Abstract
Objectives:
To evaluate quantitatively the relationship between molar intrusion (change [Δ] maxillary first molar [U6]–palatal plane [PP]) and changes in vertical and sagittal cephalometric parameters and to determine the center of mandibular autorotation.
Materials and Methods:
Twenty-one patients diagnosed with anterior open bite and successfully treated with molar intrusion (overbite [OB] > 0 mm) were retrospectively enrolled. Lateral cephalograms taken before and after molar intrusion were used to measure changes in vertical and sagittal cephalometric parameters. The center of mandibular autorotation was calculated by measuring displacement of gonion (Go) and pogonion (Pog). Paired t-tests were used to compare variables, and linear regression analysis was used to examine the relationship between ΔU6-PP and other variables.
Results:
The mandible exhibited counterclockwise rotation after maxillary molar intrusion, which led to closure of anterior open bite. Strong linear relationships, in descending order, between ΔU6-PP and ΔOB, Δanterior facial height (AFH), Δvertical reference plane (Pog), and Δsella-nasion to Go-menton (SN-GoMe), were observed. When the maxillary molar was intruded 1 mm, OB increased by 2.6 mm, AFH decreased by 1.7 mm, Pog moved forward by 2.3 mm, and SN-GoMe decreased by 2°. The center of mandibular autorotation was located 7.4 mm behind and 16.9 mm below condylion after molar intrusion.
Conclusions:
The mandible exhibited counterclockwise rotation after maxillary molar intrusion; the center of mandibular autorotation was located behind and below condylion with individual variations.
Keywords: Center of rotation, Molar intrusion, Anterior open bite
INTRODUCTION
Anterior open bite (AOB) is a challenging problem to correct because it results from the interaction of several skeletal, dental, functional, and habitual factors and is associated with a high relapse rate.1,2 Skeletal open bite is characterized by a steep mandibular plane, an increased lower facial height, and an obtuse gonial angle, while dental open bite is characterized by proclined incisors and excessive molar height.1,3 Regardless of origin, treatment of AOB is accompanied by changes in the occlusal plane and subsequent autorotation of the mandible.4,5
Surgical and nonsurgical approaches have been introduced for the correction of AOB, and similar relapse rates (approximately 21% to 23%) have been reported.6,7 In conventional surgical approaches, the maxillary posterior segment is impacted to resolve AOB and to enhance facial esthetics. With the advent of temporary anchorage devices, nonsurgical correction of AOB has become feasible by intruding the posterior teeth, and successful and stable treatment outcomes have been reported.8,9 Based on the results of a meta-analysis reporting similar stability between the two approaches,10 nonsurgical correction of AOB is preferred and is considered to be an effective and reliable method without the burdens of surgery.
Molar intrusion in patients with AOB results in counterclockwise rotation of the mandible, forward positioning of the chin, decrease in facial height, and increase in overbite (OB).11,12 It leads to changes in the vertical relationship, which also leads to changes in the sagittal relationship. Therefore, orthodontic diagnosis needs to be reevaluated after closure of AOB. For example, a patient with AOB whose skeletal and dental relationships are Class II can exhibit Class I relationships after molar intrusion, which may alter the scheme of orthodontic extraction. Therefore, it is important to quantify the proportion of changes in vertical and sagittal parameters according to the extent of molar intrusion and to determine the center of mandibular autorotation, which was defined in the present study as the center of rotation of the mandible after molar intrusion, for accurate diagnosis and correct treatment planning.
The center of rotation of the mandible following maxillary impaction surgery has been reported to exhibit significant variation.13–16 It is located at the top of condylar head,14 at the mastoid region,15 or 8.4 mm behind and 25.1 mm below,16 or 2.5 mm behind and 19.6 mm below,13 the radiographic center of the condyle. However, there have been few studies investigating the center of mandibular autorotation following molar intrusion. In particular, the relationship between the amount of molar intrusion and subsequent changes in cephalometric measurements, such as the sagittal position of pogonion (Pog), anterior facial height (AFH), and OB, have rarely been reported. One previous review, however, reported that the mandibular plane angle decreased by 2.3° to 3.9° after molar intrusion.1
If the amount of molar intrusion can be related proportionately to changes in cephalometric measurements, thereby determining the center of mandibular autorotation, this predictive model would be a valuable diagnostic tool for mandibular counterclockwise rotation following molar intrusion. Therefore, the aims of this study were to investigate quantitatively the relationship between the amount of molar intrusion and changes in vertical and sagittal cephalometric parameters and to determine the center of mandibular autorotation.
MATERIALS AND METHODS
Subjects
This retrospective study included 21 subjects (3 men, 18 women; mean age 23.9 years [range 18.5–36.4 years]) who were selected from a total of 41 consecutive orthodontic patients who visited the Yonsei University Dental Hospital between February 2004 and November 2015 and who were diagnosed with AOB and treated using molar intrusion. The inclusion criteria were as follows: initial OB <−2.0 mm, AOB resolved by intrusion of the maxillary molars bilaterally, availability of lateral cephalogram imaging data before (T1) and immediately after (T2) molar intrusion, amount of intrusion (difference in perpendicular distances of the maxillary first molar [U6] to the palatal plane [PP]) >1.0 mm, no or minor (<1 mm) tooth movement during molar intrusion, and age >18 years. The exclusion criteria were as follows: tooth extraction, except the third molars during molar intrusion; history of previous orthodontic treatment; presence of temporomandibular disorder; unstable occlusion such as CR-CO discrepancy; systemic disease; cleft lip or palate; and craniofacial syndrome(s). A sample size of 21 subjects was estimated at a significance level of P < .05, a power of 80%, and an effect size of 1.0 (G*Power 3, Düsseldorf, Germany), to detect changes in vertical and sagittal cephalometric parameters before and after molar intrusion on the basis of a previous study.2
Molar intrusion was performed bilaterally by using orthodontic miniscrews, which had been implanted in the interproximal alveolar bone of the maxillary posterior teeth on the buccal and palatal sides. The intrusive force was directly applied only to the maxillary posterior teeth that were not connected to the anterior teeth and was not applied to the mandibular molars. During molar intrusion, the other teeth, including the mandibular teeth, did not undergo orthodontic treatment or were aligned separately by an amount that was <1 mm in terms of sagittal and vertical movement of the central incisor on the lateral cephalogram. The mean amount of molar intrusion was 2.2 ± 0.8 mm, and the mean treatment period was 9.7 ± 3.2 months (range, 6.2–15.2 months). This study was approved by the Institutional Review Board of Yonsei University Dental Hospital (2-2016-0017).
Measurements
Lateral cephalograms were performed at a voltage setting of 67–71 kV at 10 mA (Cranex 3+, Soredex Orion Corp, Helsinki, Finland), and the magnification ratio was verified for every image by using a calibration bar. Four reference planes were constructed for the horizontal and vertical measurements. A horizontal reference plane (HRP) was drawn 7° upward from the sella-nasion (SN) line at nasion. A vertical reference plane (VRP) was drawn perpendicular to the HRP through sella. The PP connecting the anterior and posterior nasal spines, and the mandibular plane (MP) connecting the lower gonion (Go) and menton (Me), were also registered for the maxillary and mandibular reference planes, respectively.
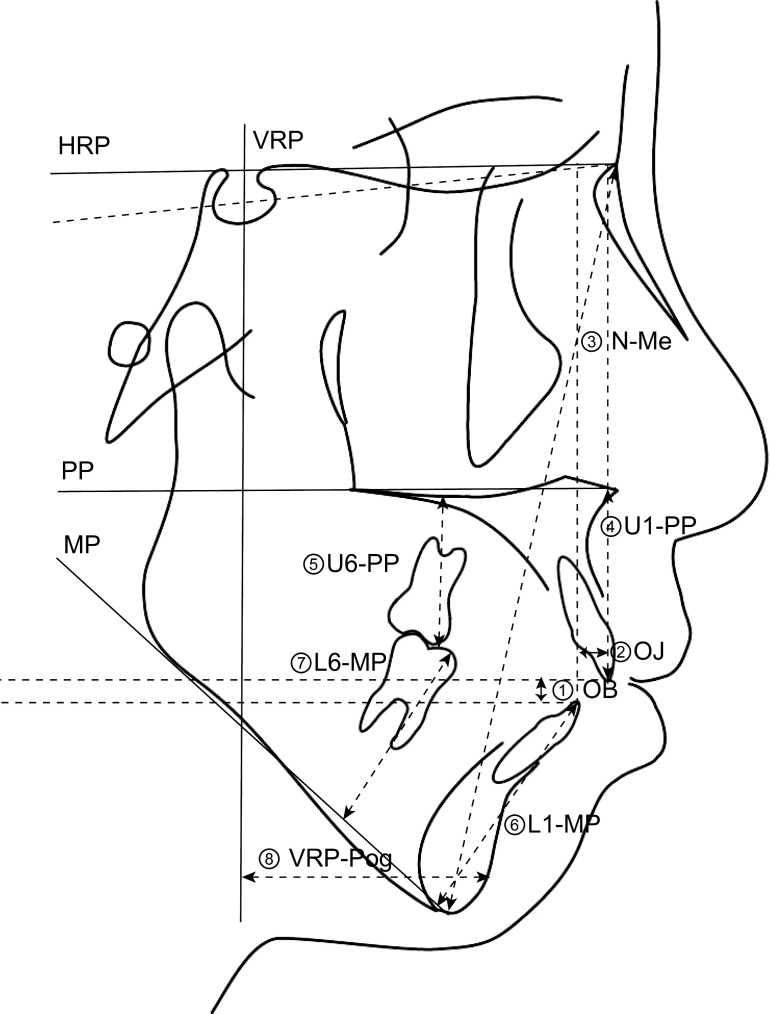
As described in Table 1 and Figure 1, SNA, SNB, ANB, overjet (OJ), and the perpendicular distance of Pog to the VRP (VRP-Pog) were measured to evaluate sagittal changes after molar intrusion; OB, SN-GoMe, and AFH were used to evaluate vertical changes. To quantify the extent of tooth movement, perpendicular distances of the central incisor and first molar to the PP and MP (U1-PP, U6-PP, L1-MP, and L6-MP) were measured. Tracings and measurements were performed using V-ceph software version 5.5 (Osstem Implant Inc, Seoul, Korea).
Table 1.
Definition of Cephalometric Measurements Used in This Studya
| Measurement |
Definition |
| Sagittal parameters | |
| SNA, ° | Sella-nasion-A point angle |
| SNB, ° | Sella-nasion-B point angle |
| ANB, ° | A point-nasion-B point angle |
| VRP-Pog, mm | Perpendicular distance of pogonion to the vertical reference plane (VRP) |
| OJ, mm | Overjet, parallel distance between the incisal edges of U1 and L1 to the horizontal reference plane (HRP) |
| Vertical parameters | |
| SN-GoMe, ° | Mandibular plane angle, the angle between sella-nasion line and gonion-menton line |
| AFH, mm | Anterior facial height, linear distance between nasion and menton |
| OB, mm | Overbite, parallel distance between the incisal edges of U1 and L1 to the VRP |
| Tooth movement | |
| U6-PP, mm | Perpendicular distance of the mesial cusptip of U6 to the palatal plane (PP) |
| U1-PP, mmb | Perpendicular distance of U1 incisal edge to the PP |
| L6-MP, mm | Perpendicular distance of the mesial cusptip of L6 to the mandibular plane (MP) |
| L1-MP, mmb | Perpendicular distance of L1 incisal edge to the MP |
U1 and L1 indicate the maxillary and mandibular central incisor, respectively; U6 and L6, the maxillary and mandibular first molar, respectively.
The most anterior tooth was used for the measurement.
Figure 1.
Cephalometric measurements. A horizontal reference plane (HRP) was drawn 7° upward from the sella-nasion line at nasion, and a vertical reference plane (VRP) was drawn perpendicular to the HRP through sella. PP indicates palatal plane; MP mandibular plane; N, nasion; Me, menton; U1 and L1, the maxillary and mandibular central incisor, respectively; U6 and L6, the maxillary and mandibular first molar, respectively; OJ, overjet; OB, overbite; Pog, pogonion.
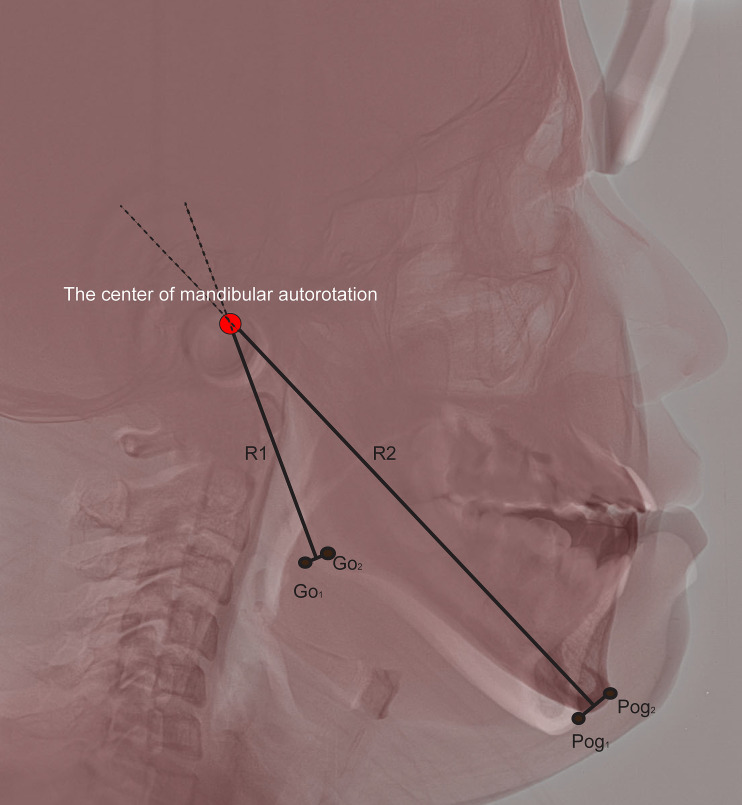
The center of mandibular autorotation was calculated for each subject according to the Reuleaux method.17 Two lateral cephalograms, captured at T1 and T2, were superimposed onto the anterior cranial base using Photoshop version CS6 (Adobe Systems Inc, San Jose, Calif) based on the best-fit method.18 By doing this, the two images could be placed on the same coordinate system. The superimposed image was reoriented by making the Frankfort horizontal plane parallel to the ground. Two mandibular landmarks (Pog and Go) were identified on each lateral cephalogram and subsequently coordinated on the superimposed image (Pog1, Pog2, Go1, and Go2) by registering condylion at T1 as a reference point (0,0). The x and y coordinates of the four landmarks were transferred from Photoshop to GeoGebra software (International GeoGebra Institute, Linz, Austria). The center of mandibular autorotation was defined as the intersection point of the two perpendicular bisectors running through the Pog1-Pog2 and Go1-Go2 lines (Figure 2).
Figure 2.
Description of locating the center of mandibular autorotation using the Reuleaux method.17 Go1 and Go2, gonion point before and after molar intrusion, respectively; Pog1 and Pog2, pogonion point before and after molar intrusion, respectively; R1, perpendicular bisector through Go1-Go2 line; R2, perpendicular bisector through Pog1-Pog2 line.
Statistical Analysis
All data were confirmed to be normally distributed using the Shapiro-Wilk test. Paired t-tests were used to compare variables at T1 and T2. Linear regression analysis was used to examine the relationship between change (Δ) U6-PP (causal variable) with four variables of interest: ΔOB, ΔSN-GoMe, ΔAFH, and ΔVRP-Pog. These four variables had been selected based on a previous systematic review investigating mandibular changes after molar intrusion.1 P < .05 was considered to be statistically significant.
The statistical analysis was performed using SPSS version 20.0 (SPSS Inc, Chicago, Ill). All variables were measured twice by the same investigator to calculate error in the method. Differences between the two sets of measurements were insignificant; the intraclass correlation coefficient was >.96.
RESULTS
After intrusion of the maxillary molars, the mandible exhibited counterclockwise rotation, which was confirmed by increases in SNB and OB; decreases in ANB, OJ, SN-GoMe, and AFH; and forward movement of Pog (P < .001; Table 2). U6-PP decreased by 2.2 mm (P < .001) and, consequently, OB increased by 4.5 mm, SN-GoMe decreased by 2.7°, AFH decreased by 3.0 mm, and VRP-Pog increased by 3.8 mm (P < .001). There were no significant differences in SNA, L6-MP, or L1-MP during molar intrusion (P > .05).
Table 2.
Cephalometric Variables Before (T1) and After (T2) Molar Intrusiona
| Variables |
T1 |
T2 |
ΔT2–T1 |
P Value |
| Sagittal parameters | ||||
| SNA, ° | 81.1 ± 3.3 | 81.0 ± 3.3 | 0.1 ± 0.3 | .374 |
| SNB, ° | 76.4 ± 3.6 | 77.5 ± 3.5 | 1.2 ± 0.7 | .000*** |
| ANB, ° | 4.8 ± 2.3 | 3.6 ± 2.3 | −1.2 ± 0.7 | .000*** |
| VRP-Pog, mm | 56.1 ± 8.3 | 59.9 ± 8.7 | 3.8 ± 1.3 | .000*** |
| OJ, mm | 4.6 ± 2.1 | 2.8 ± 1.6 | −1.7 ± 1.6 | .000*** |
| Vertical parameters | ||||
| SN-GoMe, ° | 41.9 ± 5.7 | 39.2 ± 5.6 | −2.7 ± 0.7 | .000*** |
| AFH, mm | 137.4 ± 6.9 | 134.4 ± 6.5 | −3.0 ± 1.2 | .000*** |
| OB, mm | −3.3 ± 1.3 | 1.2 ± 0.9 | 4.5 ± 1.5 | .000*** |
| Tooth movement | ||||
| U6-PP, mm | 26.4 ± 1.8 | 24.2 ± 1.8 | −2.2 ± 0.8 | .000*** |
| U1-PP, mm | 32.4 ± 2.7 | 32.9 ± 2.3 | 0.1 ± 0.9 | .000*** |
| L6-MP, mm | 33.0 ± 3.1 | 32.2 ± 3.4 | 0.4 ± 0.8 | .811 |
| L1-MP, mm | 45.5 ± 2.9 | 45.3 ± 3.2 | 0.1 ± 0.8 | .894 |
Data are presented as mean ± standard deviation. Please refer to Table 1 for the definition of each measurement. Paired t-tests were performed for each variable.
P < .001.
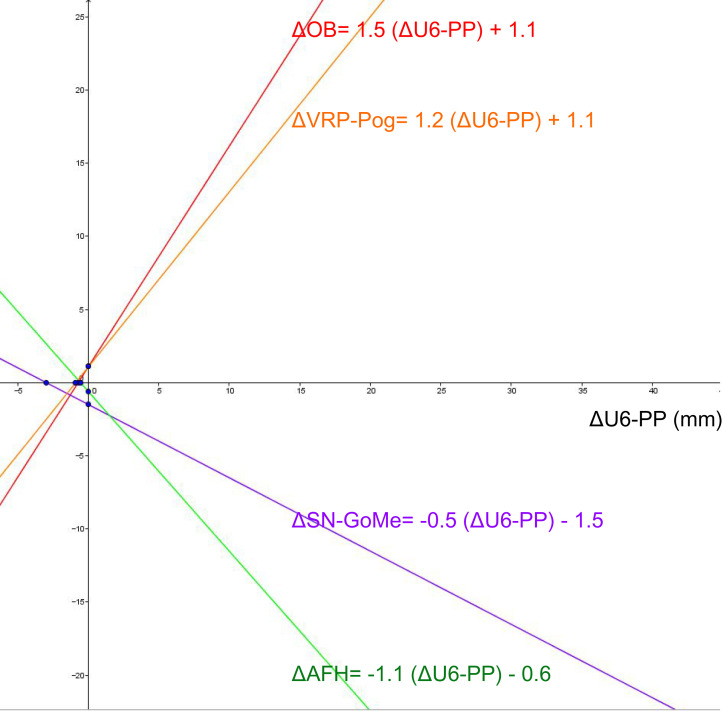
Table 3 summarizes significant associations between ΔU6-PP and ΔOB, ΔSN-GoMe, ΔAFH, and ΔVRP-Pog (P ≤ .001). From the data, the following linear models were deduced:
Table 3.
Correlation Coefficients of OB, SN-GoMe, AFH, and VRP-Pog According to U6-PPa
| Variables |
Coefficient |
SE |
R2 |
P Value |
| OB | ||||
| Constant | 1.1 | 0.5 | .718 | .047* |
| U6-PP | 1.5 | 0.2 | .000*** | |
| SN-GoMe | ||||
| Constant | −1.5 | 0.3 | .456 | .000*** |
| U6-PP | −0.5 | 0.1 | .001** | |
| AFH | ||||
| Constant | −0.6 | 0.5 | .541 | .319 |
| U6-PP | −1.1 | 0.2 | .000*** | |
| VRP-Pog | ||||
| Constant | 1.1 | 0.6 | .538 | .076 |
| U6-PP | 1.2 | 0.3 | .000*** | |
Please refer to Table 1 for the definition of the variables. A linear regression analysis was performed. SE indicates standard error.
P < .05; ** P < .01; *** P < .001.
ΔOB = 1.5ΔU6-PP + 1.1
ΔSN-GoMe = −0.5ΔU6-PP – 1.5
ΔAFH = −1.1ΔU6-PP – 0.6
ΔVRP-Pog = 1.2ΔU6-PP + 1.1
The center of mandibular autorotation was located, on average, 7.4 mm behind and 16.9 mm below condylion (Figure 3). The range in the horizontal and vertical directions (x-axis and y-axis, respectively) was 1.6–12.7 mm and 5.8–27.0 mm, with a standard deviation of 5.9 mm and 11.8 mm, respectively. The closest center of mandibular autorotation (closest to the average) was 7.3 mm behind and 16.8 mm below condylion, while the furthest was 7.0 mm ahead and 10.8 mm below condylion.
Figure 3.
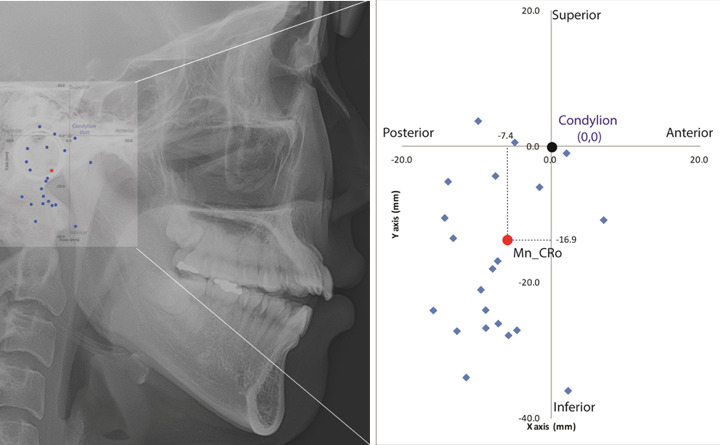
The center of mandibular autorotation (Mn_CRo) after molar intrusion. Blue “rhombus” dots represent the location of the calculated center of mandibular autorotation for each subject, and the red “round” dot demonstrates the average center of mandibular autorotation for all subjects in this study. Condylion before molar intrusion was set as a reference point (0,0) in the coordinate system.
DISCUSSION
This retrospective study confirmed the counterclockwise rotation of the mandible after orthodontic molar intrusion for AOB correction. When the maxillary molar was intruded by 1 mm, OB increased by 2.6 mm, AFH decreased by 1.7 mm, Pog moved forward by 2.3 mm, and the SN-GoMe angle decreased by 2°. From the counterclockwise mandibular rotation measured in the 21 subjects in this study, it was determined that the center of rotation of the mandible (ie, center of mandibular autorotation) was located, on average, 16.9 mm below and 7.4 mm behind condylion.
The relationship between the extent of molar intrusion (ΔU6-PP) and changes in vertical (ΔOB, ΔSN-GoMe, and ΔAFH) and sagittal (ΔVRP-Pog) cephalometric parameters was quantified. As shown in Figure 4, the strongest correlation was observed between ΔOB and ΔU6-PP. Although only subjects whose tooth movement, except molar intrusion, was <1 mm were included, extrusion of the maxillary incisors (ΔU1-PP), which was 0.5 mm, may have affected ΔOB. The weakest correlation was observed between ΔSN-GoMe and ΔU6-PP, while ΔAFH and ΔVRP-Pog were moderately correlated with ΔU6-PP. This may be because displacement of Go was smaller than that of Pog or Me because of the nearer proximity to the center of mandibular autorotation. Different scales (angular parameter) from other linear parameters or errors in the identification of Go, which was the only bilateral landmark, may have influenced the strength of correlation.
Figure 4.
Linear correlation plot of change (Δ) maxillary first molar–palatal plane (ΔU6-PP) with Δoverbite (OB), Δanterior facial height (AFH), Δvertical reference plane-pogonion (VRP-Pog), and Δsella-nasion to gonion-menton (SN-GoMe). x-axis: U6-PP; y-axis: ΔOB, ΔAFH, ΔVRP-Pog, and ΔSN-GoMe.
The center of rotation of the mandible after maxillary impaction via Le Fort I osteotomy exhibited a different location in previous studies.13–16 Different amounts of anterior and posterior impaction, and positional changes in sagittal direction after maxillary surgery, would affect mandibular rotation. The present study indicated that the center of mandibular autorotation after molar intrusion was located 7.4 mm behind and 16.9 mm below condylion, with lower standard deviation values compared with those reported in previous investigations. This may be because limited movement in the maxillary molar region after orthodontic molar intrusion would result in a more consistent pattern of mandibular rotation.
Despite the small standard deviation, there were large interindividual variations in the center of mandibular autorotation. Occlusion may have affected the results and been a cause of the large interindividual variations. Because other teeth, except the maxillary molars, did not undergo orthodontic treatment during molar intrusion, occlusal interferences may have occurred during mandibular autorotation, resulting in displacement of the mandibular position or limiting the extent of pure rotation. Individual variation in temporomandibular joint structures and ligaments (stylomandibular and sphenomandibular ligaments) can also limit pure rotation of the mandible as a free body because these two ligaments are responsible for limiting excessive opening and can affect the center of mandibular autorotation.19 Moreover, mandibular movement consists of rotation and translation.13 The center of rotation is positioned below and behind the condyle during rotational movement and shifts forward and downward during translational movement.20 In addition, the center of mandibular autorotation was identified on the basis of a two-dimensional cephalometric image, although the mandible is a three-dimensional structure. The center of mandibular autorotation in a two-dimensional image may not be representative of a real-life scenario, which may increase interindividual variation.
In the present study, only subjects in whom AOB had been resolved by intruding the maxillary molars on the buccal and palatal sides were enrolled because it is difficult to exert an intrusion force on the lingual side for mandibular molars. In addition, patients whose lateral cephalograms were taken during or after orthodontic treatment and not immediately after molar intrusion were excluded in an attempt to investigate pure mandibular movement only immediately after molar intrusion. Moreover, leveling and alignment, combined with orthodontic extraction when indicated, had been performed during molar intrusion, which resulted in a high dropout rate of approximately 49% for the subject selection. Given the limited number of subjects, the center of mandibular autorotation was calculated inductively. For future studies, it would be meaningful to determine the center of mandibular autorotation using cone-beam computed tomography, to conduct a three-dimensional analysis with more subjects, and to verify it deductively using computational simulation. A well-designed prospective study comparing before and after molar intrusion, without any orthodontic tooth movement, would provide more accurate results for changes in vertical and sagittal parameters.
CONCLUSIONS
After orthodontic molar intrusion, the mandible exhibited counterclockwise rotation.
The amount of molar intrusion (ΔU6-PP) demonstrated linear relationships with vertical (ΔOB, ΔSN-GoMe, and ΔAFH) and sagittal (ΔVRP-Pog) cephalometric parameters. When the maxillary molar was intruded 1 mm, OB increased by 2.6 mm, SN-GoMe decreased by 2°, AFH decreased by 1.7 mm, and Pog moved forward by 2.3 mm.
The center of mandibular autorotation was located, on average, 7.4 mm behind and 16.9 mm below condylion.
REFERENCES
- 1.Alsafadi AS, Alabdullah MM, Saltaji H, Abdo A, Youssef M. Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: a systematic review. Prog Orthod. 2016;17:9. doi: 10.1186/s40510-016-0122-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salehi P, Pakshir HR, Hoseini SA. Evaluating the stability of open bite treatments and its predictive factors in the retention phase during permanent dentition. J Dent (Shiraz) 2015;16:22–29. [PMC free article] [PubMed] [Google Scholar]
- 3.Haralabakis NB, Yiagtzis SC, Toutountzakis NM. Cephalometric characteristics of open bite in adults: a three-dimensional cephalometric evaluation. Int J Adult Orthodon Orthognath Surg. 1994;9:223–231. [PubMed] [Google Scholar]
- 4.Sondos Abuzinada FA. Mandibular changes associated with maxillary impaction and molar intrusion. Open J Stomatol. 2013;3:515–519. [Google Scholar]
- 5.Choi YJ, Kim DJ, Nam J, Chung CJ, Kim KH. Cephalometric configuration of the occlusal plane in patients with anterior open bite. Am J Orthod Dentofacial Orthop. 2016;149:391–400. doi: 10.1016/j.ajodo.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Baek MS, Choi YJ, Yu HS, Lee KJ, Kwak J, Park YC. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010;138:396.e1–396.e9. doi: 10.1016/j.ajodo.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 7.Denison TF, Kokich VG, Shapiro PA. Stability of maxillary surgery in openbite versus nonopenbite malocclusions. Angle Orthod. 1989;59:5–10. doi: 10.1043/0003-3219(1989)059<0005:SOMSIO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Choi YJ, Lee SH, Baek MS, Kim JY, Park YC. Consecutive condylectomy and molar intrusion using temporary anchorage devices as an alternative for correcting facial asymmetry with condylar hyperplasia. Am J Orthod Dentofacial Orthop. 2015;147:S109–S121. doi: 10.1016/j.ajodo.2014.04.025. [DOI] [PubMed] [Google Scholar]
- 9.Park YC, Lee SY, Kim DH, Jee SH. Intrusion of posterior teeth using mini-screw implants. Am J Orthod Dentofacial Orthop. 2003;123:690–694. doi: 10.1016/s0889-5406(03)00047-7. [DOI] [PubMed] [Google Scholar]
- 10.Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: a meta-analysis. Am J Orthod Dentofacial Orthop. 2011;139:154–169. doi: 10.1016/j.ajodo.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 11.Umemori M, Sugawara J, Mitani H, Nagasaka H, Kawamura H. Skeletal anchorage system for open-bite correction. Am J Orthod Dentofacial Orthop. 1999;115:166–174. doi: 10.1016/S0889-5406(99)70345-8. [DOI] [PubMed] [Google Scholar]
- 12.Albogha MH, Takahashi I, Sawan MN. Early treatment of anterior open bite: Comparison of the vertical and horizontal morphological changes induced by magnetic bite-blocks and adjusted rapid molar intruders. Korean J Orthod. 2015;45:38–46. doi: 10.4041/kjod.2015.45.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang YC, Ko EW, Huang CS, Chen YR. The inter-relationship between mandibular autorotation and maxillary LeFort I impaction osteotomies. J Craniofac Surg. 2006;17:898–904. doi: 10.1097/01.scs.0000234985.99863.97. [DOI] [PubMed] [Google Scholar]
- 14.Fish LC, Epker BN. Surgical-orthodontic cephalometric prediction tracing. J Clin Orthod. 1980;14:36–52. [PubMed] [Google Scholar]
- 15.Sperry TP, Steinberg MJ, Gans BJ. Mandibular movement during autorotation as a result of maxillary impaction surgery. Am J Orthod. 1982;81:116–123. doi: 10.1016/0002-9416(82)90035-5. [DOI] [PubMed] [Google Scholar]
- 16.Nattestad A, Vedtofte P. Mandibular autorotation in orthognathic surgery: a new method of locating the centre of mandibular rotation and determining its consequence in orthognathic surgery. J Craniomaxillofac Surg. 1992;20:163–170. doi: 10.1016/s1010-5182(05)80391-9. [DOI] [PubMed] [Google Scholar]
- 17.Reuleaux F. The Kinematics of Machinery: Outline of a Theory of Machines. London, UK: Macmillan;; 1986. [Google Scholar]
- 18.Ghafari J, Engel FE, Laster LL. Cephalometric superimposition on the cranial base: a review and a comparison of four methods. Am J Orthod Dentofacial Orthop. 1987;91:403–413. doi: 10.1016/0889-5406(87)90393-3. [DOI] [PubMed] [Google Scholar]
- 19.Gonzalez-Cabeza J. The ligaments of the temporomandibular joint. J Gnathol. 1988;7 [Google Scholar]
- 20.Terhune CE, Iriarte-Diaz J, Taylor AB, Ross CF. The instantaneous center of rotation of the mandible in nonhuman primates. Integr Comp Biol. 2011;51:320–332. doi: 10.1093/icb/icr031. [DOI] [PubMed] [Google Scholar]