Abstract
The posterior oblique ligament (POL) is the predominant ligamentous structure on the posterior medial corner of the knee joint. A thorough understanding of the anatomy, biomechanics, diagnosis, treatment and rehabilitation of POL injuries will aid orthopaedic surgeons in the management of these injuries.
The resulting rotational instability, in addition to valgus laxity, may not be tolerated by athletes participating in pivoting sports. The most common mechanism of injury – accounting for 72% of cases – is related to sports activity, particularly football, basketball and skiing. Moreover, three different injury patterns have been reported: those associated with injury to the capsular arm of the semimembranosus (SM), those involving a complete peripheral meniscal detachment and those involving disruption of the SM and peripheral meniscal detachment.
The hallmark of an injury related to POL lesions is the presence of anteromedial rotatory instability (AMRI), which is defined as ‘external rotation with anterior subluxation of the medial tibial plateau relative to the distal femur’.
In acute settings, POL lesions can be easily identified using coronal and axial magnetic resonance imaging (MRI) where the medial collateral ligament (MCL) and POL appear as separate structures. However, MRI is not sensitive in chronic cases.
Surgical treatment of the medial side leads to satisfactory clinical results in a multi-ligamentous reconstruction scenario, but it is known to be associated with secondary stiffness.
In young patients with high functional demands, return to sports is allowed no earlier than 9–12 months after they have undergone a thorough rehabilitation programme.
Cite this article: EFORT Open Rev 2021;6:364-371. DOI: 10.1302/2058-5241.6.200127
Keywords: multiple ligament injuries, posteromedial corner of the knee, posterior oblique ligament of the knee, sports medicine
Introduction
The posterior oblique ligament (POL) was described for the first time by Hughston and Eilers in 1973 who assigned clinical and biomechanical significance of the knee’s stability to it.1 Subsequently, however, Robinson et al, in their dissection study, did not find a discrete ligament, and they simply referred to all structures posterior to the superficial medial collateral ligament (sMCL) as the posteromedial joint capsule.2 Biomechanics and cadaveric studies have demonstrated that the POL can be considered to be the predominant ligamentous structure on the posterior medial corner of the knee joint. It is located at the posterior third of the medial collateral ligament, attached proximally to the adductor tubercle of the femur and distally to the tibia and posterior aspect of the joint capsule.3 The main role of the POL is to control anteromedial rotatory instability (AMRI) and to provide static resistance to the valgus loads when the knee is fully extended. Moreover, the POL plays a small role in preventing posterior translation of the tibia on the femur because the posterior cruciate ligament (PCL) is so overpowering.4 During a side-step cut, the POL contributes to keeping the pivot leg from opening in valgus, possibly acting in synergy with semimembranosus (SM) muscle activation. Additionally, the POL helps prevent excessive external tibial rotation and internal femoral rotation. Investigating the extent of injury to the POL and posterior capsule is important in decision-making because the non-operative treatment of these injuries may more likely lead to unsatisfactory results.5 The resulting rotational instability, in addition to valgus laxity, may not be tolerated by athletes participating in pivoting sports.6 This narrative review aims to demonstrate that the POL is the predominant structure in the posteromedial corner of the knee joint (PMC) and that surgical reconstruction should be considered the gold standard treatment in case of injury. Further, we analysed the best imaging and surgical strategies in the setting of POL lesions.
Anatomy
Course
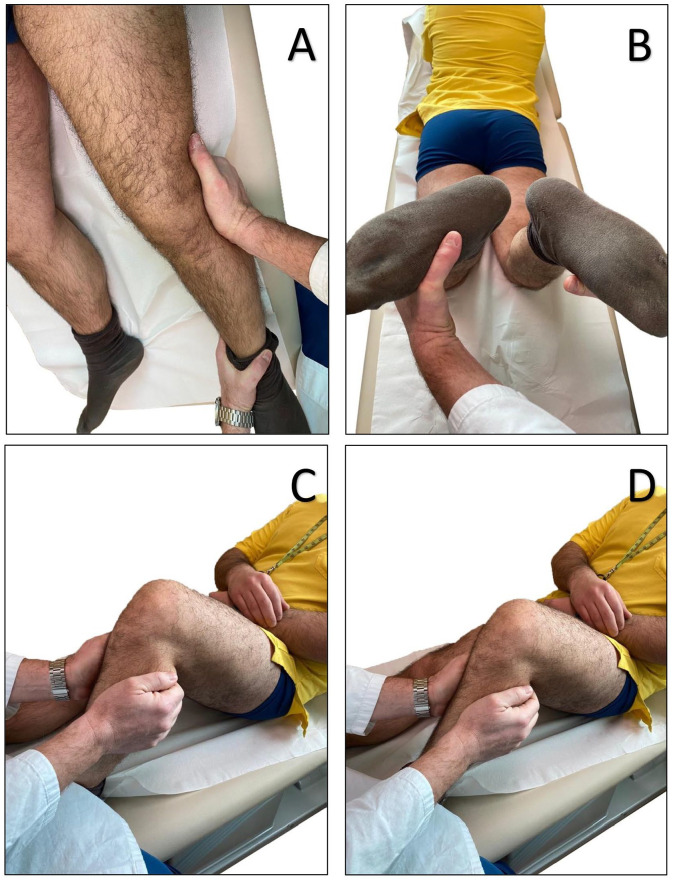
The anatomy of the PMC has been described in different ways, depending on whether it is possible to define a distinct POL as part of the posteromedial (PM) capsule. Brantigan and Voshell and Warren and Marshall have described it as part of the posterior fibre bundles of the sMCL.7,8 Some others have described the POL to be distinct from the sMCL.9,10 LaPrade et al have described in detail the anatomy of the POL, distinguishing three fascial attachments that course off the distal aspect of the SM tendon, which were previously termed as the superficial, central (tibial) and capsular arms.11 The superficial arm consists of a thin fascial expansion and courses from the medial to the anterior arm of the SM, and distally, it follows the posterior border of the sMCL. Proximally, it blends into the central arm of the POL, whereas distally, it blends into the distal tibial expansion of the SM and its tibial attachment. The central arm is the largest and thickest portion of the POL. It courses from the distal aspect of the main SM tendon and is a thick fascial reinforcement of both the meniscofemoral (MF) and meniscotibial (MT) portions of the PM capsule; it also presents a stout attachment to the medial meniscus (MM). Anteriorly, it merges with the posterior fibres of the sMCL. The central arm of the POL can be differentiated from the sMCL by the proximal course of its fanlike fibres, which runs more posteriorly towards its femoral attachment. The capsular arm of the POL consists of a thin proximal fascial expansion off the anterior aspect of the distal part of the SM tendon. It is located posteriorly and laterally to the meniscofemoral capsular attachments of the central arm and has no fibres coursing towards the tibia. The capsular arm is primarily blended with the MF portion of the PM capsule and the medial aspect of the oblique popliteal ligament, and it is also attached to the soft tissues over the medial gastrocnemius tendon, the adductor magnus tendon’s expansion to the medial gastrocnemius and the adductor magnus tendon’s femoral attachment (Fig. 1).11
Fig. 1.
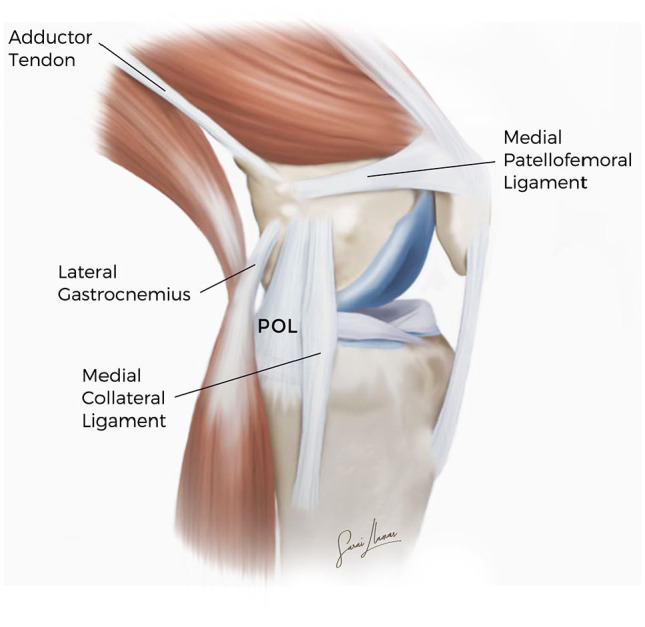
Illustration of the main medial knee structures (left knee).
Note. POL, posterior oblique ligament.
Insertions and landmarks
Few anatomic studies have been performed to identify bony landmarks and the tibial and femoral insertions of POL.11–12 The femoral ligament insertion has a mean distance of 18.1–18.3 mm from the adductor tubercle (AT). The mean distance was taken from AT and not medial epycondile (ME) and gastrocnemius tubercle (GT); in fact, during a surgical procedure in medial reconstruction, the AT may be the most reliable osseous landmark at the femur and can be easily palpated and clearly identified. The mean linear distance between the direct tibial insertion of POL and the joint line was 5.8mm. A 3D-reconstruction study revealed that the mean surface area of the femoral and tibial insertions of POL was 71.5 mm2 and 38.8 mm2 respectively (Fig. 1)12
Biomechanics
There is an important interplay between the posteromedial structures. Although often thought of as a single entity, the components of the medial collateral ligament (MCL) complex have distinctly different load-sharing characteristics that depend on the knee flexion angle. A recent systematic review of biomechanical studies13 has demonstrated the role of the POL as a primary stabilizer for internal rotation (IR) and a secondary stabilizer for valgus and external rotation, while the sMCL is the primary knee valgus stabilizer across all knee flexion angles, and it also acts as a secondary stabilizer to external and internal rotation depending on the knee flexion angle. In particular, the sMCL contributes 78% of the stability during valgus and external rotation at 25° of knee flexion, and the POL plays a primary role in IR and preventing valgus when knee flexion is between 0° and 30°.3
Injury patterns
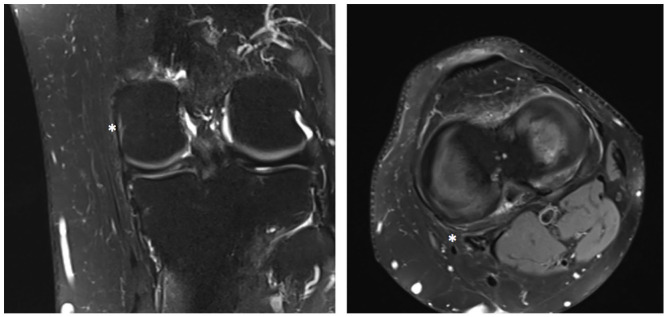
Isolated injury of the POL is rare. In 99% of cases, POL injury occurs in association with Grade III MCL injuries, and in 78% of cases with concomitant meniscal or cruciate ligament injuries.10 In 2004, Sims et al identified three different basic POL injury patterns in 93 surgical patients with medial side injury, which are as follows: (1) those associated with injury to the capsular arm of the SM (70%), (2) those involving a complete peripheral meniscal detachment (30%) and (3) those involving disruption of the SM and peripheral meniscal detachment (19%). Almost all the patients (99%) with Grade III MCL reported POL injuries, divided into focal injuries (70.6%) and multi-focal injuries (29.4%). Concomitant lesions such as to the SM or MM were found to have an incidence ranging from 40% to 70%, confirming that the POL is the most easily damaged structure in the PMC and accurate clinical, and so radiologic, evaluation should always be performed (Fig. 2).14
Fig. 2.
Major acute injury patterns to the posterior oblique ligament of a right knee: injury of the POL with semimembranosus lesion; injury of the central arm of the POL; injury of the POL associated with meniscus detachment; injury of the superficial arm of the POL.
Note. POL, posterior oblique ligament.
Chahal et al have documented injuries to the posteromedial structures of the knee using magnetic resonance imaging (MRI) and found the POL to be injured in 64% of patients with dislocated knees (14/22). Of these, nine patients had a complete injury, and five patients had a partial injury.15 Four patients demonstrated Grade III medial laxity during valgus stress testing under anaesthesia at 0° and 30°. All of these four patients had a complete tear of the POL. Not a single patient with Grade I laxity had a complete tear of the POL.
The mechanism of injury typically involves valgus knee loading, tibial external rotation or a combined force vector of valgus loading and external rotation that occurs in such sports as skiing, ice hockey and soccer, which require knee flexion. The remaining injuries were secondary to a fall or motor vehicle accident. Non-contact injuries usually resulted in low-grade sprains, whereas a direct blow to the lateral leg produced a major valgus force and a higher-grade injury. A pure valgus force often caused an isolated MCL injury. External rotation and valgus forces combined were most likely to injure the POL and other components of the PMC.
Physical examination
Patients may present with medial knee pain, tenderness, valgus instability and anteromedial rotatory instability. A detailed history and physical examination are the important initial steps in the diagnosis and help guide further workup of suspected posteromedial injuries.
During the physical examination, the clinician may perform a valgus stress test, an anterior drawer test or posterior drawer test and a dial test. These are the tests used for evaluating the integrity of the MCL and/or POL, anterior cruciate ligament (ACL) and PCL, respectively. The valgus stress test is a very specific and sensitive test for a POL injury. It is performed at 0° and 30° of flexion, and the degree of valgus gapping is related to the severity of the injury. For isolated superficial MCL tears, maximum valgus gapping should be observed with the knee at 20° to 30° of flexion. If valgus gapping is observed with the lower limb in full extension, a concurrent injury to the meniscofemoral deep MCL attachment, POL or both structures should be suspected. Furthermore, physical examination findings that are suggestive of valgus gapping in extension should raise the suspicion of a concomitant ACL injury.16,17 For suspected ACL injuries and to assess the amount of rotational stability, an anteromedial drawer test can be performed with the knee in 80–90° of flexion and the foot externally rotated 10–15°, applying a coupled anterior and external rotatory force to the knee. Increased anterior translation with the tibia in external rotation is indicative of AMRI and indicates injury to the ACL-PMC. For suspected PCL injury, a posterior drawer test should be performed with the tibia in neutral and internal rotation. In an isolated PCL injury, there will be decreased posterior tibial translation with the tibia in IR because the POL and posteromedial capsule function as secondary stabilizers to this translation, while a hyper external rotation can be due to posterolateral corner injuries. Therefore, in combined PCL-PMC injuries, there will be an equal posterior translation of the tibia relative to the femur with the tibia in both neutral and internal rotation.16,17 Finally, anteromedial instability is characterized by combined lesion of the sMCL and POL and a positive dial test may indicate it. A dial test is carried out at 30° and 90° of knee flexion with the patient in the prone or supine position to determine whether increases in external rotation (ER) occur with anterior subluxation of the lateral tibial plateau (Fig. 3).
Fig. 3.
Physical examination of a combined sMCL/POL injury. (A) Valgus stress test. (B) Dial test. (C) Anterior drawer Test. (D) Posterior drawer Test.
Note. sMCL, superficial medial collateral ligament; POL, posterior oblique ligament.
Imaging
Imaging evaluation is critical for the diagnosis of POL injuries and/or associated lesions, particularly in the setting of an acute injury when a thorough examination is not possible. In chronic cases, MRI and ultrasound (US) are not very suitable and clinical diagnosis is essential.
MRI
No recognized MRI classification has been published to classify POL injuries so far. However, House et al have proposed using the same classification that is used for the MCL. This classification divides lesions into simple sprains, partial tears and complete POL tears and can be optimally demonstrated on a combination of coronal and axial images (Table 1).18
Table 1.
Magnetic resonance imaging (MRI) classification of acute injury of the posterior oblique ligament (POL) proposed by House et al18
| Grade | Description |
|---|---|
| Grade I – microscopic tear |
Ligament of normal thickness and intact with oedema (T2 high signal) surrounding the ligament |
| Grade II – partial tear |
Thickening of the ligament with partial disruption of fibres and increased amount of surrounding oedema/haemorrhage |
| Grade III – complete tear |
Complete disruption of the ligament with surrounding oedema/haemorrhage |
MRI is a diagnostic tool that may be used preoperatively for delineating various ligamentous and capsular injuries to help design the operative approach. At present, there are no specific studies that have evaluated the sensitivity and specificity of POL visualization with MRI. MRI should be performed before the fixing of any co-existing periarticular fractures, as metal artifacts can affect the quality of the study. MRI is particularly useful when evaluating patients with multi-ligamentous knee injuries; however, it has been shown that MRI tends to overestimate injury to ligamentous structures.19
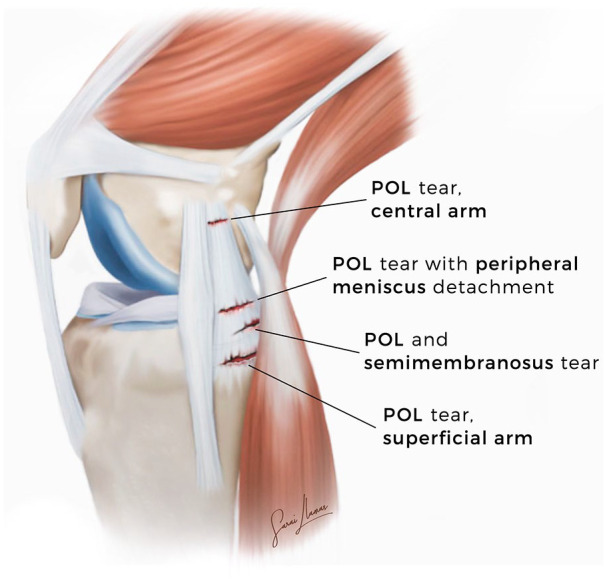
The coronal plane allowed for visualization of the POL; however, the coronal oblique plane in combination with the axial plane improved the analysis of the POL. The axial images were adequate for an analysis of the POL; however, the coronal oblique plane offered another perspective of the complex anatomy in this area. In case of doubt, the addition of intraarticular contrast material can optimize the visualization of the POL and the capsular layers in the axial plane as, most likely, these structures are displaced away from the femur (Fig. 4).19,20
Fig. 4.
Coronal (left) and Axial (right) T2-weighted fat-saturated magnetic resonance images showing normal POL (asterisk).
Note. POL, posterior oblique ligament.
Source: Case courtesy of Dr Carmelo Messina (Università degli Studi di Milano).
Ultrasound
US is an excellent imaging modality for the evaluation of superficial soft tissue structures.21,22 Direct correlation with the site of pain and comparison with the controlateral normal side are some of the advantages of US. For the evaluation of medial structures, it is important to identify the medial epicondyle as a femoral bony landmark.21 The examination of the medial compartment is conducted at 30° of flexion. Voluntary external rotation facilitates visualization of the medial knee side.23 Although MRI is superior in POL evaluation, US in the hands of an experienced sonologist can help identify injuries in acute settings. To obtain reliable results with US, two points are fundamental.22 The first is patient history and clinical examination; in fact, focusing the US examination on the possible pathology reduces the chances of misdiagnosis, especially if a dynamic examination is used. Second, US of posteromedial knee structures should be performed by specialists trained in knee sonography.21,22
Conservative treatment
The treatment for isolated Grade I and II MCL injuries is mainly conservative, while for Grade III MCL injuries it depends on whether the injuries are isolated or combined with other ligamentous injuries. A critical point involves distinguishing whether the injury involves the POL as it indicates a more serious injury that is, therefore, less likely to heal with conservative treatment.24 Most treatment protocols focus on functional bracing, early range of motion, protected weight-bearing and progression towards strengthening exercises and, of course, a gradual return to activities as the pain diminishes. Conservative treatment for a complete return to sports can generally be allowed once a patient has a painless and full range of motion and once no instability exists on examination, and the muscle strength has returned to normal and is equal to that of the uninjured side.24,25
Surgical treatment
Grade III injuries of the PMC with valgus gapping in extension have a higher risk of not healing, resulting in residual valgus and rotational instability. Persistent instability increases the load on the cruciate ligament grafts, increasing the risk of reconstruction graft failure. Therefore, in the context of a multi-ligament knee injury involving the POL, early concurrent repair or reconstruction is recommended to facilitate early mobilization and rehabilitation.26
The existing relevant literature discusses several repair and reconstruction techniques for the treatment of isolated and combined medial knee injuries. Different approaches exist within these techniques, and they may differ in terms of the graft choices, methods of fixation, number of bundles, tensioning protocol and degree of anatomic restoration of medial and PMC knee restraints.27
Kim et al and Lind et al tried to perform an anatomic double-bundle reconstruction using a semitendinosus (ST) tendon with a single femoral tunnel preserving good stability, and they achieved satisfactory results at a mean follow-up (FU) of 52.6 months and two years, respectively.28,29 LaPrade and Wijdicks proposed a new anatomic double-bundle reconstruction using two femoral tunnels and two tibial tunnels, and they showed that the medial joint opening was 1.3 mm, and the subjective International Knee Documentation Committee (IKDC) score was 76.2 (54–88) at the minimum six-months FU (Fig. 5).30 However, the need for two tunnels, one each in the tibia and femur, has limited the use of this technique. Stannard et al compared the outcomes of surgical repair versus reconstruction using allograft in one group of patients and autograft in another.31 They have reported similar results in two reconstruction groups and the superiority of the reconstruction approach over the repair approach. Recently, Xu et al and Lee et al attempted a more anatomic medial complex reconstruction using a triangular vector with a single femoral tunnel proximal and posterior to the medial femoral epicondyle reporting satisfactory clinical and functional outcomes at the mid-term FU.32,33
Fig. 5.
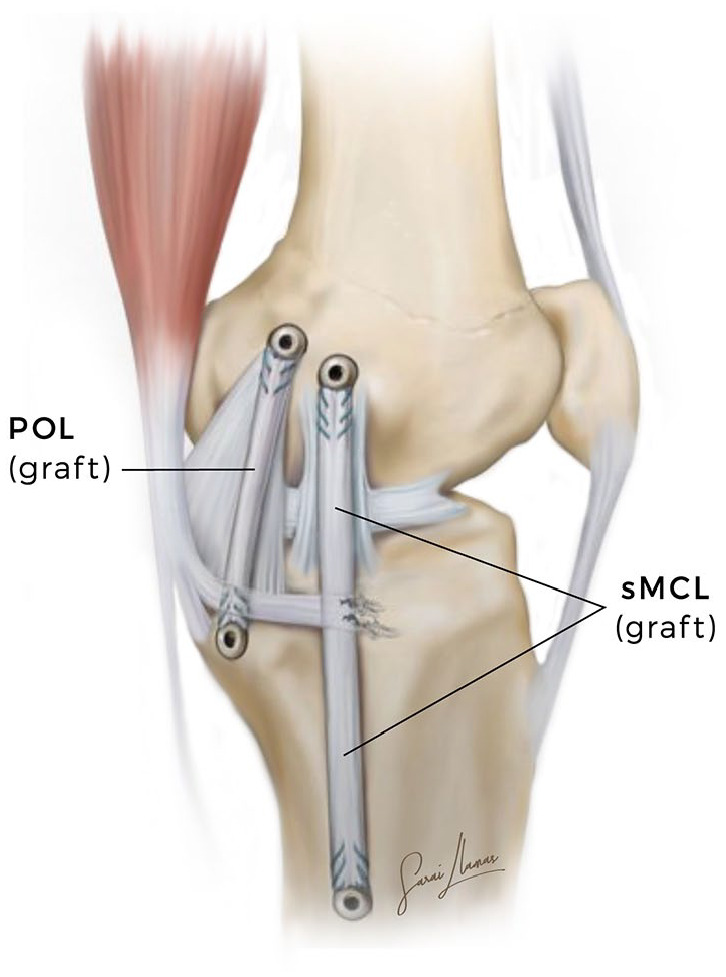
Illustration of a left knee showing the superficial medial collateral ligament (sMCL) and posterior oblique ligament (POL) reconstruction grafts.
Rehabilitation
Specific rehabilitation protocols depend on whether concomitant surgeries have been performed along with that on the POL. In cases of isolated MCL and POL reconstruction, the patient received a long-hinged non-weight-bearing brace for six weeks. Non-weight-bearing walking was encouraged, but with the advice to keep the long-hinged brace. During this period, range of motion (ROM) exercises were restricted from 0° to 90° knee flexion. Six weeks later, knee flexion progressed to a full ROM and weight-bearing walking was allowed, as tolerated. Further mobilization without brace protection was also permitted. When gait training is initiated, it is important to educate patients about avoiding pivoting motions of their foot while participating in different activities as it could stress the reconstruction grafts of the knee. Closed kinetic-chain exercises were permitted for functional strengthening with the addition of two-limb support squatting. After the initiation of weight-bearing, it is mandatory to recover normal gait mechanics. It is also important to not excessively stress the joint such that knee effusions develop due to activities that overuse quadriceps and cause lower extremity weakness.34,35
Return to sports
The decision to allow a patient to return to sports following reconstructive knee surgery is a challenging one for surgeons, physical trainers, athletic trainers and all other members of an athlete’s treatment team. Noyes reported that the return-to-play decision is based on subjective, non-specific criteria such as ‘regained full functional stability’, ‘normal knee function on clinical examination’, ‘satisfactory stability’ or ‘nearly full ROM and muscle strength’.36,37 As for the objective criteria in this regard, such considerations as the time to have passed surgery, muscle strength, ROM and effusion are most frequently taken into account.38 Further, the Vail Sport Test score can also help surgeons and therapists decide about the return-to-play timing.39 Moreover, patients should demonstrate near-normal reported outcome scores (SANE/IKDC < 5% difference from the contralateral side).
Conclusions
Our review confirms that the POL is the predominant structure of the PMC of the knee, and injury to it should always be suspected in the case of a tear of concomitant ligaments. In the case of instability with valgus laxity and medial joint opening, more than 5 mm surgery results in good to excellent clinical results regardless of the surgical techniques performed, and the complication and failure rates are also negligible in this case. Due care must be given to femoral and tibial tunnel convergence. In young patients with high functional demands, return to sports should not be allowed before 9–12 months after completing a rehabilitation programme.
Acknowledgments
The authors thank Sarai Llamas for professional medical illustrations and Dr. Carmelo Messina (Università degli Studi di Milano) for radiological imaging.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am 1973;55:923–940. [PubMed] [Google Scholar]
- 2. Robinson JR, Sanchez-Ballester J, Bull AM, Thomas RW, Amis AA. The posteromedial corner revisited: an anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Joint Surg Br 2004;86:674–681. [DOI] [PubMed] [Google Scholar]
- 3. Dold AP, Swensen S, Strauss E, Alaia M. The posteromedial corner of the knee: anatomy, pathology, and management strategies. J Am Acad Orthop Surg 2017;25:752–761. [DOI] [PubMed] [Google Scholar]
- 4. Selim NM. Combined anterior cruciate ligament, medial collateral ligament, and posterior oblique ligament reconstruction through single tibial tunnel using hamstring tendon autografts. Arthrosc Tech 2019;8:e163–e173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Petersen W, Loerch S, Schanz S, Raschke M, Zantop T. The role of the posterior oblique ligament in controlling posterior tibial translation in the posterior cruciate ligament-deficient knee. Am J Sports Med 2008;36:495–501. [DOI] [PubMed] [Google Scholar]
- 6. Wijdicks CA, Griffith CJ, LaPrade RF, et al. Medial knee injury: part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med 2009;37:1771–1776. [DOI] [PubMed] [Google Scholar]
- 7. Brantigan OC, Voshell AF. The tibial collateral ligament: its function, its bursae, and its relation to the medial meniscus. J Bone Joint Surg Am 1943;25:121–131. [Google Scholar]
- 8. Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am 1979;61:56–62. [PubMed] [Google Scholar]
- 9. Tibor LM, Marchant MH, Jr, Taylor DC, Hardaker WT, Jr, Garrett WE, Jr, Sekiya JK. Management of medial-sided knee injuries, part 2: posteromedial corner. Am J Sports Med 2011;39:1332–1340. [DOI] [PubMed] [Google Scholar]
- 10. Lundquist RB, Matcuk GR, Jr, Schein AJ, et al. Posteromedial corner of the knee: the neglected corner. Radiographics 2015;35:1123–1137. [DOI] [PubMed] [Google Scholar]
- 11. LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000–2010. [DOI] [PubMed] [Google Scholar]
- 12. Saigo T, Tajima G, Kikuchi S, et al. Morphology of the insertions of the superficial medial collateral ligament and posterior oblique ligament using 3-dimensional computed tomography: a cadaveric study. Arthroscopy 2017;33:400–407. [DOI] [PubMed] [Google Scholar]
- 13. D’Ambrosi R, Corona K, Guerra G, Rubino M, Di Feo F, Ursino N. Biomechanics of the posterior oblique ligament of the knee. Clin Biomech (Bristol, Avon) 2020;80:105205. [DOI] [PubMed] [Google Scholar]
- 14. Sims WF, Jacobson KE. The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med 2004;32:337–345. [DOI] [PubMed] [Google Scholar]
- 15. Chahal J, Al-Taki M, Pearce D, Leibenberg A, Whelan DB. Injury patterns to the posteromedial corner of the knee in high-grade multiligament knee injuries: a MRI study. Knee Surg Sports Traumatol Arthrosc 2010;18:1098–1104. [DOI] [PubMed] [Google Scholar]
- 16. Swinford ST, LaPrade R, Engebretsen L, Cohen M, Safran M. Biomechanics and physical examination of the posteromedial and posterolateral knee: state of the art. J ISAKOS 2020;5:378–388. [Google Scholar]
- 17. Craft JA, Kurzweil PR. Physical examination and imaging of medial collateral ligament and posteromedial corner of the knee. Sports Med Arthrosc Rev 2015;23:e1–e6. [DOI] [PubMed] [Google Scholar]
- 18. House CV, Connell DA, Saifuddin A. Posteromedial corner injuries of the knee. Clin Radiol 2007;62:539–546. [DOI] [PubMed] [Google Scholar]
- 19. Loredo R, Hodler J, Pedowitz R, Yeh LR, Trudell D, Resnick D. Posteromedial corner of the knee: MR imaging with gross anatomic correlation. Skeletal Radiol 1999;28:305–311. [DOI] [PubMed] [Google Scholar]
- 20. Gaetke-Udager K, Yablon CM. Imaging of ligamentous structures within the knee includes much more than the ACL. J Knee Surg 2018;31:130–140. [DOI] [PubMed] [Google Scholar]
- 21. Jacobson JA, Ruangchaijatuporn T, Khoury V, Magerkurth O. Ultrasound of the knee: common pathology excluding extensor mechanism. Semin Musculoskelet Radiol 2017;21:102–112. [DOI] [PubMed] [Google Scholar]
- 22. Paczesny Ł, Kruczyński J. Ultrasound of the knee. Semin Ultrasound CT MR 2011;32:114–124. [DOI] [PubMed] [Google Scholar]
- 23. De Maeseneer M, Marcelis S, Boulet C, et al. Ultrasound of the knee with emphasis on the detailed anatomy of anterior, medial, and lateral structures. Skeletal Radiol 2014;43:1025–1039. [DOI] [PubMed] [Google Scholar]
- 24. Bonasia DE, Bruzzone M, Dettoni F, et al. Treatment of medial and posteromedial knee instability: indications, techniques, and review of the results. Iowa Orthop J 2012;32:173–183. [PMC free article] [PubMed] [Google Scholar]
- 25. Chahla J, Kunze KN, LaPrade RF, et al. The posteromedial corner of the knee: an international expert consensus statement on diagnosis, classification, treatment, and rehabilitation. Knee Surg Sports Traumatol Arthrosc 2020. doi: 10.1007/s00167-020-06336-3 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cinque ME, Chahla J, Kruckeberg BM, DePhillipo NN, Moatshe G, LaPrade RF. Posteromedial corner knee injuries: diagnosis, management, and outcomes: a critical analysis review. JBJS Rev 2017;5:e4. [DOI] [PubMed] [Google Scholar]
- 27. DeLong JM, Waterman BR. Surgical techniques for the reconstruction of medial collateral ligament and posteromedial corner injuries of the knee: a systematic review. Arthroscopy 2015;31:2258–2272.e1. [DOI] [PubMed] [Google Scholar]
- 28. Kim SJ, Lee DH, Kim TE, Choi NH. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br 2008;90:1323–1327. [DOI] [PubMed] [Google Scholar]
- 29. Lind M, Jakobsen BW, Lund B, Hansen MS, Abdallah O, Christiansen SE. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med 2009;37:1116–1122. [DOI] [PubMed] [Google Scholar]
- 30. LaPrade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res 2012;470:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Stannard JP, Black BS, Azbell C, Volgas DA. Posteromedial corner injury in knee dislocations. J Knee Surg 2012;25:429–434. [DOI] [PubMed] [Google Scholar]
- 32. Xu H, Kang K, Zhang J, et al. An anatomical-like triangular-vector ligament reconstruction for the medial collateral ligament and the posterior oblique ligament injury with single femoral tunnel: a retrospective study. J Orthop Surg Res 2017;12:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee DW, Kim JG. Anatomic medial complex reconstruction in serious medial knee instability results in excellent mid-term outcomes. Knee Surg Sports Traumatol Arthrosc 2020;28:725–732. [DOI] [PubMed] [Google Scholar]
- 34. Thomson LC, Handoll HH, Cunningham A, Shaw PC. Physiotherapist-led programmes and interventions for rehabilitation of anterior cruciate ligament, medial collateral ligament and meniscal injuries of the knee in adults. Cochrane Database Syst Rev 2002;2:CD001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kim C, Chasse PM, Taylor DC. Return to play after medial collateral ligament injury. Clin Sports Med 2016;35:679–696. [DOI] [PubMed] [Google Scholar]
- 36. Medvecky MJ, Zazulak BT, Hewett TE. A multidisciplinary approach to the evaluation, reconstruction and rehabilitation of the multi-ligament injured athlete. Sports Med 2007;37:169–187. [DOI] [PubMed] [Google Scholar]
- 37. Lorenz DS, Reiman MP, Walker JC. Periodization: current review and suggested implementation for athletic rehabilitation. Sports Health 2010;2:509–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Drew MK, Finch CF. The relationship between training load and injury, illness and soreness: a systematic and literature review. Sports Med 2016;46:861–883. [DOI] [PubMed] [Google Scholar]
- 39. Garrison JC, Shanley E, Thigpen C, Geary R, Osler M, Delgiorno J. The reliability of the vail sport test™ as a measure of physical performance following anterior cruciate ligament reconstruction. Int J Sports Phys Ther 2012;7:20–30. [PMC free article] [PubMed] [Google Scholar]