Abstract
Equinus contracture is the most common deformity at clubfoot relapse and causes pain and functional limitation. It presents a challenge to the orthopaedic surgeon throughout childhood.
A systematic review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Studies included were: (i) original articles, (ii) investigating management of relapsed idiopathic clubfoot, (iii) with at least a partial study population of primarily equinus deformity, and (iv) a paediatric study population of independent walking age.
Nine studies were included with a total of 163 patients (207 feet). Studies presented five management paradigms: gastrocnemius-soleus complex release, extensive posterior soft tissue and joint release, anterior distal tibial hemi-epiphysiodesis, distal tibial osteotomy, and circular frame distraction.
All approaches reported success in at least one of our selected outcome domains: plantigrade status, range of motion, clinical outcome scores, functional status, radiographic outcomes, patient-reported outcomes, and complications. Younger children tend to be managed with soft tissue release while older children tend to require more extensive bone/joint procedures. Relapse in surgically treated feet is harder to treat.
Comparison across treatment approaches is limited by the small size and low evidence level of the literature, as well as a lack of consistent outcome reporting. It is therefore not possible to recommend any one treatment option in any age group.
This review highlights the need for a validated core outcome set to enable high-quality research into the management of equinus deformity.
Cite this article: EFORT Open Rev 2021;6:354-363. DOI: 10.1302/2058-5241.6.200110
Keywords: clubfoot, CTEV, equinus, management, recurrent, relapse
Introduction
Congenital talipes equinovarus (CTEV) is the most common congenital limb deformity, with an estimated incidence of 1–2 in 1,000 live births.1–4 As of the late 20th Century, the gold-standard treatment has comprised serial manipulation and casting according to the Ponseti method.1,5,6 Primary correction rates are very high,7–9 and this method is superior to surgical first-line management.10,11
While the Ponseti method provides predictable correction, there is no universally accepted definition of a corrected foot and it is assumed rather than proven that all treated feet are corrected fully, without residual equinus deformity. Despite acknowledged excellent results of early treatment, management of CTEV continues throughout childhood and is not without its challenges.1,5 Relapse or recurrence of the deformity is a known and significant occurrence.12 Relapse following Ponseti treatment has mostly been associated with non-adherence to the post-casting bracing protocol.13 It is recognized that a foot with residual deformity will be difficult to brace and hence compliance will be low.14 Poor evertor activity of the corrected foot has also been reported as a predictive factor for relapse.15,16
The prospect of relapsed deformity raises the question of how to best manage affected individuals. Relapse may include all four components of the clubfoot deformity and may present at any time following primary correction.6,17 Recurrent deformity in a surgically treated clubfoot presents an even greater challenge due to joint stiffness and tissue scarring18 but may be improved by use of the Ponseti technique.
Equinus deformity is reported as the most common deformity at relapse,19 and is a cause of pain and functional limitation. Stouten et al reported that isolated equinus deformity accounted for 40% of all observed relapses, with a further 36% displaying some element of equinus.20 In a study assessing correlations between foot function and perceived disability, McCahill et al found that perceived disability was associated with equinus deformity, hindfoot deformity in coronal and sagittal planes, and medial forefoot pressure gait parameters.21 Residual or recurrent deformity of the hindfoot causes significant disability. It is challenging to correct and also to maintain the correction.
The approach to isolated equinus relapse in the young child will most commonly involve repeat serial casting.22,23 Those in whom serial casting is not sufficient present a challenge for management up to the age of skeletal maturity.
In addition to casting, numerous surgical approaches have been described in the literature, including repeat Achilles tenotomy, limited-to-extensive soft tissue release, various corrective osteotomies, and gradual soft tissue and/or callus distraction with circular frame devices with or without a concurrent osteotomy.22,24–29 Selection of approach depends on age, static and dynamic findings on clinical examination, imaging, treatment chronology, and surgeon’s preference.
In this systematic review, we will synthesize the current evidence available regarding the treatment of isolated equinus deformity in idiopathic clubfoot in children of walking age.
Methods
Search strategy
A systematic literature search was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.30 It was prospectively registered on PROSPERO (registration number: CRD42020186307).
PubMed, EMBASE, and MEDLINE databases were searched from the beginning of their records to August 2020. The search terms were: “CTEV”, “congenital talipes”, “equinus”, “clubfoot”, “relapse*”, “recurrent*”, “residual”, “management”, “treatment”, “correct*”, “surgery”. These terms were combined with AND/OR statements and filtered for ages up to 18 years to optimize results. Articles of all levels of evidence were included. Sources of grey literature and reference lists of identified relevant articles were also consulted.
Eligibility criteria
The inclusion criteria were: published original articles; studies of all methodologies; studies investigating management of relapsed CTEV; at least a partial study population of relapsed isolated equinus deformity; and a paediatric study population of independent walking age. The exclusion criteria were: studies of non-idiopathic clubfoot (e.g. neurogenic deformity, arthrogryposis); studies investigating primary (i.e. first-presentation) CTEV; studies solely investigating CTEV in children of non-walking age; studies solely investigating neglected CTEV; studies solely investigating multi-dimensional (i.e. not isolated equinus) CTEV deformities; and single case reports.
Two authors (DM and MR) reviewed titles for all articles identified by the literature search against the inclusion and exclusion criteria, followed by a review of abstracts, full texts and reference lists. In any instances of disagreement, the senior author (YG) was consulted and disagreements were resolved in consensus.
Data extraction and analysis
Data extracted for analysis were: year and country of publication; number of participants; participant age; follow-up time; previous treatments; intervention trialled; and treatment outcomes. Selected outcomes collected were: plantigrade status; ankle range of motion (ROM); radiographic outcomes; clinical scoring outcomes; functional outcomes; patient-reported outcome measures (PROMs); and complications (Table 1). Articles were categorized by trial intervention. Data were extracted into a standardized collection form using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). Bias assessment of case series was carried out in accordance with published guidance from Murad and colleagues,31 and assessment of non-randomized interventional studies was carried out using the ROBINS-I tool.32
Table 1.
Systematic review defined outcome groups
| Outcome groups | Notes |
|---|---|
| Plantigrade status | Actual reported plantigrade status where available, otherwise ankle dorsiflexion ≥ 10° taken as plantigrade. |
| Ankle ROM | Reported as change in mean pre and post intervention. Dorsiflexion range most relevant in management of equinus. |
| Radiographic outcomes | Reported as change in mean angle pre and post intervention. All reported radiographic angles are included. |
| Clinical scoring outcomes | AOFAS score reported by one study.41 Modified Clubfoot Outcome Grading System reported by one study.33 |
| Functional outcomes | Across all studies: very few functional outcomes reported. |
| Patient-reported outcomes | Pain and patient or parent satisfaction are main PROMs reported. |
| Complications | All reported complications included. |
Notes. ROM, range of motion; AOFAS, American Orthopedic Foot and Ankle Society.
Results
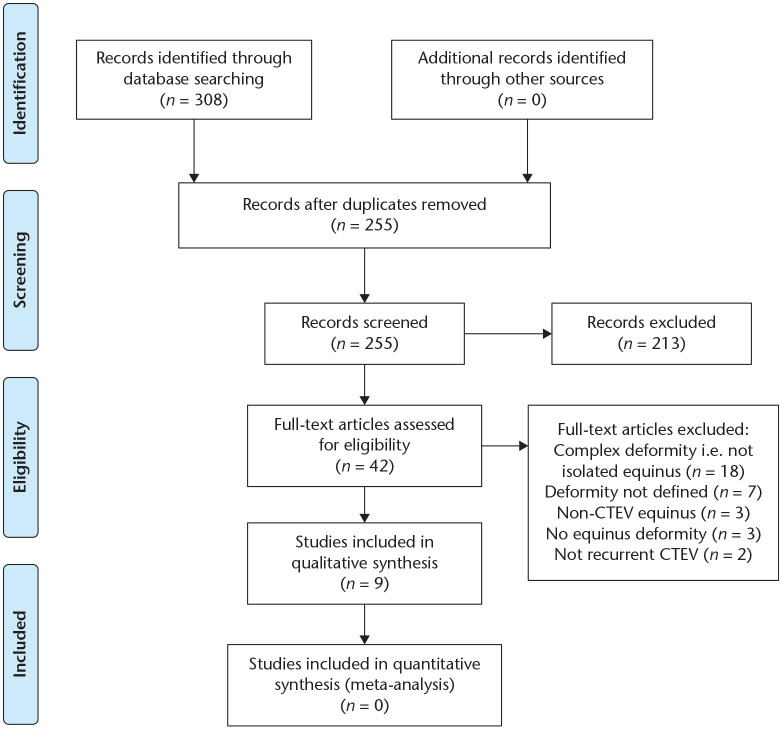
The literature search resulted in a total of 308 results. The PRISMA flow chart of study selection is presented in Fig. 1. Nine studies33–41 met the inclusion criteria and were included for analysis. All included studies were retrospective case series.
Fig. 1.
Flow chart of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) process.
Note. CTEV, congenital talipes equinovarus.
Patient demographics
The nine included studies33–41 contributed a total of 163 patients with 207 clubfeet. One-hundred and three (63.2%) patients were male and 52 (31.9%) were female. Eight patients (4.9%) did not have their gender reported.30 Mean patient ages of the studies ranged from 2.4 to 11.3 years.
Primary CTEV treatment
Five studies included only surgically-corrected feet33–37 and three reports included only Ponseti-corrected feet.38–40 Refai et al reported a mixed cohort of feet corrected by the Ponseti method and a surgical posteromedial release.41
Follow-up
Mean follow-up periods varied from 1.2 to 5.0 years. None of the included studies followed patients to skeletal maturity. Follow-up times are presented in Table 2.
Table 2.
Study protocols and demographics
| Study type | Treatment protocol | Patient numbers (feet) | Previous treatments | Mean age (years) | Mean follow-up (years) | |
|---|---|---|---|---|---|---|
| Park et al. Foot Ankle Int 2012.39 | Retrospective case series | Vulpius procedure (distal gastrocnemius + soleus release) | 17 (22)14 male, 3 female | Ponseti method | 2.4 (range 0.5–4.3) |
4.0 |
| Shah et al. J Pediatr Orthop B 2019.40 | Retrospective case series | Repeat Ponseti casting Tendo-Achilles lengthening |
44 (63) 36 male, 8 female |
Ponseti method | 3.2 (range 1.0–5.5) |
2.8 |
| Jauregui et al. J Pediatr Orthop 2017.38 | Retrospective case series | Repeat Ponseti casting Posterior capsulotomy |
16 (20) 3 male, 13 female |
Ponseti method | 6.1 (range 3–9) |
5.0 |
| Al-Aubaidi et al. J Pediatr Orthop 2011.34 | Retrospective case series | ADTH | 25 (31) 16 male, 9 female |
EPR | 7.0 | 2.2 |
| Zargarbashi et al. J Foot Ank Surg 2020.37 | Retrospective case series | ADTH | 8 (9) 4 male, 4 female |
EPR | 7.3 (range 5–12) |
1.2 |
| Napiontek and Nazar. J Pediatr Orthop 1994.36 | Retrospective case series | DTO ± K-wires | 14 (19) total 12 feet with equinus deformity 5 male, 4 female |
Previous surgical management | 7.6 (range 2.1–17.0) |
4.3 |
| Refai et al. Clin Orthop Relat Res 2012.41 | Retrospective case series | Repeat Ponseti casting OR posterior release Ilizarov frame Post-frame K-wires + cast |
18 (19) 12 male, 6 female |
Ponseti (9 feet) Posteromedial release (10 feet) |
8 (range 4–15) |
4.5 |
| Segev et al. J Orthop Surg (Hong Kong) 2008.33 | Retrospective case series | DTO + Iizarov frame | 13 (14) Eight feet idiopathic CTEV Six feet neurogenic Patient gender not reported |
Eight idiopathic feet had previous surgery (EPR) Four had Evans procedure |
11.2 (range 8.0–15.5 in idiopathic group) |
2.6 |
| Ebert et al. J Pediatr Orthop 2020.35 | Retrospective case series | ADTH | 18 (23) 13 male, 5 female |
All previously surgically treated Range of operations |
11.3 (range 8.3–12.9) |
3.7 |
Notes. ADTH, anterior distal tibial hemi-epiphysiodesis; CTEV, congenital talipes equinovarus; DTO, distal tibial osteotomy; EPR, extensive posteromedial release.
Treatment method
The nine studies33–41 that fitted the inclusion criteria reported five treatment options for equinus in clubfoot. Two studies performed soft tissue release of the gastrocnemius-soleus complex (GSC), i.e. tendon Achilles lengthening (TAL) or Vulpius procedure.39,40 One study also performed posterior capsulotomy.38 Two studies performed distraction via a circular frame (one with distal tibial osteotomy [DTO] but neither with hindfoot osteotomy),33,41 one further study utilized DTO,35 and three studies performed anterior distal tibial hemi-epiphysiodesis (ADTH) using either 8-plates or staples.34,35,37
Protocols by Jauregui et al, Shah et al, and Refai et al,38,40,41 state the use of serial casting as initial management of relapsed feet; other protocols do not state whether serial casting was utilized prior to the investigational intervention.
The procedures used in each study showed correlation with age (Table 2). Soft tissue procedures were utilized in the younger patients (mean ages 2.4–6.1 years, range 0.5–9.3 years). ADTH and DTO were utilized in patients around seven years old in two studies, and older children (mean age 11.3 years, range 10.2–12.9 years) in another. Circular frames were preferred in older children (mean ages 8.0 and 11.2 years, range 4.0–15.5 years).
Risk of bias was found to be high in two studies36,38 and medium in the remaining seven studies (Table 3).
Table 3.
Bias assessment according to Murad et al31
| Selection | Ascertainment | Causality | Reporting | Risk of bias | ||
|---|---|---|---|---|---|---|
| Do selected patients represent total experience of the clinician’s practise? | Was exposure adequately ascertained? | Was the outcome adequately ascertained? | Was follow-up long enough for outcomes to occur? | Is there sufficient detail for findings to be relevant/applicable to others? | ||
| Al-Aubaidi et al. J Pediatr Orthop 2011.34 | Yes | Yes | Yes | No | Yes | Medium |
| Jauregui et al. J Pediatr Orthop 2017.38 | No | Yes | Yes | No | Yes | High |
| Napiontek and Nazar. J Pediatr Orthop 1994.36 | No | Yes | No | No | Yes | High |
| Park et al. Foot Ankle Int 2012.39 | Yes | Yes | Yes | No | Yes | Medium |
| Refai et al. Clin Orthop Relat Res 2012.41 | Yes | Yes | Yes | No | Yes | Medium |
| Segev et al. J Orthop Surg (Hong Kong) 2008.33 | Yes | Yes | Yes | No | Yes | Medium |
| Shah et al. J Pediatr Orthop B 2019.40 | Yes | Yes | Yes | No | Yes | Medium |
| Ebert et al. J Pediatr Orthop 2020.35 | Yes | Yes | Yes | No | Yes | Medium |
| Zargarbashi et al. J Foot Ank Surg 2020.37 | No | Yes | Yes | No | Yes | Medium |
Notes. Performed according to criteria from Murad, Mohammad Hassan, Shahnaz Sultan, Samir Haffar, and Fateh Bazerbachi. Methodological quality and synthesis of case series and case reports. Evidence-Based Med 2018;23:60–63. https://doi.org/10.1136/bmjebm-2017-110853.
Treatment outcome
Various outcome measures were chosen by the studies with no single outcome reported in all studies. All studies reported success in at least one of our defined outcomes (Table 1). Outcomes are presented in Table 4.
Table 4.
Results presented by defined outcome group
| Treatment protocol | % feet corrected to plantigrade | ROM | Radiographic | Clinical scoring outcomes | Functional | Pain | Satisfaction | Complications | |
|---|---|---|---|---|---|---|---|---|---|
| Park et al. Foot Ankle Int 2012.39 |
Vulpius procedure (distal gastrocnemius + soleus release) | 100% dorsiflexion 10–25° at last follow-up Plantigrade per se not reported |
Mean improved ankle dorsiflexion –0.7° to +14.5° | Improved LAT TalCA: 18.6° to 26.9° | Not reported | Not reported | Not reported | Not reported | No complications Five feet required further correction |
| Shah et al. J Pediatr Orthop B 2019.40 |
Repeat Ponseti casting Tendo-Achilles lengthening |
73% [without need for posterior release] | Not reported | Not reported | Not reported | Not reported | Successful outcome: pain-free, plantigrade foot, without the need for extensive soft tissue release in 73% | Not reported | Relapse in 27% Non-adherence to bracing in 11% |
| Jauregui et al. J Pediatr Orthop 2017.38 |
Repeat Ponseti casting Posterior capsulotomy |
Not reported | Mean improved ankle dorsiflexion –6.5° to +8.3° Mean change plantar flexion 37.5° to 37.4° |
Improved LAT TibCA: 98.9° to 63.7° No improvement in other metrics (AP and LAT TMT1) |
Not reported | Not reported | Not reported | 80% parents satisfied atone year Reasons for dissatisfaction: pain, functional limit Scoring tool not reported |
Not reported |
| Al-Aubaidi et al. J Pediatr Orthop 2011.34 |
ADTH | 97% dorsiflexion 0–10° Plantigrade per se not reported |
Mean improved ankle dorsiflexion +2.5° to +4.5° | Improved ADTA: 85° to 70° | Not reported | Not reported | Not reported | Not reported | Misplacement of metalwork Some malalignment |
| Zargarbashi et al. J Foot Ank Surg 2020.37 |
ADTH | 89% | Mean improved ankle dorsiflexion –27.7° to –2.2° | Improved ADTA: 86.3° to 69.0° | Not reported | Not reported | Not reported | Not reported | None |
| Napiontek and Nazar. J Pediatr Orthop 1994.36 |
DTO ± K-wires | 33% | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Relapsed deformity in 7/9 patients. |
| Refai et al. Clin Orthop Relat Res 2012.41 |
Repeat Ponseti casting OR posterior release Ilizarov frame Post-frame K-wires + cast |
84% | Not reported | Improved AP TalCA: 5° to 30° Improved AP TMT1: 32° to 9.5° Improved LAT CMT1: 111° to 136° |
Mean AOFAS score improved (57 to 81) Very wide range (32–71 pre-op, 32–91 post-op) Mean AOFAS score improved (57 to 81) Very wide range (32–71 pre-op, 32–91 post-op) |
16 of 19 feet pain-free at last follow-up | Not reported | 19/19 feet pin infections 4 flat-top talus 4 temporary foot stiffness 8 toe flexion contracture needing PC release Recurrence of deformity in 2 pts (age 12 and 15) |
|
| Segev et al. J Orthop Surg (Hong Kong) 2008.33 | DTO + Iizarov frame | 71% | No improvement | Improved AP TMT1: 42.6° to 8.6° (idiopathic patients only) | Used modified clubfoot outcome grading system 44
Mean improvement of 52.1 to 98.9 |
No improvement | No improvement | Improvement, related to appearance | 6/8 feet pin tract infection 4/8 toe flexion contracture |
| Ebert et al. J Pediatr Orthop 2020.35 | ADTH | 100% | Mean improved ankle dorsiflexion –3.3° to +6.1° | Improved ADTA: 87.5° to 75.8° | Not reported | Not reported | Not reported | Not reported | One loose screw requiring surgery for replacement |
Notes. ADTA, anterior distal tibial angle; ADTH, anterior distal tibial hemi-epiphysiodesis; AOFAS, American Orthopedic Foot and Ankle Society; AP, anteroposterior; CMT1, calcaneo-first metatarsal angle; DTO, distal tibial osteotomy; LAT, lateral; ROM, range of motion; TalCA, talocalcaneal angle; TibCA, tibiocalcaneal angle; TMT1, talo-first metatarsal angle.
Achievement of a plantigrade foot was reported in eight out of nine articles,33–37,38–41 with success rates from 33–100%.
Improvements in ROM were directly reported with five treatment protocols. Soft tissue release of the GSC resulted in a change from –0.7° to +14.5° dorsiflexion at final follow-up in one study.39 The other did not report any direct ROM metrics, but reported a ‘pain-free, plantigrade foot, without the need for extensive soft tissue release’.40 Posterior capsulotomy improved mean ankle dorsiflexion from –6.5° pre operation to +9.7° post operation, and +8.3° at final follow-up.38
ADTH resulted in a mean improvement in ankle dorsiflexion of 12.3° (range 2.4–14.8°) across three studies.34,35,37
Gradual distraction using circular frames delivered mixed results. One study reported an overall improvement in patients’ American Orthopedic Foot and Ankle Society (AOFAS) score, which assesses function and alignment.41 However, in the protocol combined with DTO, no improvement in ROM or functional metrics after intervention was reported.33 The study examining DTO alone did not report any ROM or functional metrics.36
Assessment of radiographic outcomes
Seven studies33–35,37–39,41 reported improved radiographic outcomes (Table 4). Vulpius procedure demonstrated an improvement in the lateral (LAT) talocalcaneal angle (TalCA) from 18.6° to 26.9°.39 The other study examining release of the GSC did not report radiographic outcomes.40 Posterior capsulotomy delivered mixed radiographic results with a significant improvement in mean LAT tibiocalcaneal angle (TibCA) from 98.9° to 63.7°, but no improvement in anteroposterior (AP) or LAT talo-first metatarsal angle (TMT1).38
ADTH demonstrated an improvement in anterior distal tibial angle (ADTA) from 85° to 70° in one study,34 87.5° to 75.8° in a second study,35 and 86.3° to 69.0° in a third.37
Gradual distraction using circular frame improved radiographic outcome measures in both studies it was used in.33,41 In the protocol by Refai et al, the mean AP TalCA improved from 5° preoperatively to 30° at last follow-up; the mean AP TMT1 improved from 32° to 9.5°; and the LAT calcaneo-first metatarsal angle (CMT1) improved from 111° to 136°.41 In the study by Segev et al, which combined circular frame distraction with DTO, the mean AP TMT1 improved from 42.6° to 8.6° in the idiopathic CTEV cohort.33
Osteotomy protocols had mixed reporting of radiographic outcomes: one study reported an improvement,33 while one did not report any radiographic outcomes.36
Assessment of PROMs and patient satisfaction
The PROMs reported in the included studies were presence of pain and satisfaction with treatment. The only protocol which reported clear reduction in pain scores was repeat TAL lengthening.40 Gradual distraction using circular frame showed improvement in pain scoring in one study,41 but no improvement in the other.33 No other protocols provided information on presence of pain before or after intervention.
Patient or parent satisfaction was only reported in two studies.33,38 Posterior capsulotomy resulted in an 80% parent satisfaction rate one year post intervention.38 While this study did not directly report pain-related outcomes, the authors report that some of the parents’ dissatisfaction is related to the presence of pain. Segev and colleagues’ DTO with the use of Ilizarov frame produced a statistically significant improvement in parent satisfaction according to the Modified Clubfoot Outcome Grading System.33,42
Assessment of complications
The most complications were reported in protocols utilizing circular frame fixation, with the most common being pin tract infections and toe flexion contractures requiring percutaneous release (Table 4).33,41 Complications were also reported following ADTH, including loose screws, misplaced metalwork, and joint malalignment.34,35 Relapse or deformity requiring further correction were identified as complications in both articles reporting soft tissue release of the GSC.39,40 The studies of posterior capsulotomy and DTO with K-wire fixation did not report presence or absence of complications.36,38
Comparison by previous management
Two studies38,39 reported outcomes of their intervention in feet previously treated only with the Ponseti method. They achieved a weighted mean improvement in dorsiflexion of 15.0°. Three studies reported outcomes in feet previously managed via surgical intervention.33,34,37 They achieved a weighted mean improvement in dorsiflexion of 4.1°.
Discussion
Equinus is the most common deformity seen in the relapsed clubfoot. It can result from residual or recurrent deformity, and can present following Ponseti correction or after surgical intervention. Hindfoot equinus in the sagittal plane may be associated with a loss of eversion ability at the subtalar joint and the appearance of varus in the coronal plane. Forefoot equinus may increase the overall appearance of hindfoot equinus but the two elements must be considered separately. Hindfoot equinus poses a treatment challenge with no consensus regarding the best protocol for management in the walking-age child. It is important to decide not only whether to intervene surgically but also with what method. This systematic review looks at treatment methods documented in the literature and their respective outcomes.
Five approaches to treatment were identified from the literature: A repeat Ponseti treatment including minor soft tissue release to the Achilles tendon or GSC, extensive posterior soft tissue release, ADTH, DTO, and gradual distraction with circular external fixator. Three studies reported pre-operative serial casting.38,40,41
TAL in the relapsed clubfoot demonstrated success according to the authors’ definition in 73% of cases,40 and GSC release delivered improvements in ROM and radiographic measurements in the other study performed.39 Both studies reported serial casting prior to the surgery which is an important stage in correcting the equinus deformity. The subtalar abduction resulting in a lateral position of the anterior tuberosity of the calcaneum allows a better superior migration and equinus correction. The mean follow-up periods of 2.8 and 4.0 years are relatively short, and up to 27% of the study population relapsed within each follow-up period. Given the young age of the study populations39,40 there is a high probability of further recurrence before skeletal maturity as shown in other studies.24
Extensive posterior soft tissue release achieved improvement in ROM.38 It also demonstrated good radiological outcomes, good parent satisfaction, and very few complications after mean follow-up period of five years. This approach was implemented in younger children (mean age 6.1 years, range 3–9 years); but a five-year follow-up period leaves the possibility of future relapse. From previous studies of long-term outcomes following soft tissue release, it is known that a significant proportion of these feet are painful and stiff.5,43 These outcomes informed the shift towards the Ponseti method of treatment.
Circular frame application delivered qualified success; however, results were not consistent across study protocols. Improvement was documented in radiographic outcomes, and, in one study, the aggregate AOFAS score.33,41 There was no reported improvement in function, and there was discrepancy in pain improvement. This approach had the highest reported rate of complications; mostly related to pin track infections which, although uncomfortable, may not have compromised the final outcome. The ages of children treated with this method were older than those treated using soft tissue methods (weighted mean age 9.3 years across both studies). The choice of the AOFAS scale as an outcome measure has been questioned regarding its validity and reliability in paediatric clinical practice.44,45
Three studies examined ADTH, with all reporting success in reaching a plantigrade foot.34,35,37 All three reported improvements in ankle dorsiflexion and radiographic outcomes (Table 4). The large increase in dorsiflexion reported in Zargarbashi and colleagues’ study (25.5° vs. 2.0° and 8.8° in the other two studies) likely reflects worse starting equinus in the study population. While plantigrade status was reported at last follow-up in each study, only follow-up to skeletal maturity would be able to determine whether this correction is sustainable. No information was collected on function or PROMs in any study, and there were several complications associated with this approach.
DTO was reported in two studies with contradicting results.33,36 The first study reported poor outcomes: seven out of nine patients relapsed within the mean follow-up period of 4.3 years.36 No reporting was provided for our other key defined outcomes; any broader analysis of the success of the protocol is therefore limited. The second study reported improved radiographic measurement and satisfaction with no quantifiable clinical improvement.33 Both ADTH and DTO attempt to correct the equinus deformity at a fulcrum above the lateral process of the calcaneus, which thus results in a relative anterior translation of the foot which may affect push off.
It is pertinent to discuss treatment outcomes according to patient age. Vulpius39 and TAL40 procedures delivered good outcomes in the youngest patient groups identified, with the former achieving significant improvements in ankle dorsiflexion and LAT TalCA in patients with a mean age of 2.4 years, and the latter achieving a plantigrade foot in 73% of cases with a mean age of 3.2 years. The outcomes of posterior capsulotomy in a group with a mean age of 6.1 years were mixed, with an improvement in LAT TibCA but no significant changes in AP TMT1, LAT TMT1, or ROM.38 It was not reported whether the posterior capsulotomy followed previous procedures to the Achilles tendon complex and whether this contributed to the failure to achieve improvement in ROM.
ADTH,34,37 DTO,36 and circular frame distraction41 were investigated in patients aged 7–8 years. In this age range, ADTH resulted in an improved ADTA (mean improvement 16.2° from the two studies in this age group) and reliable correction to plantigrade,33,37 while relapse occurred in seven of nine patients treated with DTO.36 Circular frame distraction also delivered good results with improvements in AOFAS score, and in AP TalCA, AP TMT1, and LAT CMT1. Recurrence was noted in only two of 18 patients.41 However, direct comparison between circular frame and ADTH in this age group is difficult as the studies document crude reporting of a plantigrade foot but have no other outcomes in common.
DTO with circular frame distraction in an older patient group (mean age 11.2 years) achieved an improved AP TMT1 and improved patient satisfaction with relation to appearance, but no improvements in ROM or pain.33 In the same age group, Ebert et al investigated ADTH and reported better outcomes in ROM with fewer complications.35 Both studies report improvements in radiographic outcomes, but direct comparison is not possible because different metrics are used.33,35
We can also compare outcomes in patients previously treated using the Ponseti method only, versus those previously treated via surgical methods (including extensive posteromedial release). Due to variability in outcome reporting, we can only compare ROM data. Interventions in feet treated previously with only the Ponseti method achieved greater dorsiflexion (weighted mean 15.0°) following post-relapse intervention compared to feet previously treated with surgery (weighted mean 4.1°).
Endorsement of any one of these approaches is limited by the body of literature available. There is no agreed-upon set of core outcomes for assessing management of clubfoot in the walking-age child. Furthermore, reporting of outcomes in each of our key domains is variable, with only one study reporting on all six.33 It is therefore difficult to make comparisons across studies. While radiographic outcomes are relatively common, different angles are used by different authors: TalCA, TMT1, CMT1, ADTA, and TibCA are all reported. Furthermore, studies reporting on presence of pain had mean follow-up periods of 3.2 and 4.5 years40,41 and cannot comment on the likelihood of significant or chronic pain in the medium to long term as the child approaches adolescence or adulthood.
It is evident from the literature that the treatment of equinus in clubfoot is ongoing throughout childhood. The acknowledged ideal management is meticulous primary correction adhering to the Ponseti method with the aim of avoiding residual deformity which leads to an early cascade of battling with the deformity.
Following a complete primary correction and a strict foot abduction brace regime it is our belief that every sign of relapse should be identified and addressed immediately with repeated casting according to the same principles. Management of the residual deformity following casting utilizes various degrees of posterior soft tissue release in the younger age group and osteotomies, distraction and hemi-epiphysiodesis in the older age group. The approaches reported in this review present variable outcomes over a short follow-up period and thus do not allow us to endorse any one treatment philosophy. A validated core outcome set (COS) for CTEV as well as randomized controlled trials with sufficient follow-up are much-needed next steps in order to decide on the best surgical treatment for equinus at every age.
Strengths and limitations
This is the first available systematic review focusing on this challenging clinical question that paediatric orthopaedic surgeons face frequently in their practice. The strengths of this review are its relevance, broad inclusion criteria, and strict methodology. This review is limited mainly by the small size and low level of evidence of the available literature. In addition, variability in reported outcomes, patient age, and follow-up period limit interpretation and comparison of results across studies.
Conclusions
Equinus deformity following clubfoot correction poses an ongoing treatment challenge. The main identifiable trend from our review is a tendency towards use of soft tissue procedures in younger patients and more extensive procedures in older children, and greater success in feet that were previously treated with the Ponseti method compared with those previously treated surgically. There is no clear advantage to any of the reported methods. The variability of outcomes and follow-up time in the reported studies hinders appropriate comparison and analysis. A much-anticipated COS will allow high-quality research into the best way to manage equinus deformity in clubfoot.
Footnotes
ICMJE Conflict of interest statement: DE reports lecturing expenses from Biomarin and royalties from OUP, from Oxford University Press, outside the submitted work.
The other authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Gibbons PJ, Gray K. Update on clubfoot. J Paediatr Child Health 2013;49:E434–E437. [DOI] [PubMed] [Google Scholar]
- 2. Dobbs MB, Gurnett CA. Update on clubfoot: etiology and treatment. Clin Orthop Relat Res 2009;467:1146–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Smythe T, Kuper H, Macleod D, Foster A, Lavy C. Birth prevalence of congenital talipes equinovarus in low- and middle-income countries: a systematic review and meta-analysis. Trop Med Int Health 2017;22:269–285. [DOI] [PubMed] [Google Scholar]
- 4. Chen C, Kaushal N, Scher DM, Doyle SM, Blanco JS, Dodwell ER. Clubfoot etiology: a meta-analysis and systematic review of observational and randomized trials. J Pediatr Orthop 2018;38:e462–e469. [DOI] [PubMed] [Google Scholar]
- 5. Ponseti I, Smoley E. Congenital clubfoot: the results of treatment. J Bone Joint Surg 1963;45:261–276. [Google Scholar]
- 6. Gelfer Y, Wientroub S, Hughes K, Fontalis A, Eastwood DM. Congenital talipes equinovarus: a systematic review of relapse as a primary outcome of the Ponseti method. Bone Joint J 2019;101-B:639–645. [DOI] [PubMed] [Google Scholar]
- 7. Gelfer Y, Dunkley M, Jackson D, et al. Evertor muscle activity as a predictor of the mid-term outcome following treatment of the idiopathic and non-idiopathic clubfoot. Bone Joint J 2014;96-B:1264–1268. [DOI] [PubMed] [Google Scholar]
- 8. Dunkley M, Gelfer Y, Jackson D, et al. Mid-term results of a physiotherapist-led Ponseti service for the management of non-idiopathic and idiopathic clubfoot. J Child Orthop 2015;9:183–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gelfer Y, Hughes KP, Fontalis A, Wientroub S, Eastwood DM. A systematic review of reported outcomes following Ponseti correction of idiopathic club foot. Bone Jt Open 2020;1:457–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cooper DM, Dietz FR. Treatment of idiopathic clubfoot: a thirty-year follow-up note. J Bone Joint Surg Am 1995;77:1477–1489. [DOI] [PubMed] [Google Scholar]
- 11. Smith PA, Kuo KN, Graf AN, et al. Long-term results of comprehensive clubfoot release versus the Ponseti method: which is better? Clin Orthop Relat Res 2014;472:1281–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ponseti IV. Relapsing clubfoot: causes, prevention, and treatment. Iowa Orthop J 2002;22:55–56. [PMC free article] [PubMed] [Google Scholar]
- 13. Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am 2004;86:22–27. [DOI] [PubMed] [Google Scholar]
- 14. Hemo Y, Segev E, Yavor A, Ovadia D, Wientroub S, Hayek S. The influence of brace type on the success rate of the Ponseti treatment protocol for idiopathic clubfoot. J Child Orthop 2011;5:115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Eamsobhana P, Kongwachirapaitoon P, Kaewpornsawan K. Evertor muscle activity as a predictor for recurrence in idiopathic clubfoot. Eur J Orthop Surg Traumatol 2017;27:1005–1009. [DOI] [PubMed] [Google Scholar]
- 16. Little Z, Yeo A, Gelfer Y. Poor evertor muscle activity is a predictor of recurrence in idiopathic clubfoot treated by the Ponseti method: a prospective longitudinal study with a 5-year follow-up. J Pediatr Orthop 2019;39:e467–e471. [DOI] [PubMed] [Google Scholar]
- 17. Jowett CR, Morcuende JA, Ramachandran M. Management of congenital talipes equinovarus using the Ponseti method: a systematic review. J Bone Joint Surg Br 2011;93:1160–1164. [DOI] [PubMed] [Google Scholar]
- 18. Mehrafshan M, Rampal V, Seringe R, Wicart P. Recurrent club-foot deformity following previous soft-tissue release: mid-term outcome after revision surgery. J Bone Joint Surg Br 2009;91:949–954. [DOI] [PubMed] [Google Scholar]
- 19. Chand S, Mehtani A, Sud A, Prakash J, Sinha A, Agnihotri A. Relapse following use of Ponseti method in idiopathic clubfoot. J Child Orthop 2018;12:566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stouten JH, Besselaar AT, Van Der Steen MCM. Identification and treatment of residual and relapsed idiopathic clubfoot in 88 children. Acta Orthop 2018;89:448–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McCahill JL, Stebbins J, Harlaar J, Prescott R, Theologis T, Lavy C. Foot function during gait and parental perceived outcome in older children with symptomatic club foot deformity. Bone Jt Open 2020;1:384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hosseinzadeh P, Kelly DM, Zionts LE. Management of the relapsed clubfoot following treatment using the Ponseti method. J Am Acad Orthop Surg 2017;25:195–203. [DOI] [PubMed] [Google Scholar]
- 23. Hosseinzadeh P, Kiebzak GM, Dolan L, Zionts LE, Morcuende J. Management of clubfoot relapses with the Ponseti method: results of a survey of the POSNA members, 2017. http://links.lww.com/BPO/A98 (date last accessed 21 September 2020). [DOI] [PubMed]
- 24. Eidelman M, Kotlarsky P, Herzenberg JE. Treatment of relapsed, residual and neglected clubfoot: adjunctive surgery. J Child Orthop 2019;13:293–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tripathy SK, Saini R, Sudes P, et al. Application of the Ponseti principle for deformity correction in neglected and relapsed clubfoot using the Ilizarov fixator. J Pediatr Orthop B 2011;20:26–32. [DOI] [PubMed] [Google Scholar]
- 26. Souchet P, Ilharreborde B, Fitoussi F, et al. Calcaneal derotation osteotomy for clubfoot revision surgery. J Pediatr Orthop B 2007;16:209–213. [DOI] [PubMed] [Google Scholar]
- 27. Hassan FOA, Jabaiti S, El tamimi T. Complete subtalar release for older children who had recurrent clubfoot deformity. Foot Ankle Surg 2010;16:38–44. [DOI] [PubMed] [Google Scholar]
- 28. Ferreira RC, Costa MT, Frizzo GG, Santin RAL. Correction of severe recurrent clubfoot using a simplified setting of the Ilizarov device. Foot Ankle Int 2007;28:557–568. [DOI] [PubMed] [Google Scholar]
- 29. Digge V, Desai J, Das S. Expanded age indication for Ponseti method for correction of congenital idiopathic talipes equinovarus: a systematic review. J Foot Ankle Surg 2018;57:155–158. [DOI] [PubMed] [Google Scholar]
- 30. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med 2018;23:60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Segev E, Ezra E, Yaniv M, Wientroub S, Hemo Y. V osteotomy and Ilizarov technique for residual idiopathic or neurogenic clubfeet. J Orthop Surg (Hong Kong) 2008;16:215–219. [DOI] [PubMed] [Google Scholar]
- 34. Al-Aubaidi Z, Lundgaard B, Pedersen NW. Anterior distal tibial epiphysiodesis for the treatment of recurrent equinus deformity after surgical treatment of clubfeet. J Pediatr Orthop 2011;31:716–720. [DOI] [PubMed] [Google Scholar]
- 35. Ebert N, Ballhause TM, Babin K, et al. Correction of recurrent equinus deformity in surgically treated clubfeet by anterior distal tibial hemiepiphysiodesis. J Pediatr Orthop 2020;40:520–525. [DOI] [PubMed] [Google Scholar]
- 36. Napiontek M, Nazar J. Tibial osteotomy as a salvage procedure in the treatment of congenital talipes equinovarus. J Pediatr Orthop 1994;14:763–767. [DOI] [PubMed] [Google Scholar]
- 37. Zargarbashi R, Abdi R, Bozorgmanesh M, Panjavi B. Anterior distal hemiepiphysiodesis of tibia for treatment of recurrent equinus deformity due to flat-top talus in surgically treated clubfoot. J Foot Ankle Surg 2020;59:418–422. [DOI] [PubMed] [Google Scholar]
- 38. Jauregui JJ, Zamani S, Abawi HH, Herzenberg JE. Ankle range of motion after posterior subtalar and ankle capsulotomy for relapsed equinus in idiopathic clubfoot. J Pediatr Orthop 2017;37:199–203. [DOI] [PubMed] [Google Scholar]
- 39. Park SS, Lee HS, Han SH, Park JW, de Peralta MJB. Gastrocsoleus fascial release for correction of equinus deformity in residual or relapsed clubfoot. Foot Ankle Int 2012;33:1075–1078. [DOI] [PubMed] [Google Scholar]
- 40. Shah A, Mehta R, Aroojis A. The Ponseti method of clubfoot treatment in walking age children: is it effective? A study of 56 children from 1 to 10 years of age. J Pediatr Orthop B 2019;28:159–166. [DOI] [PubMed] [Google Scholar]
- 41. Refai MA, Song SH, Song HR. Does short-term application of an Ilizarov frame with transfixion pins correct relapsed clubfoot in children? Clin Orthop Relat Res 2012;470:1992–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ezra E, Hayek S, Gilai AN, Khermosh O, Wientroub S. Tibialis anterior tendon transfer for residual dynamic supination deformity in treated club feet. J Pediatr Orthop B 2000;9:207–211. [DOI] [PubMed] [Google Scholar]
- 43. Carroll NC. Surgical technique for talipes equinovarus. Oper Tech Orthop 1993;3:115–120. [Google Scholar]
- 44. SooHoo NF, Shuler M, Fleming LL; American Orthopaedic Foot and Ankle Society. Shuler M, Fleming LL. Evaluation of the validity of the AOFAS clinical rating systems by correlation to the SF-36. Foot Ankle Int 2003;24:50–55. [DOI] [PubMed] [Google Scholar]
- 45. Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int 2004;25:521–525. [DOI] [PubMed] [Google Scholar]