Abstract
Purpose of review
Severe acute respiratory syndrome coronavirus (SARS-CoV2) infection rates are currently occurring at alarmingly accelerated rates. There is also a long-standing and concurrent rise in the prevalence and severity of substance use disorders (SUD). Therefore, the intersection between these two conditions needs to be carefully considered to ensure a more effective delivery of healthcare.
Recent findings
Generally, those with SUDs are more likely to have higher risk social determinants of health factors. Therefore, these patients are more likely to have barriers that can create difficulties in following appropriate infection control measures which in turn increases the risk of exposure to SARS-CoV2. In addition, these individuals have higher rates of medical comorbidities which increases the risk of all adverse outcomes, including mortality, from SARS-CoV2 infection.
Summary
Individuals with SUDs are at increased risk of both contracting SARS-CoV2 infection and suffering from worse outcomes afterwards. Though these risks of adverse outcomes are specific of SARS-CoV2 infection, the risk of exposure to other infectious diseases is increased in this population too. Healthcare providers and policymakers should then consider how to better protect this at-risk population and alleviate this increased disease burden.
Keywords: coronavirus disease 2019, outcomes, risks, severe acute respiratory syndrome coronavirus, substance use disorders
INTRODUCTION
Severe acute respiratory syndrome coronavirus (SARS-CoV2) is a virus in the coronavirus family that causes coronavirus disease 2019 (COVID-19). The World Health Organization declared a global pandemic related to SARS-CoV2 in March 2020. At the end of 2020, it was estimated that the United States has documented over twenty million COVID-19 cases and over 400,000 total deaths with more than 100 million cases worldwide [1]. These increasing statistics are occurring concurrently with a systematic increase in the prevalence of opioid use disorders and in mortality rates associated with its consequences.
There is limited data at this time on how socioeconomic status, race, and other factors like history of substance use affect the rates of infection and possible outcomes [2▪▪]. However, it is generally observed that SARS-CoV2 disproportionately infects and COVID-19 disproportionately affects those with various preexisting conditions, such as diabetes, obesity, chronic lung disease, and hypertension [3▪▪,4]. Though current data estimates that up to 80% of SARS-CoV2 infections are asymptomatic or minimally symptomatic, individuals with these preexisting conditions are more likely to develop COVID-19 that is not only symptomatic, but more severe [2▪▪]. Patients with these preexisting medical conditions are also more likely to experience severe complications such as acute respiratory distress syndrome (ARDS), secondary bacterial pneumonias, septic shock and multi-organ failure [2▪▪]. Patients with substance use disorders (SUDs) have significantly higher rates of several preexisting conditions, including chronic liver and kidney disease, lung diseases, cardiovascular diseases, diabetes, obesity, and cancer. These individuals are also at higher risk of exposure and infection with SARS-CoV2 due to inadequate infection control measures in socially disadvantaged populations [2▪▪,3▪▪,5▪]. This increased risk of SARS-CoV2 infection is observed to be greatest in those with opioid use disorder and tobacco use disorders [3▪▪]. The likelihood of poorer outcomes with infection was also observed to be greater in those with lifetime diagnoses of SUDs than in those with newer diagnoses. Overall, those with SUDs were found to be about 30% more likely to require hospitalization due to severe symptomatic COVID-19 infections and were about 50% more likely to die of complications from their COVID-19 infections [3▪▪].
In addition, people with SUDs generally have poor access to healthcare services, face stigma when seeking care, and have been observed to receive a lower quality of care when brought to medical attention [2▪▪]. This data inherently suggests that those with SUDs are at higher risk of developing symptomatic COVID-19, as well as at greater danger of developing serious, and potentially fatal consequences of COVID-19.
Current statistics from the Substance Abuse and Mental Health Services Administration (SAMHSA), indicate that upwards of 164.8 million people use alcohol, tobacco, opioids, stimulants, or other illicit drugs in any given month. Further estimates state that, in a span of one year, an average of 47 million people used tobacco products, 139.8 million consumed alcohol, 43.5 million used marijuana, and 10.3 million people misused opioids [6]. The SAMHSA ultimately concludes that three out of five people over the age of 12 used some type of substance and that 20.3 million people met criteria for a diagnosis of a SUD [6]. According to the US Centers for Disease Control and Prevention, deaths related to overdose of all opioids have increased almost six times in the last 20 years. Given the novelty of SARS-CoV2 and COVID-19 and the paucity of current data on how substance use affects the risks of infection and possible outcomes, these numbers are staggering.
Box 1.
no caption available
Literature search
For this review, we performed two literature searches of PubMed to find articles. The first search used the keywords ‘COVID-19,’ ‘risks,’ and ‘substance use’ and the second search used the words ‘COVID-19,’ ‘outcomes,’ and ‘substance use.’ The search was not initially restricted by study design or language but was limited to articles published between January to December 2020. Review articles published in English were included. Full-text references cited in these articles were also researched for additional relevant studies. The inclusion criteria were on-topic articles discussing the effect of substance use on the risks of COVID-19 and its impact on outcomes after infection. The exclusion criteria were any study designs that were case reports, surveys, or study protocols, or articles that were not published in English. All authors reviewed the articles relevant to the topic and the decision to include or exclude studies was based on consensus after reviewing all the full-text articles. A total of 249 articles were identified from the two systematic literature searches. After excluding duplicates, the remaining 211 were screened. Of these, 199 were excluded as they were either off-topic or were case reports, study protocols, surveys, or otherwise contained in the final articles. Twelve articles remained for inclusion (Fig. 1).
FIGURE 1.
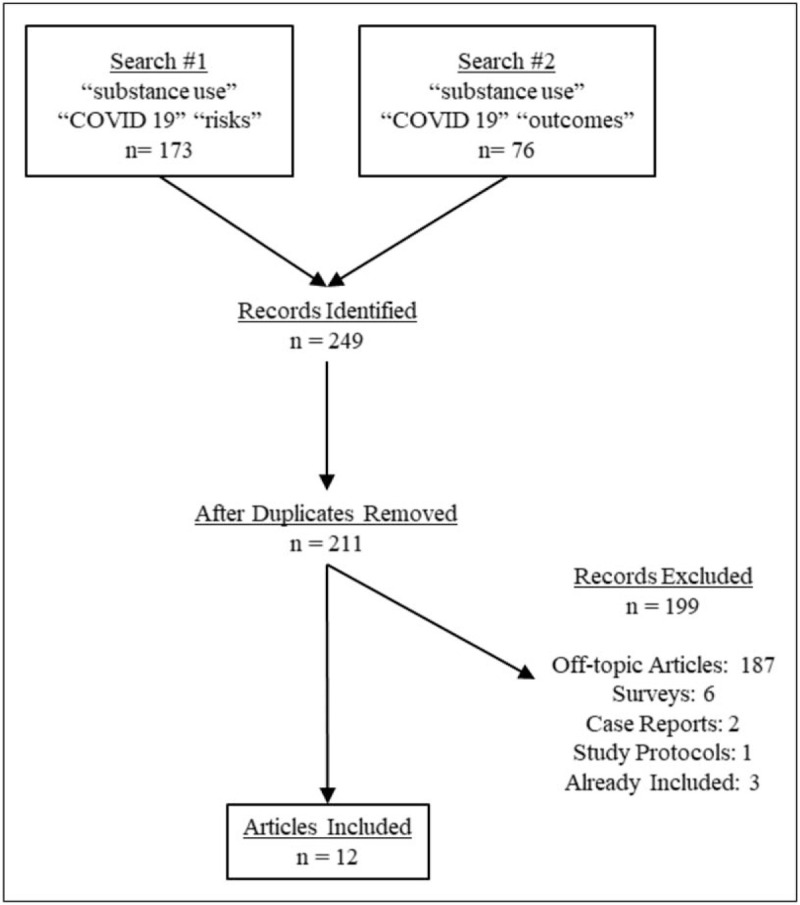
PRISMA flow diagram of included articles.
Four of the included articles were review articles, commentaries, or expert opinions and two were systematic literature reviews. The remaining six articles were an evidence-informed policy brief, a matched cohort study, an observational study, an online survey, a retrospective case-control study, and a retrospective review. Only a limited number of articles directly assessed patient data or outcomes [3▪▪,7,8,9▪,10].
SUBSTANCE USE AND RISK OF SEVERE ACUTE RESPIRATORY SYNDROME CORONAVIRUS TRANSMISSION
All the twelve included articles concluded, at least theoretically, that having a preexisting diagnosis of SUD increased the risk of infection with SARS-CoV2 [2▪▪,3▪▪,7,8,9▪,10,11▪–13▪,14–16]. Among those diagnosed with COVID-19, a significant proportion had diagnoses of SUDs [2▪▪,3▪▪,7,8,9▪,10,11▪–13▪,14–16]. This increased risk can be further stratified into socioeconomic disparities and medical comorbidities.
Effects of marginalization and homelessness
Those with SUDs are more likely to be of lower socioeconomic status and are thus more at risk of facing housing and other financial insecurities [2▪▪]. These disparities can result in a decreased ability to comply with physical distancing and quarantine or lockdown measures which directly increases their risk of SARS-CoV2 exposure and developing COVID-19 [2▪▪]. Similarly, those who reside in homeless shelters or prisons are also at increased risk of SARS-CoV2 exposure and contracting COVID-19 along with those who are migrant workers or otherwise marginalized [2▪▪,11▪,12▪]. Given the large proportion of individuals within these communities who have SUDs, this represents another factor contributing to the increased risk of infection [11▪,12▪]. Due to lockdown measures and social distancing protocols that were enforced, often for prolonged periods of time, the normal supply and access patterns of various substances were interrupted or altered [14]. This disruption may cause people with SUDs to seek new sources or increase the chances of multiple individuals sharing needles, joints, or other drug-associated paraphernalia which can increase risk of exposure to SARS-CoV2 and developing COVID-19 [14].
Effects of immune dysfunction
Generally, those with SUDs were also found to be more likely to have a compromised immune system [7,9▪,12▪,13▪]. A large proportion of individuals with SUDs have underlying immunosuppressive conditions such as HIV or liver cirrhosis secondary to hepatitis C infection, which can make them more susceptible to severe illness from viral pathogens [7]. The mucociliary function of those who smoke tobacco, marijuana, or other substances is often suppressed leading to increased susceptibility to any viral or bacterial respiratory infections [2▪▪,8,15]. Apart from these risks, there is also data that suggests that smoking increases expression of the angiotensin-converting enzyme type 2 receptor [12▪]. This increases the potential for virus entry into cells, further augmenting risk of infection [12▪]. Opioid use can also lead to suppression of immune function through inhibition of cytokine secretion and leading to immune cell dysfunction [13▪]. Several substances, such as nicotine and alcohol, have also been known to impede the normal function of the blood-brain barrier and increase susceptibility to central nervous infection [13▪].
SUBSTANCE USE AND OUTCOMES FROM COVID-19
Eleven of the twelve articles also concluded that a history of substance use increases the risk of most adverse outcomes from COVID-19 infection, including hospitalization due to severe disease and even death [2▪▪,3▪▪,7,8,9▪,10,11▪–13▪,14–16]Table 1. It was estimated that the increase in the risk of hospitalization due to complications from COVID-19 ranged as high as 50% [3▪▪,9▪]. This risk persisted even when adjusting for other confounding variables such as obesity and demographic characteristics and even when adjusting for preexisting conditions. A matched analysis based on demographic data and characteristics like obesity and diabetes, found an increased risk of hospitalization (32.5% vs 20.7%, OR = 1.84, 95% CI = 1.69–2.01), ventilator use (6.0% vs 4.2%, OR = 1.45, 95% CI = 1.22–1.72), and death (4.9% vs 2.8%, OR = 1.30, 95% CI = 1.08–1.56) among those who had a diagnosis of SUD prior to COVID-19 infection. The increased risk of hospitalization (30.9% vs 22.6%, OR = 1.53, 95% CI = 1.40–1.65) persisted even when individuals were matched based on several preexisting conditions such as hypertension, chronic obstructive pulmonary disease, heart disease, and cerebrovascular disease. In this population, however, there was not an observable increase in risk of mortality (4.7% vs 4.7%, OR = 1.00, 95% CI = 0.84–1.20) [9▪]. Individuals with SUDs were generally observed to have higher rates of several underlying health conditions, such as diabetes, cardiovascular diseases, cancers, chronic kidney disease, asthma and other respiratory diseases, hypertension, and obesity [2▪▪,3▪▪,11▪,12▪,8]. These diagnoses are generally associated with poorer outcomes following COVID-19 [2▪▪,3▪▪,11▪,12▪,8].
Table 1.
Summary of results from included articles
| Author | Pub. Date | Article/Study Type | Substance studied | Risks of infection | Risks of adverse outcomes |
| Melamed [2▪▪] | Jul-20 | Review/Commentary | - Multiple substances | - Socioeconomic barriers increase risk of virus exposure- Drug procurement can increase exposure | - High rates of smoking-associated lung disorders increase risk of adverse outcomes- Chronic SU causes immune dysfunction- SU increases risk of illness complications |
| Wang [3▪▪] | Jun-20 | Retrospective Case-Control Study | - Multiple substances | - Pts with SUD have significantly higher rates of COVID-19 infections; OUD pts had highest risk- Pharmacological effects of substances can increase rates of COVID-19 | - SUD pts had higher rates of asthma, kidney disease, COPD, diabetes, cancer, HIV, chronic liver disease, cardiovascular diseases- Hospitalization rates were much higher- Pharmacological effects of substances can increase COVID-19 adverse outcomes |
| Volkow [11▪] | Apr-20 | Review/ Opinion | - Opioid use disorder | - SUD pts are at increased risk of infection due to housing instability, incarceration, reduced access to healthcare and recovery support services- Prisons and homeless shelters are particularly high-risk environments- Social distancing/ quarantine increase sharing of drug equipment, overdose risk | - Severe COVID-19 infection occurs in those who are elderly and in those who are immunocompromised- Risk is increased in those with underlying health conditions like diabetes, cancer, heart, and respiratory diseases. These underlying diseases are common in those with SUD- SUD pts delay care and face stigma from medical systems |
| Dubey [12▪] | Jun-20 | Literature Review | - Multiple substances | - SUD pts at increased risk due to preexisting comorbid conditions, mucociliary dysfunction, immune dysfunction, socioeconomic barriers, poor healthcare access- Smoking increases expression of ACE which increases virion entry- SUD increased chance of high-risk behaviors like sharing needles etc., | - SUD pts delay care and face stigma from medical systems- Some data that nicotinic receptors modulate immune response and decrease risk of symptomatic infection- Increased risk of having premorbid conditions that increase risk of adverse outcomes- SUD pts have immune system dysfunction, vitamin deficiency, and increased risk of aspiration pneumonia- OU: respiratory depression and hypoxemia- MU: increased lung injury, pulmonary HTN |
| Schimmel [13▪] | Jul-20 | Review/Commentary | - Opioid use disorder | - Chronic OU causes immune dysfunction which increases risk of infection | - Respiratory toxicity from opioid use can worsen outcomes from lung infection |
| Wei [7] | Jul-20 | Literature Review | - Multiple substances | - Pts with SUD are vulnerable due to socioeconomic barriers | - Increased risk of HIV and hepatitis C; can cause immunosuppression- Smoking increases risk of COPD; leads to complications of COVID-19- OU: respiratory depression, hypoxemia- MU: increased lung injury, pulmonary HTN- Various substances have direct impacts on immune system function increasing risk of adverse outcomes from infection |
| Enns [14] | Sep-20 | Evidence-Informed Policy Brief | - Multiple substances | - Changes in SU patterns can be barriers to infection reduction- SU paraphernalia sharing increases risk of transmission | |
| Boschuetz [15] | Sep-20 | Online Survey | - Alcohol use disorder | - AU increases risk of medical comorbidities – increased risk of adverse outcomes | |
| Valecillo [8] | Oct-20 | Observational Study | - Multiple substances | - High risk behaviors (obtaining substances, sharing drug equipment, etc.) increase risk of exposure- Socioeconomic barriers (living in shelters, inability to maintain quarantine) can increase risk of transmission | - People with SUD have increased prevalence of cardiovascular and respiratory diseases, obesity, cirrhosis, chronic heart disease, diabetes, renal disease, hypertension, cancer which increase complications and mortality- Risk of hospitalization due to pneumonia was lower - attributed to lower median age |
| Rubin [16] | Oct-20 | Review/Commentary | - Multiple substances | - OUD: increased risk of COVID-19- SUD pts more likely to develop COVID-19 (AOR 8.7) | - People with SUD were more likely to be hospitalized and die from COVID-19 |
| Baillargeon [9▪] | Nov-20 | Matched Cohort Study | - Multiple substances | - Higher rates of infection due to homelessness, poor living conditions, having poor access to healthcare | - SUD increases risk of immunosuppression; increases risk of infection, adverse reactions- HTN, COPD, ischemic and cardiovascular disease increases risk of poor outcomes- Increased risk of adverse outcomes due to increased ACE expression- Prolonged alcohol use linked to mucociliary dysfunction, respiratory disease |
| Allen [10] | Dec-20 | Retrospective Review | - Multiple substances | - Pts with SUDs: higher risk of critical illness |
ACE, angiotensin-converting enzyme; AU, alcohol use; HTN, hypertension; MU, methamphetamine use; OU, opioid use; OUD, opioid use disorder; pts, patients; SU, substance use; SUD, substance use disorder.
In addition, the use of substances can directly impact the ability of the body to mount a successful immune response to COVID-19. Chronic smoking of tobacco products has long been established as a direct causative factor in the development of lung and cardiovascular diseases [11▪]. Furthermore, respiratory toxicity and suppression of pulmonary function through the use of opioids, methamphetamines, marijuana, or other substances can also lead to increased susceptibility of adverse outcomes [13▪]. The use of stimulants, such as methamphetamines or cocaine, has been linked to the development of adverse cardiovascular outcomes such as hypertension, cardiac ischemia, hemorrhage, or thromboembolic events [8]. One article mentioned a hypothetical association between nicotine and the blunting of an overwhelming immune response leading to better outcomes [12▪]. However, the use of any substances through smoking is generally understood to cause widespread inflammation, suppress immune function, and decrease the respiratory capacity to tolerate or surmount infections [8,12▪]. Sustained use of alcohol, cocaine, or methamphetamine has been linked to impaired immunity, disrupted pulmonary function, and increased potential for respiratory complications with infection, such as ARDS, pneumonia, or alveolar hemorrhage [8].
Accessing medical care
Due to various social and health barriers and widespread stigma, individuals with SUDs are also largely marginalized by the healthcare systems [2▪▪,11▪]. This may lead to a delay in obtaining necessary medical care, being deprioritized for care, or receiving a lower quality of medical care in general [2▪▪,11▪]. Due to new barriers created by lockdown measures and social distancing protocols that have disrupted many of the rehabilitation and support structures in place for those with SUDs, these individuals may experience an increase in the utilization of various substances or in rates of relapse [7]. This places an already at-risk population at even greater risk of contracting COVID-19 and suffering from adverse outcomes.
Possible lower rates of hospitalization due to confounding factors
Out of the twelve studies included, one inferred that there were lower rates of hospitalization from pneumonia after COVID-19 although those with SUDs were more likely to be diagnosed with COVID-19 [8]. Observational in nature, the study found a prevalence of only 1.3% of SUDs among those hospitalized with COVID-19 related pneumonia. This was attributed to a lower median age group of individuals with SUDs as those who suffered serious consequences were generally older with more preexisting conditions prior to infection. However, the limitations from a small sample size based in Europe and a relatively homogenous population, must be taken into consideration when drawing conclusions [8].
CONCLUSION
Generally, all the 12 included articles concluded that a preexisting diagnosis of SUDs increased the risk of contracting SARS-CoV2 and being diagnosed with COVID-19. This risk was generally attributed both to socioeconomic barriers disrupting and circumventing appropriate infection control measures and to direct consequences of obtaining and using substances. All articles also generally concluded that a preexisting diagnosis of SUDs led to an increased risk of adverse outcomes following COVID-19 diagnosis including hospitalization, intensive medical care, invasive ventilation, or even death. This increased risk of adverse outcomes was attributed to two factors; those with SUDs having a greater prevalence of medical comorbidities prior to SARS-CoV2 exposure and COVID-19 diagnosis and due to direct effects of substances on respiratory and immune function.
Despite these conclusions, there is a dearth of literature on this topic. Among the articles found, only five provided any quantifiable measures assessing risks of infection or adverse outcomes. Most articles found were commentaries, literature reviews, or expert opinion pieces. This relative lack of published literature to emphasize that COVID-19 is a relatively new area of research.
However, currently available data does indicate that there is a strong association between SUDs and the risk of both contracting SARS-CoV2 infection and suffering from more serious outcomes after infection. It is also worthwhile to note that the increased risks of infection in those with substance use are generally associated with barriers in social determinants of health, such as inability to follow social distancing and quarantine measures, associated stigma, and unhygienic practices like sharing drug paraphernalia. These risks are not specific to SARS-CoV2 infection and COVID-19 and indicate that individuals with SUDs are at increased risk for other infectious diseases too. For example, opioid use disorder has been shown to be a contributing factor in the rise of several other infectious diseases such as HIV, viral hepatitides, endocarditis, and other skin and soft tissue infections [17▪]. Cigarette smoking has been linked to a substantial increase in developing influenza, pneumococcal pneumonias, and most significantly, tuberculosis [18].
The results of this review indicate that individuals with SUDs are at increased risk of contracting SARS-CoV2 infection and COVID-19 and having increased morbidity and mortality with COVID-19 through similar mechanisms that predispose individuals with SUDs to other infectious disease processes. These risks are primarily attributable to increased socioeconomic disparities and other barriers related to social determinants of health. This points to several opportunities for intervention particularly from a public health standpoint. Given that these individuals are an at-risk population, providers may even consider vaccinating these individuals against most infectious diseases.
This is a rapidly evolving area with a lot of opportunity for future research. Given the increasing prevalence of SUDs, it is imperative that future studies continue to assess the intersections of substance use with infectious disease processes.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1. Worldometers.info. Coronavirus Cases: Worldometer. https://www.worldometers.info/coronavirus/. Published December 30, 2020. [Accessed 30 December 2020] [Google Scholar]
- 2▪▪.Melamed OC, Hauck TS, Buckley L, et al. COVID-19 and persons with substance use disorders: inequities and mitigation strategies. Subst Abus 2020; 41:286–291. [DOI] [PubMed] [Google Scholar]; This article provide an extensive overview of the various effects of substance use disorders on the risk of SARS-CoV2 exposure and developing COVID-19. The article outlines the increased risk of COVID-19 infection particularly due to socioeconomic barriers, the risk of adverse consequences, challenges in healthcare delivery, and the current state of research in this area.
- 3▪▪.Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry 2020; 26:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article provide an extensive overview of the various effects of substance use disorders on the risk of SARS-CoV2 exposure and developing COVID-19. The review outlines the increased risk of SARS-CoV2 infection and the risk of adverse outcomes after infection. The review article also stratifies these risks based on individual types of substance use disorders.
- 4.Robinson P. Long-term conditions and severe acute respiratory syndrome SARS-CoV-2 (COVID-19). Br J Community Nurs 2020; 25:247–251. [DOI] [PubMed] [Google Scholar]
- 5▪.Winhusen T, Theobald J, Kaelber DC, Lewis D. Medical complications associated with substance use disorders in patients with type 2 diabetes and hypertension: electronic health record findings. Addiction 2019; 114:1462–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article is a useful reference on understanding the interface between substance use disorders and SARS-CoV2 exposure and developing COVID-19. This article expands upon the specific medical comorbidities faced by those with type 2 diabetes and hypertension.
- 6. Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- 7.Wei Y, Shah R. Substance use disorder in the covid-19 pandemic: a systematic review of vulnerabilities and complications. Pharmaceuticals 2020; 13:1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vallecillo G, Perelló R, Güerri R, et al. Clinical impact of COVID-19 on people with substance use disorders. J Public Health (Oxf) 2021; 43:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9▪.Baillargeon J, Polychronopoulou E, Kuo YF, Raji MA. The Impact of Substance Use Disorder on COVID-19 Outcomes. Psychiatr Serv 2021; 72:578–581. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article is a useful reference on understanding the interface between substance use disorders and SARS-CoV2 exposure and developing COVID-19. It expands upon how preexisting diagnoses of substance use disorders affect COVID-19 outcomes after infection.
- 10.Allen B, El Shahawy O, Rogers ES, et al. Association of substance use disorders and drug overdose with adverse COVID-19 outcomes in New York City. J Public Health 2020; fdaa241.doi: 10.1093/pubmed/fdaa241. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11▪.Volkow ND. Collision of the covid-19 and addiction epidemics. Ann Intern Med 2020; 173:61–62. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article is a useful reference on understanding the interface between substance use disorders and SARS-CoV2 exposure and developing COVID-19. This article expands upon the ways in which the COVID-19 pandemic and addiction epidemics intersect and interact with each other.
- 12▪.Dubey MJ, Ghosh R, Chatterjee S, et al. COVID-19 and addiction. Diabetes Metab Syndr 2020; 14:817–823. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article is a useful reference on understanding the interface between substance use disorders and SARS-CoV2 exposure and developing COVID-19; some are also useful in describing how substance use disorders can affect the risks of exposure to other infectious processes
- 13▪.Schimmel J, Manini AF. Opioid use disorder and covid-19: biological plausibility for worsened outcomes. Subst Use Misuse 2020; 55:1900–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article is a useful reference on understanding the interface between substance use disorders and SARS-CoV2 exposure and developing COVID-19. This article expands upon the ways in which the COVID-19 pandemic and addiction epidemics intersect and interact with each other.
- 14.Enns A, Pinto A, Venugopal J, et al. Substance use and related harms in the context of COVID-19: a conceptual model. Health Promot Chronic Dis Prev Can 2020; 40:342–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boschuetz N, Cheng S, Mei L, Loy VM. Changes in alcohol use patterns in the united states during covid-19 pandemic. WMJ 2020; 119:171–176. [PubMed] [Google Scholar]
- 16.Rubin R. Substance use disorder linked to higher covid-19 risk. JAMA 2020; 324:1598. [DOI] [PubMed] [Google Scholar]
- 17▪.Schwetz TA, Calder T, Rosenthal E, et al. Opioids and infectious diseases: a converging public health crisis. J Infect Dis 2019; 220:346–349. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article is a useful reference on understanding the interface between substance use disorders and SARS-CoV2 exposure and developing COVID-19. This article is very useful in describing how substance use disorders, particularly opioid use disorders, can affect the risks of exposure to other infectious processes
- 18.Arcavi L, Benowitz NL. Cigarette smoking and infection. Arch Intern Med 2004; 164:2206–2216. [DOI] [PubMed] [Google Scholar]


