Abstract
Objectives:
To conduct a pilot study to determine if the presence of obstructive sleep apnea (OSA) influences the orthodontic treatment outcome of Class II hyperdivergent patients receiving comprehensive orthodontic treatment.
Materials and Methods:
Patients between the ages of 12 and 14 who received orthodontic treatment at the Hospital of Stomatology, Wuhan University, China, were included in this study. Patients were divided into two groups: the OSA group and the control group, based on the outcome of pretreatment polysomnography findings and lateral cephalometric radiograph examination. Patients in the control group were matched with the OSA group for age, sex, ethnicity, weight, and height. Cephalometric measurements were used to record the skeletal and dental changes from before to after treatment. Data were analyzed using the t-test.
Results:
Twenty three OSA patients and 23 control patients were included. After comprehensive orthodontic treatment, the mandibular plane angle (SN-GoMe), articular angle (SArGo), sum of Jarabak angles (SUM) and the lower gonial angle (NGoMe) were found to increase significantly in the OSA group but remained unchanged or decreased slightly in the control group (P < .05). In the non-OSA group, the growth pattern became more horizontal. In contrast, in the OSA group the growth pattern became more vertical. Otherwise, similar treatment results were obtained for both groups in terms of sagittal change and occlusion.
Conclusions:
The presence of OSA in pediatric patients has a deleterious effect on the development of hyperdivergent malocclusions. Early diagnosis and management of pediatric OSA can affect the orthodontic treatment outcome of these patients.
Keywords: Pediatric OSA, Malocclusion, Orthodontic treatment
INTRODUCTION
Sleep-disordered breathing (SDB) is characterized by prolonged increased upper airway resistance, partial upper airway obstruction, or complete obstruction that disrupts pulmonary ventilation, oxygenation, or sleep quality. Obstructive sleep apnea hypopnea syndrome (OSAHS) was first reported in children by Guilleminault et al. in 1976.1 Since then, the influence of pediatric SDB on dentofacial growth and development has been a widely debated and controversial issue within the orthodontic community for decades.2–5 The size of the adenoids and nasopharyngeal space are major factors that determine nasopharyngeal obstruction. The presence of OSAHS in children is mainly caused by hypertrophy of the adenoids and tonsils. Children suffering from OSAHS have different dentofacial morphology to nonobstructed children during growth, thus resulting in unfavorable craniofacial dentofacial complex development.6–8
Along with the vast amount of research including animal experiments and literature reviews concerning airway and its influence on dentofacial growth and development,9–12 many investigators have attempted to resolve pediatric OSAHS by the use of orthodontic appliances such as rapid maxillary expansion appliances.13–17 However, few studies reported on the follow-up observation on the impact of OSAHS on patients treated with fixed orthodontic appliances.
Tonsillectomy and adenoidectomy (T & A) is the most commonly performed procedure to resolve OSAHS problems in children and is deemed curative in approximately 83% of children.18 Several investigators suggested an association between adenoidectomy and the change in mode of breathing and the establishment of a more horizontally growing mandible.7,19–22 The objective of the present study was to determine if the presence of obstructive sleep apnea (OSA) influences the orthodontic treatment outcome of patients with Class II hyperdivergent malocclusions.
MATERIALS AND METHODS
Sample Description
Patients between the ages of 12 and 14 who received orthodontic treatment at the Department of Orthodontics, School of Stomatology, Wuhan University, China, from 2012 to 2016 were selected for this study. The study was approved by the Ethics Committee of the School of Stomatology, Wuhan University (Approval 2016-51). The inclusion criteria were subjects with full permanent dentition and no missing teeth (except for third molars); distal molar relationship with ANB ≥ 4; hyperdivergent skeletal growth pattern (SNGoMe ≥ 36); degree of crowding < 3 mm. The exclusion criteria were obese subjects (BMI > 25kg/m2); failure to thrive; or temporomandibular joint problems.
Subjects were divided into an OSAHS group and control group based on polysomnography (PSG) findings and lateral cephalometric radiograph examination before orthodontic treatment. Subjects with apnea/hypopnea index (AHI) ≥ 1/h and enlarged adenoids with adenoid to nasopharynx ratio (A/N) > 0.6 were categorized into the OSAHA group. Subjects with AHI < 1/h and no enlarged adenoids were placed in the control group. All subjects were treated by the same orthodontist using an identical comprehensive treatment protocol, which included the extraction of the upper first premolars and the lower second premolars, as well as the use of a transpalatal arch/Nance holding arch as an anchorage reinforcement device.
Cephalometric Analysis
All lateral cephalometric radiographs were obtained with the same cephalostat (Soredex, Tuusula, Finland) according to a standard protocol (73 kV, 10 mA) and performed by the same operator. All radiographs were taken in centric occlusion and natural head position.23,24 Dolphin Imaging software (Version 11.7, Dolphin Imaging & Management Systems, Chatsworth, Calif) was used to digitize and analyze the pretreatment (T0) and posttreatment (T1) data. All data were measured again four weeks later to determine the error measurements. The reference points and lines used in the cephalometric analysis are shown in Table 1 and Figure 1. The cephalometric variables that were used in this study are shown in Table 2. Even though the radiographic image was only two-dimensional, a high correlation was found between nasopharyngeal airway and the size of the adenoids with the results of posterior rhinoscopy as adenoids lie on the posterior wall of the nasopharynx. An adenoid ratio (A/N) > 0.6 represented hypertrophy of the adenoids (Figure 2).
Table 1.
Cephalometric Landmarks Used in the Analysis of the Children in the Study
| Landmarks |
Definition |
| N |
Most Posterior Point on the Curve at the Bridge of the Nose |
| S | Midpoint of the sella turcica |
| Ba | Most inferior-posterior point on margin of the foramen magnum |
| Ar | Point of intersection of the inferior cranial base surface and the averaged posterior surfaces of the mandibular condyles |
| Go | Most posterior-inferior point on the outline of the mandible angle |
| Po | Most superior point of the outline of the external auditory meatus. |
| Or | Deepest point on the infra-orbital margin |
| Me | Most inferior point on the outer inferior margin of the mandible |
| Gn | Most anterior-inferior point on the outline of the bony chin |
| Pog | Most anterior point on the contour of the bony chin |
| DC | Center of the mandibular condyle lying on the line N-Ba |
| ANS | Anterior tip of the median palate |
| PNS | Most posterior point on the bony hard palate |
| Pt | Posterior outline of the Pterygo-Maxillary Fissure |
| A | Most posterior point on the anterior contour of the upper alveolar process |
| B | Most posterior point on the anterior contour of the lower alveolar process |
| PM | Point on the anterior border of the symphysis between point B and Po where the curvature changes from concave to convex |
| D | Center point of a circle |
| R1 | Point at the deepest notch of front margin of the mandibular ramus |
| R2 | Point in the center of the back margin of the mandibular ramus |
| R3 | Most inferior point in the sigmoid notch |
| R4 | Point on the lower border of the mandible directly inferior to R3 |
Figure 1.

Reference points and lines for skeletal and dental measurements.
Table 2.
Cephalometric Linear Measurements Used in the Analysis of Children in the Studya
| Value |
Full Name |
| NSAr |
Saddle Angle |
| SArGo | Articular angle |
| ArGoMe | Gonial angle |
| SUM | Sum angle |
| NGoAr | Upper gonial angle |
| NGoMe | Lower gonial angle |
| SAr:ArGo | Ratio of lat. cranial base and ramus height |
| GoMe:NS | Ratio of mand. and cranial base length |
| SNGoMe | Angle of anterior cranial base to mand. plane |
| NSG | Y axis to SN |
| SGo:NMe | Ratio of posterior to anterior facial height |
| ANS-Xi-Pm | Lower facial height |
| NBa-PtG | Facial axis |
| DC-Xi-Pm | Mandibular arc angle |
lat. indicates lateral; mand., mandibular.
Figure 2.
Line A to A': Measurement of adenoid thickness; B line: The occipital slope extracranial tangent; C point: posterior superior point of the hard palate; D point: posterior superior point of pterygoid lamina root; N line: Nasopharyngeal cavity width.
Sleep Monitoring (Polysomnography)
Polysomnography25 was conducted using a computerized Alice 5 system (Philips Respironics, Cedar Grove, New Jersey) for home monitoring of sleep disorder in the Sleep Monitor Center, Hospital of Stomatology, Wuhan University. The assembly of the PSG and the criteria for the report met the parameters described in the American Academy of Sleep Medicine manual.26 Pediatric PSG guidelines for diagnosing OSAS in children have been published.27 The AHI, defined as the average number of apneas and hypopneas per hour of total sleep time, was used for the diagnosis of OSAS, which was identified by an AHI of 1 or higher. Pediatric OSAHS severity was classified as mild (AHI < 5); moderate (AHI ≥ 5 to < 10); or severe (AHI ≥ 10). The lowest arterial oxygen saturation (Lsa O2%) as measured by pulse oximetry was used for diagnosis of hypoxemia. Hypoxemia severity was classified as mild (85%–91%), moderate (75%–84%), or severe (<75%).
Statistical Analysis
Changes of craniofacial structures were analyzed using cephalometric films. All measurements were repeated at an interval of at least four weeks and the error of method28 was calculated using the formula: s = , where s is the error of method, d is the difference between the first and second measurements, and 2n is the number of double registrations. All statistical analyses were performed using SPSS 17.0 (SPSS Inc., Chicago, Ill). Thus, the independent-samples t-test was used to compare the changes of craniofacial measurements from T0 to T1 of the two groups. A sample size calculation was not performed, as there has been no similar study in the literature.
, where s is the error of method, d is the difference between the first and second measurements, and 2n is the number of double registrations. All statistical analyses were performed using SPSS 17.0 (SPSS Inc., Chicago, Ill). Thus, the independent-samples t-test was used to compare the changes of craniofacial measurements from T0 to T1 of the two groups. A sample size calculation was not performed, as there has been no similar study in the literature.
RESULTS
The final sample consisted of 23 OSA children (mean age: 12.6 ± 1.2 years, range: 11–14 years) and 23 non-OSA children (mean age: 12.0 ± 1.2 years, range: 11–14 years). There were nine boys and 14 girls in the OSA group and seven boys and 16 girls in the non-OSAHS group. Pretreatment craniofacial measurements in the OSA group and the matched control group are shown in Table 3. No significant differences were found between the two groups. The molar relationship was Class I and the overbite and overjet were normalized after the treatment.
Table 3.
Comparison of Pretreatment Craniofacial Measurements Between OSA and Control Groups
| Variable |
Control Group, Mean ± SD |
OSA Group, Mean ± SD |
P Value*, P < .05 |
| NSAr | 123.39 ± 4.91 | 124.61 ± 4.73 | .427 |
| SArGo | 150.43 ± 4.88 | 151.61 ± 6.22 | .637 |
| ArGoMe | 120.78 ± 4.63 | 122.11 ± 6.55 | .583 |
| SUM | 394.60 ± 61.67 | 397.33 ± 5.35 | .265 |
| NGoAr | 45.61 ± 3.91 | 46.61 ± 4.60 | .455 |
| NGoMe | 75.17 ± 2.93 | 77.61 ± 4.22 | .096 |
| SNGoMe | 37.17 ± 8.45 | 37.11 ± 5.35 | .402 |
| NSG | 71.52 ± 3.53 | 73.39 ± 4.03 | .122 |
| ANS-Xi-Pm | 48.63 ± 3.88 | 48.85 ± 6.23 | .889 |
| NBa-PtG | 83.31 ± 3.27 | 82.23 ± 4.53 | .381 |
| DC-Xi-Pm | 33.15 ± 3.82 | 33.78 ± 4.46 | .623 |
| SAr:ArGo | 81.09 ± 8.33 | 81.22 ± 10.20 | .963 |
| GoMe:NS | 101.00 ± 14.64 | 102.67 ± 5.82 | .652 |
| SGo:NMe | 65.27 ± 2.29 | 62.39 ± 4.57 | .122 |
P < .05.
Radiographs were traced and measured on two separate occasions by the same author (KP-P) at least four weeks apart to calculate the error of the assessment, which was determined by intraclass correlation coefficients (ICC) using an absolute agreement definition. ICC varied from 0.934 to 0.993 for angular measurements and from 0.934 to 0.998 for linear measurements, indicating a satisfactory level of intra-investigator reliability.
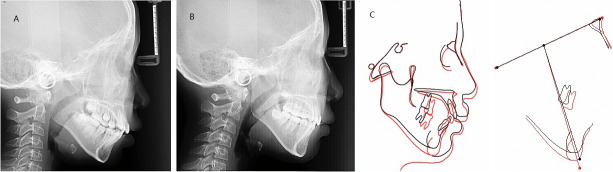
The gonial angle (NGoMe) and mandibular plane angle (SNGoMe) increased in the OSA group and decreased in the control group. The articular angle (SArGo) was found to increase in the OSAHS group but remain relatively unchanged in the control group. The sum of Jarabak angles (SUM) increased in the OSA group and decreased in the control group. The change in variables SArGo, SUM, NGoMe, and SN-GoMe from before to after orthodontic treatment were all found to be significantly different between the two groups (P < .05, Table 4). In the non-OSA group, there was an improvement in the craniofacial morphology; the mandibular plane angle decreased and the growth pattern became more horizontal (Figure 3). In contrast, the mandibular plane angle of subjects in the OSA group increased and the growth pattern became more vertical (Figure 4).
Table 4.
Cephalometric Changes of OSAHS and Control Groups Pretreatment and Posttreatment (Positive Values Signify Increase; Negative Values Signify Decrease)
| Variable |
Control Group, Mean ± SD |
OSAHS Group, Mean ± SD |
P Value*, P < .05 |
| NSAr | 0.348 ± 1.668 | −0.739 ± 2.281 | .072 |
| SArGo | −0.609 ± 2.624 | 4.012 ± 2.393 | .035* |
| ArGoMe | 0.044 ± 2.619 | 1 ± 2.486 | .211 |
| SUM | −0.22 ± 1.596 | 2.27 ± 1.825 | .025* |
| NGoAr | −0.044 ± 1.988 | −1.044 ± 1.965 | .702 |
| NGoMe | −0.174 ± 1.696 | 0.957 ± 1.96 | .019* |
| SNGoMe | −1 ± 1.537 | 2.85 ± 1.613 | .006* |
| NSG | −0.221 ± 1.421 | 0.392 ± 1.276 | .387 |
| ANS-Xi-Pm | 0.522 ± 1.697 | 1.171 ± 1.714 | .436 |
| NBa-PtG | 0.478 ± 1.236 | 0.313 ± 1.663 | .704 |
| DC-Xi-Pm | 1.144 ± 3.286 | 0.226 ± 2.881 | .32 |
| SAr:ArGo | −3.044 ± 5.085 | −2.391 ± 4.429 | .654 |
| GoMe:NS | 2.565 ± 3.087 | 1.608 ± 2.692 | .269 |
| SGo:NMe | 1.019 ± 1.49 | 0.031 ± 2.027 | .908 |
P < .05.
Figure 3.
Typical example of an OSAHS subject treated with fixed orthodontic appliances showing an unsatisfactory improvement in the craniofacial morphology: (A) pretreatment radiograph. (B) posttreatment radiograph. (C) cephalometric superimposition (pretreatment in black, posttreatment in green).
Figure 4.
Typical example of a subject in the control group (non-OSAHS) with fixed orthodontic appliances showing an improvement in the craniofacial morphology: (A) pretreatment radiograph, (B) posttreatment radiograph, (C) cephalometric superimposition (pretreatment in black, posttreatment in green).
DISCUSSION
The adenoids are a mass of nasopharyngeal lymphatic tissue and normally provide resistance against upper respiratory tract infections. The size is largest at the age of 10 and, thereafter, the size decreases. Adenoid hypertrophy from various causes is a common cause of upper airway obstruction in pediatric patients. Studies have shown that there is a bilateral relationship between upper airway obstruction and dentofacial developmental disorders.2,29
According to the complex function hypothesis, soft tissue covering the inside and outside of hard tissues guides the direction and volume of hard tissue growth; nasal breathing allows proper growth and development of the craniofacial complex. Macari and Haddad reviewed the various aspects of the association between mouth breathing and dentofacial growth and came to the conclusion that orthodontists play an important role in the early diagnosis of airway impairment and early clearance of the airway as ear, nose, and throat specialists became more aware of the potential effect on craniofacial development.30 Investigators have found an association between adenoidectomy and the change in the mode of breathing and the establishment of a more horizontally growing mandible.31 Although several reports have demonstrated dentofacial changes associated with upper airway obstruction, the current study is the first to show the effect of upper airway obstruction on the outcomes of fixed orthodontic treatment.
In normal growth and development, the mandible assumes a counterclockwise growth pattern with a decrease in the mandibular plane angle with age. In the presence of upper airway obstruction, studies have shown that the mandible assumes a more clockwise rotation.8 In children with a hyperdivergent growth pattern or high mandibular plane angle, extraction of four premolars may allow the mandibular molars to move forward and reduce lower facial height. Children with upper airway obstruction tend to have a backward and downward rotating mandible, which tends to oppose the orthodontic treatment goal. Orthodontic treatment for patients diagnosed with sleep apnea problems should be followed for a longer period of time because if airway problems persist after orthodontic treatment, relapse may occur.32
In the present study, the control subjects consisted of children whose adenoids either went through atrophy or had adenoidectomy before orthodontic treatment. Most of the OSAHS subjects in this study had mild to moderate upper airway obstruction symptoms since those children who had severe symptoms already received adenoidectomy treatment in most cases. Fortunately, significant findings were still evident between the two groups in the current study.
Vertical control is important for resolving hyperdivergent malocclusions. Orthodontists have found many ways to control vertical height, such as by using mini-implants and transpalatal arches. In the present study, pediatric OSA was shown to be a critical and influential factor to be considered in the vertical control during treatment of hyperdivergent malocclusions. In the future, craniofacial morphologic changes other than mandibular rotation should also be studied.
A limitation of this study was that there were several variables that could not be controlled such as force application and the rate of tooth movement that may differ from individual to individual. In the current study, only craniofacial hard tissues were assessed. Evaluation of soft tissue outcomes requires longer follow-up periods and, therefore, was not included in this pilot. Future research is needed for long-term observation of the effects of airway obstruction on craniofacial changes affecting three-dimensional soft tissue development.
Overnight polysomnography is considered to be the gold standard for the diagnosis of OSA in children.25 However, the procedure is costly, time-consuming, and frequently inaccessible for many children. Thus, not all of the children in this study participated in sleep monitoring during, or at the end of, orthodontic treatment to check on the sleep breathing conditions. In the current study, this procedure was only performed at the beginning of treatment.
Despite its limitations, this study demonstrated the possible impact of airway obstruction on growth and treatment. The results agreed with a five-year longitudinal study,7 which reported that a change in breathing mode could influence both the spatial position of the mandible (by halting the posterior rotation originally encountered) and the mandibular form (by producing a more anterior direction of growth). The present study provides additional evidence for a need to work with ENT specialists in the orthodontic treatment of pediatric patients with OSAHS.
CONCLUSIONS
The presence of OSA has a deleterious effect on the treatment outcome of hyperdivergent patients receiving comprehensive orthodontic treatment. Examination of airway obstruction and sleep breathing disorders is recommended for routine treatment planning. Early diagnosis and management of pediatric OSA can affect the orthodontic treatment outcome of these patients.
REFERENCES
- 1.Guilleminault C, Eldridge FL, Simmons FB, Dement WC. Sleep apnea in eight children. Pediatrics. 1976;58:23–30. [PubMed] [Google Scholar]
- 2.McNamara J. Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981;51:269–300. doi: 10.1043/0003-3219(1981)051<0269:IORPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Clark W. Preventing dentofacial abnormalities with the proper correction of pediatric upper airway obstruction. Arch Otolaryngol Head Neck Surg. 2005;131:916–918. doi: 10.1001/archotol.131.10.916. [DOI] [PubMed] [Google Scholar]
- 4.Peltomki T. The effect of mode of breathing on craniofacial growthrevisited. Eur J Orthod. 2007;29:426–429. doi: 10.1093/ejo/cjm055. [DOI] [PubMed] [Google Scholar]
- 5.Al Ali A, Richmond S, Popat H, et al. The influence of snoring, mouth breathing and apnoea on facial morphology in late childhood a three-dimensional study. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-009027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grauer D, Cevidanes LS, Styner MA, Ackerman JL, Proffit WR. Pharyngeal airway volume and shape from cone-beam computed tomography: relationship to facial morphology. Amer J Orthodontics. 2009;136:805–814. doi: 10.1016/j.ajodo.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zettergren-Wijk L, Forsberg CM, Linder-Aronson S. Changes in dentofacial morphology after adeno-/tonsillectomy in young children with obstructive sleep apnoea–a 5-year follow-up study. Eur J Orthodont. 2006;28:319–326. doi: 10.1093/ejo/cji119. [DOI] [PubMed] [Google Scholar]
- 8.Harari D, Redlich M, Miri S, Hamud T, Gross M. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. The Laryngoscope. 2010;120:2089–2093. doi: 10.1002/lary.20991. [DOI] [PubMed] [Google Scholar]
- 9.Carvalho FR, Lentini-Oliveira DA, Carvalho GM, Prado LB, Prado GF, Carvalho LB. Sleep-disordered breathing and orthodontic variables in children–pilot study. Int J Pediatr Otorhi. 2014;78:1965–1969. doi: 10.1016/j.ijporl.2014.08.040. [DOI] [PubMed] [Google Scholar]
- 10.Borges Pde T, Filho ES, Araujo TM, et al. Correlation of cephalometric and anthropometric measures with obstructive sleep apnea severity. Int Arch Otorhi. 2013;17:321–328. doi: 10.7162/S1809-977720130003000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang YS, Guilleminault C. Pediatric obstructive sleep apnea and the critical role of oral-facial growth: evidences. Front Neurol. 2012;3:184. doi: 10.3389/fneur.2012.00184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Esteller Moré E, Pons Calabuig N, Romero Vilariño E, et al. Dentofacial development abnormalities in paediatric sleep-related breathing disorders. Acta Otorrinolaringol. (English Edition) 2011;62:132–139. doi: 10.1016/j.otorri.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Tsuda H, Fastlicht S, Almeida FR, Lowe AA. The correlation between craniofacial morphology and sleep-disordered breathing in children in an undergraduate orthodontic clinic. Sleep Breath. 2011;15:163–171. doi: 10.1007/s11325-010-0345-4. [DOI] [PubMed] [Google Scholar]
- 14.Villa MP, Rizzoli A, Rabasco J, et al. Rapid maxillary expansion outcomes in treatment of obstructive sleep apnea in children. Sleep Med. 2015;16:709–716. doi: 10.1016/j.sleep.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 15.Katyal V, Pamula Y, Daynes CN, et al. Craniofacial and upper airway morphology in pediatric sleep-disordered breathing and changes in quality of life with rapid maxillary expansion. Am J Orthod Dentofac. 2013;144:860–871. doi: 10.1016/j.ajodo.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 16.Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion (RME) for pediatric obstructive sleep apnea: a 12-year follow-up. Sleep Med. 2015;16:933–935. doi: 10.1016/j.sleep.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 17.Ashok N, Varma NK, Ajith VV, Gopinath S. Effect of rapid maxillary expansion on sleep characteristics in children. Contemp Clin Dent. 2014;5:489–494. doi: 10.4103/0976-237X.142817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosen G. Identification and evaluation of obstructive sleep apnea prior to adenotonsillectomy in children: is there a problem? Sleep Med. 2003;4:273–274. doi: 10.1016/s1389-9457(03)00115-1. [DOI] [PubMed] [Google Scholar]
- 19.Linder-Aronson WD., S1 Normalization of incisor position after adenoidectomy. Am J Orthod Dentofac. 1993;103:412–427. doi: 10.1016/S0889-5406(05)81792-5. [DOI] [PubMed] [Google Scholar]
- 20.Linder-Aronson S, Woodside DG. Mandibular growth direction following adenoidectomy. Amer J Orthod. 1986;89:273–284. doi: 10.1016/0002-9416(86)90049-7. [DOI] [PubMed] [Google Scholar]
- 21.Woodside DG, Linder-Aronson S. The channelization of upper and lower anterior face heights compared to population standard in males between ages 6 to 20 years European Journal of Orthodontics. 1979;1(1):25–40. doi: 10.1093/ejo/1.1.25. [DOI] [PubMed] [Google Scholar]
- 22.Woodside DG, Linder-Aronson S. Mandibular and maxillary growth after changed mode of breathing. Am J Orthod Dentofac. 1991;100:1–18. doi: 10.1016/0889-5406(91)70044-W. [DOI] [PubMed] [Google Scholar]
- 23.Moorrees CFA. Natural head position, a basic consideration in the interpretation of cephalometric radiographs. Am J Phys Anthropol. 2013;16:213–234. [Google Scholar]
- 24.Cassiabd D. Natural position of the head: review of two-dimensional and three-dimensional methods of recording. Br J Oral Maxillofac Surg. 2016;54:233–240. doi: 10.1016/j.bjoms.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 25.Carroll JL, Loughlin GM. Diagnostic criteria for obstructive sleep apnea syndrome in children. Pediatr Pulm. 1992;14:71–74. doi: 10.1002/ppul.1950140202. [DOI] [PubMed] [Google Scholar]
- 26.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anonymous. Standards and indications for cardiopulmonary sleep studies in children. American Thoracic Society. Am J Resp Crit Care. 1996;153:866–878. doi: 10.1164/ajrccm.153.2.8564147. [DOI] [PubMed] [Google Scholar]
- 28.Dahlberg G. Statistical methods for medical and biological student by Gunnar Dahlberg. BMJ. 1940;2:358–359. [Google Scholar]
- 29.Dunn GF, Gree LJ, Cunat JJ. Relationships between variation of mandibular morphology and variation of nasopharyngeal airway size in monozygotic twins. Angle Orthod. 1973;43:129–135. doi: 10.1043/0003-3219(1973)043<0129:RBVOMM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Macari AT, Haddad RV. The case for environmental etiology of malocclusion in modern civilizations—Airway morphology and facial growth. Semin Orthod. 2016;22:223–233. [Google Scholar]
- 31.Becking BE, Verweij JP, Kalf-Scholte SM, Valkenburg C, Bakker EWP, van Merkesteyn JPR. Impact of adenotonsillectomy on the dentofacial development of obstructed children: a systematic review and meta-analysis. Eur J Orthod. 2017;39:509–518. doi: 10.1093/ejo/cjx005. [DOI] [PubMed] [Google Scholar]
- 32.Schmidt-Nowara W, Lowe A, Wiegand L, Cartwright R, Perez-Guerra F, Menn S. Oral appliances for the treatment of snoring and obstructive sleep aepna: a review. Sleep. 1995;18:501–510. doi: 10.1093/sleep/18.6.501. [DOI] [PubMed] [Google Scholar]