Abstract
Objectives:
The aim of this study was to assess three-dimensionally the upper airway changes following functional appliance treatment in growing Class II patients.
Materials and Methods:
Pre-and post-treatment Cone beam computed tomography scans of 20 patients (age range: 9 to 12; mean: 11.4 ± 1.0 years) were retrieved from the list of patients previously treated with functional appliances in the Postgraduate Clinic at the Section of Orthodontics, Aarhus University, Denmark. Total and partial volumes of the upper airway (ie, lower nasopharynx, velopharynx, and oropharynx) were calculated. To rule out the effect of growth, the changes in the functional appliance group were compared to an age-matched Class I group of 18 patients (age range: 8 to 14; mean: 11.8 ± 1.4 years).
Results:
In the functional appliance group, all the partial and total volumes were significantly larger at the end of treatment when compared to the start of treatment (P < .003). On the other hand, when comparing the changes for the total and partial volumes of the upper airway in the functional appliance group with the Class I group, a statistical difference was seen only for the oropharynx (P = .022) and total volume (P = .025), with the functional appliance group showing a larger volume increment.
Conclusions:
An increase in the upper airway volume was found after treatment with functional appliances. This difference was mainly related to the changes at the oropharynx level, which differed significantly from what was observed in the Class I group.
Keywords: Cone-beam computed tomography, Upper airway, Functional appliance
INTRODUCTION
One of the first indications for using functional appliances was related to their effect on the upper airway. Indeed, in 1934, Pierre Robin suggested using an intraoral appliance to bring the lower jaw forward in newborns with mandibular deficiency, thereby preventing posterior relocation of the tongue during sleep and the occurrence of oropharyngeal collapse.1 This concept is now widely used in adult obstructive sleep apnea (OSA) patients to prevent an upper airway collapse during sleep using similar oral appliances.2 Moreover, the concept to relocate the mandible anteriorly is applied in dentofacial orthopedics by using functional appliances to stimulate mandibular growth in skeletal Class II growing patients with mandibular deficiency.3 Several authors have hypothesized that the functional orthopedic treatment of growing patients with deficient mandibles may lead to increased oropharyngeal airway dimensions, and some have suggested a possible reduction in the risk of future respiratory problems.4–7 In most of those investigations, the assessment of the upper airway was based on lateral cephalograms. On the other hand, Warren and Spalding stated that the relationship between nasorespiratory function and dentofacial development remained controversial as conventional plane 2D radiographic evidence is questionable.8 Indeed, 2D images are influenced by artifacts of distortion, differences in magnification, and superimposition of bilateral craniofacial structures.9,10 Most importantly, lateral cephalograms do not provide information on cross sectional areas or volumes, although it is known that linear measurements are only weakly correlated with cross-sectional areas or volumes of the upper airway. 11
Cone beam computed tomography (CBCT) facilitates accurate two-dimensional (2D) and three-dimensional (3D) measurements, therefore allowing assessment of cross-sectional areas and volumes of various maxillofacial structures. There is a lower radiation dose and relatively shorter scanning time compared to CT and magnetic resonance imaging, respectively.12 For these reasons, CBCT has been increasingly used for diagnosis, treatment planning, and treatment outcome assessment in the craniofacial area and it has been extensively used to study the relationship between upper airway dimensions and craniofacial morphology.13,14
The aim of the present study was to determine whether functional appliance therapy influences upper airway morphology in Class II growing patients. The null hypothesis of this retrospective study was that upper airway volume would not change following mandibular advancement treatment with functional appliances.
MATERIALS AND METHODS
Subjects
In this retrospective study, the data of Class II patients were collected from the database of the Section of Orthodontics, Department of Dentistry and Oral Health, Aarhus University, Denmark. Permission to analyze the data was obtained from the Danish Health Board (#2015-57-0002), and the data were collected under the permission of the Danish Data Protection Agency (#62908).
The inclusion criteria were: subjects were preadolescents having overjet equal to or greater than 6 mm, had been treated with an orthopedic functional appliance for stimulation of mandibular growth, had pre-and post-treatment large field of view CBCT scans in order to encompass all the relevant structures, and with the scans taken in a supine position and in occlusion. Exclusion criteria were subjects with pathologies involving the upper airway, subjects who had a medical history of allergic rhinitis, subjects who had a previous adenotonsillectomy procedure, and/or subjectively perceived respiratory problems as retrieved from the patients' records.
To rule out the effect of growth, the changes in the test group were compared with the corresponding changes in an age-matched Class I group selected from the same database of patients treated between 2008 and 2012. The inclusion criteria for this group were subjects were preadolescents with less than 6 mm overjet and a Class I molar relationship, had been treated without the use of a functional appliance or bite jumping appliance or intermaxillary elastics or expansion device, and had pre- and post-treatment CBCT scans with the same characteristics as described for the test group. Exclusion criteria for the Class I group were the same as for the test group. Baseline descriptive data of the two groups were used to check whether the two groups were matching with respect to age and treatment duration.
In the functional appliance group, records of 20 subjects (12 females, 8 males) with an age range of 9 to 12 (mean: 11.4 ± 1.0 years) were retrieved. For the Class I group, records of 18 patients (14 females, 4 males) with an age between 8 and 14 (mean: 11.8 ± 1.4 years) were retrieved.
3D Image Processing
All CBCT scans were taken with a supine scanner (NewTom 3G and 5G, QR s.r.l., Verona, Italy) and reconstructed with an isotropic voxel dimension of 0.30 mm. Raw data obtained from CBCT scanning were exported in DICOM (digital imaging and communications in medicine) format and imported into a specific software program (Mimics 15, Materialise, Leuven, Belgium). All measurements were done using a slightly modified version of the method described by Lenza and colleagues.11 The threshold levels used to generate the 3D reconstructions were determined for each CBCT dataset individually on the basis of a profile line traced through the upper airway starting from basion (Ba) until the posterior nasal spine (PNS) on the sagittal image corresponding to the midsagittal plane.11,15
Determination of Landmarks and Cephalometric Analysis
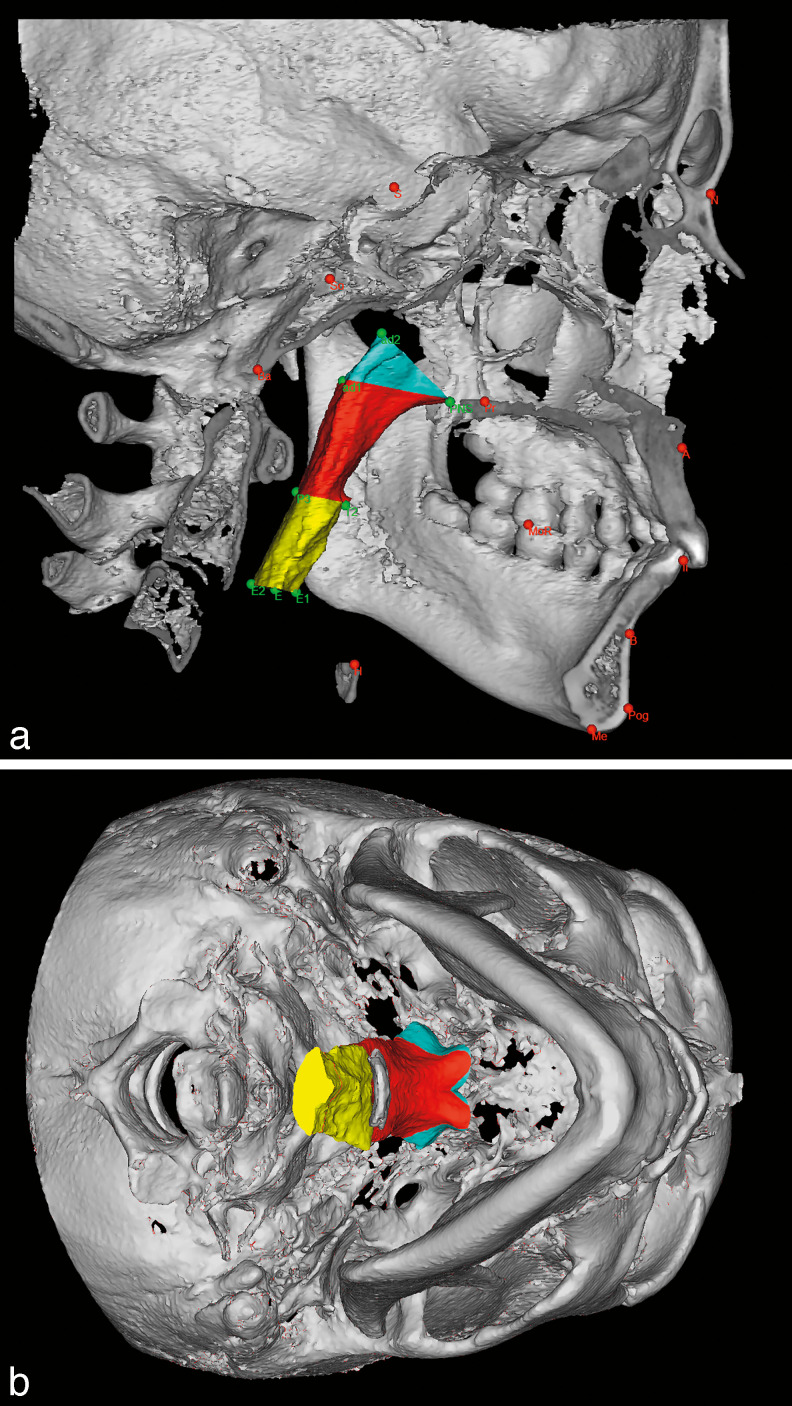
Twenty-three conventional landmarks were identified for the cephalometric analysis (Table 1). All landmarks were identified in the sagittal view of the midsagittal plane, and their position was checked on all three orthogonal planes (ie, coronal, sagittal, and transversal planes), except for the bilateral points that were identified on the 3D surface and finely adjusted by checking and relocating them on the axial, coronal, and sagittal views. Specific descriptions of the cephalometric measurements can be found in Table 1. The upper airway analysis was performed selecting eight anteroposterior landmarks to delimit the upper airway boundaries according to Di Carlo et al. 15 In order to describe the upper airway volumes, four planes passing through two of the previously defined points and perpendicular to the sagittal plane were generated (Table 2). According to the location of the planes, the total upper airway was divided into three parts and their volumes were calculated (Figures 1a and b): lower nasopharynx volume (LNP), bounded superiorly by ad2-PNS plane and inferiorly by ad1-PNS plane; velopharynx volume (VLP), bounded superiorly by ad1-PNS plane and inferiorly by T2-P3 plane; and oropharynx volume (ORP), bounded superiorly by T2-P3 plane and inferiorly by E1-E2 plane. Subsequently, the total volume, bounded superiorly by ad2-PNS plane and inferiorly by E1-E2 plane, was calculated (TV).
Table 1.
Cephalometric Landmarks and Measurements
| Description |
|
| Points | |
| Skeletal | |
| A | Position of the deepest concavity on anterior profile of the maxilla |
| ANS | Tip of anterior nasal spine |
| B | Most posterior point on the anterior contour of the lower alveolar process |
| Ba | Most postero-inferior point on the clivus |
| GoL | The most inferior-posterior point on the left angle of the mandible |
| GoR | The most inferior-posterior point on the right angle of the mandible |
| ii | A point midway between the incisal edges of the maxillary and mandibular central incisors |
| MoL | The distal tip of the first left molar in the jaw of interest |
| MoR | The distal tip of the first right molar in the jaw of interest |
| N | The intersection of the internasal and frontonasal sutures in the midsagittal plane |
| PNS | The most posterior point on the bony hard palate |
| Pl | Centroid of the greater palatine foramen left |
| Pr | Centroid of the greater palatine foramen right |
| PoG | The most anterior point of the bony chin in the midsagittal plane |
| S | Midpoint of the sella turcica |
| So | Midpoint of the sella-basion line |
| Airway | |
| ad1 | Intersection of the line PNS-Ba and the posterior nasopharyngeal wall |
| ad2 | Intersection of the line PNS-So and the posterior nasopharyngeal wall |
| P3 | Intersection between the posterior pharyngeal wall and the bisected Occlusal plane (OP) |
| T2 | Intersection between the contour of the tongue and the bisected OP |
| E | Most superior point of epiglottis |
| E1 | Frontal wall of pharyngeal airway over E1-E2 line |
| E2 | Posterior wall of pharyngeal airway over E1-E2 line |
| Measurements | |
| Overjet | This angle indicates the horizontal position of the maxilla relative to the cranial base. |
| ANB | Linear measurement from line through the upper incisal edge point perpendicular to the occlusal plane to a line through the lower incisal edge point perpendicular to the occlusal plane |
| Palatal width | Angle formed by the intersection of lines NA and NB, which measures the anterior-posterior relation of the maxilla and the mandible |
| SNB | Linear measurement from the left palatal point to the right |
| SNA | This angle expresses the horizontal position of the mandible relative to the cranial base. |
Table 2.
Airway Measurements
| Description |
|
| ad2-PNS | Upper sagittal depth of the nasopharyngeal airway |
| ad1-PNS | Lower sagittal depth of the nasopharyngeal airway |
| T2-P3 | Airway space measured from the dorsum of the tongue to the posterior pharyngeal wall on the bisected occlusal plane (OP) |
| E2-E1 | Plane passing through E perpendicular to PRLa |
PRL indicates line perpendicular to Frankfort horizontal plane passing through porion.
Figure 1.
(a, b) Three-dimensional reconstruction of the skull and airway volumes delimited by eight anteroposterior landmarks. Light blue = lower nasopharynx (LNP); red = velopharynx (VLP); yellow = oropharynx (ORP).
Statistical Analysis
The statistical analysis was carried out using SPSS (Version 13; SPSS, Chicago, Ill, USA). All measurements were performed by one operator (SI), who was previously trained and calibrated to identify 3D landmarks. Every DICOM file was anonymized and the operator was blinded regarding the type of image (Class II or Class I group, pre- or post-treatment). The intra-examiner error was calculated based on double measurements of 10 randomly selected cases at two different times using Dahlberg's formula.16 The coefficient of reliability, calculated as CoR = 1 − s2 / SD2 was calculated and a paired t-test was performed on the double measurements (Table 3). The data were checked for normal distribution; as they were not normally distributed, the intra group differences were assessed by the Wilcoxon signed-rank test. To compare intergroup differences, the Mann-Whitney rank-sum test was used.
Table 3.
Error of the Method (Double Measurements)a
| Error |
CoR |
Paired t-test |
|
| ANB (°) | 0.46 | 0.95 | 0.94 |
| LNP (mm3) | 148 | 0.98 | 0.86 |
| VLP (mm3) | 390 | 0.88 | 0.39 |
| ORP (mm3) | 314 | 0.94 | 0.25 |
| TV (mm3) | 706 | 0.92 | 0.35 |
Error indicates Dahlberg formula; CoR, coefficient of reliability.
RESULTS
The calculation of the error of the method revealed that the errors were small for all the measurements. The coefficient of reliability was good for all measurements and no systematic error in measuring was detected (Table 3).
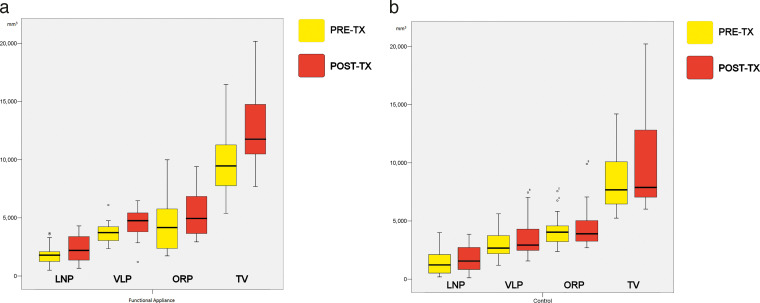
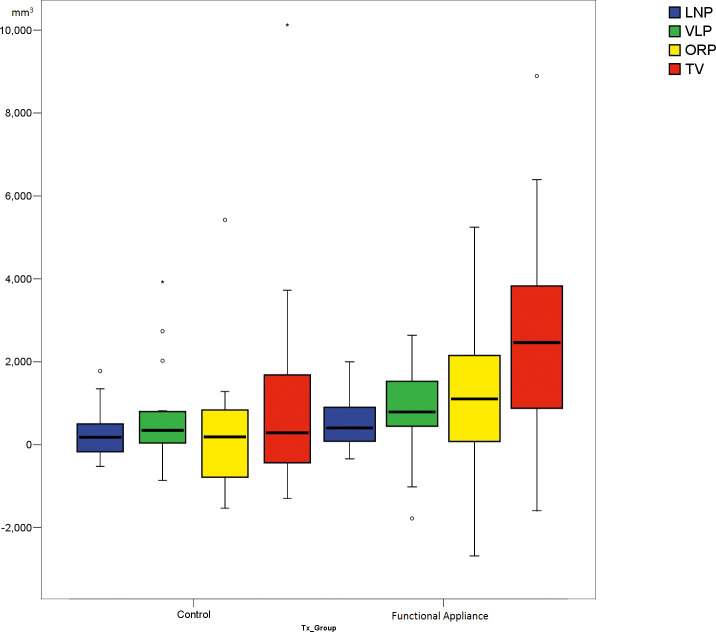
Treatment time was significantly shorter (21.7 ± 8.4 months) for the Functional appliance group compared to the Class I group (29 ± 8.5 months; P = .03). Functional appliances in the study group were distributed as follows: 8 Twin Block appliances and 12 modified monobloc activators. The pre- and post-treatment data for both groups are reported in Table 4, and the dental and skeletal treatment effects are reported in Table 5. The total and partial airway volumes (TV, LNP, VLP, and ORP) before and after treatment as well as the changes during treatment for both the Functional appliance and Class I groups are reported in Table 6, and Figures 2a, 2b, and 3.
Table 4.
Baseline Data and Post-treatment for Both Groups
| Functional Appliance |
Class I |
|||||||
| Pre-tx |
Post-tx |
Difference |
P Value |
Pre-tx |
Post-tx |
Difference |
P Value |
|
| Overjet (mm) | 9.5 ± 2.1 | 3.4 ± 1.1 | −6.2 ± 2.4 | <.001 | 4.5 ± 1.8 | 3.3 ± 0.8 | −1.2 ± 1.9 | .002 |
| ANB (°) | 5.7 ± 2.0 | 4.6 ± 1.7 | −1.1 ± 1.6 | .009 | 3.3 ± 1.4 | 3.3 ± 1.2 | 0.0 ± 0.7 | n.s. |
| SNA (°) | 80.6 ± 4.9 | 79.7 ± 4.5 | −1.0 ± 3.0 | n.s | 80.3 ± 5.1 | 80.2 ± 4.6 | −0.1 ± 1.3 | n.s. |
| SNB (°) | 75.1 ± 4.5 | 75.3 ± 3.7 | −0.2 ± 2.8 | n.s | 77.1 ± 4.4 | 77.1 ± 4.8 | 0.0 ± 1.2 | n.s. |
| Palatal width (mm) | 27.6 ± 1.7 | 28.7 ± 1.8 | 1.1 ± 1.2 | <.001 | 27.4 ± 2.5 | 28.2 ± 2.5 | 0.8 ± 1.0 | =.005 |
Table 5.
Difference in Treatment Effects
| Treatment Effect* Functional/Class I |
||
| Difference |
P Value |
|
| Overjet (mm) | −5 | <.001 |
| ANB (°) | −1.1 | .02 |
| SNA (°) | −0.9 | n.s. |
| SNB (°) | −0.2 | n.s. |
| Palatal width (mm) | 0.3 | n.s. |
Treatment effect = difference between pre-post-treatment changes between groups.
Table 6.
Baseline Data of Airway Measurements and Difference in Treatment Effects*
| Functional Appliance |
||||
| Pre-tx |
Post-tx |
Difference |
P Value |
|
| LNP (mm3) | 1791 ± 888 | 2359 ± 1129 | 568 | <.001 |
| VLP (mm3) | 3725 ± 876 | 4580 ± 1239 | 855 | .003 |
| ORP (mm3) | 4306 ± 2220 | 5472 ± 2031 | 1167 | .002 |
| TV (mm3) | 9822 ± 2660 | 12411 ± 2976 | 2590 | <.001 |
Tx effect = difference between pre-post treatment changes between groups; n.s. indicates not statistically significant.
Figure 2.
Differences between pre- and post-treatment partial and total volumes. (a) the Functional appliance group and (b) the Control group.
Figure 3.
Boxplot depicting the changes in upper airway during treatment for the partial and total volumes.
Table 6.
Extended
| Class I Group |
Tx Effect (Functional - Control) |
||||
| Pre-tx |
Post-tx |
Difference |
P Value |
Difference |
P Value |
| 1443 ± 1014 | 1715 ± 1156 | 271 | n.s | 297 | n.s |
| 2919 ± 1132 | 3543 ± 1689 | 624 | .04 | 231 | n.s |
| 4231 ± 1330 | 4465 ± 1823 | 234 | n.s | 933 | .022 |
| 8594 ± 2657 | 9722 ± 3845 | 1128 | n.s | 1462 | .025 |
DISCUSSION
The main purpose of this study was to assess with CBCT the changes in upper airway characteristics in children with Class II malocclusion after functional appliance treatment. When evaluating the upper airway, it was previously reported that the evaluation of the smallest cross-section alone was very imprecise.11,17,18 Therefore, it was decided to look only at the total and partial volume changes. This decision is supported by the existence of a strong correlation between the smallest cross-sectional area and the total volume.11,19 However, it has been shown in a large sample that a wide variability in airway volumes exists, which was confirmed by the present study.15,20
Thresholding is a major issue when measuring the upper airways on CBCTs. In the present study, a manual threshold value was individually determined for each CBCT scan: Though this is a time-consuming approach, this method was judged to be the most reproducible.11,20,21 This was also confirmed by the present study, where a high intraobserver reliability was observed. Moreover, the justification supporting this decision was that automatic segmentation is a notoriously difficult task to perform in computer graphics, especially when the images are characterized by noise and poor voxel consistency, as is the case with CBCT.20 Selecting voxels of a specific density range will invariably ignore some voxels that should be selected and include others that should not be selected.20
The upper airway dimension has been reported to be very dependent on head posture, mandibular position, tongue position, and respiration phase during CBCT acquisition.22 In this study, the patients were asked to bite in maximal intercuspation, not to swallow and to limit breathing during acquisition. The latter is quite difficult to control, especially in children; this might generate some inaccuracies when measuring the airway size. Moreover, CBCT scans were taken in the supine position. Although the upright position is closer to the natural head position and recommended for baseline assessment of upper airway morphology and dimensions, CBCT acquisition in a supine position is closer to sleeping position where a collapse of the airway is more prone to occur, though it is known that during sleep patients present different muscular tone compared to when they are awake.13,15
When dealing with treatment effect in growing patients, it is not easy to distinguish between changes due to treatment alone and due to growth. One possible way to solve this issue is to compare the treatment outcome with a matched control group. As this was a retrospective study based on CBCT scans, the settings were different from the ideal study design: a randomized control trial where the treatment effect would be evaluated using subjects with the same baseline characteristics, randomized into a treatment and a control group. However, performing such a randomized controlled trial raises ethical issues related to leaving a group of skeletal Class II subjects untreated for a long time, and with unnecessary exposure to ionizing radiation.23 An alternative could be the use of a Class II control group treated with Class II non-compliance distalization or elastics. However, there was not such a group of patients in the database, having both CBCT data pre- and post-treatment. For this reason, in the present study, treated Class I patients with a similar age range as the Functional appliance patients were used as controls. Although growth patterns are not necessarily the same in Class I and Class II patients, treated Class I patients were the only ethically acceptable control group, as exposing untreated Class II patients to CBCTs would not be possible. Still, using orthodontically treated Class I patients as controls, without treatment of the maxilla-mandibular relationship, would allow the evaluation of the effect of growth alone. Thus, this treated control group was considered as adequate to compare the changes of the volumes of the upper airway after functional appliance treatment.24
Subjects from the Class I group received CBCTs for oral surgery indications (ie, impacted teeth). This is in agreement with the current diagnostic and treatment planning indications for CBCTs at the Section of Orthodontics, Department of Dentistry and Oral Health, Aarhus University.14 By contrast, since the subjects in the Functional appliance group had been treated between 2008 and 2012, they were not subject to the present CBCT indications, but to previous guidelines, where functional appliance treatment was included as an indication for taking CBCTs. However, since 2015, according to the revised diagnostic and treatment planning indications for CBCTs in the department based on more recent evidence, functional appliance treatment is no longer an indication for CBCT imaging.14 Thus, currently it would not be possible to acquire CBCT data for this type of study; this highlights the relevance of the present retrospective study.
The Class I group was matching the Functional appliance group for the baseline characteristics, yet the treatment length was significantly longer in the Class I group compared to the Functional appliance group. The main reason was that some patients in the Functional appliance group were treated only with a functional appliance, whereas all of the patients in the Class I group were treated with fixed appliances. This slightly longer treatment time in the Class I group probably gave room for more growth to happen, thus possibly resulting in a larger airway volume after treatment. Despite this, significantly larger airway volumes in the oropharynx and in the total volume were found in the Functional appliance group after treatment.
Some of the functional appliances used in the study had built-in expansion devices, which might cause some skeletal palatal expansion. In order to evaluate the expansion produced, the pre- and post-treatment palatal dimensions were compared. Although a significant increase in palatal width in the Functional appliance group was observed after treatment, when this was compared to the Class I group, which did not have any active expansion, no statistically significant difference was found. This finding underlines the importance of having a control group. By looking at the Functional appliance group alone, one would erroneously conclude that functional appliances have a significant expansion effect on the palate. Yet, when comparing this to the increase observed in the control group, it is reasonable to believe that most of the expansion was simply related to growth.
In the present study, the Functional appliance group presented initially with a larger overjet and ANB angle than the Class I group. As a consequence, different upper airway volumes might be expected in the two groups. Surprisingly, no differences in the upper airway volumes, except for the VLP, were present before treatment. When the two groups were compared, only the total and the oropharynx volumes displayed a statistically significant increment in the Functional appliance group (Table 6). The observed increment of the oropharynx volume was in agreement with previously reported studies.4,24 A recent literature review concluded that the effects produced by functional appliances were mainly dentoalveolar.25 However, a significant modification of the oropharyngeal airway was found in the current study. One hypothesis could be that the dentoalveolar modifications occurring after functional appliance therapy guide the tongue to a more forward position, thus indirectly enlarging the posterior airway space. Indeed, a forward displacement of the tongue is part of a typical surgical strategy when treatment of sleep disorder breathing is required. In particular, a similar finding was observed in two previous CBCT studies where the effect of functional appliances was compared to a control group; an enlargement of the oropharyngeal volume was reported as well.24,26 To verify that these volume increments would be maintained with time, it would be necessary to have a long-term follow-up. However, no long-term CBCTs are available in this retrospective study, for evident ethical reasons.
One of the limitations of this study was that different types of functional appliances were used, possibly leading to different amounts of skeletal effect. However, advantages in terms of mandibular growth stimulation with one specific functional appliance rather than another could not be confirmed by the literature. Therefore, the variety of appliances used in the present study should not affect the outcomes.27
CONCLUSIONS
An increase in oropharyngeal volume was found after functional appliance treatment in Class II patients, leading to an increase in total volume of the upper airway.
However, the long-term effects of these changes should be considered with caution since no evidence exists that this increase will be maintained with time.
ACKNOWLEDGMENT
We truly acknowledge the editor, associate editor, and the reviewers for their insightful comments and suggestions, which helped to improve the overall quality of our article.
REFERENCES
- 1.Robin P. Glossoptosis due to atresia and hypotrophy of the mandible. Am J Dis Child. 1934;48:541–547. [Google Scholar]
- 2.Clark GT, Arand D, Chung E, Tong D. Effect of anterior mandibular positioning on obstructive sleep apnea. Am Rev Respir Dis. 1993;147:624–629. doi: 10.1164/ajrccm/147.3.624. [DOI] [PubMed] [Google Scholar]
- 3.Antonarakis GS, Kiliaridis S. Short-term anteroposterior treatment effects of functional appliances and extraoral traction on class II malocclusion. A meta-analysis. Angle Orthod. 2007;77:907–914. doi: 10.2319/061706-244. [DOI] [PubMed] [Google Scholar]
- 4.Ozbek MM, Memikoglu TU, Gogen H, Lowe AA, Baspinar E. Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68:327–336. doi: 10.1043/0003-3219(1998)068<0327:OADAFO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Temani P, Jain P, Chaudhary S, Rathee P, Pachori Y, Temani R. Computed tomographic evaluation of three- dimensional changes in pharyngeal airway in class II division 1 patients treated with Twin Block Appliance. J Ind Orthod Soc. 2014;48:439–445. [Google Scholar]
- 6.Kannan A, Sathyanarayana HP, Padmanabhan S. Effect of functional appliances on the airway dimensions in patients with skeletal class II malocclusion: A systematic review. J Orthodont Sci. 2017;6:54–64. doi: 10.4103/jos.JOS_154_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Godt A, Koos B, Hagen H, Goz G. Changes in upper airway width associated with Class II treatments (headgear vs activator) and different growth patterns. Angle Orthod. 2011;81:440–446. doi: 10.2319/090710-525.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warren DW, Spalding P. Dentofacial morphology and breathing: a century of controversy. In: Melsen B, editor. Controversies in Orthodontics. Chicago, IL: Quintessence Publishing; 1990. pp. 45–76. [Google Scholar]
- 9.Baumrind S, Frantz RC. The reliability of head film measurements. 2. Conventional angular and linear measures. Am J Orthod. 1971a;60:505–517. doi: 10.1016/0002-9416(71)90116-3. [DOI] [PubMed] [Google Scholar]
- 10.Baumrind S, Frantz RC. The reliability of head film measurements. 1. Landmark identification. Am J of Orthod. 1971b;60:111–127. doi: 10.1016/0002-9416(71)90028-5. [DOI] [PubMed] [Google Scholar]
- 11.Lenza MG, Lenza MM, Dalstra M, Melsen B, Cattaneo PM. An analysis of different approaches to the assessment of upper airway morphology: a CBCT study. Orthod Craniofac Res. 2010;13:96–105. doi: 10.1111/j.1601-6343.2010.01482.x. [DOI] [PubMed] [Google Scholar]
- 12.Cattaneo PM, Melsen B. The use of cone-beam computed tomography in an orthodontic department in between research and daily clinic. World J Orthod. 2008;9:269–282. [PubMed] [Google Scholar]
- 13.Guijarro-Martinez R, Swennen GR. Cone-beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011;40:1227–1237. doi: 10.1016/j.ijom.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Kapila SD, Nervina JM. CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dentomaxillofac Radiol. 2015;44:20140282. doi: 10.1259/dmfr.20140282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Carlo G, Polimeni A, Melsen B, Cattaneo PM. The relationship between upper airways and craniofacial morphology studied in 3D. A CBCT study. Orthod Craniofac Res. 2015;18:1–11. doi: 10.1111/ocr.12053. [DOI] [PubMed] [Google Scholar]
- 16.Dahlberg G. Standard error and medicine. Acta Genetica et Statistica Medica. 1949;1:313–321. doi: 10.1159/000150653. [DOI] [PubMed] [Google Scholar]
- 17.Haskell JA, McCrillis J, Haskell BS, Scheetz JP, Scarfe WC, Farman AG. Effects of mandibular advancement device (MAD) on airway dimensions assessed with cone-beam computed tomography. Semin Orthod. 2009;15:132–158. [Google Scholar]
- 18.Pillar G, Lavie P. Upper airway in obstructive sleep apnea– controversies continue. J Sleep Res. 2008;17:123–124. doi: 10.1111/j.1365-2869.2008.00668.x. [DOI] [PubMed] [Google Scholar]
- 19.Tso HH, Lee JS, Huang JC, Maki K, Hatcher D, Miller AJ. Evaluation of the human airway using cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:768–776. doi: 10.1016/j.tripleo.2009.05.026. [DOI] [PubMed] [Google Scholar]
- 20.El H, Palomo JM. Measuring the airway in 3 dimensions: a reliability and accuracy study. Am J Orthod Dentofacial Orthop. 2010;137:S50, e1–9, S50–52. doi: 10.1016/j.ajodo.2010.01.014. discussion. [DOI] [PubMed] [Google Scholar]
- 21.Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:468–479. doi: 10.1016/j.ajodo.2007.04.043. [DOI] [PubMed] [Google Scholar]
- 22.Gurani SF, Di Carlo G, Cattaneo PM, Thorn JJ, Pinholt EM. Effect of head and tongue posture on the pharyngeal airway dimensions and morphology in three-dimensional imaging: a systematic review. J Oral Maxillofac Res. 2016;7:e1. doi: 10.5037/jomr.2016.7101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tulloch JF, Phillips C, Koch G, Proffit WR. The effect of early intervention on skeletal pattern in Class II malocclusion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 1997;111:391–400. doi: 10.1016/s0889-5406(97)80021-2. [DOI] [PubMed] [Google Scholar]
- 24.Iwasaki T, Takemoto Y, Inada E, et al. Three-dimensional cone-beam computed tomography analysis of enlargement of the pharyngeal airway by the Herbst appliance. Am J Orthod Dentofacial Orthop. 2014;146:776–785. doi: 10.1016/j.ajodo.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 25.Koretsi V, Zymperdikas VF, Papageorgiou SN, Papadopoulos MA. Treatment effects of removable functional appliances in patients with Class II malocclusion: a systematic review and meta-analysis. Eur J Orthod. 2015;37:418–434. doi: 10.1093/ejo/cju071. [DOI] [PubMed] [Google Scholar]
- 26.Rizk S, Pangrazio Kulbersh V, Al-Qawasmi R. Changes in the oropharyngeal airway of Class II patients treated with the mandibular anterior repositioning appliance. Angle Orthod. 2016;86:955–961. doi: 10.2319/042915-295.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Čirgić E, Kjellberg H, Hansen K. Treatment of large overjet in Angle Class II: division 1 malocclusion with Andresen activators versus prefabricated functional appliances-a multicenter, randomized, controlled trial. Eur J Orthod. 2016;38:516–524. doi: 10.1093/ejo/cjv080. [DOI] [PubMed] [Google Scholar]