1. Introduction
As a result of COVID-19 pandemic, pulmonary rehabilitation (PR) programs were impeded for patients with non-COVID-19 conditions such as those with chronic respiratory diseases (CRD). Remote interventions are feasible and have demonstrated similar outcomes to traditional centre-based PR, mostly in chronic obstructive pulmonary disease (COPD) [1], [2]. We previously demonstrated the feasibility and effectiveness of face-to-face home-based PR in patients with CRD [3], [4], but due to the pandemic, we transitioned to an intervention combining face-to-face supervised home sessions and telehealthcare. We briefly report the feasibility, safety and effectiveness of this combined intervention conducted in France during the lockdown from March 17 to May 11, 2020.
2. Patients and methods
We retrospectively included all participants that were referred to the 8-week home-based PR program, without other specific criteria than those previously described [3], [4], [5]. Details regarding the ethical approval, informed consent of participants, and PR program can be found elsewhere [3], [4], [5]. The program included an initial educational needs assessment, performed at home or by telehealthcare after March 17, followed by a home visit to provide training equipment, supervise the first exercise session and perform the evaluations. During the lockdown, only two members of the PR team conducted home visits, using personal protective equipment, physical distancing and hand hygiene. After which, the program consisted of once- or twice-weekly structured telehealth calls to achieve 90 minutes of individually supervised intervention weekly. Participants were expected to perform a personalized action plan the rest of the week. Telehealth sessions were promoted through phone or video calls (WhatsApp® and Doctolib®) depending on the resources available to the patient.
Dyspnea (modified medical research council, mMRC), fatigue (fatigue assessment scale, FAS), anxiety and depressive symptoms (hospital anxiety and depression scale, HAD), health-related quality of life (visual-analogue scale (VAS) of the EQ-5D-3L questionnaire) and exercise tolerance (6-minute stepper test, 6MST) were assessed at the beginning (M0) and at the end of the intervention (M2).
Data were analysed with SAS V9.4 (SAS Institute, Cary NC, USA). The changes in study outcomes over time were analysed using paired Wilcoxon test and Bonferroni post hoc procedure.
3. Results
3.1. Feasibility
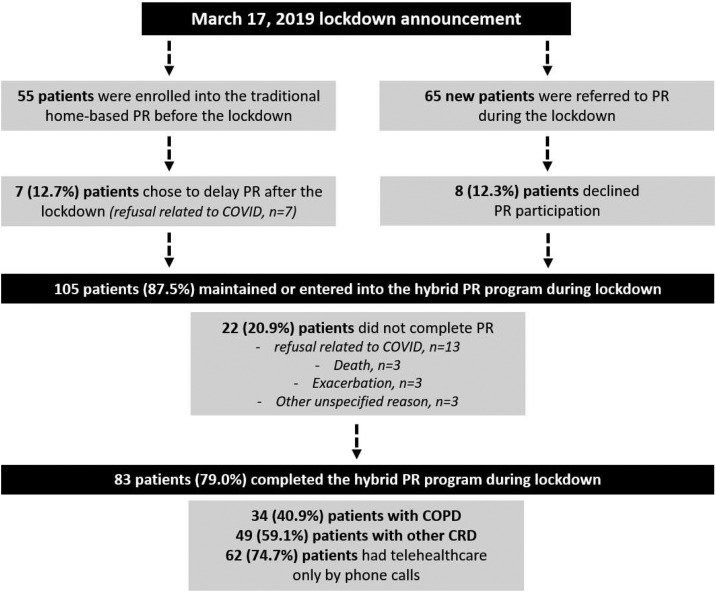
Before March 17, 55 patients were participating in the home-based intervention. Amongst them, 7 (12.7%) delayed the program after the lockdown. During the lockdown, 65 new patients were referred for PR. Amongst them, 8 (12.3%) patients refused to participate. Of the 105 patients managed during this period, 13 (12.4%) suspended the intervention after one visit, and 9 (8.6%) did not complete the program (13 refusal related to COVID-19 pandemic, three deaths, three exacerbations, three others causes) (Fig. 1 ). There was no significant difference between participants who delayed or suspended the intervention and those who completed PR (n = 83). Among these 83 participants, 62 received telehealthcare through phone calls and 21 through video calls. Twenty-seven participants did not performed the 6MST because they refused the home visit or team members were unavailable. All participants performed the others outcomes either by face-to-face home visits or telehealthcare.
Fig. 1.
Flow chart of the study participants.
3.2. Safety
No adverse events related to PR or positive COVID-19 cases in participants or team members were reported.
3.3. PR Effectiveness
The majority of the 83 included participants were 63 years old and men (55.4%), and included 34 COPD and 49 other CRD's (15 asthmatics, 9 idiopathic pulmonary fibrosis, 8 nonspecific interstitial lung disease, 7 obesity-hypoventilation syndrome and 10 others). At M2, the COPD group improved the VAS of the EQ-5D-3L questionnaire (P < 0.01), 6MST (P < 0.001) and mMRC (P < 0.05) scores, but not HAD and FAS scores (Table 1 ). The CRD's group showed improvements in all outcomes with the exception for mMRC.
Table 1.
Changes of the outcomes.
| Outcomes | COPD (n = 34) |
Other CRD's (n = 49) |
||||
|---|---|---|---|---|---|---|
| n | M2 | Δ | n | M2 | Δ | |
| mMRC, score (0–4) | 34 | 2.6 ± 1.2* | −0.3 ± 0.7 | 46 | 2.0 ± 1.4 | −0.1 ± 0.9 |
| HAD-Anxiety score (0–21) | 34 | 8.2 ± 4.9 | 0.5 ± 3.7 | 46 | 6.8 ± 4.7*** | −2.3 ± 3.7 |
| HAD-Depression, score (0–21) | 34 | 6.8 ± 4.6 | −0.2 ± 5.7 | 46 | 4.4 ± 3.5*** | −1.9 ± 3.3 |
| FAS, score (10–50) | 34 | 25.4 ± 9.3 | −0.4 ± 6.2 | 46 | 21.3 ± 6.9** | −2.7 ± 6.3 |
| VAS (EQ-5D-3L), score (0–100) | 32 | 59.8 ± 22** | 9.8 ± 17.2 | 43 | 66.0 ± 16.3*** | 4.8 ± 24.0 |
| 6MST, strokes | 12 | 409 ± 175*** | 101 ± 66 | 19 | 522 ± 123* | 40 ± 87 |
M0: baseline; M2: end of PR program; n: number of participants at M2; Δ: delta M2–M0; mMRC: modified medical research council dyspnea scale; HAD: hospital anxiety and depression scale; FAS: fatigue assessment scale; VAS: visual-analogue scale; 6MST: 6-minute stepper test; *: P < 0.05; **: P < 0.01; ***: P < 0.001, different from baseline. Data are presented as the mean ± SD.
4. Discussion
This brief report shows that 8 weeks of PR, combining supervised home visits and telehealthcare, was feasible, safe and effective for improving exercise tolerance, quality of life, anxiety, depression and fatigue score in patients with CRD. We also raised important points to consider: i) the majority of participants (74.7%) only had access to phone calls for telehealthcare; ii) the number of patients who stopped or declined PR after the first session (12.4%) was higher than a previous result (2.9%) [5], but the number of PR non-completers was similar (8.6% vs. 7.6%) [3]; iii) the pandemic prevented 32.5% of participants from having the physical assessments at home (6MST); iiii) PR was pursued by reducing the number of face-to-face visits and by following health recommendations.
The positive effects of home-based PR have been repeatedly confirmed in CRD's [1], [3], [4], [6] and telerehabilitation had shown promising results regarding its feasibility and short-term effectiveness [2], [7]. Using a mixed intervention, we confirmed our previous results, with the exception for patients with COPD whose anxiety, depression and fatigue scores were not reduced after PR. This result suggests that to improve psychological features, face-to-face visits are more important for people with COPD than for those with other CRD's. Moreover, 6MST results should be taken cautiously because of the small sample size at M2.
The retrospective nature of this study and the small sample size may limit the generalizability of the results. Moreover, the study was also limited by the number of home visits which differed between the participants during the lockdown, and by the absence of randomization regarding the tools used during telehealth sessions. That being said, the present report describes real-life PR designed to respond to emergencies caused by COVID-19 pandemic, and demonstrates that PR could have been pursued by combining home visits and telehealthcare, warranting replicating this finding using a randomized controlled trial. Furthermore, it is a fact that COVID-19 has contributed to sudden recognition for the need of telehealthcare including during PR. A dialogue needs to be open between PR professionals and health authorities on how remote intervention can be implemented and regulated as part of ongoing standard care.
Funding
Home-based PR were financially supported by Adair, Aeris Santé, Bastide, France Oxygène, Homeperf, LVL, Medopale, NorOx, Santélys, SOS Oxygène, Sysmed, VitalAire, and ARS Hauts-de-France. The funders played no role in the design, conduct or reporting of this study.
Author contribution
JMG and SG contributed to the study design, the recruitment of patients, the acquisition and analysis of the data, the interpretation of the results, and the redaction of the manuscript. OLR and CC contributed to the study design, the recruitment of patients, and the redaction of the manuscript. All authors approved the final version of the manuscript.
Disclosure of interest
JMG reports non-financial support unrelated to the submitted work from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKlein, Novartis, Vitalaire, and Roche. OLR reports personal fees and/or non-financial support from AstraZeneca, Boehringer Ingelheim, Chiesi, Lilly and Novartis, non-financial support from GlaxoSmithKline, Mayoli, MSD, Pfizer, PulmonX, Santelys association, Vertex, Vitalaire and Zambon, outside the submitted work. CC reports personal fees and non-financial support unrelated to the submitted work from ALK-Abello, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKlein, MEDA Pharma, Medexact, Novartis, Pierre Fabre, Pfizer, Roche, Sanofi, Santélys, and TEVA.
Acknowledgements
We thank the members of the rehabilitation team: Sophie Duriez, Mathieu Grosbois, Marjorie Lambinet, Gaelle Tywoniuk, Valentine Opsomer, Florence Urbain, and Virginie Wauquier.
References
- 1.Maltais F., Bourbeau J., Shapiro S., Lacasse Y., Perrault H., Baltzan M., et al. Chronic Obstructive Pulmonary Disease Axis of Respiratory Health Network FdresdQ Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2008;149:869–878. doi: 10.7326/0003-4819-149-12-200812160-00006. [DOI] [PubMed] [Google Scholar]
- 2.Hansen H., Bieler T., Beyer N., Kallemose T., Wilcke J.T., Ostergaard L.M., et al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: a randomised multicentre trial. Thorax. 2020;75:413–421. doi: 10.1136/thoraxjnl-2019-214246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grosbois J.M., Gicquello A., Langlois C., Le Rouzic O., Bart F., Wallaert B., et al. Long-term evaluation of home-based pulmonary rehabilitation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:2037–2044. doi: 10.2147/COPD.S90534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallaert B., Duthoit L., Drumez E., Behal H., Wemeau L., Chenivesse C., et al. Long-term evaluation of home-based pulmonary rehabilitation in patients with fibrotic idiopathic interstitial pneumonias. ERJ Open Res. 2019;5(2) doi: 10.1183/23120541.00045. [00045-2019. eCollection 2019 Apr] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gephine S., Le Rouzic O., Machuron F., Wallaert B., Chenivesse C., Saey D., et al. Long-term effectiveness of a home-based pulmonary rehabilitation in older people with chronic obstructive pulmonary disease: a retrospective study. Int J Chron Obstruct Pulmon Dis. 2020;15:2505–2514. doi: 10.2147/COPD.S268901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nolan C.M., Kaliaraju D., Jones S.E., Patel S., Barker R., Walsh J.A., et al. Home versus outpatient pulmonary rehabilitation in COPD: a propensity-matched cohort study. Thorax. 2019;74:996–998. doi: 10.1136/thoraxjnl-2018-212765. [DOI] [PubMed] [Google Scholar]
- 7.Knox L., Dunning M., Davies C.A., Mills-Bennet R., Sion T.W., Phipps K., et al. Safety, feasibility, and effectiveness of virtual pulmonary rehabilitation in the real world. Int J Chron Obstruct Pulmon Dis. 2019;14:775–780. doi: 10.2147/COPD.S193827. [DOI] [PMC free article] [PubMed] [Google Scholar]