Abstract
Introduction
The effects of healthcare-related inequalities are most evident in low-resource settings. Such settings are often not explicitly defined, and umbrella terms which are easier to operationalise, such as ‘low-to-middle-income countries’ or ‘developing countries’, are often used. Without a deeper understanding of context, such proxies are pregnant with assumptions, insinuate homogeneity that is unsupported and hamper knowledge translation between settings.
Methods
A systematic scoping review was undertaken to start unravelling the term ‘low-resource setting’. PubMed, Africa-Wide, Web of Science and Scopus were searched (24 June 2019), dating back ≤5 years, using terms related to ‘low-resource setting’ and ‘rehabilitation’. Rehabilitation was chosen as a methodological vehicle due to its holistic nature (eg, multidisciplinary, relevance across burden of disease, and throughout continuum of care) and expertise within the research team. Qualitative content analysis through an inductive approach was used.
Results
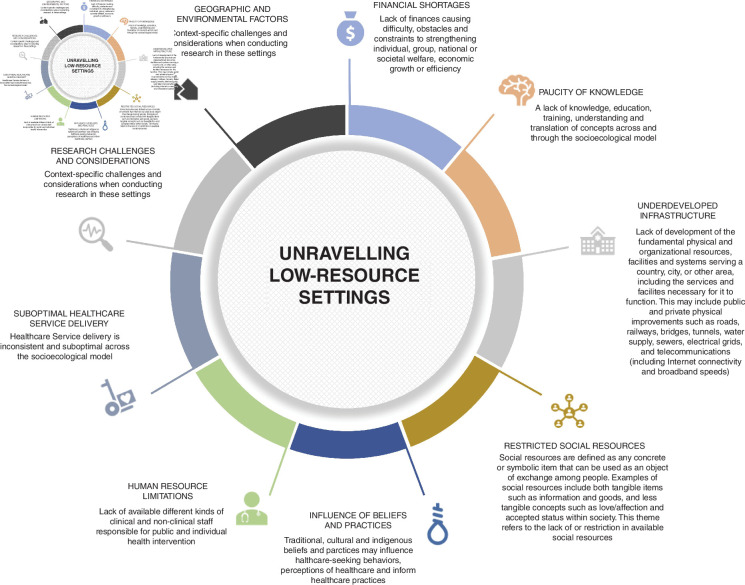
A total of 410 codes were derived from 48 unique articles within the field of rehabilitation, grouped into 63 content categories, and identified nine major themes relating to the term ‘low-resource setting’. Themes that emerged relate to (1) financial pressure, (2) suboptimal healthcare service delivery, (3) underdeveloped infrastructure, (4) paucity of knowledge, (5) research challenges and considerations, (6) restricted social resources, (7) geographical and environmental factors, (8) human resource limitations and (9) the influence of beliefs and practices.
Conclusion
The emerging themes may assist with (1) the groundwork needed to unravel ‘low-resource settings’ in health-related research, (2) moving away from assumptive umbrella terms like ‘low-to-middle-income countries’ or ‘low/middle-income countries’ and (3) promoting effective knowledge transfer between settings.
Keywords: qualitative study, health systems, review, public health
Key questions.
What is already known?
Health inequalities are more pronounced in resource-constrained settings.
Such settings are often described using proxies such as ‘low-to-middle-income countries’, ‘low/middle-income countries’ and more recently, ‘low-resource settings’.
Without clear operationalisation, umbrella terms like ‘low-resource setting’ remain pregnant with unsupported assumptions.
What are the new findings?
The term ‘low-resource settings’ could be expanded to nine themes which show that these settings are not unidimensional or dichotomous (ie, adequate vs inadequate), yet rather reflect a complex network of inter-related resource limitations and concepts.
The complexity of the term is further demonstrated by the convergence of settings reported as ‘low resource’, yet include countries classified by the World Bank as a high-income country.
What do the new findings imply?
Using proxies (ie, low-to-middle-income countries, or low-resource settings) undermines the complexity of such settings and insinuates a level of homogeneity that is unsupported.
To promote knowledge transfer between settings and accelerate innovations to promote health equity, all stakeholders (eg, researchers, clinicians, policy-makers) can benefit from being more deliberate in describing the context in which their work is embodied.
This review lays the groundwork for the development of a theoretical framework to do so.
Introduction
In low-resource settings (LRSs), it is thought that the vast differences in the burden of disease and life expectancies, are reflective of underlying determinants (eg, quality, access, availability), which cause widespread inconsistencies and systematic differences in health.1–3 Moreover, when such health inequalities are unjust, unnecessary and preventable, they lead to health inequity.4 In general, differences in health, such as those based on gender or religion, are considered health inequities because they reflect an unfair distribution of health risks and resources.5 Given that unjust differences in health risks are likely the product of the entire setting, rather than solely a reflection of the healthcare system,1 one would need clear understanding of the context to promote transferability of resources (including knowledge). Primary and secondary research are instrumental in promoting that understanding within and between settings.
Research that has explored various health system components in relation to health or health inequity often refers to the work being conducted in an LRS or (a specific) low-income to middle-income country (LMIC).6–8 Other umbrella terms often used in conjunction with LMIC include for instance ‘low/middle-income countries’ or ‘global south’ (as opposed to global north). While there is a sizeable association between healthcare expenditure and healthcare provision,9 it is a widely held view that the capacity of a setting to provide adequate healthcare is dependent on a myriad of interrelated factors, rather than government spending (the gross national product determines classification as low, lower-middle or upper-middle-income country). To acknowledge the fact that health inequities persist in developed and high-income countries, researchers increasingly use the term ‘LRS’. To our knowledge, Holt was one of the first to use this term, while also acknowledging the notion of LRSs in developed countries.10 Currently, close to 5000 articles in the field of healthcare explicitly refer to ‘LRSs’ in either the title or abstract. Unfortunately, too often when using ‘LRS’ as an umbrella term, or LMIC alike, unexamined assumptions persist with respect to the homogeneity between countries (or settings), as they are rarely adequately described. Yet, if a clear understanding and nuance of the context in which healthcare research is conducted is poorly described, knowledge transfer from one setting to another and sustainability of the research findings, could be hindered.
One particularly important, yet notoriously resource-intensive model of care for those with chronic conditions and subsequent disability, is rehabilitation.11 A comprehensive rehabilitation programme may often involve multiple skilled health disciplines, various core components (eg, exercise, education), effective lines of referral, adequate physical resources and equipment and patient compliance through adherence and social support, among others. Despite the evidence for the benefits of rehabilitation across a wide variety of medical conditions,12 there is an overwhelming unmet and increasing need for rehabilitation globally.13 14 As a result of multifacetted resource constraints,15 the inability of healthcare systems to meet the growing need for rehabilitation has the potential to further exacerbate continued health inequalities and inequities. Improved understanding of the resource-constraints referred to when rehabilitation is studied in LRSs, could aid in the successful development, study and implementation of rehabilitation interventions in these settings. Hence, on the one hand there is growing need for rehabilitation globally, which may have a profound impact on LRSs specifically. Yet, on the other hand, there is insufficient understanding and reporting16 of the ‘resource constraints’ that contribute to the challenges faced when upscaling or rethinking rehabilitation in LRSs.
Using a qualitative approach, the objective of this review is to analyse the descriptions used in published literature in relation to the implicit concept of ‘LRSs’. Through unravelling the implicit concept of ‘LRSs’, we aim to improve our understanding of resource shortages given a specific context, exemplified through the field of rehabilitation medicine, as well as to challenge the generic use of umbrella terms (like LRSs) in global health.
Methods
A systematic scoping review17 was undertaken to identify published literature within the field of rehabilitation. The review is reported in adherence to the Preferred Reporting for Systematic Reviews and Meta-Analyses extension for Scoping Reviews guidelines.18
Inclusion and exclusion criteria
An iterative process was used to decide on and refine the inclusion and exclusion criteria as the researchers became more familiar with the literature. Original research, published in English, including a self-reported setting of ‘low resource’ in title, abstract or keywords were included. As LRSs are not endemic to LMICs, the inclusion criteria and subsequent search strategy focusses on settings of low-resource, rather than income classifications. In addition, we limited the search to studies published within the past 5 years. This decision was based on the continually fluctuating global economy which impacts the World Bank classification. We excluded case studies, case reports, case series or reviews, and studies pertaining to the rehabilitation of the use, misuse, or abuse of substances such as, but not limited to, alcohol, smoking, medication, drugs, etc. We also excluded studies that evaluated healthcare worker perspectives, system or cost evaluations.
Definition of rehabilitation
Rehabilitation was defined as ‘a set of interventions designed to optimise functioning and reduce disability in individuals with health conditions in interaction with their environment. Health condition refers to disease (acute or chronic), disorder, injury or trauma’.15 As such, a health condition ‘may also include other circumstances such as pregnancy, ageing, stress, congenital anomaly or genetic predisposition’, where rehabilitation may be required ‘by anyone with a health condition who experiences some form of limitation in functioning, such as in mobility, vision or cognition’.15 Furthermore, rehabilitation is ‘characterised by interventions that address impairments, activity limitations and participation restrictions, as well as personal and environmental factors (including assistive technology) that have an impact on functioning’.15 Rehabilitation, particularly because it is a resource-intensive model of care, is indicated for many pathologies (eg, quadruple burden of disease), and its access is challenged across many settings,14 19 is considered a timely vehicle to further explore the notion of ‘LRSs’ comprehensively.
Data sources and search strategy
Four electronic databases were accessed and searched within the 5 years preceding 24 June 2019: PubMed, Africa-Wide, Web of Science and Scopus. A search strategy for each database (online supplemental file 1) was developed in collaboration with a medical librarian to identify studies. The use of terminology related to rehabilitation components, conducted in LRSs, in the title, abstract or keywords, were included.
bmjgh-2021-005190supp001.pdf (35.6KB, pdf)
Study selection process
The initial screening of the identified article titles was done independently by two researchers (CvZ and MH). Potentially eligible titles and abstracts to be included for the second iteration of independent screening (CvZ and MH) were agreed on, following discussions on any discord in the initial screening results. These discussions were used to refine the in/exclusion criteria. A third researcher (SH) was available for review in the case of discordance between the aforementioned researchers. Subsequently, full-text review was done independently by two researchers (CvZ and MH) and agreement was reached on the final full-text articles included. No appraisal on risk of bias or methodological quality was conducted, as is consistent with the guidance provided on scoping review methodology.17
Data extraction and synthesis
A data extraction form was created to tabulate the description of the included studies by authors and publication dates, methodological design, disease profiles reported according to the Global Health Data Exchange,20 geographical location, World Bank income group in the year of the study publication,21 the setting’s most recent GINI index value,22 and a short synopsis of the rehabilitation model. Data extraction was performed by one researcher (CvZ) and verified by a second researcher (MH). The included articles were subsequently analysed using qualitative content analysis through an inductive approach.23 24 ATLAS.ti (https://atlasti.com/) software was used to store and organise the data during the process of abstraction and interpretation. This review made use of a research team comprising of four individuals: (1) a clinical physiotherapist and novice researcher, (2) a physiotherapist and senior academic with qualitative research expertise, (3) a physiotherapist and senior academic with vast experience in quantitative and qualitative research, and lastly, (4) a senior academic and experienced quantitative and qualitative researcher.
A combination of in vivo (ie, verbatim) and descriptive coding (ie, summarising the meaning of the extracted text into a word or short phrase) was used to analyse the included articles.25 The combination of these two coding techniques helped to identify the significance of the text as it was presented, but also allowed the opportunity for a degree of interpretation to grasp the underlying meaning of the information presented. All of the articles were coded, in their entirety, through multiple rigorous iterations, during which the first version of the codebook was developed and constantly refined. The full codebook is available (online supplemental file 2).
bmjgh-2021-005190supp002.pdf (416.5KB, pdf)
During the second cycle of coding, the use of a socio-ecological model was introduced to guide the process of grouping the codes into content categories.26 The socioecological model examines the ways in which multiple levels of influence can impact health outcomes including at the intrapersonal, interpersonal, institutional, community/society and policy levels of influence. Moreover, the socioecological model is widely adopted in public health practice as a guide to describe the interactive attributes of individuals and environments that lead to health outcomes.27 28 Although this framework was only introduced after the initial or first cycle of coding was completed (indicating inductive coding at origin), it provided the required starting point for organising and grouping codes into content categories in a systematic fashion, without affecting the source data (ie, codes). Six layers transpired that provided structure, with decreasing proximity to the patient, being (intra)personal, interpersonal, community, healthcare organisational, national and academic. The development of the content categories was based on a rigorous process in which the codebook was constantly refined and reflected on. To express the underlying meaning of the content, the same process was used to group content categories into major themes relating to the term ‘LRS’.
Patient and public involvement
Patients and public were not involved in the design and conduct of this review.
Results
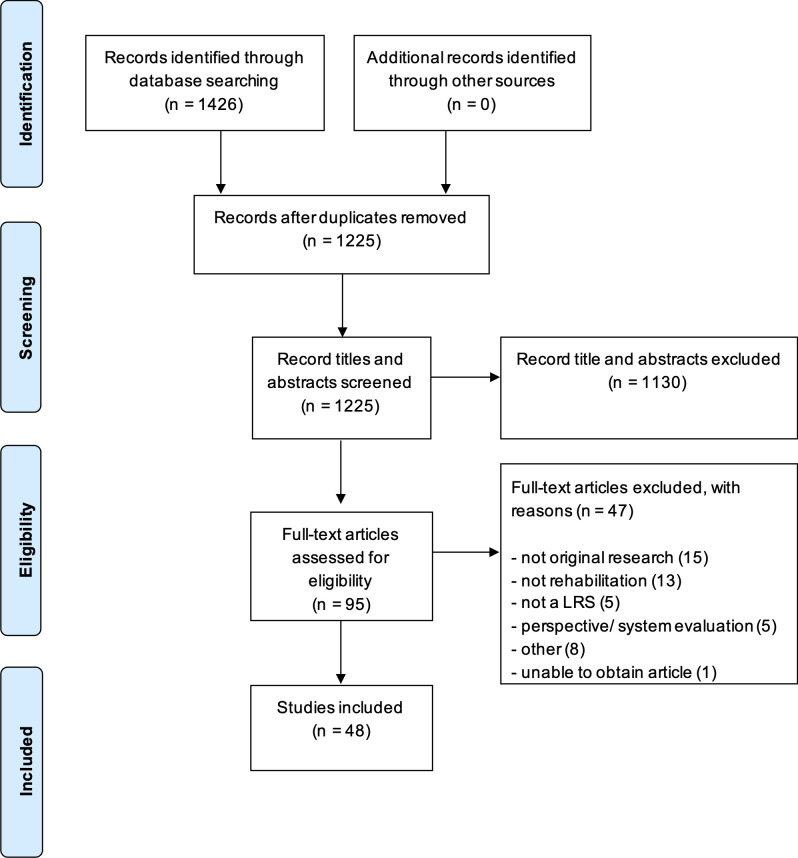
A total of 1426 articles were identified using the search strategy (figure 1). Of these, 48 articles met the selection criteria.29–76
Figure 1.
PRISMA flow chart. LRS, low-resource setting; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Description of the included studies
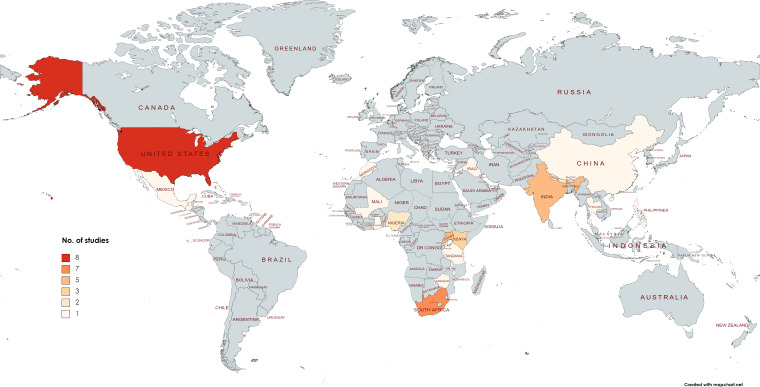
A detailed sample description of the included articles is tabulated in online supplemental file 3). Most studies used a randomised controlled trial design (n=18, 38%), followed by cohort studies (n=11, 23%), qualitative reports (n=8, 17%), cross-sectional studies (n=5, 10%) and others used a different design (n=6, 12%). The included articles reported on patients with non-communicable diseases (NCDs) (including cardiovascular, respiratory, neurological, mental disorders, etc; n=32, 68%), uncategorised (eg, obesity, persons with disabilities etc; n=10, 21%), communicable, maternal, neonatal and nutritional diseases (n=4, 9%) and injuries (n=1, 2%). The World Bank income groups in the year of study publication included lower-middle-income countries (n=14, 31%), upper-middle-income countries (n=13, 28%), low-income countries (n=11, 24%) and a high-income country (n=8, 17%). The highest GINI index, where 100 would mean the highest level of inequality, was 63 (South Africa) and the lowest value was 29 (Kosovo). The IQR showed that 50% of the studies fell in the range of 38 to 45. Figure 2 presents a density map of countries in which ‘low-resource’ settings were described.
Figure 2.
Density map of countries in which ‘low-resource settings’ were described.
bmjgh-2021-005190supp003.pdf (80.8KB, pdf)
Content category and theme descriptions
A total of 410 codes were grouped into 63 unique content categories, across six layers of the socioecological model. Grouping the 63 categories created nine themes relating to the term ‘LRS’ in the context of rehabilitation. The layers of the socioecological model display the content categories among multiple levels of influence in LRSs. Each theme is individually described, in no specific order, and the collective is visually presented in figure 3. Table 1 provides a comprehensive overview of each content category, organised by theme (rows) and layers within the socioecological model (columns). The content category descriptions are a direct reflection of the underlying codes (see online supplemental file 4). Owing to the multiple levels of influence displayed in the socioecological model, as well as the multimodal and comprehensive nature of rehabilitation, content categories may be present in more than one theme.
Figure 3.
Nine major themes were identified that describe a low-resource setting.
Table 1.
Overview of the nine themes and their respective content categories, across the six layers informed by the socioecological model
| Theme | Layers of the socio-ecological model | |||||
| Personal | Interpersonal | Community | Healthcare organisational | National | Academic | |
| Financial pressure: Uncertainties regarding finances causing obstacles to, difficulties in and constraints to strengthening individual, group, national or societal welfare, economic growth or efficiency. | Financial hardship | Lack of family involvement | Difficulties in obtaining and/or retaining employment | Financial constraints | Dependency on government involvement in healthcare provision | Research funding challenges |
| Grant usage | Lack of resources for caregivers | Socio-economically disadvantaged | Economic variability | |||
| Subsistence/’blue collar’ type employment | National healthcare service delivery challenges | |||||
| Undernutrition | NGO involvement is necessary | |||||
| World Bank income groups | ||||||
|
Suboptimal healthcare delivery: Healthcare Service delivery is inconsistent and suboptimal across the socioecological model |
Pathological variance | Disease burden | Access barriers | Dependency on government involvement in healthcare provision | ||
| Communication gaps | Disease burden | |||||
| Heavy burden of care | National healthcare service delivery challenges | |||||
| Local healthcare system gaps | NGO involvement is necessary | |||||
| Suboptimal quality of care | ||||||
|
Underdeveloped infrastructure: Lack of development of physical and organisational resources, systems and facilities serving an area (eg, water, sanitation and electrical supply, roads and bridges, telecommunication networks, etc) |
Access to technology | Challenges with internet/mobile access | Access barriers | National healthcare service delivery challenges | ||
| Transport issues | Increasing internet/mobile access | Challenges with assistive devices | ||||
| Lack of basic services | Challenges with physical Resources | |||||
| Facility limitations | ||||||
| Insufficient technological resources | ||||||
|
Paucity of knowledge: A lack of knowledge, education, training, understanding and translation of concepts across and through the socioecological model. |
Lack of awareness | Lack of resources for caregivers | Low education Levels | Communication gaps | Knowledge gaps in published data/information | |
| Low education Levels | Language barriers | Providers lack adequate skills and knowledge | Limited context-specific information | |||
| Low health literacy | ||||||
|
Research considerations and challenges: Context-specific challenges and considerations when conducting research. |
Access to technology | Challenges with internet/mobile access | NGO involvement is necessary | Participant compensation strategies | ||
| Time constraints | Increasing internet/mobile access | Participant recruitment and retention strategies | ||||
| Transport issues | Setting-specific Research Design Challenges | |||||
| Setting-specific research design used | ||||||
|
Restricted social resources: The lack of tangible, material or symbolic exchangeable resources, within the available social network, (eg, information, goods, acceptance, love etc). |
Psychosocial challenges | Insufficient social support | Indigenous community structure | Demographic transition | ||
| Lack of family involvement | Inequality in community structures | Political instability | ||||
| Negative effects on caregiver well-being | Minority groups | |||||
| Sufficient social support | Socio-economically disadvantaged | |||||
|
Geographical and environmental factors: Factors related to the physical features/aspects of an area, the natural world and/or the impact of human activity on its condition. |
Transport issues | Environmental challenges | Challenges with assistive devices | Political instability | Participant recruitment and retention strategies | |
| Subsistence/’blue collar’ type employment | Geographical challenges | Participant recruitment and retention challenges | ||||
| Setting-specific research design challenges | ||||||
|
Human resource limitations: Lack of available different kinds of clinical and non-clinical staff responsible for public and individual health intervention. |
Lack of family Involvement | Heavy burden of care | ||||
| Lack of trained professionals | ||||||
| Scheduling Considerations | ||||||
|
Influence of beliefs and practices: Traditional, cultural and indigenous beliefs and practices may influence health care-seeking behaviours, perceptions of healthcare and inform healthcare practices. |
Influence of individual characteristics | Discrimination and stigma | Cultural influences | Participant compliance challenges | ||
| Indigenous community structure | Participant recruitment and retention strategies | |||||
| Minority groups | ||||||
Note that content categories can reflect across multiple themes. A detailed description of each content category can be found in online supplemental file 4.
It would be potentially misleading to infer explicit conclusions from a quantitative representation (eg, number or percentage) of the relative importance of themes. Simply because a specific resource-constraint is not mentioned across a number of articles, does not mean it is less relevant. For instance, this resource-constraints might biased by the fact that other resource constraints are highly prevalent in such settings.
NGO, non-governmental.
bmjgh-2021-005190supp004.pdf (121.7KB, pdf)
Theme 1: financial pressure
Financial uncertainties appear to be a core component when describing LRSs, reflected by the presence of content categories related to financial pressure in every layer of the socioecological model. The underlying content categories elucidate important factors contributing to uncertainties regarding financial resources such as insufficient income, lack of healthcare insurance, dependency on subsidised healthcare, unemployment, subsistence employment and undernutrition. These appear to directly affect an individual’s ability to access, engage and maintain rehabilitation strategies. Furthermore, our findings show that uncertainties around financial resources may restrict national, organisational and research initiatives which should inform and meet the needs of a setting.
The majority of the district’s population rely on health care provided by the state, age or disability pensions, and family members who go out to work to sustain the household. (South Africa, exercise program)64
Participants in our study reported that financial constraints limited access to institutional care and contributed to food scarcity, which affected full participation in the home-based rehabilitation intervention. (South Africa, home-based rehabilitation)35
Moreover, the lack of financial resources to govern the associated high cost of managing specific disease clusters, particularly those with increasing incidence and prevalence in these settings, may stretch the burden on health systems already failing to optimise health outcomes.
The increasing prevalence of diabetes and the associated cost of managing this complicated disease have a significant impact on public health outcomes and health expenditures. (USA, mobile health intervention)33
Theme 2: suboptimal healthcare service delivery
Five of the 11 content categories which contributed to the development of this theme, were allocated to the organisational layer of the socioecological mode (in this case, organisation of healthcare). We have observed that the six remaining content categories allocated within the personal, community and national layers of the socio-ecological layer, may also influence the quality of healthcare service delivery. Barriers to delivering care in LRSs are multidimensional and include issues with access to healthcare, communication gaps, heavy burden of care, gaps in the existing healthcare system and suboptimal quality of care.
…disorders are often poorly managed and treated, particularly in marginalized, impoverished areas, where the mental health gap and the treatment gap can reach 90%. (Morocco, mental health rehabilitation)51
Information and assistance in accessing health care services once the patient has been discharged into the community are also difficult to obtain. Patients and caregivers report not routinely being provided with information on how to access the next step in the sequence of care. (USA, community transition program)52
Service delivery may further be hindered by relatively high disease burden, high prevalence of complications and different pathologies in these settings:
Racial and ethnic minorities bear a disproportionate burden of the diabetes epidemic, along with poor diabetes control and higher complication rates. (USA, undergraduate volunteers as patient partners)55
Theme 3: underdeveloped infrastructure
The lack of fundamental physical and organisational resources, facilities, systems and services necessary for these settings to function adequately, was multifaceted. At a personal level, the lack of basic amenities and services may influence ability to travel, ability to work, the execution of rehabilitation strategies, quality of life and accessibility of healthcare services. Service delivery and access to care on a national and healthcare organisational level appeared impeded by non-existent, underequipped and underdeveloped facilities and a lack of physical and technological resources, including assistive devices.
…the changes in physical activity levels among the urban populace is not reflected in low-resourced communities due to a lack of facilities, a safe environment, and poverty. (South Africa, exercise intervention)61
Rural populations in India are primarily served by non-governmental organizations (NGOs) that are not well-equipped because of little financial support from the government and infrastructures that are inadequate for serving most of India’s population (68.84%), which is located in rural areas. (India, behavioural management program)54
Interestingly, the emerging use of mobile devices and increasing internet connectivity in these settings, has pioneered opportunities for alternative and innovative research initiatives and rehabilitation solutions:
Such programs would take advantage of increased use of smartphones and tablets within the community among children and adolescents. (Uganda, cognitive rehabilitation)31
Yet, the reality of major challenges with mobile access and reliable and affordable internet connectivity, creates obstacles in employing these types of rehabilitation strategies:
…the poor quality and high cost of internet connections interfered negatively with some participants’ motivation to engage in the sessions… (South Africa, computer-based rehabilitation)39
Theme 4: paucity of knowledge
A lack of knowledge, education, training and understanding of concepts was found across five of the six layers of the socioecological model in LRSs. This was mostly evident in the personal, interpersonal and community levels, where the lack of education (illiteracy, low literacy, low education levels, low numeracy, etc), awareness and health literacy may be significant barriers to healthcare service delivery and individual disease management. Furthermore, barriers imposed by communication gaps between patients and practitioners were created by the limited use of lay or local language and insufficient health education or information.
… due to low literacy levels, including health literacy, that are associated with low education attainment. Low literacy could affect the ability to process and understand information. The effects of low literacy could be exacerbated by the lack of previous participation in structured diabetes education programmes and the fact that not all nutrition education sessions were offered in the local language. (South Africa, nutrition education)58
This may be further exacerbated by the fact that available professionals were insufficiently trained and lacked the necessary skills and knowledge to address specific or shifting needs:
…health workers often lack adequate knowledge about how to effectively manage patients with diabetes… (Nigeria, patient-education)38
…in many parts of China, especially in rural regions, where there are few health professionals specifically trained in recognition and management of stroke-related complications. (China, care-giver delivered stroke rehabilitation)76
Moreover, the absence of published and context-specific information remains a barrier to understanding and informing rehabilitation implementation in a large portion of LRSs:
There are as yet no published data on the non-pharmacological therapy of this debilitating disease from the rural developing world. (India, pulmonary rehabilitation)32
Theme 5: research challenges and considerations
Conducting research within these settings came with context-specific challenges and considerations; challenges and considerations that may be paramount in the quality of research and development of new knowledge in these settings. Researchers had to adapt to culturally appropriate (familiar concepts and motifs), feasible and context-specific (use of local language, oral or thumbprint consent due to illiteracy, easy to understand material due to low education levels, etc) research methodologies and approaches to pursue research aims. In addition, challenges and considerations ranged from logistical, geographic, transport difficulties, unreliable contact details, innovative recruitment strategies and adapting the timing of interventions to suit the practices of the setting.
A one day village-wide announcement, facilitated by the village head (traditional ruler) of Tsakuwa was utilized to recruit patients with nonspecific chronic low back pain… (Nigeria, exercise and education program)47
Additionally, reference to the need for and development of high-quality, evidence-based and context-specific rehabilitation tailored to the environment was reiterated:
Given the limited therapeutic resources and lack of trained professionals, systematic and resource-effective treatment programmes are needed which are context appropriate. (South Africa, expressive arts and counselling)73
Theme 6: restricted social resources
The availability of social resources may indirectly or directly influence health status and the management of health threats in these settings. These resources may be concrete or symbolic items that can be exchanged among people and may include information, services, affection or love, acceptance and societal status.77
In South Africa many social and economic barriers prevent survivors of sexual abuse from gaining access to the treatment they need… (South Africa, expressive arts and counselling)73
The content categories which contributed to the development of this theme and affect the availability of these resources include inequality within community structures, personal psychosocial factors, political instability and national demographic transition. Insufficient social support was clearly defined as a barrier to rehabilitation in this theme, with clear reference to the lack of and need for sufficient social support within LRSs:
…many participants were worried about their social and financial problems during the treatment and asked Kosova Rehabilitation Centre for Torture Victims to help them to access official or other social support. (Kosovo, cognitive-behavioural therapy)74
In contrast, studies which incorporated strategies targeted at improving social support, found that sufficient social support is possible and a facilitator to rehabilitation in LRSs:
Some of the participants felt further encouraged by the support of family members and, in return, showed a desire to get their families and other community members involved in the exercises. (South Africa, home-based rehabilitation)35
Theme 7: geographical and environmental factors
Our findings suggest that factors related to the geographical features of an area, the natural world and/or the impact of human activity on its condition, were components of these settings which need to be considered. Remoteness and rurality were factors commonly referred to, but certain settings were still deemed as ‘low resource’, despite semiurban or urban characterisation. Mention of travel distance, the types of travel terrain and subsistence/blue collar employment all related to the geographical and environmental factors contributing to the context of the setting. These factors were deemed particularly important when considering the accessibility of rehabilitation services and when issuing assistive devices. Geographical and environmental factors differ from area to area and present their own distinctive barriers and rehabilitation adaptations, within the context:
Because of the distances needed to travel in the rural mountainous region, the majority of encounters were provided in the form of phone visits.’ (USA, community transition program)52
There are not many outpatient therapy departments in the remote parts of the country… (India, home-based rehabilitation)63
Theme 8: human resource limitations
The shortage of different kinds of clinical and non-clinical staff responsible for public and individual health intervention emerged consistently. This reportedly contributes to the heavy burden of care and negatively impacts the time spent with individuals during their care:
Across the continent there are very few neurologists, geriatricians, or psychiatrists and an estimated 200 times fewer trained mental health workers per 100 000 people compared to high-income countries (Tanzania, cognitive stimulation therapy)62
There are also less than 30 000 doctors in Nigeria today and the approximate average doctor: patient ratio of 1:53 333 indicates that their time should not be spent on educational programmes… (Nigeria, patient-education)38
Strategies and rehabilitation techniques which focused on task shifting or tapping into unrealised human potential (volunteers, peer-led programmes, support persons or family involvement), to address the unmet need for a rehabilitation workforce, were often a specific focus:
This is potentially a scalable and sustainable model for health care centers in low-resource settings and provides volunteer opportunities for patients who successfully complete community health worker-led diabetes self-management education programs and would like to support other patients grappling with diabetes.” (USA, diabetes self-management program)69
Task shifting rehabilitation activities to unpaid caregivers might offer a sustainable alternative to conventional rehabilitation (India, home-based rehabilitation)56
Theme 9: influence of beliefs and practices
Traditional, cultural and indigenous diversity appear to be important features of LRSs. As such, these characteristics may influence healthcare-seeking behaviours, perceptions of healthcare and inform healthcare practices. Our observations suggest that personal attitudes and beliefs may affect healthcare behaviours in any setting. Yet, the existence of disease-related and disability-related stigma, use of traditional medicine and specific cultural influences may have particular implications for the planning, execution and understanding of health systems, research and policies in LRSs:
Stroke survivors often resort to alternative forms of treatment and refuse orthodox care due to highly prevalent stroke related stigma. (Ghana, tele-rehabilitation program)67
Many people in the community believe that children with intellectual disabilities can transfer their disabilities to other children. (India, behavioural management)54
Recognising and acknowledging potential gaps in health knowledge, facilitated by deep contextual understanding, may potentially improve health outcomes, without undermining or discrediting the beliefs of the communities being served:
…most rural dwellers in Nigeria have poor knowledge of the roles and scope of physiotherapy, poor health care-seeking behaviour, and patronize traditional health workers. (Nigeria, exercise plus education program)47
Discussion
From the 48 articles included in this review, we have identified 63 different resource categories culminating into nine different themes that characterise LRSs. The themes that were developed from the data describe resource limitations at a personal, interpersonal, community, healthcare organisational, national and academic level. To our knowledge, this review is the first systematic and rigorous attempt to unravel the term ‘LRS’.
A complex network of interrelated concepts
The provision of healthcare, and the health systems through which health interventions are provided, is complex, dynamic and context-specific.78 79 The themes that have emerged from this study clearly demonstrate that the lack of ‘resources’ within LRSs requires a holistic frame of mind. Using the socioecological model to guide the grouping of codes into content categories emphasised the fact that there are multiple actors and levels of influence in the provision of comprehensive healthcare interventions in LRSs. Moreover, some resource constraints span across different levels of the socioecological model (eg, financial constraints are not merely experienced at the level at which healthcare is organised). Therefore, the themes are not unidimensional or dichotomous (ie, adequate vs inadequate), yet rather reflect a complex network or spectrum of interrelated resource limitations and concepts which inform a ‘setting of low resource’. While our analysis highlights the diversity and complexity of actors and determinants that describe a setting—as it is—it fails to provide a thorough analysis on the processes of interaction between themes, content categories and layers within the socio-ecological model. In other words, the level by which resource constraints impact healthcare delivery and quality is, in part, a product of these interactions and the ways in which they are governed within the different levels of the healthcare system (institutional vs stakeholders vs policy and regulations).80 Addressing a single ‘resource’ is unlikely to result in the provision of quality care, as each factor should be recognised as equally necessary, yet equally inadequate on their own.81 We would like to note that due to the nature of our inquiry, the themes predominantly highlight resource ‘shortages’. However, it is reassuring that the literature also supports the role of LRSs, including their specific challenges, as an opportunity to develop new and innovative approaches to healthcare.
The country classification by the World Bank into LMIC is often used in conjunction with LRSs. This review indicates that there is no mandate to make inferences about a specific country or setting, in terms of healthcare delivery and/or quality, on the premises of being a LMIC alone. Yet, it also recognises that the use of umbrella terms for the sake of generalisability is common practice in public and global health research. However, caution needs to be exercised when using umbrella terms (eg, LMIC, LRSs, low/middle-income countries) without adequate consideration of the complexity that each term entails. The use of LMIC (135 or 60% of economies globally) as an umbrella term21 is based on economic metrics alone. Moreover, inference that all healthcare in high-income countries is therefore fully resourced to meet population needs, is unsupported.13 The latter is further strengthened by the finding that almost one fifth of the studies in our sample were, in fact, from a high-income country (17%). Alternatively, ‘low/middle-income countries’, a classification based on the human development index (a statistical composite index based on life expectancy, education and per capita income indicators) may be more reflective of the underlying complexities that differ between countries or settings, yet fails to recognise differences related to healthcare per se. Moreover, the use of low/middle-income countries’ as an umbrella term would ignore that healthcare challenges persist in countries that are considered ‘developed’, for instance, driven by agglomeration of people living in poverty, proximity to healthcare infrastructure (ie, rurality), or rapid migration due to conflict, among others. Hence, the term LRSs, as the subject of this review, provides a more open concept and is subject to interpretation, yet the specific resource-constraints need to be adequately described to avoid make-shift underlying assumptions that are not supported, hamper knowledge transfer or promote invalid conclusions.
Social determinants of health
WHO2 defines social determinants of health as ‘the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life’. Furthermore, WHO states that social determinants of health are mainly responsible for health inequalities, including inequity. In other words, one could argue that a holistic view of the context in which healthcare is provided, is paramount in light of improving health equity, and that the biggest gains in health may not necessarily be achieved by improving healthcare alone. Interestingly, various social determinants of health are clearly reflected in many of the derived content categories (insufficient social support, low education levels, employment difficulties, etc) underlying the nine proposed themes. In consequence, one could argue that part of the way forward in tackling the unmet need for rehabilitation specifically, can be found in addressing one or more social determinants of health, rather than upscaling the availability of rehabilitation per se. Addressing such social determinants could include tackling income inequality/poverty, healthcare organisational service delivery challenges, restriction in social resources and education disparities, among others.82
Some of the key health inequalities which have been associated with adverse social determinants of health include life expectancy (particularly in children), maternal mortality and prevalence of communicable disease (specifically tuberculosis).2 While being cognisant of the burden of communicable disease, what remains a concern, is the fact that 87% of premature deaths in LMICs occur as a result of NCDs. In addition, the high cost of disease management associated with NCDs is propelling around 100 million people into poverty, annually.2 This is further supported by reports of exacerbating poverty due to high costs of care and reducing healthcare access for those without any or sufficient healthcare insurance, as a result of the dependency on out-of-pocket expenditure.9 Maintaining an increase in government health spending is imperative as it could supply funding for vital health services and could indirectly influence other health outcomes by reserving household finances for different health determinants, like education and nutrition.9 However, it should be noted that increasing health expenditure, does not necessarily translate to improvements in healthcare access, quality or outcomes.9 Furthermore, perhaps alternative healthcare expenditure models can be considered that are more reflective of the local context than conventional models. Such contemporary models may include innovative approaches to rehabilitative care (eg, community-orientated primary care, use of community healthcare workers, etc). Many of the included articles in this study used rehabilitation models, specifically designed for the disproportionately affected populations, which were directed at the prevention of the progression of disease, prior to the development of incapacitating symptoms or dangerous episodes.83 Many of these models included innovative approaches (eg, task-shifting) and were aimed at cost-effectiveness. Better understanding of the context in which these models were studied may aid knowledge translation between settings.
A way forward
The nine major themes identified in this review, have the potential to assist in strengthening the evidence base and knowledge transfer between LRSs. Irrespective of geographical location and proximity to one another, each setting is complex in many aspects (culturally, environmentally, socially and structurally). In other words, each setting is a unique reflection of the interaction of a spectrum of resources, and no umbrella term will be able to grasp this complexity in a satisfactory manner. Determining the transferability of our themes beyond the field of rehabilitation could potentially be addressed by developing a structured way of auditing the setting in which a specific study is conducted—subsequently allowing for more in-depth analyses on the relative contribution of specific resource constraints on healthcare provision in a specific setting,
While the use of umbrella terms like ‘LMICs’ or ‘LRSs’ can be useful in parsimony and generalisability, it is paramount that the nuance and meaning underlying these terms are better addressed, in both primary and secondary research. While we do not advocate for complete abstinence of terms such as LMIC, we do challenge the use of these terms without providing sufficient nuance. The themes identified in this review merely aim to prompt researchers, clinicians, policy-makers and other stakeholders, to actively consider the complex context in which their work, or that of others, is embedded. Moreover, if setting-related and research-related challenges and considerations are more explicitly recorded when conducting research in these settings, the external validity of the findings may be safeguarded, and the underlying assumptions when using umbrella terms can be challenged. This review may be a first step towards the development of support structures, through the development of consensus statements and/or reporting frameworks that promote sound and structured reporting of context (in LRSs and beyond), as well as theory development.84
Limitations
There are some limitations to this study. First, somewhat surprisingly, our search strategy did not identify any articles from countries on the South American continent. While cognisant of the weak association between income classification and resource-constraints described earlier, this may present a gap, as two-thirds of Latin America’s population can be allocated to low-income or lower-middle income strata.85 In part, this could be a reflection of the applied language limitations (ie, English), and omitting pearling or the inclusion of region specific databases like Latin American and Caribbean Health Sciences Literature (LILACS). Though, given the level of data saturation reached during the coding process, it is plausible that no further or different themes may have emerged had we added more articles. Second, the search underlying this review dates back >1 year at time of publication. An update of the search was considered, but decided against for three reasons, namely (1) by renewing the search, one would need to step away from the inductive approach (ie, one cannot ‘unlearn’), (2) one can contest that more articles would not have led to new themes (ie, saturation) and (3) one can expect a high influx of studies pertaining to COVID-19. Third, this review was specifically focused on rehabilitation medicine, due to the background of the review team, as well as the holistic nature of rehabilitation. Given the complex nature of LRSs, as well as the multifacetted components of rehabilitation interventions, one would need to ascertain whether the findings presented here relate solely to the setting, or whether the nature of rehabilitation influenced the concept of an LRS derived from this review. It possible that the width of themes may not apply in situations that do not require the same extent of resources. That being said, the choice of rehabilitation in this study is considered a strength, as it highlighted the broad complexity of this problem. Due to the multidisciplinary, multimodal and comprehensive nature of rehabilitation, there is a stronger likelihood of identifying aspects of LRSs that would otherwise have been missed. An important step would be to explore the level of saturation in our themes when mirrored against other fields of study, particularly due to the combination of the complex natures of both rehabilitation and LRSs. In our view, these findings may serve as a platform for more specific or niched studies in this field. Fourth, the organisation of codes into content categories, and content categories into themes, was driven by the socioecological model that transpired after the initial coding process was completed. Choosing a different model to guide the development of content categories and themes may have altered the structure, however, arguably, it would have been unlikely that the content categories and themes themselves would have been altered. Finally, it is paramount that we recognise whose’ ‘voices’ we ‘analysed’. As this review reflects on academic contributions, the reported perception of resource-constraints may be biased based on the (specific) academic lens that was used, as well the authors’ history in working in the respective setting (eg, external contributors).86 Depending on the nature of the collaboration that led to the specific article, we need to be cognisant of potential colonial or power imbalances that may have driven that academic lens and the resulting resource-constraints identified.85 86 However, by pin-pointing the complexity that make up resource-constraints in healthcare, this review may also contribute to the changing rhetoric (or decolonisation) in both global and public health moving forward.87
Conclusion
The concept of ‘LRSs’, in the context of rehabilitation, can be described in line with nine themes including (1) financial pressure, (2) suboptimal healthcare service delivery, (3) underdeveloped infrastructure, (4) paucity of knowledge, (5) research challenges and considerations, (6) restricted social resources, (7) geographical and environmental factors, (8) human resource limitations and (9) influence of beliefs and practices. This review may lay the foundation for healthcare administrators, clinicians, researchers and other stakeholders, to move away from assumptive umbrella terms, and more actively and purposefully engage with resource limitations in their respective context. Furthermore, improving understanding of the concept of LRSs may aid in the transferability of research findings from one setting to another, through improved transparency and reporting.
Footnotes
Handling editor: Seye Abimbola
Twitter: @m_heine01
Contributors: MH conceived the review. CvZ had primary responsibility over the data extraction, qualitative analysis, and drafted the first manuscript. MB provided expert guidance in qualitative methods. All authors (CvZ, MB, SH and MH) developed the review procedures, interpretation of review findings, and reviewing the draft manuscript. All authors approved the final manuscript.
Funding: The funder (AXA Research Fund) of the study had no role in study design, data extraction, data analysis, data interpretation or writing of the report. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Map disclaimer: The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All data has been derived from published work; the full data codebook is available as online supplemental information.
References
- 1.Barreto ML. Health inequalities: a global perspective. Cien Saude Colet 2017;22:2097–108. 10.1590/1413-81232017227.02742017 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation . WHO | social determinants of health. WHO, 2020. Available: http://www.who.int/social_determinants/en/ [Accessed 31 Aug 2020].
- 3.Marmot M, Allen J, Bell R, et al. Who European review of social determinants of health and the health divide. Lancet 2012;380:1011–29. 10.1016/S0140-6736(12)61228-8 [DOI] [PubMed] [Google Scholar]
- 4.Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action 2015;8:27106. 10.3402/gha.v8.27106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kawachi I, Subramanian SV, Almeida-Filho N. A glossary for health inequalities. J Epidemiol Community Health 2002;56:647–52. 10.1136/jech.56.9.647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chorwe-Sungani G, Chipps J. A systematic review of screening instruments for depression for use in antenatal services in low resource settings. BMC Psychiatry 2017;17:112. 10.1186/s12888-017-1273-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grace SL, Turk-Adawi KI, Contractor A, et al. Cardiac rehabilitation delivery model for low-resource settings: an international Council of cardiovascular prevention and rehabilitation consensus statement. Prog Cardiovasc Dis 2016;59:303–22. 10.1016/j.pcad.2016.08.004 [DOI] [PubMed] [Google Scholar]
- 8.Aranda-Jan CB, Jagtap S, Moultrie J. Towards a framework for holistic contextual design for low-resource settings. International Journal of Design 2016;10:43–63. [Google Scholar]
- 9.Global Burden of Disease Health Financing Collaborator Network . Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995-2050. Lancet 2019;393:2233–60. 10.1016/S0140-6736(19)30841-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holt R. Ru 486/prostaglandin: considerations for appropriate use in low-resource settings. Law Med Health Care 1992;20:169–83. 10.1111/j.1748-720x.1992.tb01185.x [DOI] [PubMed] [Google Scholar]
- 11.Stucki G, Bickenbach J, Gutenbrunner C, et al. Rehabilitation: the health strategy of the 21st century. J Rehabil Med 2018;50:309–16. 10.2340/16501977-2200 [DOI] [PubMed] [Google Scholar]
- 12.Cochrane collaboration. Available: https://rehabilitation.cochrane.org/evidence
- 13.Kamenov K, Mills J-A, Chatterji S, et al. Needs and unmet needs for rehabilitation services: a scoping review. Disabil Rehabil 2019;41:1227–37. 10.1080/09638288.2017.1422036 [DOI] [PubMed] [Google Scholar]
- 14.Pesah E, Turk-Adawi K, Supervia M, et al. Cardiac rehabilitation delivery in low/middle-income countries. Heart 2019;105:1806–12. 10.1136/heartjnl-2018-314486 [DOI] [PubMed] [Google Scholar]
- 15.World Health Organisation . Rehabilitation 2030: a call for action. meeting report. rehabilitation: key for health in the 21st century. The need to scale up rehabilitation. health information systems and rehabilitation 2017.
- 16.Siriwardhana C. Promotion and reporting of research from resource-limited settings. Infect Dis 2015;8:IDRT.S16195. 10.4137/IDRT.S16195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peters MDJ, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141–6. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 18.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 19.Heine M, Lupton-Smith A, Pakosh M. Exercise-based rehabilitation for non-communicable disease in low-resource settings - a systematic scoping review. BMJ Global Health 2019:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.IHME DATA . GBD results tool | GHDx. Institute for health metrics and evaluation, 2019. Available: http://ghdx.healthdata.org/gbd-results-tool [Accessed 10 Jun 2020].
- 21.The World Bank . World bank country and lending groups – world bank data help desk. the world bank, 2020. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Accessed 10 Jun 2020].
- 22.The World Bank . GINI index (world bank estimate) | data. world bank, development Research Group 2019:1.
- 23.Erlingsson C, Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med 2017;7:93–9. 10.1016/j.afjem.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graneheim UH, Lindgren B-M, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today 2017;56:29–34. 10.1016/j.nedt.2017.06.002 [DOI] [PubMed] [Google Scholar]
- 25.Saldaña J. The coding manual for qualitative researchers. 2nd edn. SAGE Publications Ltd, 2013. [Google Scholar]
- 26.Bronfenbrenner U. Environments in developmental perspective: Theoretical and operational models. In: Measuring environment across the life span: Emerging methods and concepts. Washington, DC, US: American Psychological Association, 1999: 3–28. [Google Scholar]
- 27.Golden SD, Earp JAL. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav 2012;39:364–72. 10.1177/1090198111418634 [DOI] [PubMed] [Google Scholar]
- 28.Baron SL, Beard S, Davis LK, et al. Promoting integrated approaches to reducing health inequities among low-income workers: applying a social ecological framework. Am J Ind Med 2014;57:539–56. 10.1002/ajim.22174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aikens JE, Trivedi R, Heapy A, et al. Potential impact of incorporating a Patient-Selected support person into mHealth for depression. J Gen Intern Med 2015;30:797–803. 10.1007/s11606-015-3208-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baruah U, Pandian RD, Narayanaswamy JC, et al. A randomized controlled study of brief family-based intervention in obsessive compulsive disorder. J Affect Disord 2018;225:137–46. 10.1016/j.jad.2017.08.014 [DOI] [PubMed] [Google Scholar]
- 31.Boivin MJ, Nakasujja N, Sikorskii A, et al. A randomized controlled trial to evaluate if computerized cognitive rehabilitation improves Neurocognition in Ugandan children with HIV. AIDS Res Hum Retroviruses 2016;32:743–55. 10.1089/AID.2016.0026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhattacharyya P, Ghosh R, Saha D, et al. The impact on health status in short- and long-terms of a novel and non-orthodox real-world COPD rehabilitation effort in rural India: an appraisal. Int J Chron Obstruct Pulmon Dis 2018;13:3313–9. 10.2147/COPD.S160665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burner ER, Menchine MD, Kubicek K, et al. Perceptions of successful cues to action and opportunities to augment behavioral triggers in diabetes self-management: qualitative analysis of a mobile intervention for low-income Latinos with diabetes. J Med Internet Res 2014;16:16. 10.2196/jmir.2881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caagbay D-M, Black K, Dangal G, et al. Can a leaflet with brief verbal instruction teach Nepali women how to correctly contract their pelvic floor muscles? J Nepal Health Res Counc 2017;15:105–9. 10.3126/jnhrc.v15i2.18160 [DOI] [PubMed] [Google Scholar]
- 35.Cobbing S, Chetty V. Participants' reflections on a home-based rehabilitation intervention for people living with HIV in KwaZulu-Natal, South Africa. J Assoc Nurses AIDS Care 2019;30:218–23. 10.1097/JNC.0000000000000009 [DOI] [PubMed] [Google Scholar]
- 36.Dambi JM, Jelsma J. The impact of hospital-based and community based models of cerebral palsy rehabilitation: a quasi-experimental study. BMC Pediatr 2014;14:301. 10.1186/s12887-014-0301-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Debussche X, Besançon S, Balcou-Debussche M, et al. Structured peer-led diabetes self-management and support in a low-income country: the ST2EP randomised controlled trial in Mali. PLoS One 2018;13:e0191262. 10.1371/journal.pone.0191262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Essien O, Otu A, Umoh V, et al. Intensive patient education improves glycaemic control in diabetes compared to conventional education: a randomised controlled trial in a Nigerian tertiary care hospital. PLoS One 2017;12:e0168835. 10.1371/journal.pone.0168835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ferreira-Correia A, Barberis T, Msimanga L. Barriers to the implementation of a computer-based rehabilitation programme in two public psychiatric settings. S Afr J Psychiatr 2018;24:24. 10.4102/sajpsychiatry.v24.i0.1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flood D, Hawkins J, Rohloff P. A home-based type 2 diabetes self-management intervention in rural Guatemala. Prev Chronic Dis 2017;14:E65. 10.5888/pcd14.170052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Foley P, Steinberg D, Levine E, et al. Track: a randomized controlled trial of a digital health obesity treatment intervention for medically vulnerable primary care patients. Contemp Clin Trials 2016;48:12–20. 10.1016/j.cct.2016.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Foley AR, Masingila JO. The use of mobile devices as assistive technology in resource-limited environments: access for learners with visual impairments in Kenya. Disabil Rehabil Assist Technol 2015;10:332–9. 10.3109/17483107.2014.974220 [DOI] [PubMed] [Google Scholar]
- 43.Giordani B, Novak B, Sikorskii A, et al. Designing and evaluating brain powered games for cognitive training and rehabilitation in at-risk African children. Glob Ment Health 2015;2:e6. 10.1017/gmh.2015.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haddad NS, Istepanian R, Philip N, et al. A feasibility study of mobile phone text messaging to support education and management of type 2 diabetes in Iraq. Diabetes Technol Ther 2014;16:454–9. 10.1089/dia.2013.0272 [DOI] [PubMed] [Google Scholar]
- 45.Hamid LN, Kobusingye O, Baine SO, et al. Disability characteristics of community-based rehabilitation participants in Kayunga district, Uganda. Ann Glob Health 2017;83:478–88. 10.1016/j.aogh.2017.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hasan AA, Callaghan P, Lymn JS. Evaluation of the impact of a psycho-educational intervention for people diagnosed with schizophrenia and their primary caregivers in Jordan: a randomized controlled trial. BMC Psychiatry 2015;15:72. 10.1186/s12888-015-0444-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ibrahim AA, Akindele MO, Ganiyu SO. Motor control exercise and patient education program for low resource rural community dwelling adults with chronic low back pain: a pilot randomized clinical trial. J Exerc Rehabil 2018;14:851–63. 10.12965/jer.1836348.174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Järnhammer A, Andersson B, Wagle PR, et al. Living as a person using a lower-limb prosthesis in Nepal. Disabil Rehabil 2018;40:1426–33. 10.1080/09638288.2017.1300331 [DOI] [PubMed] [Google Scholar]
- 49.Johnson MJ, Montes S, Bustamante K. TheraDrive in a robot gym: toward stroke rehabilitation beyond inpatient rehabilitation settings in USA and Mexico 2014:307–11.
- 50.Jones R, Kirenga BJ, Katagira W, et al. A pre-post intervention study of pulmonary rehabilitation for adults with post-tuberculosis lung disease in Uganda. Int J Chron Obstruct Pulmon Dis 2017;12:3533–9. 10.2147/COPD.S146659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Khabbache H, Jebbar A, Rania N, et al. Empowering patients of a mental rehabilitation center in a low-resource context: a Moroccan experience as a case study. Psychol Res Behav Manag 2017;10:103–8. 10.2147/PRBM.S117456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kitzman P, Hudson K, Sylvia V, et al. Care coordination for community transitions for individuals post-stroke returning to low-resource rural communities. J Community Health 2017;42:565–72. 10.1007/s10900-016-0289-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ku GMV, Kegels G. Effects of the first line diabetes care (FiLDCare) self-management education and support project on knowledge, attitudes, perceptions, self-management practices and glycaemic control: a quasi-experimental study conducted in the Northern Philippines. BMJ Open 2014;4:e005317. 10.1136/bmjopen-2014-005317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lakhan R. Behavioral management in children with intellectual disabilities in a resource-poor setting in Barwani, India. Indian J Psychiatry 2014;56:39–45. 10.4103/0019-5545.124712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee TC, Frangos SN, Torres M. Integrating undergraduate patient partners into diabetes self-management education: evaluating a free clinic pilot program for the underserved 2017;27:1689–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lindley RI, Anderson CS, Billot L, et al. Family-led rehabilitation after stroke in India (attend): a randomised controlled trial. Lancet 2017;390:588–99. 10.1016/S0140-6736(17)31447-2 [DOI] [PubMed] [Google Scholar]
- 57.Luyten A, Bettens K, D'haeseleer E, et al. Short-Term effect of short, intensive speech therapy on articulation and resonance in Ugandan patients with cleft (lip and) palate. J Commun Disord 2016;61:71–82. 10.1016/j.jcomdis.2016.03.006 [DOI] [PubMed] [Google Scholar]
- 58.Muchiri JW, Gericke GJ, Rheeder P. Impact of nutrition education on diabetes knowledge and attitudes of adults with type 2 diabetes living in a resource-limited setting in South Africa: a randomised controlled trial. J Endocrinol Metabol Diabetes S Af 2016;21:26–34. 10.1080/16089677.2016.1200324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Muchiri J, Gericke G, Rheeder P. Subjects’ experiences of a nutrition education programme: a qualitative study of adults with type 2 diabetes mellitus living in a rural resource-limited setting in South Africa. South Afr J Clin Nutr 2016;29:83–9. 10.1080/16070658.2016.1216511 [DOI] [Google Scholar]
- 60.Muchiri JW, Gericke GJ, Rheeder P. Effect of a nutrition education programme on clinical status and dietary behaviours of adults with type 2 diabetes in a resource-limited setting in South Africa: a randomised controlled trial. Public Health Nutr 2016;19:142–55. 10.1017/S1368980015000956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Onagbiye SO, Moss SJ, Cameron M. Managing noncommunicable diseases in an African community: effects, compliance, and barriers to participation in a 4-week exercise intervention. Int Q Community Health Educ 2016;36:165–76. 10.1177/0272684X16647357 [DOI] [PubMed] [Google Scholar]
- 62.Paddick S-M, Mkenda S, Mbowe G, et al. Cognitive stimulation therapy as a sustainable intervention for dementia in sub-Saharan Africa: feasibility and clinical efficacy using a stepped-wedge design. Int Psychogeriatr 2017;29:979–89. 10.1017/S1041610217000163 [DOI] [PubMed] [Google Scholar]
- 63.Pandian JD, Felix C, Kaur P, et al. FAmily-Led rehabilitation aftEr stroke in India: the attend pilot study. Int J Stroke 2015;10:609–14. 10.1111/ijs.12475 [DOI] [PubMed] [Google Scholar]
- 64.Puckree T, Balance NP. And Stability–Focused exercise program improves stability and balance in patients after acute stroke in a resource-poor setting. PM&R 2014;6:1081–7. [DOI] [PubMed] [Google Scholar]
- 65.Rispin K, Wee J. Comparison between performances of three types of manual wheelchairs often distributed in low-resource settings. Disabil Rehabil Assist Technol 2015;10:316–22. [DOI] [PubMed] [Google Scholar]
- 66.Rispin K, Wee J. A paired outcomes study comparing two pediatric wheelchairs for low-resource settings: the regency pediatric wheelchair and a similarly sized wheelchair made in Kenya. Assistive Technology 2014;26:88–95. [DOI] [PubMed] [Google Scholar]
- 67.Sarfo FS, Adusei N, Ampofo M. Pilot trial of a tele-rehab intervention to improve outcomes after stroke in Ghana: a feasibility and user satisfaction study. Journal of the Neurological Sciences 2018;387:94–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seshan V, Muliira JK. Effect of a Video-Assisted Teaching Program for Kegel’s Exercises on Women’s Knowledge About Urinary Incontinence. J Wound Ostomy Continence Nurs 2015;42:531–8. [DOI] [PubMed] [Google Scholar]
- 69.Spencer MS, Kieffer EC, Sinco B. Outcomes at 18 months from a community health worker and peer leader diabetes self-management program for Latino adults. Diabetes care 2018;41:1414–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tongsiri S, Ploylearmsang C, Hawsutisima K. Modifying homes for persons with physical disabilities in Thailand. Bull World Health Organ 2017;95:140–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tyson AF, Kendig CE, Mabedi C. The effect of incentive spirometry on postoperative pulmonary function following laparotomy a randomized clinical trial. JAMA Surgery 2015;150:229–36. [DOI] [PubMed] [Google Scholar]
- 72.Verusia C, Tanuja D, Simira M. Satisfaction and adherence of patients with amputations to physiotherapy service at public hospitals in KwaZulu-Natal, South Africa. Afr Health Sci 2015;15:450–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Visser M, du Plessis J. An expressive art group intervention for sexually abused adolescent females. J Child Adolesc Ment Health 2015;27:199–213. 10.2989/17280583.2015.1125356 [DOI] [PubMed] [Google Scholar]
- 74.Wang S-J, Bytyçi A, Izeti S. A novel bio-psycho-social approach for rehabilitation of traumatized victims of torture and war in the post-conflict context: a pilot randomized controlled trial in Kosovo. Conflict and Health 2017;10:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Washburn LT, Cornell CE, Phillips M. Strength training in community settings: impact of lay leaders on program access and sustainability for rural older adults. J Phys Act Health 2014;11:1408–14. [DOI] [PubMed] [Google Scholar]
- 76.Zhou B, Zhang J, Zhao Y. Caregiver-Delivered stroke rehabilitation in rural China: the recover randomized controlled trial. Stroke 2019;50:1825–30. [DOI] [PubMed] [Google Scholar]
- 77.Webel AR, Sattar A, Schreiner N. Social resources, health promotion behavior, and quality of life in adults living with HIV. Applied Nursing Research 2016;30:204–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nambiar B, Hargreaves DS, Morroni C, et al. Improving health-care quality in resource-poor settings. Bull World Health Organ 2017;95:76–8. 10.2471/BLT.16.170803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Samb B, Desai N, Nishtar S. Chronic diseases: chronic diseases and development 4 prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Comment Lancet 2010;376:1619–40. [DOI] [PubMed] [Google Scholar]
- 80.Abimbola S. Health system governance: a triangle of rules. BMJ Global Health 2020;5:3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Saini V, Garcia-Armesto S, Klemperer D. Drivers of poor medical care. The Lancet 2017;390:178–90. [DOI] [PubMed] [Google Scholar]
- 82.Donkin A, Goldblatt P, Allen J. Global action on the social determinants of health. BMJ Global Health 2018;3:e000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Richardson CR, Franklin B, Moy ML. Advances in rehabilitation for chronic diseases: improving health outcomes and function. The BMJ 2019:365. [DOI] [PubMed] [Google Scholar]
- 84.Green EP. 6 the role of theory in global health | global health research: designs and methods. Available: http://themethodsection.com/ebook/ [Accessed 18 Mar 2021].
- 85.United Nations - Economic Commission for Latin America and the Caribbean (ECLAC) . ECLAC: the region has underestimated inequality | press release | economic Commission for Latin America and the Caribbean, 2019. Available: https://www.cepal.org/en/pressreleases/eclac-region-has-underestimated-inequality [Accessed 5 Jul 2020].
- 86.Dimitris MC, Gittings M, King NB. How global is global health research? A large-scale analysis of trends in authorship. BMJ Glob Health 2021:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Khan M, Abimbola S, Aloudat T. Decolonising global health in 2021: a roadmap to move from rhetoric to reform. BMJ Global Health 2021;6:e005604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-005190supp001.pdf (35.6KB, pdf)
bmjgh-2021-005190supp002.pdf (416.5KB, pdf)
bmjgh-2021-005190supp003.pdf (80.8KB, pdf)
bmjgh-2021-005190supp004.pdf (121.7KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. All data has been derived from published work; the full data codebook is available as online supplemental information.