Abstract
Objective:
To elucidate the positional and dimensional temporomandibular joint (TMJ) changes after correction of posterior crossbite in growing patients.
Materials and Methods:
A systematic unrestricted search was done in six databases until June 27, 2017. A manual search in the reference lists of the included studies and gray literature was also performed. The eligibility criteria included randomized controlled trials and prospective nonrandomized controlled clinical trials and a sample of growing subjects with posterior crossbite that required maxillary expansion. Risk of bias assessment was performed using Cochrane's Risk of Bias Tool. The literature search, study inclusion, risk of bias assessment, evaluation of quality of evidence (GRADE), and data extraction were performed by two reviewers independently.
Results:
Only two articles were finally eligible to be included in the qualitative analysis. Both studies were RCTs and were assessed as having unclear risk of bias. Meta-analysis was not possible since one study used cone-beam computed tomography as an assessment tool while the other used ultrasonography. One study reported significant reduction in the condylar positional difference between centric and habitual occlusion in the treatment group, while no spontaneous correction of condylar asymmetric position occurred in the control group. The other study reported minor changes of condylar position in both treatment and control groups.
Conclusions:
The current available data provide insufficient and weak evidence to form a solid and firm conclusion. There is poor, very low-quality evidence regarding the positional and dimensional effects of posterior crossbite correction on the TMJs.
Keywords: Systematic review, Maxillary expansion, Temporomandibular joint
INTRODUCTION
Posterior crossbite is one of the most frequent malocclusions encountered by orthodontists during the primary, mixed, and permanent dentition stages. Its prevalence in the primary and mixed dentition stages ranges from 7% and 23%.1–6 Posterior crossbite can be of skeletal or dental origin, either affecting one side, where it is called unilateral posterior crossbite, or affecting both sides, where it is called bilateral posterior crossbite. The classical literature suggests that posterior crossbite in children should be treated as early as possible to promote bilateral condylar symmetry and provide a favorable environment to allow normal growth and development to occur.7
If a functional posterior crossbite (FPXB) is left untreated, it can have deleterious effects on the development and function of the temporomandibular joints (TMJs). Skeletal remodeling of the TMJs can occur over time so that the condyles become more asymmetrically positioned in their fossae, and facial asymmetry and mandibular midline deviation toward the crossbite side might persist. Subsequent adaptation of the neuromusculature to the acquired mandibular position can cause asymmetric mandibular growth, facial disharmony, and severe skeletal crossbite in the permanent dentition. Some authors suggested that neither mandibular structure asymmetry nor condylar asymmetry would develop if a posterior crossbite was left untreated.8,9 Several studies documented that a more symmetrical condyle position was achieved after treating posterior crossbite.10,11 One other study reported minor changes of condylar position following posterior crossbite correction.12
The influence of untreated posterior crossbite on craniomandibular asymmetry varies from none to considerable. This considerable variation may be due to variation in study design, sample size, research approaches, and radiographic techniques used to investigate the condyle-fossa relationship, thus producing disparate outcomes among these investigations.
Mandibular and condylar asymmetries are believed to be a common feature of temporomandibular dysfunction (TMD).13 A recent study suggested a correlation between posterior crossbite with mandibular deviation and some signs and symptoms of TMD.14,15 However, the direct role of posterior crossbite as a contributing factor in TMD is still controversial.
Because spontaneous correction of posterior crossbite is rare, early treatment has been recommended.16–18 Maxillary expansion is the treatment choice for FPXB because it resolves the transverse maxillary deficiency and allows the mandible to regain a normal centric-intercuspal position. Several appliances are available for the correction of FPXB, such as rapid maxillary expanders (RMEs), slow maxillary expanders (SMEs), and semirapid expanders. Studies on the effects of posterior crossbite correction on the condyle are limited, and the question of whether posterior crossbite correction affects the condyle negatively or positively has still not received a clear answer. Therefore, the aim was to determine whether correction of posterior crossbite compared with nontreated crossbite results in actual changes of TMJs in growing patients.
MATERIALS AND METHODS
This systematic review was done following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement19 and Cochrane Handbook for Systematic Reviews of Interventions.20 The protocol was registered at the Evidence Based Center, Faculty of Dentistry, Cairo University. The steps of screening the articles according to the title and abstract and full text, extraction of data, and quality assessment were done independently by the first two authors. Any conflict between the two authors was resolved by the third author if they did not reach a decision after discussion.
Eligibility Criteria
Inclusion criteria.
Participants: growing patients with posterior crossbite
Intervention: slow or semirapid or rapid maxillary expansion
Control: growing patients with posterior crossbite receiving no treatment
Outcome: linear or angular TMJ measurements
Study design: randomized clinical trials (RCTs), quasi randomized clinical trials, and prospective controlled clinical trials (CCTs)
Exclusion criteria.
Studies of patients having cleft lip and/or palate or any craniofacial anomalies
Studies with no posterior crossbite control group
Studies including patients who had received previous orthodontic treatment or combined surgical and/or orthodontic treatment
Abstracts, letters to the editors, commentaries, laboratory studies, descriptive studies, individual case reports, series of cases, reviews, retrospective studies, and meta-analyses
Information Sources, Search Strategy, and Study Selection
The search was carried out using the following databases: PubMed, Cochrane Library, Ovid, Scopus, Web of Science, and Latin American and Caribbean Health Sciences Literature (LILACS) systematically and comprehensively until June 27, 2017, with no language restriction using a combination of keywords, MESH terms, and truncations that were adjusted for each database (Appendix 1). Citation tracking and searching of reference lists of the included studies was performed to identify relevant research. Egyptian Universities Libraries Consortium was searched for the gray literature, and the reference lists of the included studies were scanned for any eligible studies.
After the duplicate references were removed using references software (EndNote X7.1, Clarivate Analytics, Philadelphia, USA), the articles were screened based on the title and abstract according to the predefined eligibility criteria. If the abstract did not provide the information to judge whether to include the study or not, the full text was screened.
Data Items and Collection
A data extraction form was developed and included the following items: authors' name and country, year of publication, setting, study design, sample size, age and gender of the patients, device used, rate of expansion, activation duration, activation limit and consolidation period, crossbite type and side, outcome of interest, time of measurements, and measuring instruments.
Risk of Bias in Individual Studies
The Cochrane Risk of Bias Tool20 was used to assess the risk of bias (RoB) in the included RCTs. An overall unclear/high RoB was given to the study when at least one domain from the seven domains was judged as unclear/high RoB.
Quality of the Evidence
The quality of evidence was evaluated according to the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.21 The GRADE approach appraises the quality of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. The GRADE profiler was used to summarize the quality of evidence using the GRADE pro GDT software (http://gdt.guidelinedevelopment.org). This assessment was based on certain considerations, including study design, RoB, consistency, directness, heterogeneity, precision, publication bias, and other aspects reported by studies included in the systematic review. Depending on the seriousness, the quality of the evidence can be downgraded by one or two levels for each aspect.
RESULTS
Study Selection
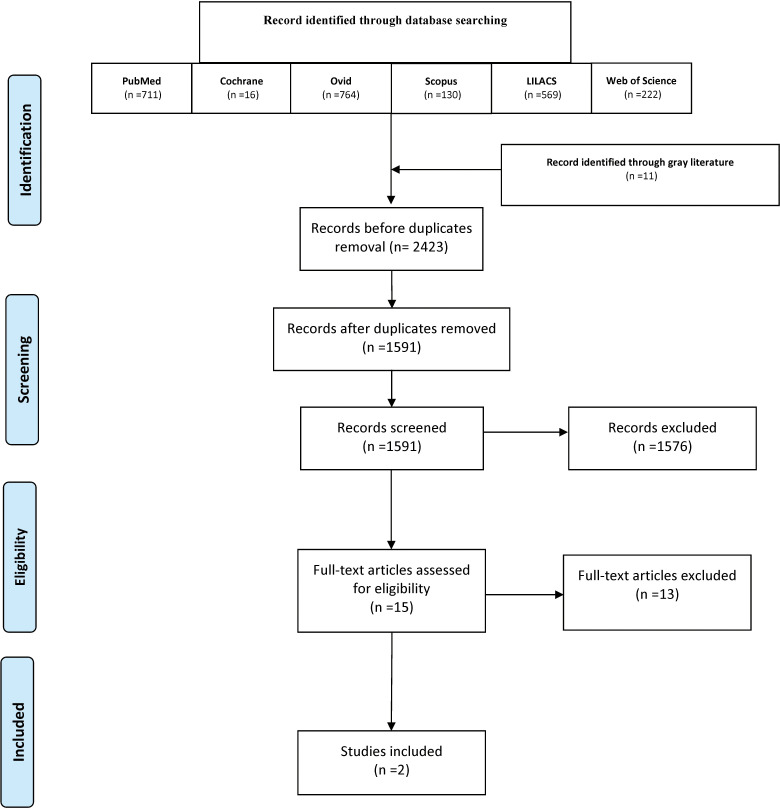
The electronic and manual search initially identified 2423 relevant records. After removal of duplicate citations, a total of 1591 articles were screened by reading titles and abstracts, and 1576 studies were excluded. Subsequently, the remaining 15 studies were read in full text for eligibility assessment according to the inclusion criteria. The excluded studies7,10,22–32 and reasons for their exclusion are summarized in Table 1. Finally, two studies were included in this review: Lippold et al. (2008)11 and McLeod et al. (2016).12 The details of studies' inclusion are shown in the PRISMA flow diagram (Figure 1).
Table 1.
Articles Excluded After Full-Text Evaluation Based on Eligibility Criteria
| Reference |
Reason for Exclusion |
| Myers et al.7 | No control group |
| Kecik et al.10 | No untreated control group |
| Hesse et al.22 | No control group |
| de Boer and Steenks23 | No joint measurements |
| Martin et al.24 | No joint measurements |
| Arat et al.25 | No control group |
| Costa et al.26 | No control group |
| Matta et al.27 | No control group |
| Masi et al.28 | No control group |
| Lagravere et al.29 | No joint measurements |
| Leonardi et al.30 | No untreated control group |
| Venancio et al.31 | No joint measurements |
| Melgaco et al.32 | No crossbite in the treatment group |
Figure 1.
PRISMA flow diagram summarizing the literature search.
Study Characteristics
Both included studies were prospective RCTs and conducted in university settings. Both studies reported the age for the two groups separately, and the samples in both studies consisted of males and females. RME using the hyrax appliance was used in both studies. The outcomes of interest were measured using cone-beam computed tomography (CBCT) in one study12 and ultrasound in the other.11 Table 2 summarizes the characteristics of the included studies.
Table 2.
Summary Table of Characteristics of the Included Studiesa
| Author, Year, Country, Setting |
Study Design |
Sample Size, Gender |
Age, y |
Device Used, Rate of Expansion |
| Lippold et al., 2008,11 Germany, Westphalian Wilhelm University | RCT | I: 31, 13 boys 18 girls | I: 6.9 ± 2.2 | Bonded palatal expansion appliance + U-bow activator of type I, 0.2 mm/d |
| C: 35, 17 boys 18 girls | C: 6.9±2 | |||
| McLeod et al., 2016,12 Canada, University of Alberta | RCT | I: 19, Unclear | I: 14 ± 1 | Hyrax (RME), 0.25 mm per turn (0.5 mm/d) |
| C:18, Unclear | C: 13 ± 1 |
C indicates comparator; CBCT, cone-beam computed tomography; I, intervention; RCT, randomized controlled trial; UPFXP, unilateral posterior functional crossbite.
Table 2.
Extended
| Activation Duration |
Activation Limit, Consolidation Period |
Crossbite Side, Crossbite Inclusion Criteria |
Outcome |
Time of Measurements, Measuring Instrument |
| 2 or 3 wk | Until 2-mm overcorrection, the appliance was left in place for 16 wk | UPFXP in late deciduous and early mixed dentition | Condylar deviation | Ultrasound at the beginning (T1) and after 12 mo of treatment (T2) |
| Unclear | 20% overcorrection, the appliance was left in place for 6 mo | Unclear (patients with maxillary transverse deficiency) | Condylar position | CBCT at initial treatment (T1) and 6 mo later (T2) |
RoB Within the Included Studies
This review included two RCTs. According to the Cochrane Risk of Bias Tool, both studies were judged as having low RoB for random-sequence generation and blinding of participants and personnel. Regarding allocation concealment and blinding of outcome assessment domains, both studies were judged as having unclear RoB, as it was not mentioned whether allocation concealment and blinding of outcome assessors were done or not. For incomplete outcome data domain, the Lippold et al. (2008)11 study was judged as having low RoB, while it was judged as unclear for the other study12 because of the imbalance in numbers of patients who were recruited from another clinical research project29 without giving any reasons for this imbalance and attrition. Both studies were judged as having unclear RoB regarding selective reporting domain as study protocols were not available to identify any other unreported outcome. Sample size was not calculated in the McLeod et al. (2016)12 study, whereas no standard deviations, confidence intervals, or exact P values were mentioned in the Lippold et al. (2008)11 study. Therefore, both studies were considered as having unclear RoB in other bias domains. Eventually, both studies were judged to have an overall unclear RoB. The details of RoB assessment are summarized in Figure 2 and Appendix 2.
Figure 2.
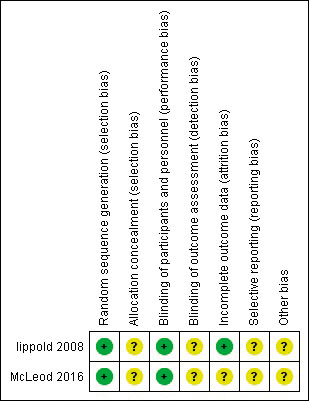
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Effect of Interventions
Because of the great amount of heterogeneity in the measuring devices, the methods of outcomes measurement, and the follow-up duration, it was not possible to combine the data for meta-analysis. One study11 reported a non–statistically significant reduction in the condylar positional difference between centric and habitual occlusion at T1 and T2 in the control group in all three spatial planes on the crossbite and non-crossbite sides while there was a statistically significant reduction in the treatment group. The other study12 reported that changes in the condyle position were minor in both groups (<1.9 mm average for both groups). The largest difference in both groups was found when measuring the distance between the left and right condylar heads. When comparing changes between both groups, no statistically significant difference was found between changes in the condyles. Of all condylar measurements studied, only two measurements showed statistically significant differences between the control and treatment groups: the distance from left posterior condylar pole to midpoint on a line connecting right and left foramen spinosum (ELSA), and the distance from left posterior condylar pole to the foramen magnum. Long-term results were not reported in any study reviewed.
Quality of the Evidence
Overall, the evidence for the outcomes evaluated by the GRADE system was assessed as very low quality, suggesting very little confidence in the effect estimate. The true effect was likely to be substantially different from the estimate of effect. The reasons for this judgment are outlined in Table 3.
Table 3.
GRADE of Evidence: Does Posterior Crossbite Correction Compared With Untreated Posterior Crossbite Control Result in Temporomandibular Joint Changes?
| No. of Participants (Studies) |
Risk of Bias |
Inconsistency |
Indirectness |
Imprecision |
Publication Bias |
Overall Certainty of Evidence |
Comments |
| Changes of condylar position | |||||||
| 79 (2 RCTs) | Seriousa | Very seriousb | Seriousc | Very seriousd | Publication bias strongly suspectede | ⊕○○○ | |
| VERY LOW | |||||||
| Changes of condylar dimensions | |||||||
| 0 (0 studies) | — | No study: there were no published data that fulfilled the inclusion criteria for the question asked | |||||
| Changes of glenoid fossa position | |||||||
| 0 (0 studies) | — | No study: there were no published data that fulfilled the inclusion criteria for the question asked | |||||
| Changes of joint spaces | |||||||
| 37 (1 RCT) | Seriousf | Not serious | Not serious | Seriousg | Publication bias strongly suspectede | ⊕○○○ | |
| VERY LOW | |||||||
GRADE Working Group grades of evidence
High certainty: We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect.
Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect
The evidence was downgraded by one level because of serious concern regarding the risk of bias; both studies have unclear risk of bias.
The evidence was downgraded by two levels because of high degree of heterogeneity in the methodology and high degree of inconsistency in the results.
The evidence was downgraded by one level because one study used ultrasound, which was not the most informative way of measuring effects of the interventions (could not determine the direction of condylar deviation).
The evidence was downgraded by two levels because of lack of confidence intervals and standard deviations in results of one study and large standard deviations in results of the other study. Also, the results of both studies come from small number of participants.
The evidence was downgraded by one level because the results come from small studies and small number of participants.
The evidence was downgraded by one level because of serious concern regarding the risk of bias; the study has unclear risk of bias.
The evidence was downgraded by one level because the results come from small number of participants and have large standard deviations.
DISCUSSION
Although many studies7,10,11,22 recommended maxillary expansion to correct posterior crossbite to place the condyles in a more symmetrical position to avoid true asymmetry of the TMJs in the future, other authors12,30 thought that there was no correlation between posterior crossbite correction and condylar position. Moreover, some authors7,33,34 thought that correction of posterior crossbite using SME was superior to RME in placing the condyles in a more symmetrical position. This assumption does not rely on strong evidence as no evidence exists denoting that one type of expansion is superior to the others regarding its effect on TMJs, improving condylar position, and providing a good environment for proper growth of the TMJ to avoid any mandibular and condylar asymmetry.
RCTs, along with meta-analyses, are considered to be at the top of the hierarchy of research design and are followed by CCTs. In this review, only RCTs and prospective CCTs were included because poorly designed trials may give misleading results. Large amounts of data obtained from a poorly designed study cannot compensate for its poor design; also, combining poor-quality studies with the more rigorously conducted ones may not be useful and can result in misleading estimates of the underlying true effect. This review included only studies with control groups consisting of untreated growing patients with posterior crossbite. The control group consisted of patients exhibiting the same baseline characteristics as the experimental groups, except for the variable applied to the latter.35 This has the advantage of eliminating and isolating confounding variables and bias and ruling out imagined or random effects of the treatment. Control groups with normal occlusion were considered invalid because they did not share baseline characteristics with treatment groups; therefore, all studies that included patients without posterior crossbite as a control group were excluded. Inclusion of an untreated control group ensures that the effect on the TMJs, if any, was only the result of treatment and excludes the effect of growth. These studies dealt with growing patients and made sure that no TMJ changes occurred spontaneously.
Although a comprehensive literature search was conducted, a shortage of high-quality clinical trials was evident. The two included studies were assessed as having unclear RoB. Because of methodological heterogeneity and the noncomparability of original data of the included studies, performing a meta-analysis was not possible. Lippold et al. (2008)11 used ultrasound to determine condylar differences between centric and habitual occlusion before and after maxillary expansion. They noted statistically significant differences between the control and treatment groups after expansion. The treated patients exhibited a distinct improvement manifested as significant reduction in the differences between centric and habitual occlusion. On the other hand, no significant changes were observed in the control group.
McLeod et al. (2016)12 evaluated condylar positions three-dimensionally before and after maxillary expansion using CBCT. They noted that most condylar positional changes were not significant between treatment and control groups. There were only two measurements that differed significantly between the treatment and control groups: left posterior condylar pole-foramen magnum distance (mean difference = 1.6 mm) and left posterior condylar pole-ELSA (mean difference = 0.82 mm).
Although there were minor TMJ changes in both of the reviewed studies, which were statistically significant for some measurements, these changes may have little impact clinically, especially considering that there was an absence of correlation between these positional TMJ changes and any TMJ clinical signs. Moreover, these changes were evaluated shortly after correction of posterior crossbite and may have been a temporary effect as there was no long-term follow-up.
The validity of the technique used for assessment and outcome measurements is crucial as it can greatly affect the findings observed. As suggested by a recent review,36 CBCT is now considered as the most diagnostic, informative, and accurate method for evaluating the hard tissue components of the TMJ, and although McLeod et al. (2016)12 used three-dimensional (3D) CBCT imaging, their findings were analyzed using 2D measurements. More accurate results would have been achieved if 3D evaluation of the condyle and the joint spaces were used. To the contrary, Lippold et al. (2008)11 used ultrasonography, which is not the most informative method of measuring the outcome, and that is why the authors were not able to determine the direction of condylar deviation. To overcome these methodological problems in future research, CBCT should be used together with 3D measurements of the TMJ. A comprehensive 3D CBCT analysis of the TMJ developed by Alhammadi et al. (2015)37 could be used to standardize the analysis and measurements used in evaluating TMJ changes. This analysis provides descriptive measurements for condylar position in the three orthogonal planes and can be used also for assessment of joint spaces and condylar symmetry. When studies with a standardized technique and evaluation method become available, their results can be combined in a meta-analysis to increase power and improve estimates of the size of the effect.
Quality of the Evidence
Using the GRADE tool, the overall certainty of the evidence was assessed to be very low for condylar position and joint space outcomes for which data were available. In addition to publication bias, the two included trials had an unclear RoB and serious/very serious concerns regarding the directness, consistency, and precision of results. There were sparse data for condylar position outcome, indicating very little confidence in the effect estimate and suggesting that further trials are needed. For the other outcomes, there were no published data that fulfilled the inclusion criteria for the question asked.
The present systematic review highlighted the knowledge gap in the available literature with respect to the effect of correcting posterior crossbite on the TMJ. Also, this review pinpointed the weaknesses of the very limited available evidence. These weaknesses should be taken into consideration in any future clinical research.
CONCLUSIONS
There is a very-low-quality evidence regarding the positional and dimensional effects of posterior crossbite correction by maxillary expansion on the TMJs.
There is no evidence available regarding the long-term effect of posterior crossbite correction on the TMJs.
In the available literature, there is an absence of well-designed RCTs that could answer the current systematic review question.
Clinical Implications
Although there is a rationale for early correction of posterior crossbites, early posterior crossbite correction cannot be recommended only on the basis of aiming to improve condylar position and preventing TMD because of conflicting results and limited and very low quality of the available evidence.
Recommendations for Future Research
High-quality RCTs investigating the short- and long-term effects of correcting posterior crossbite on the TMJs, using standardized techniques and evaluation methods, are required to address whether these changes are of clinical importance and if the treatment permanently changes the TMJs or if the changes are only temporary.
APPENDIX 1.
Search Terms Specific for Each Database and Truncations
| Electronic Database |
Search Strategy Used |
Items found |
| PubMed | ((((((((((((correct*) OR treatment)) AND ((((posterior) OR molar) OR bicuspid) OR premolar)) AND ((cross*bite) OR cross?bite))) OR ((((maxill* AND expan*) OR palat* AND expan* OR “Palatal Expansion Technique"[Mesh]))))) AND (((((((((((tmj) OR tmd) OR temporomandibular) OR temporo?mandibular) OR temporo*mandibular) OR “Temporomandibular Joint"[Mesh]) OR “Temporomandibular Joint Dysfunction Syndrome"[Mesh]) OR “Temporomandibular Joint Disc"[Mesh] OR condyl*) OR articular fossa) OR glenoid fossa) OR disc)) | 711 |
| Cochrane Central Register of Controlled Trials | (((TMJ OR TMD OR temporomandibular OR temporo*mandibular OR Temporo?mandibular OR condyl* OR condyl? OR disc OR glenoid fossa OR articular fossa:ti,ab,kw))) AND (((Maxill? expan? OR maxill* expan* OR palat? expan? OR palat* expan*) OR ((crossbite OR cross?bite OR cross*bite) AND (correct OR correct? OR correct* OR treatment))) | 16 |
| Web of Science | TS=(Temporomandibular) OR TS=(Temporo-mandibular) OR TS=(Temporo?mandibular) OR TS=(Temporo*mandibular) OR TS=(Temporomandibular joint dysfunction) OR TS=(tmd) OR TS=(Condyl?) OR TS=(Condyl*) OR TS=(Disc) OR TS=(Articular fossa) OR TS=(Glenoid fossa) AND TS=(maxilla* expan*) OR TS=(Palat* expan*) OR TS=(cross*bite corre*) OR TS=(cross*bite treatment) | 222 |
| Scopus | ( ( maxill* AND expan* OR maxill? AND expan? OR palat* AND expan* OR palat? AND expan? ) OR ( ( correct* OR correct? OR treatment ) AND ( cross*bite OR cross?bite ) ) ) AND ( tmj OR tmd OR temporomandibular OR temporo?mandibular OR temporo*mandibular OR condyle OR condyle OR condyl* OR articular AND fossa OR glenoid AND fossa OR disc ) | 130 |
| Ovid | (maxill* expan* or maxill? expan? or palat* expan* or palat? expan?).af. OR ((cross*bite or cross?bite).af. AND (correct* or correct? or treatment).af.) AND (Tmj or TMD or temporo*mandibular or temporo?mandibular or condyl* or Condyl? or glenoid fossa or articular fossa or disc or temporomandibular).af. | 764 |
| LILACS | (tw:(maxill$ expanr$ OR palat$ expan$)) AND (tw:(Tmj OR temporomandibular OR temporo$mandibular OR condyl$ OR glenoid fossa OR articular fossa OR disc OR tmd)) | 569 |
APPENDIX 2.
Assessment of Risk of Bias (RoB) for the Included RCTs
| Study |
Random-Sequence Generation (Selection Bias) |
Allocation Concealment (Selection Bias) |
Blinding of Participants and Personnel (Performance Bias) |
| Lippold et al. 200811 | Low = block randomization | Unclear = no mention of the allocation concealment | Low = blinding will not affect the outcome |
| Mcleod et al. 201612 | Low = random numbers generated list | Unclear = no mention of the allocation concealment | Low = blinding will not affect the outcome |
APPENDIX 2 Extended.
Assessment of Risk of Bias (RoB) for the Included RCTs
| Blinding of Outcome Assessment (Detection Bias) |
Incomplete Outcome Data (Attrition Bias) |
Selective Reporting (Reporting Bias) |
Other Bias |
Overall Risk of Bias |
| Unclear = no mention of blinding of the outcome assessors | Low | Unclear = no mention of study protocol | Unclear = no standard deviation, no exact P value, and no confidence interval | Unclear |
| Unclear = no mention of blinding of the outcome assessors | Unclear = imbalance in patient numbers included | Unclear = no mention of study protocol | Unclear = no sample size calculation | Unclear |
REFERENCES
- 1.Bjork A, Krebs A, Solow B. A method for epidemiological registration of malocclusion. Acta Odontol Scand. 1964;22:27–41. doi: 10.3109/00016356408993963. [DOI] [PubMed] [Google Scholar]
- 2.Day AJ, Foster TD. An investigation into the prevalence of molar crossbite and some associated aetiological conditions. Dent Pract Dent Rec. 1971;21(11):402–410. [PubMed] [Google Scholar]
- 3.da Silva Filho OG, Santamaria M, Jr, Capelozza Filho L. Epidemiology of posterior crossbite in the primary dentition. J Clin Pediatr Dent. 2007;32(1):73–78. doi: 10.17796/jcpd.32.1.h53g027713432102. [DOI] [PubMed] [Google Scholar]
- 4.Shalish M, Gal A, Brin I, Zini A, Ben-Bassat Y. Prevalence of dental features that indicate a need for early orthodontic treatment. Eur J Orthod. 2013;35(4):454–459. doi: 10.1093/ejo/cjs011. [DOI] [PubMed] [Google Scholar]
- 5.de Sousa RV, Ribeiro GL, Firmino RT, Martins CC, Granville-Garcia AF, Paiva SM. Prevalence and associated factors for the development of anterior open bite and posterior crossbite in the primary dentition. Braz Dent J. 2014;25(4):336–342. doi: 10.1590/0103-6440201300003. [DOI] [PubMed] [Google Scholar]
- 6.Gungor K, Taner L, Kaygisiz E. Prevalence of posterior crossbite for orthodontic treatment timing. J Clin Pediatr Dent. 2016;40(5):422–424. doi: 10.17796/1053-4628-40.5.422. [DOI] [PubMed] [Google Scholar]
- 7.Myers DR, Barenie JT, Bell RA, Williamson EH. Condylar position in children with functional posterior crossbites: before and after crossbite correction. Pediatr Dent. 1980;2(3):190–194. [PubMed] [Google Scholar]
- 8.Uysal T, Sisman Y, Kurt G, Ramoglu SI. Condylar and ramal vertical asymmetry in unilateral and bilateral posterior crossbite patients and a normal occlusion sample. Am J Orthod Dentofacial Orthop. 2009;136(1):37–43. doi: 10.1016/j.ajodo.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Veli I, Uysal T, Ozer T, Ucar FI, Eruz M. Mandibular asymmetry in unilateral and bilateral posterior crossbite patients using cone-beam computed tomography. Angle Orthod. 2011;81(6):966–974. doi: 10.2319/022011-122.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kecik D, Kocadereli I, Saatci I. Evaluation of the treatment changes of functional posterior crossbite in the mixed dentition. Am J Orthod Dentofacial Orthop. 2007;131(2):202–215. doi: 10.1016/j.ajodo.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 11.Lippold C, Hoppe G, Moiseenko T, Ehmer U, Danesh G. Analysis of condylar differences in functional unilateral posterior crossbite during early treatment—a randomized clinical study. J Orofac Orthop. 2008;69(4):283–296. doi: 10.1007/s00056-008-0803-9. [DOI] [PubMed] [Google Scholar]
- 12.McLeod L, Hernandez IA, Heo G, Lagravere MO. Condylar positional changes in rapid maxillary expansion assessed with cone-beam computer tomography. Int Orthod. 2016;14:342–356. doi: 10.1016/j.ortho.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Yanez-Vico RM, Iglesias-Linares A, Torres-Lagares D, Gutierrez-Perez JL, Solano-Reina E. Association between condylar asymmetry and temporomandibular disorders using 3D-CT. Med Oral Patol Oral Cir Bucal. 2012;17(5):e852–e858. doi: 10.4317/medoral.17786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thilander B, Bjerklin K. Posterior crossbite and temporomandibular disorders (TMDs): need for orthodontic treatment? Eur J Orthod. 2012;34(6):667–673. doi: 10.1093/ejo/cjr095. [DOI] [PubMed] [Google Scholar]
- 15.Jussila P, Krooks L, Napankangas R, et al. The role of occlusion in temporomandibular disorders (TMD) in the Northern Finland Birth Cohort (NFBC) 1966. Cranio. 2018. pp. 1–7. [DOI] [PubMed]
- 16.Thilander B, Wahlund S, Lennartsson B. The effect of early interceptive treatment in children with posterior crossbite. Eur J Orthod. 1984;6(1):25–34. doi: 10.1093/ejo/6.1.25. [DOI] [PubMed] [Google Scholar]
- 17.Schroder U, Schroder I. Early treatment of unilateral posterior crossbite in children with bilaterally contracted maxillae. Eur J Orthod. 1984;6(1):65–69. doi: 10.1093/ejo/6.1.65. [DOI] [PubMed] [Google Scholar]
- 18.Lindner A. Longitudinal study on the effect of early interceptive treatment in 4-year-old children with unilateral crossbite. Scand J Dent Res. 1989;97(5):432–438. doi: 10.1111/j.1600-0722.1989.tb01457.x. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. London: The Cochrane Collaboration;; 2011. [Google Scholar]
- 21.Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for Grading the Quality of Evidence and the Strength of Recommendations using the GRADE Approach. GRADE Working Group; 2013. [Google Scholar]
- 22.Hesse KL, Artun J, Joondeph DR, Kennedy DB. Changes in condylar position and occlusion associated with maxillary expansion for correction of functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1997;111(4):410–418. doi: 10.1016/s0889-5406(97)80023-6. [DOI] [PubMed] [Google Scholar]
- 23.de Boer M, Steenks MH. Functional unilateral posterior crossbite: orthodontic and functional aspects. J Oral Rehabil. 1997;24(8):614–623. doi: 10.1046/j.1365-2842.1997.00633.x. [DOI] [PubMed] [Google Scholar]
- 24.Martin C, Alarcon JA, Palma JC. Kinesiographic study of the mandible in young patients with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2000;118(5):541–548. doi: 10.1067/mod.2000.109494. [DOI] [PubMed] [Google Scholar]
- 25.Arat FE, Arat ZM, Tompson B, Tanju S. Muscular and condylar response to rapid maxillary expansion. Part 3: magnetic resonance assessment of condyle-disc relationship. Am J Orthod Dentofacial Orthop. 2008;133(6):830–836. doi: 10.1016/j.ajodo.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 26.TDd Costa, Carneiro MSA, Capelli Júnior J. Avaliação tomográfica da posição condilar em pacientes portadores de mordida cruzada posterior unilateral funcional. Revista Dental Press de Ortodontia e Ortopedia Facial. 2009;14:75–82. [Google Scholar]
- 27.ENRd Matta, Souza MMGd, Sant'Anna EFd, Silva SCd. Avaliação por tomografia computadorizada helicoidal dos efeitos da expansão rápida da maxila no posicionamento condilar em pacientes com mordida cruzada posterior funcional. Revista Dental Press de Ortodontia e Ortopedia Facial. 2009;14:40e41–40e49. [Google Scholar]
- 28.Masi M, Lederman HM, Yamashita HK, de Arruda Aidar LA. Temporomandibular joint evaluation with magnetic resonance imaging in children with functional unilateral posterior crossbite, treated with rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2009;136(2):207–217. doi: 10.1016/j.ajodo.2007.10.048. [DOI] [PubMed] [Google Scholar]
- 29.Lagravere MO, Carey J, Heo G, Toogood RW, Major PW. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2010;137(3):304. doi: 10.1016/j.ajodo.2009.09.016. e301–312. [DOI] [PubMed] [Google Scholar]
- 30.Leonardi R, Caltabiano M, Cavallini C, et al. Condyle fossa relationship associated with functional posterior crossbite, before and after rapid maxillary expansion. Angle Orthod. 2012;82(6):1040–1046. doi: 10.2319/112211-725.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Venancio F, Alarcon JA, Lenguas L, Kassem M, Martin C. Mandibular kinematic changes after unilateral crossbite with lateral shift correction. J Oral Rehabil. 2014;41(10):723–729. doi: 10.1111/joor.12199. [DOI] [PubMed] [Google Scholar]
- 32.Melgaco CA, Columbano Neto J, Jurach EM, Nojima Mda C, Nojima LI. Immediate changes in condylar position after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2014;145(6):771–779. doi: 10.1016/j.ajodo.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 33.Bell RA. A review of maxillary expansion in relation to rate of expansion and patient's age. Am J Orthod. 1982;81(1):32–37. doi: 10.1016/0002-9416(82)90285-8. [DOI] [PubMed] [Google Scholar]
- 34.Bell RA, Kiebach TJ. Posterior crossbites in children: developmental-based diagnosis and implications to normative growth patterns. Semin Orthod. 2014;20(2):77–113. [Google Scholar]
- 35.Kinser PA, Robins JL. Control group design: enhancing rigor in research of mind-body therapies for depression. Evid Based Complement Alternat Med. 2013;2013:140467. doi: 10.1155/2013/140467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44(1):20140235. doi: 10.1259/dmfr.20140235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alhammadi MS, Fayed MS, Labib AH. Comprehensive Three Dimensional CBCT Analyses of the TM Joint. Saarbrücken, Germany: Lambert Academic Publishing;; 2015. [Google Scholar]