Abstract
Purpose of review
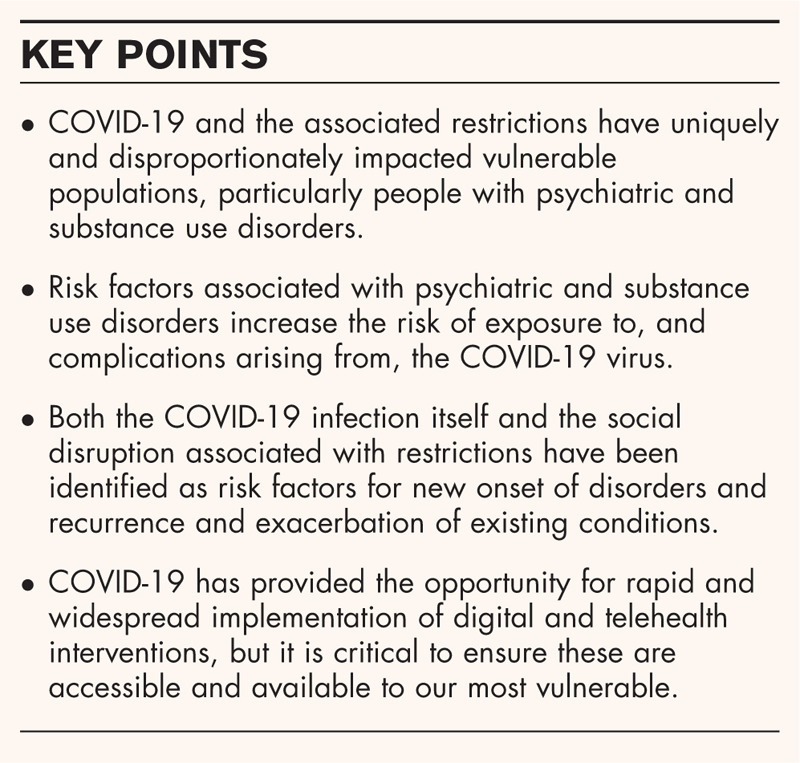
The COVID-19 pandemic and associated restrictions have uniquely and disproportionately affected vulnerable populations. This review summarizes recent evidence on the relationship between psychiatric disorders, substance use disorders and COVID-19, highlighting acute and long-term risks, pharmacotherapy interactions and implications regarding appropriate and timely evidence-based treatment.
Recent findings
Evidence points to a complex relationship between psychiatric and substance use disorders and COVID-19. A range of risk factors associated with psychiatric and substance use disorders increases the risk of exposure to, and complications arising from, the COVID-19 virus. COVID-19 infection has been indicated as having acute and potential long-term impacts on both psychiatric and substance use disorders. Social disruption associated with restrictions imposed to curb transmission has also been identified as a risk factor for new onset of disorders and recurrence and exacerbation of existing conditions.
Summary
Early recognition and intervention are key to preventing chronic disability associated with psychiatric disorders, substance use disorders, and their co-occurrence. It is critical that those most in need of services do not fall through the cracks of our healthcare systems. The pandemic has fast tracked the opportunity for widespread implementation of digital health interventions but ensuring these are accessible and available to all, including our most vulnerable, will be a critical task for our future health and social ecosystems.
Keywords: comorbidity, COVID-19, evidence-based treatment, mental disorders, substance use
INTRODUCTION
For more than 12 months, the coronavirus disease 19 (COVID-19) has been wreaking havoc across the globe, pushing healthcare systems beyond the limits of their capacity. By the first week of February 2021, just 13 months after COVID-19 was first identified, more than 104 million cases had been reported worldwide, in over 190 countries, with almost 2.3 million deaths [1,2]. From the earliest stages of the pandemic, there have been concerns about the potential impact of the virus on vulnerable populations, that is people who are disproportionately exposed to risk [3]. The past year has seen an explosion of commentary, and more recently, new evidence focusing on population groups at disproportionate risk of COVID-19-related complications, including people with psychiatric disorders and people with substance use disorders. Individually, each of these conditions are associated with a range of risk factors, including physical health comorbidities, that increase risk of exposure to, and complications arising from, the COVID-19 virus [4▪▪]. For individuals with both conditions, these problems are likely to be compounded. This review is based on a search of the PsycINFO database conducted in January 2021, designed to capture studies published in English which focused on the relationship between substance use, mental disorders and COVID-19 since the emergence of the disease. Forward and backward searches of key studies were conducted to identify relevant research studies and reviews. The current review synthesizes these key findings that have emerged over the past year with reference to the unique impact of COVID-19 in relation to psychiatric and substance use disorders, including acute and long-term risks, multimorbidity, pharmacotherapy interactions; challenges and opportunities regarding access to, and the provision of, appropriate and timely evidence-based treatment.
Box 1.
no caption available
ACUTE AND LONG-TERM EFFECTS OF COVID-19 INFECTION, PSYCHIATRIC AND SUBSTANCE USE DISORDERS
COVID-19 is a complex multisystem disease. Evidence is emerging that COVID-19 not only impacts the respiratory system but also impacts the neurological, cardiovascular, renal, gastrointestinal, musculoskeletal and haematological systems [5]. Evidence regarding the long-term consequences that may be experienced following recovery from acute infection is also growing [6,7]. In addition to research on physiological effects, there has been an increasing focus in the literature on the acute and potential long-term impact of COVID-19 on psychiatric and substance use disorders, including suicidal ideation, psychosis, anxiety, depression [8▪].
Current evidence suggests lower mental health quality, elevated anxiety and depression and posttraumatic stress disorder (PTSD) in individuals who have recovered from acute COVID-19 [4▪▪,9]. In a recent US cohort analysis, close to one in five (18.1%) COVID-19 survivors were found to have received a psychiatric diagnosis within 3 months of their COVID-19 diagnosis, including 5.8% that were new-onset conditions. Indeed, the risk of being newly diagnosed with a psychiatric disorder was more than twice that of other health events [4▪▪]. Early recognition and intervention are crucial to ensure we do not have a significant increase in the number of people experiencing mental health problems, making them vulnerable to other poor health outcomes including substance use disorders.
This same cohort analysis found that individuals with a past 12-month or past 3-year diagnosis of psychiatric disorder were at 65 and 80% greater risk of being diagnosed with COVID-19, respectively, compared with those who did not have psychiatric diagnoses [4▪▪]. These findings suggest that the presence of psychiatric disorder may increase both the proximal and more distal risk of infection. It is unclear why the risk is elevated among these groups; however, behavioural and socioeconomic factors (such as noncompliance with COVID-19 restrictions), physical health comorbidities and smoking have been posited [4▪▪].
In addition to the direct impact of COVID-19 infection on individuals, the response to the COVID-19 pandemic itself can potentially have long-term effects. More than 180 countries have implemented a variety of restrictions in attempts to slow the rate of transmission and reduce the impact on overburdened healthcare systems [10,11]. Responses have included physical distancing, partial or full lockdowns, school and workplace closures, cancellation of public events and social gatherings, mandating face masks, restricting domestic and international travel, as well as widespread testing and contact tracing [10,11]. Although restrictions have been vital in reducing the spread of the virus and saving countless lives, the concomitant economic and social impacts have been considerable [4▪▪,12▪,13▪,14▪▪,15]. The significant social disruption places individuals at further risk of poor mental health, and has left those with preexisting psychiatric conditions (who are already vulnerable), at an increased risk of isolation, with evidence of the amplification of existing mental health issues [16].
Although COVID-19 and associated restrictions have disproportionately affected marginalised population groups, reports from Australia's First Nations’ response may be the exception. First Nations people are at an increased risk of contracting COVID-19 and experiencing COVID-19 related complications due to higher rates of smoking and multiple chronic diseases than non-Indigenous Australians [17–20]. Despite these risk factors, and despite First Nations people representing 3.3% of the Australian population, the latest available data from Australia's COVID-19 epidemiology report (which included data up to 14 February 2021) illustrated only 149 cases of COVID-19 among First Nation Australians, representing 0.5% of all Australian cases [17,21]. The avoidance of widespread illness and death is thought to be due to the rapid, collective response led by First Nations health leaders in the very early days of the pandemic. This included the lobbying of all levels of government to close remote communities, help with protective equipment, testing and contact tracing; the provision of staff training, accommodation for homeless people and information via social media; and ensuring culturally appropriate services were implemented by establishing partnerships with government and nongovernment organizations [18].
MULTIMORBIDITY, COVID-19-RELATED COMPLICATIONS AND PHARMACOTHERAPY INTERACTIONS
There is clear evidence demonstrating the association between psychiatric and substance use disorders and poor physical health across a number of domains [13▪,15,22,23▪,24], all of which increase the risk of contracting COVID-19 and experiencing more severe COVID-19-related complications if infected [22,23▪,25–27]. High rates of smoking, overweight and obesity, metabolic syndrome, hypertension and cardiovascular disease, alongside confinement in forensic, residential and in-patient facilities, can increase susceptibility to infection and disease [28▪▪,29]. Preexisting psychiatric symptoms may be exacerbated due to fear and worry about being infected, social isolation and the lack of connectivity, distressing medical symptoms and death [28▪▪,30▪▪].
One of the unique challenges for clinicians who are managing and treating COVID-19 among people with psychiatric and substance use disorders, and particularly those with comorbid conditions, is the complexities surrounding the well tolerated prescribing of pharmacotherapies. A recent review highlighted potential safety risks associated with interactions between COVID-19 treatments and psychiatric medications and pharmacotherapies for substance use disorders, including selective serotonin reuptake inhibitors (SSRIs), serotonin–norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), antipsychotics, mood stabilizers, benzodiazepines, methadone and bupropion. Safety risks include respiratory distress, cardiovascular events, infections, coagulation and delirium [30▪▪]. Although there is evidence highlighting the dangers associated with interactions between medications, the dearth of data makes drawing conclusions regarding the magnitude of risk difficult [30▪▪]. Despite this uncertainty, general guidance on well tolerated prescribing includes close monitoring of any risk interactions; assessing psychotropic-related risk of respiratory depression and cardiovascular events; and the provision of psychosocial interventions [28▪▪,30▪▪,31]. Further, an online ‘Interaction Checker’, containing information on potential interactions between pharmacotherapies and COVID-19 experimental agents, has been developed to assist clinicians [32].
COVID-19 AND ALCOHOL AND OTHER DRUG-RELATED HARMS
People with substance use disorders often experience higher rates of homelessness, unstable or higher density housing, incarceration and social disadvantage compared with the general population, all of which can increase the risk of COVID-19 transmission [22,27,33]. The provision of sterile injecting equipment to people who inject drugs remains critical, yet many needle and syringe exchange programs have had difficulties delivering their usual services [34▪,35], resulting in some people reusing, or sharing injecting equipment [33].
Physical distancing is at the forefront of the global public health response to COVID-19, yet it may inadvertently increase the risk of serious drug-related harms. General public health guidance recommends people who use drugs never do so alone, with another person available to respond and call emergency services in the event of an overdose or other adverse event [34▪,36,37▪]. The implications of conflicting guidance may force a choice between wanting to avoid potential exposure to COVID-19, adhering to government orders and using drugs safely [34▪,36].
Loneliness, self-isolation, financial and economic stress may also lead to an exacerbation of psychiatric disorders (such as depression, anxiety, self-harm and suicidal ideation), which are highly prevalent among people with substance use disorders [38]. These circumstances may also present the ideal risk factors for someone who had stopped using substances to experience a lapse or relapse, or increase patterns of current use to ‘self-medicate’ psychiatric symptoms [39–41]. Existing psychiatric conditions may be further exacerbated by reduced access to substances. Supply shortages, due in part to international travel restrictions, may also lead some people to source illicit substances in particular from unfamiliar and untrusted providers, increasing the risk of exposure to contaminated supplies [34▪,41,42]. The inability to access substances may lead to withdrawal, the symptoms of which (fever, sweats, fatigue, aches and pains) could be mistaken for COVID-19 and vice versa [23▪].
Conversely, the classification of alcohol as an ‘essential’ commodity in many countries around the world has led to its increased availability through home delivery and advertising, including targeted COVID-19 advertising [13▪,43,44]. The financial, economic and social stressors caused by COVID-19 and associated restrictions are likely to be exacerbated by increased consumption of alcohol at home, compounding the risk of experiencing or being exposed to domestic, family and intimate family violence, child neglect, heavier drinking, underage consumption, serious or traumatic injury, and death [43–45,46▪,47].
CHALLENGES AND OPPORTUNITIES FOR THE PROVISION OF EVIDENCE-BASED TREATMENT
Despite evidence that the COVID-19 pandemic has exacerbated psychiatric and substance use symptoms, the ability of services and practitioners to provide, and patients to access, treatment has been limited by public health responses introduced in efforts to reduce the transmission of COVID-19. With healthcare systems under pressure and under resourced, there is the risk that people with chronic co-occurring psychiatric and substance use disorders may be even more marginalized by a health system prioritizing the urgency of COVID-19 patients [15,48]. Patients with these disorders may find it difficult to continue current treatment, access medications or attend new treatment if symptoms recur or become exacerbated with some services not accepting new patients [15,33,41,49,50▪▪,51▪▪]. In a cross-sectional study conducted among clinical and community youth cohorts in Canada in April 2020, participants reported having difficulty accessing mental health services [52▪]. Types of services that were identified as being unavailable included therapy/counselling, substance use and psychiatric services. At a service level, one qualitative study conducted among 18 opioid substitution therapy (buprenorphine) prescribers in the US found many were reluctant to accept new patients or treat those who did not have a prior history with the service [50▪▪]. It is ironically those who need services the most who are most likely to fall through the cracks of health systems. In addition to services and clinicians lacking the capacity and resources to provide care to patients, there is the added challenge of how to address fear of exposure to infection preventing some patients from attending appointments [31,53]. No studies examining access to telehealth among disadvantaged patients were identified, nor were any accounts of patients’ experience using telehealth services.
Rapid changes have been made in services worldwide, in attempts to ensure continued provision of opioid substitution therapies. In North America, new regulations allow for pharmacists to adjust opioid substitution therapy doses, and several countries, including Australia, have relaxed restrictions regarding take-home doses [23▪,53]. Although rapid modifications have been necessary in attempts to minimize potential disruptions to treatment, it is vital that any changes are implemented within a coordinated care approach. For example, pharmacists communicating any dosage adjustments back to prescribing doctors, and taking the time to speak to patients about any implications arising from increase/decrease in dosages, such as contraindications or interactions with other pharmacotherapies and/or medications.
It has been recommended in Australia that longer-acting depot formulations of buprenorphine replace daily methadone/buprenorphine dosing, and potentially be provided to those at risk of overdose or dose diversion (e.g. stockpiling takeaway doses, using all doses quickly and supplementing with other opioids) [23▪,33]. The provision of buprenorphine-naloxone in place of buprenorphine to minimize use by injection has also been recommended, alongside take-home naloxone [23▪].
The pandemic has fast tracked the opportunity for upscaling the use of digital health interventions. Telehealth, comprising computerised, web and telephone-based medicine, has the potential to overcome many barriers preventing access to, and provision of healthcare services for people with psychiatric and substance use disorders. These include providing access to those afraid of exposure to infection; people living in rural or remote locations; improving continuity of care; with flexibility for both providers and patients who can provide and access care wherever most convenient; at reduced cost [42]. Despite numerous advantages, there has been concern about the identification of high-risk situations (e.g. self-harm, suicidal ideation) via computer or telephone, where the assessment of a person's mental state and general behaviour is critical [54]. Other practical and logistical challenges include the need for access to a smartphone and phone credit, computer and stable internet coverage, as well as a well tolerated and private therapeutic space in which patients can engage in treatment [33,54]. Lack of equal access to technology required for engaging in telehealth, and challenges finding available technology during COVID-19 restrictions (e.g. via public libraries and other shared spaces) makes providing equal care difficult [51▪▪,54]. The implementation of an e-mental health ecosystem that delivers to all will take some time, but ensuring that digital health interventions are accessible and available for all, including our most vulnerable, will be a critical task for our future health systems and essential to full utilisation of digital technologies.
IMPLICATIONS FOR CLINICIANS, SERVICE PROVIDERS AND GOVERNMENTS
The COVID-19 pandemic has driven dramatic global shifts in all areas of life, and healthcare systems will never be the same. The rapid change has also presented novel opportunities to explore different models and think differently about how to best provide evidence-based care to those who are uniquely and disproportionately affected by the pandemic and subsequent restrictions. Despite the development and current roll out in many countries of vaccines, there is general consensus that the virus will be with us, and need to be managed, for a long time. An ongoing response is needed that continues to monitor and model the impact of COVID-19 and associated societal changes on substance use and psychiatric health at national and local levels. Such evidence is critical to informing health and social ecosystems, and improving service capacity, linkage and coordination.
Acknowledgements
None.
Financial support and sponsorship
Christina Marel, Katherine Mills and Maree Teesson are supported by Australian National Health and Medical Research Council (NHMRC) Fellowships.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Parker E. COVID-19 tracker [Internet]. 2021. https://shiny.rstudio.com/gallery/covid19-tracker.html. [Accessed 5 February 2021] [Google Scholar]
- 2.Dong E, Du H, Gardner L. COVID-19 dashboard. Lancet Infect Dis 2020; 20:533–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lancet T. Redefining vulnerability in the era of COVID-19. Lancet 2020; 395:1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4▪▪.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2020; 8:130–140. [DOI] [PMC free article] [PubMed] [Google Scholar]; On the basis of the TriNetX Analytics Network, which captures electronic health records across 54 healthcare organizations in the USA, representing 69.8 million patients. This study analysed 62 354 patients diagnosed with COVID-19 between 20 January and 1 August 2020, and assessed risk of developing psychiatric sequalae during the first 14 and 90 days following COVID-19 diagnosis, as well as antecedents of COVID-19.
- 5. NIHR Themed Review: Living with Covid19; October 2020; doi:10.3310/themedreview_41169. [Google Scholar]
- 6. World Health Organization. What we know about long-term effects of COVID-19. Coronavirus update 36 [Internet]. https://www.who.int/docs/default-source/coronaviruse/risk-comms-updates/update-36-long-term-symptoms.pdf?sfvrsn=5d3789a6_2. [Accessed 13 February 2021] [Google Scholar]
- 7.Nabavi N. Long covid: how to define it and how to manage it. BMJ 2020; 370. [DOI] [PubMed] [Google Scholar]
- 8▪.Wildwing T, Holt N. The neurological symptoms of long COVID-19: a comparison with other neurological conditions and implications for healthcare services. Ther Adv Chronic Dis 2021; 12:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]; A systematic review exploring the impact of longer-term neurological symptoms of COVID-19, and implications for healthcare services.
- 9.Méndez R, Balanzá-Martínez, Vicent Luperdi SC, et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J Intern Med 2021; doi:10.1111/joim.13262, Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet 2020; 396:1525–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hale T, Webster S, Petherick A, et al. Oxford COVID-19 government response tracker [Internet]. Blavatnik School of Government. Data use policy: creative commons attribution CC BY standard. 2021. https://covidtracker.bsg.ox.ac.uk/. [Accessed 29 January 2021] [Google Scholar]
- 12▪.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020; 7:883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]; This longitudinal cohort study of 42 330 adults from households in the UK examined trends in mental health before and during the COVID-19 pandemic. Mental health deterioration was found to be associated with preexisting inequalities.
- 13▪.Dubey MJ, Ghosh R, Chatterjee S, et al. COVID-19 and addiction. Diabetes Metab Syndr Clin Res Rev 2020; 14:817–823. [DOI] [PMC free article] [PubMed] [Google Scholar]; A review of the literature summarizing the association between COVID-19 and addiction. Explanations for why those with substance use disorders at an increased risk of contracting COVID-19 are discussed.
- 14▪▪.Rogers AH, Shepherd JM, Garey L, Zvolensky MJ. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res 2020; 293:113407. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study examined how levels of COVID-19-related fear and worry differed between people who did not use substances, those who used subustances pre-COVID-19 and those who initiated substance use during COVID-19. The study also sought to examine how levels of COVID-19-related worry and fear were related to coping strategies in relation to substance use.
- 15.Spagnolo PA, Montemitro C, Leggio L. New challenges in addiction medicine: COVID-19 infection in patients with alcohol and substance use disorders: the perfect storm. Am J Psychiatry 2020; 177:805–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ismael F, Bizario JCS, Battagin T, et al. Post-infection depressive, anxiety and post-traumatic stress symptoms: a retrospective cohort study with mild COVID-19 patients. medRxiv 2020; doi: 10.1016/j.psychres.2020.113407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir 2020; 8:547–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eades S, Eades F, McCaullay D, et al. Australia's First Nations’ response to the COVID-19 pandemic. Lancet 2020; 396:237–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Australian Bureau of Statistics. National Aboriginal and Torres Strait Islander Health Survey: 2018–19 [Internet]. 2019. https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/national-aboriginal-and-torres-strait-islander-health-survey/2018-19#diet-weight-and-exercise-adult-. [Accessed 3 March 2021] [Google Scholar]
- 20. Australian Bureau of Statistics. National Health Survey: first results: 2017-18 [Internet]. 2018. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release#health-risk-factors. [Accessed 3 March 2021] [Google Scholar]
- 21.COVID-19 National Incident Room Surveillance Team. COVID-19 Australia: epidemiology report 35. Commun Dis Intell 2021; 45:1–10. [Google Scholar]
- 22.Marsden J, Darke S, Hall W, et al. Mitigating and learning from the impact of COVID-19 infection on addictive disorders. Addiction 2020; 115:1007–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23▪.Dunlop A, Lokuge B, Masters D, et al. Challenges in maintaining treatment services for people who use drugs during the COVID-19 pandemic. Harm Reduct J 2020; 17:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Early review of the evidence in relation to treatment provision for people with substance use, and in particular, opioid substitution therapy. Key strategies for workplace safety, relapse prevention and minimizing harm to population groups are discussed.
- 24.Wei Y, Shah R. Substance use disorder in the COVID-19 pandemic: a systematic review of vulnerabilities and complications. Pharmaceuticals (Basel) 2020; 13:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu LT, Ghitza UE, Zhu H, et al. Substance use disorders and medical comorbidities among high-need, high-risk patients with diabetes. Drug Alcohol Depend 2018; 186:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schulte MT, Hser YI. Substance use and associated health conditions throughout the lifespan. Public Health Rev 2013; 35: 10.1007/BF03391702https://doi.org/10.1007/BF03391702 (see https://publichealthreviews.biomedcentral.com/articles/10.1007/BF03391702#citeas). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med 2020; 173:61–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28▪▪.Anmella G, Arbelo N, Fico G, et al. COVID-19 inpatients with psychiatric disorders: real-world clinical recommendations from an expert team in consultation-liaison psychiatry. J Affect Disord 2020; 274:1062–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]; Using three case scenarios from a team of clinical experts, this study provides an overview of key pharmacological recommendations for consideration in the management of patients with COVID-19. One of the primary strengths is discussion of potential drug interactions with COVID-19 phramacotherapy.
- 29.Basrak N, Mulcrone N, Sharifuddin S, et al. Risk of adverse outcome of COVID-19 among patients in secure psychiatric services: observational cohort study. BJPsych open 2021; 7:e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30▪▪.Ostuzzi G, Papola D, Gastaldon C, et al. Safety of psychotropic medications in people with COVID-19: evidence review and practical recommendations. BMC Med 2020; 18:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]; A review of the evidence regarding the safety of psychiatric medications in patients with COVID-19, highlighting numerous potentially severe safety issues that require consideration. Evidence-based practical recommendations are made by an international, multidisciplinary working group.
- 31.Luykx JJ, Van Veen SMP, Risselada A, et al. Safe and informed prescribing of psychotropic medication during the COVID-19 pandemic. Br J Psychiatry 2020; 217:471–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. The University of Liverpool. COVID-19 drug interactions [Internet]. 2020 . https://www.covid19-druginteractions.org/checker. [Accessed 12 February 2021] [Google Scholar]
- 33.Marel C, Mills KL, Stirling R, et al. Impact of COVID-19 on substance use and treatment provision in Australia. Adv Dual Diagn 2021; 14:1–7. [Google Scholar]
- 34▪.LeSaint KT, Snyder HR. Impact of social distancing on individuals who use drugs: considerations for emergency department providers. West J Emerg Med 2020; 21:1102–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]; Commentary discussing key concerns regarding substance use and public health approaches, including implications for emergency clinicians.
- 35.Whitfield M, Reed H, Webster J, Hope V. The impact of COVID-19 restrictions on needle and syringe programme provision and coverage in England. Int J Drug Policy 2020; 83:102851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schlosser A, Harris S. Care during COVID-19: drug use, harm reduction, and intimacy during a global pandemic. Int J Drug Policy 2020; 83:102896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37▪.Stack E, Leichtling G, Larsen JE, et al. The impacts of COVID-19 on mental health, substance use, and overdose concerns of people who use drugs in rural communities. J Addict Med 2020; 00: Nov 3. doi: 10.1097/ADM.0000000000000770. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; A qualitative study examining the impact of COVID-19 in rural communities, conducted among people who use substances in the US. Experiences unique to rural communities are discussed.
- 38.Teesson M, Slade T, Mills K. Comorbidity in Australia: findings of the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 2009; 43:606–614. [DOI] [PubMed] [Google Scholar]
- 39.Teesson M, Marel C, Darke S, et al. Long-term mortality, remission, criminality and psychiatric comorbidity of heroin dependence: 11-year findings from the Australian treatment outcome study. Addiction 2015; 110:986–993. [DOI] [PubMed] [Google Scholar]
- 40.Teesson M, Marel C, Darke S, et al. Trajectories of heroin use: 10–11-year findings from the Australian Treatment Outcome Study. Addiction 2017; 112:1056–1068. [DOI] [PubMed] [Google Scholar]
- 41.Dietze PM, Peacock A. Illicit drug use and harms in Australia in the context of COVID-19 and associated restrictions: anticipated consequences and initial responses. Drug Alcohol Rev 2020; 39:297–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.López-Pelayo H, Aubin HJ, Drummond C, et al. The post-COVID era’: challenges in the treatment of substance use disorder (SUD) after the pandemic. BMC Med 2020; 18:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Colbert S, Wilkinson C, Thornton L, Richmond R. COVID-19 and alcohol in Australia: industry changes and public health impacts. Drug Alcohol Rev 2020; 39:435–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neufeld M, Lachenmeier DW, Ferreira-Borges C, Rehm J. Is alcohol an ‘Essential Good’ during COVID-19? Yes, but only as a disinfectant!. Alcohol Clin Exp Res 2020; 44:1906–1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reynolds J, Wilkinson C. Accessibility of ‘essential’ alcohol in the time of COVID-19: casting light on the blind spots of licensing? Drug Alcohol Rev 2020; 39:305–308. [DOI] [PubMed] [Google Scholar]
- 46▪.Huckle T, Parker K, Romeo JS, Casswell S. Online alcohol delivery is associated with heavier drinking during the first New Zealand COVID-19 pandemic restrictions. Drug Alcohol Rev 2020; Nov 30; doi: 10.1111/dar.13222. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; A cross-sectional study conducted online that examined self-reported alcohol purchasing and drinking among New Zealand adults in April–May 2020. Findings illustrated that online alcohol delivery was associated with heavier drinking.
- 47.Iob E, Steptoe A, Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br J Psychiatry 2020; 217:543–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oesterle TS, Kolla B, Risma CJ, et al. Substance use disorders and Telehealth in the COVID-19 pandemic era: a new outlook. Mayo Clin Proc 2020; 95:2709–2718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rosen D. Increasing participation in a substance misuse programs: lessons learned for implementing Telehealth solutions during the COVID-19 pandemic. Am J Geriatr Psychiatry 2021; 29:24–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50▪▪.Uscher-Pines L, Sousa J, Raja P, et al. Treatment of opioid use disorder during COVID-19: Experiences of clinicians transitioning to telemedicine. J Subst Abuse Treat 2020; 118:108124. [DOI] [PMC free article] [PubMed] [Google Scholar]; A qualitative study describing challenges being experienced by opioid prescribers in the transition to telehealth. More than half of clinicians were only providing treatment via telehealth, and the lack of visible information to inform decision-making was identified as an ongoing challenge. Many services were not accepting new patients.
- 51▪▪.Yang J, Landrum MB, Zhou L, Busch AB. Disparities in outpatient visits for mental health and/or substance use disorders during the COVID surge and partial reopening in Massachusetts. Gen Hosp Psychiatry 2020; 67:100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]; This US study examined disparities in outpatient visits for patients with a mental health and/or substance use diagnosis. Findings highlighted disparities between population groups, which have been exacerbated during the COVID-19 pandemic, as some populations lack access to infrastructure necessary for digital health.
- 52▪.Hawke LD, Barbic SP, Voineskos A, et al. Impacts of COVID-19 on youth mental health, substance use, and well being: a rapid survey of clinical and community samples: Répercussions de la COVID-19 sur la santé mentale, l’utilisation de substances et le bien-être des adolescents: un sondage rapide. Can J Psychiatry 2020; 65:701–709. [DOI] [PMC free article] [PubMed] [Google Scholar]; A cross-sectional study conducted among clinical and community youth cohorts, which found deterioration of mental health symptoms in both groups. Participants reported difficulties accessing mental health services and concern about their mental health.
- 53.Bach P, Robinson S, Sutherland C, Brar R. Innovative strategies to support physical distancing among individuals with active addiction. Lancet Psychiatry 2020; 7:731–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Galea-Singer S, Newcombe D, Farnsworth-Grodd V, et al. Challenges of virtual talking therapies for substance misuse in New Zealand during the COVID-19 pandemic: an opinion piece. N Z Med J 2020; 133:104–111. [PubMed] [Google Scholar]


