria for prodromal progression and 90 who were psychotic. Results of the Kruskal–Wallis analysis indicated that the groups significantly differed on tobacco (χ2 = 19.60, p = 0.001, η2 = 0.04) and cannabis use (χ2 = 14.41, p = 0.006, η2 = 0.03), but not on alcohol use (χ2 = 4.97, p = 0.29). Considering tobacco, post-hoc tests indicated lower use in controls as compared with CHR participants who met criteria for prodromal progression (p < 0.001), who were symptomatic (p = 0.004) and who were psychotic (p < 0.001). For cannabis use, post-hoc tests showed that controls had significantly lower use than CHR participants who were symptomatic (p = 0.005), in remission (p = 0.01) and were psychotic (p < 0.001). For the analysis of tobacco, controls had significantly lower use of tobacco than people who were prodromal progression, while controlling for cannabis use (p = 0.001). For the analysis of cannabis, controls had significantly lower use of cannabis than people who were psychotic, while controlling for tobacco use (p = 0.007).
Comparison of the 90 who made the transition to psychosis with the 272 CHR participants who did not demonstrated no differences in tobacco use severity or frequency (U = 11495.5, p = 0.24; U = 11 638.0, p = 0.35, respectively); alcohol use severity or frequency (U = 12 019.0, p = 0.76, U = 12 196.0, p = 0.95, respectively), or cannabis use severity (U = 11 341.0, p = 0.16) or frequency (U = 114 689.5, p 0.24). These results of the analysis of tobacco remained non-significant when controlling for cannabis use (p = 0.007). Similarly, the analysis of cannabis was also non-significant when controlling for tobacco use (p = 0.007). Age at first use of cannabis did not significantly differ between these two groups (t = 0.85, p = 0.40).
All t tests and χ2 tests survived Bonferroni correction for 13 multiple comparisons, except for the analysis of cannabis ever smoked: yes/no (p = 0.01), in Table 3.
Discussion
Several noteworthy findings emerged from this prospective study in youth at CHR of psychosis. First, CHR participants endorsed significantly higher cannabis and tobacco use, and lower mean severity of alcohol use, at baseline and over a 1-year period compared with controls. As reported previously, the use of other illicit drugs was relatively rare (Addington et al. 2014). Second, relative to controls, CHR youth had higher lifetime prevalence and frequency of cannabis use, were significantly younger at age of first use, and were more likely to use during the day than evening and alone than socially. Third, baseline substance use could not differentiate participants who later transitioned to psychosis from those who did not transition. Finally, CHR participants who met criteria for a symptomatic, prodromal progression or psychotic clinical outcome at the 2-year assessment reported greater use of tobacco at baseline than controls but not CHR participants in remission.
This study found that 32.4% of CHR participants were currently using cannabis, which falls in the midrange of previously published data (Phillips et al. 2002; Dragt et al. 2010; Korver et al. 2010; Gill et al. 2013). However, 5.15% of CHR subjects met criteria for a cannabis use disorder which is similar to some (Corcoran et al. 2008) but lower than most previously published reports (Kristensen & Cadenhead, 2007; Machielsen et al. 2010; Dragt et al. 2012), probably due to the exclusion of participants with a substance use disorder in the current NAPLS-2 cohort. The results complement previous works that have established a higher lifetime history of cannabis in CHR subjects compared with controls (Auther et al. 2012; Stowkowy & Addington, 2013).
The results of this study support a growing literature on elevated rates of tobacco use in youth at CHR for psychosis relative to non-clinical youth (Addington et al. 2014), and a previous study documenting heightened cannabis use in CHR youth relative to controls (Auther et al. 2012). These analyses augment prior research by documenting that this pattern persists across the first year after inclusion into a CHR for psychosis research program. Very recent data suggest that one reason for continued use of cannabis in CHR individuals could be to ‘enhance mood’ (e.g. makes you feel good, to get high) (Gill et al. 2013), and this has also been reported in people with psychoses (Spencer et al. 2002; Thornton et al. 2012). A secondary motivation may be related to social motives (e.g. it is what most of my friends do, it makes social gatherings more enjoyable), although this may be less applicable to our current sample given their preference to use alone rather than socially. Alternatively, social motives may be an impetus of alcohol use (Thornton et al. 2012). Cannabis use was also found to be significantly associated with increased attenuated psychotic symptoms in our CHR participants; however, the strength of this relationship was weak (Dancey & Reidy, 2004) and may reflect an overpowered CHR sample. Moreover, there is little evidence to suggest that CHR participants use cannabis to ‘self-medicate’ their subthreshold psychotic symptoms (Gill et al. 2013). In any case, future work on this topic may want to track longitudinal cannabis use in tandem with self-reported motives for cannabis use in CHR individuals.
Results from the additional cannabis items revealed that CHR subjects were more likely to use alone and during the day as compared with controls who were more likely to use in a social context and at evening. Here it is relevant to note that CHR youth also endorsed lower alcohol use than controls. This combination of results (i. e. lesser alcohol consumption, solitary cannabis use and daytime use) may indicate lower sociability in general in these individuals (Thornton et al. 2012). There is evidence in schizophrenia samples that patients’ readiness to change may be an important factor in their willingness to decrease cannabis use or engage in substance use treatment interventions (Kolliakou et al. 2011). Although the present work focuses on youth at risk of psychotic disorders, and not schizophrenia per se, it may be interesting to evaluate CHR participants’ readiness to change this problematic behavior, and the role of factors such as motivation, recognition and ambivalence (Miller & Tonigan, 1996) in this population may be of interest for future research, and may facilitate the development of more effective prevention and intervention strategies.
Baseline substance use did not differ in CHR participants who transitioned to psychosis as compared with those who did not transition, which is supported by the current literature on this topic (Addington et al. 2014). In particular, the present investigation is the fourth large study to find that baseline cannabis use does not predict psychosis onset (Phillips et al. 2002; Auther et al. 2012; Buchy et al. 2014). Moreover, age at first cannabis use did not differ between CHR participants who transitioned to psychosis and those who did not. However, the analysis is based on very few observations for ‘abuse’ or ‘dependence’, so their contribution is probably unremarkable. Samples of CHR participants with heavier substance use may provide larger representations in these categories, which may provide more meaningful conclusions about heavy substance use and transition to psychosis. Interestingly, retrospective data have indicated that progression to daily cannabis use prior to the onset of psychosis may be linked to an elevated risk of onset of psychotic symptoms (Compton et al. 2009; Clausen et al. 2014). In this regard, change in use severity may be an important factor in the transition to psychosis, and may be potentially informative for future research.
Much research has focused on the impact of substance use on transition to psychosis in CHR individuals. Our analysis of the effects of baseline substance use on 2-year clinical state permitted the observation that cannabis use and tobacco use are differentially represented across qualitatively distinct clinical outcome groups. In particular, our findings suggest that cannabis exposure exerts a negative impact in some CHR participants, particularly in people on the pathway toward a symptomatic or psychotic clinical outcome, but also in those who achieved remission. Therefore, contradictory claims that substance use is (Kristensen & Cadenhead, 2007; Cannon et al. 2008) or is not (Phillips et al. 2002; Ruhrmann et al. 2010; Thompson et al. 2011; Auther et al. 2012) a reliable factor for transition to psychosis may be explained by the fact that a dichotomous CHR group (transitioned, did not transition) was evaluated without considering the heterogeneity of prodromal clinical state over time.
These results should be considered in the context of several methodological limitations. Individuals at CHR for psychosis are difficult to find; thus, there may be limitations in sampling as the sample consists of all help-seekers that sites could possibly recruit, which may have implications for the external validity of the results. Details on cannabis use including type and dosage were not collected and therefore their potential impact on psychosis onset or clinical outcome cannot be determined. Limited observations for ‘abuse’ or ‘dependence’ were recorded for alcohol, cannabis and tobacco due to exclusion criteria, and this may limit an ability to detect a contribution of heavy substance use to psychotic transition and/or clinical outcome. Missing substance use data at the 6- and 12-month assessments should also be noted as a limitation. Alcohol, tobacco and cannabis were the most commonly used substances together, leaving unclear the relative contribution of these variables to clinical outcome. Urine toxicology data would have also provided important biological information on cannabis use in the sample. Moreover, as with other studies in psychiatry comparing cases with controls, in the present multi-site study we cannot control for background genetic and environmental variation which might otherwise explain the observed association. Nevertheless, the results expand an accumulating literature describing higher baseline substance use rates, and now a stable 12-month progression, in CHR as compared with healthy comparison subjects. Moreover, the results point to the impact of baseline cannabis and tobacco use on 2-year clinical outcome. A recent stream of research has identified early developmental adversities including trauma and stress in adolescents as a moderator of the effects of cannabis use on psychotic experiences, as well as the trajectory of psychotic experiences in cannabis users who later develop psychosis (Henquet et al. 2008), and may be of interest in future work on substance use in youth at CHR for psychosis.
In conclusion, CHR participants used more cannabis and tobacco and less alcohol at baseline and over 1 year compared with controls. CHR participants also had higher lifetime prevalence and frequency of cannabis use, began using cannabis at a younger age, and were more likely to use during the day than evening and alone than socially. Substance use was similar across CHR participants who did and did not transition to psychosis. Finally, after 2 years in the study, CHR participants with a symptomatic, prodromal progression or psychotic clinical outcome reported greater tobacco use at baseline than controls, though only the latter survived when controlling for cannabis use. CHR participants with a psychotic clinical outcome after 2 years had significantly higher baseline cannabis use than controls when adjusting for cannabis use.
Acknowledgements
This study was supported by the National Institute of Mental Health (NIMH) [grant U01MH081984 to J.A.; grants U01 MH081928; P50 MH080272; Commonwealth of Massachusetts SCDMH82101008006 to L.J.S.; grants R01 MH60720, U01 MH082022 and K24 MH76191 to K. S.C.; grant U01MH081902 to T.D.C.; P50 MH066286 (Prodromal Core) to C.E.B.; grant U01MH082004 to D.O. P.; grant U01MH081988 to E.F.W.; grant U01MH08022 to S.W.W.; and UO1 MH081857-05 grant to B.A.C.]. The NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
We would like to thank: J. Stowkowy, T. Raedler, L. McGregor, D. Marulanda, L. Legere, L. Liu, C. Marshall, E. Falukozi, E. Fitton, L. McAusland and K. Smith (University of Calgary); T. Alderman, K. Shafer, I. Domingues, A. Hurria and H. Mirzakhanian (UCSD); B. Walsh, J. Saksa, N. Santamauro, A. Carlson, J. Kenney and B. Roman (Yale University); K. Woodberry, J. Giuliano, W. Stone, J. M. Rodenhiser, L. Tucker, R. Serur, G. Min and R. Szent-Imrey (Beth Israel Deaconess Medical Center/Harvard); C. Bearden, P. Bachman, J. Zinberg, S. DeSilva, A. Andaya and S. Uguryan (UCLA); J. Brasfield and H. Trotman (Emory University); A. Pelletier, K. Lansing, H. Mates, J. Nieri, B. Landaas, K. Graham, E. Rothman, J. Hurta and Y. Sierra (University of North Carolina); and A. Auther, R. Carrion, M. McLaughlin and R. Olsen (Zucker Hillside Hospital).
References
- Addington J, Addington D (2007). Patterns, predictors and impact of substance use in early psychosis: a longitudinal study. Acta Psychiatrica Scandinavica 115, 304–309. [DOI] [PubMed] [Google Scholar]
- Addington J, Cadenhead KS, Cornblatt BA, Mathalon DH, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Addington JA, Cannon TD (2012). North American Prodrome Longitudinal Study (NAPLS 2): overview and recruitment. Schizophrenia Research 142, 77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Case N, Saleem MM, Auther AM, Cornblatt BA, Cadenhead KS (2014). Substance use in clinical high risk for psychosis: a review of the literature. Early Intervention in Psychiatry 8, 104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE (2002). Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 325, 1212–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auther AM, McLaughlin D, Carrion RE, Nagachandran P, Correll CU, Cornblatt BA (2012). Prospective study of cannabis use in adolescents at clinical high risk for psychosis: impact on conversion to psychosis and functional outcome. Psychological Medicine 42, 2485–2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett JH, Werners U, Secher SM, Hill KE, Brazil R, Masson K, Pemet DE, Kirkbride JB, Murray GK, Bullmore ET, Jones PB (2007). Substance use in a population-based clinic sample of people with first-episode psychosis. British Journal of Psychiatry 190, 515–520. [DOI] [PubMed] [Google Scholar]
- Buchy L, Perkins D, Woods SW, Liu L, Addington J (2014). Impact of substance use on conversion to psychosis in youth at clinical high risk of psychosis. Schizophrenia Research 156, 277–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R (2008). Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Archives of General Psychiatry 65, 28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, Harrington H, Taylor A, Arseneault L, Williams B, Braithwaite A, Poulton R, Craig IW (2005). Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene x environment interaction. Biological Psychiatry 57, 1117–1127. [DOI] [PubMed] [Google Scholar]
- Clausen L, Hjorthoj CR, Thorup A, Jeppesen P, Petersen L, Bertelsen M, Nordentoft M (2014). Change in cannabis use, clinical symptoms and social functioning among patients with first-episode psychosis: a 5-year follow-up study of patients in the OPUS trial. Psychological Medicine 44, 117–126. [DOI] [PubMed] [Google Scholar]
- Compton MT, Kelley ME, Ramsay CE, Pringle M, Goulding SM, Esterberg ML, Stewart T, Walker EF (2009). Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodrome and age at onset of psychosis in first-episode patients. American Journal of Psychiatry 166, 1251–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper J, Mancuso SG, Borland R, Slade T, Galletly C, Castle D (2012). Tobacco smoking among people living with a psychotic illness: the second Australian Survey of Psychosis. Australian and New Zealand Journal of Psychiatry 46, 851–863. [DOI] [PubMed] [Google Scholar]
- Corcoran CM, Kimhy D, Stanford A, Khan S, Walsh J, Thompson J, Schobel S, Harkavy-Friedman J, Goetz R, Colibazzi T, Cressman V, Malaspina D (2008). Temporal association of cannabis use with symptoms in individuals at clinical high risk for psychosis. Schizophrenia Research 106, 286–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dancey C, Reidy J (2004). Statistics without Maths for Psychology: using SPSS for Windows. Prentice Hall: London. [Google Scholar]
- Dragt S, Nieman DH, Becker HE, van de Fliert R, Dingemans PM, de Haan L, van Amelsvoort TA, Linszen DH (2010). Age of onset of cannabis use is associated with age of onset of high-risk symptoms for psychosis. Canadian Journal of Psychiatry 55, 165–171. [DOI] [PubMed] [Google Scholar]
- Dragt S, Nieman DH, Schultze-Lutter F, van der Meer F, Becker H, de Haan L, Dingemans PM, Birchwood M, Patterson P, Salokangas RK, Heinimaa M, Heinz A, Juckel G, Graf von Reventlow H, French P, Stevens H, Ruhrmann S, Klosterkötter J, Linszen DH; EPOS Group (2012). Cannabis use and age at onset of symptoms in subjects at clinical high risk for psychosis. Acta Psychiatrica Scandinavica 125, 45–53. [DOI] [PubMed] [Google Scholar]
- Drake RE, Mueser K, McHugo G (1996). Clinical rating scales. In Outcomes Assessment in Clinical Practice (ed. Sederer L and Dickey B), pp. 113–116. Williams and Wilkins: Baltimore. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW (1998). Structured Clinical Interview for DSM-IV Patient Edition (SCID-I/P V and SCID-I/NP Version 2.0). Biometric Research Department: New York. [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P (2012). Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry 69, 220–229. [DOI] [PubMed] [Google Scholar]
- Gill KE, Poe L, Azimov N, Ben-David S, Vadhan NP, Girgis R, Moore H, Cressman V, Corcoran CM (2013). Reasons for cannabis use among youths at ultra high risk for psychosis. Early Intervention in Psychiatry. Published online 26 November 2013. doi: 10.1111/eip.12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henquet C, Di Forti M, Morrison P, Kuepper R, Murray RM (2008). Gene-environment interplay between cannabis and psychosis. Schizophrenia Bulletin 34, 1111–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henquet C, Krabbendam L, Spauwen J, Kaplan C, Lieb R, Wittchen HU, van Os J (2005). Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 330, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolliakou A, Joseph C, Ismail K, Atakan Z, Murray RM (2011). Why do patients with psychosis use cannabis and are they ready to change their use? International Journal of Developmental Neuroscience 29, 335–346. [DOI] [PubMed] [Google Scholar]
- Korver N, Nieman DH, Becker HE, van de Fliert JR, Dingemans PH, de Haan L, Spiering M, Schmitz N, Linszen DH (2010). Symptomatology and neuropsychological functioning in cannabis using subjects at ultra-high risk for developing psychosis and healthy controls. Australian and New Zealand Journal of Psychiatry 44, 230–236. [DOI] [PubMed] [Google Scholar]
- Kristensen K, Cadenhead KS (2007). Cannabis abuse and risk for psychosis in a prodromal sample. Psychiatry Research 151, 151–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuepper R, van Os J, Lieb R, Wittchen HU, Hofler M, Henquet C (2011). Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10 year follow-up cohort study. BMJ 342, d738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machielsen M, van der Sluis S, de Haan L (2010). Cannabis use in patients with a first psychotic episode and subjects at ultra high risk of psychosis: impact on psychotic- and pre-psychotic symptoms. Australian and New Zealand Journal of Psychiatry 44, 721–728. [DOI] [PubMed] [Google Scholar]
- McGlashan TH, Walsh BC, Woods SW (2010). The Psychosis Risk Syndrome: Handbook for Diagnosis and Follow-up. Oxford University Press: New York. [Google Scholar]
- Miller WR, Tonigan JS (1996). Assessing drinkers’ motivation for change: the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychology of Addictive Behaviors 10, 81–89. [Google Scholar]
- Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, Lewis G (2007). Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet 370, 319–328. [DOI] [PubMed] [Google Scholar]
- Phillips LJ, Curry C, Yung AR, Yuen HP, Adlard S, McGorry PD (2002). Cannabis use is not associated with the development of psychosis in an ‘ultra’ high-risk group. Australian and New Zealand Journal of Psychiatry 36, 800–806. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK (1990). Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA 264, 2511–2518. [PubMed] [Google Scholar]
- Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, Birchwood M, Patterson P, Juckel G, Heinz A, Morrison A, Lewis S, von Reventlow HG, Klosterkotter J (2010). Prediction of psychosis in adolescents and young adults at high risk: results from the Prospective European Prediction of Psychosis Study. Archives of General Psychiatry 67, 241–251. [DOI] [PubMed] [Google Scholar]
- Spencer C, Castle D, Michie PT (2002). Motivations that maintain substance use among individuals with psychotic disorders. Schizophrenia Bulletin 28, 233–247. [DOI] [PubMed] [Google Scholar]
- Stowkowy J, Addington J (2013). Predictors of a clinical high risk status among individuals with a family history of psychosis. Schizophrenia Research 147, 281–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson A, Nelson B, Yung A (2011). Predictive validity of clinical variables in the “at risk” for psychosis population: international comparison with results from the North American Prodrome Longitudinal Study. Schizophrenia Research 126, 51–57. [DOI] [PubMed] [Google Scholar]
- Thornton LK, Baker AL, Johnson MP, Kay-Lambkin F, Lewin TJ (2012). Reasons for substance use among people with psychotic disorders: method triangulation approach. Psychology of Addictive Behaviors 26, 279–288. [DOI] [PubMed] [Google Scholar]
- Wechsler D (1999). Wechsler Abbreviated Scale of Intelligence. The Psychological Corporation: San Antonio, TX. [Google Scholar]


