Abstract
Purpose of review
To reduce the spread of infection from the coronavirus disease 2019 (COVID-19), mental healthcare facilities were forced to make the rapid transition from face-to-face services to virtual care. This systematic review aims to synthesize the extant literature reporting on barriers of telemental health (TMH) during the COVID-19 pandemic and how facilities have worked to overcome these barriers, to inform best practices for TMH delivery.
Recent findings
Most recent findings came from case studies from mental health professionals which reported on barriers related to institutional, provider and patient factors, and how these barriers were overcome. Common barriers identified in the literature include: technological difficulties; issues regarding safety, privacy and confidentiality; therapeutic delivery and the patient-provider relationship; and a loss of sense of community. Studies also reported on the benefits to TMH interventions/tools, as well as suggestions for improvements in the delivery of TMH services.
Summary
As the COVID-19 pandemic evolves, mental healthcare providers continue to find creative and feasible solutions to overcome barriers to the delivery of TMH. Dissemination of these solutions is imperative to ensure the best quality of mental healthcare for patients across the globe.
Keywords: coronavirus disease 2019, telemental health, telemental health barriers, telemental health benefits, telepsychiatry
INTRODUCTION
In March 2020, the coronavirus disease 2019 (COVID-19) was declared a global pandemic by the World Health Organization (WHO) [1]. Due to the absence of a vaccine, social distancing has been adopted as part of the mitigation strategies. Despite its benefits in slowing the spread of COVID-19, social distancing is accompanied with several consequences, including a rapid increase in the levels of psychological distress worldwide and projected increase in rates of suicide [2–4]. In response to these well founded concerns, telemental health (TMH) has been implemented as the main mode of service delivery during these unprecedented times [2].
TMH encompasses the delivery of mental health services, both psychiatric and psychological, via different technological platforms. Unique to the field of psychiatry and mental health, in-person contact is not always essential in providing care. As such, TMH is a plausible and logical option. However, as countries across the world have adopted TMH, numerous barriers have been identified. These barriers include, but are not limited to: lack of access to required technology or technical difficulties [5▪–7▪]; privacy and confidentiality concerns [8▪,9▪▪,10▪]; reduced quality of therapeutic delivery and patient-provider relationships; and a loss of sense of community [9▪▪,10▪]. Moreover, although federal and state regulators have recognized the importance of telehealth during these times, further legal and regulatory actions are necessary to remove public policy barriers [11].
Based on the current state of the pandemic, mental healthcare will continue to be delivered virtually for the foreseeable future. Thus, it is imperative that additional attention and resources be allocated to evaluating this method of care. The current situation provides a unique opportunity to improve the delivery of mental healthcare and expand the scope of individuals who can be reached by mental health professionals. There is a growing body of literature in which psychiatrists and other mental health professionals are sharing their experiences with TMH and providing feasible solutions to common barriers. The current review aims to summarize this literature to inform mental healthcare providers regarding optimal delivery of TMH.
Box 1.
no caption available
METHODS
A systematic search following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was conducted on PubMed, GoogleScholar, Web of Science and PsychInfo from database inception to August 2020 [12]. A manual citation search was conducted in the reference list of the included articles and other relevant reviews. The search terms that were used were: (COVID-19 OR 2019-nCoV OR SARS-CoV-2 OR coronavirus) AND (psychiatry) AND (eHealth OR mHealth OR Mobile Health OR telehealth OR health, mobile OR telemedicine). The PRISMA flow diagram details the search and selection process applied during our systematic literature search and critical review (Fig. 1).
FIGURE 1.
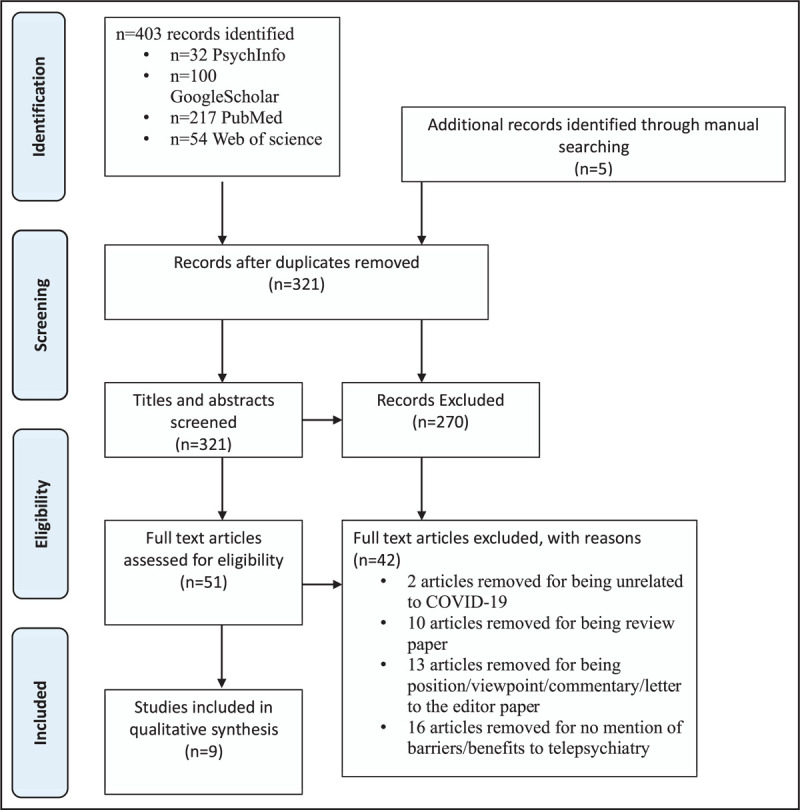
Preferred Reporting Items for Systematic Reviews and Meta-Analyses study selection flow diagram. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram details the search and selection process applied during our systematic literature search and critical review.
Articles were selected according to the following inclusion criteria: first, studies based on empirical evidence; second, assessed the barriers and/or benefits to TMH during the COVID-19 pandemic and the associated means for those overcoming barriers. Studies were excluded if they were not written or translated into English; discussed TMH outside of the COVID-19 context; discussed potential barriers rather than empirical findings. Figure 1 reports the flow diagram of inclusion of the studies. The quality of articles was assessed using the Cochrane Risk of Bias (Table 1).
Table 1.
Cochrane risk of bias assessment
| Study (year) | Risk of bias domain | Risk of bias outcome | Reason for ‘other’ |
| Barney et al. (2020) | Incomplete outcome data | Low | N/A |
| Selective reporting | Low | ||
| Other sources of bias | Low | ||
| Sequeira et al. (2020) | Incomplete outcome data | Low | N/A |
| Selective reporting | Low | ||
| Other sources of bias | Low | ||
| Falicov et al. (2020) | Incomplete outcome data | Low | N/A |
| Selective reporting | Low | ||
| Other sources of bias | Low | ||
| Hom et al. (2020) | Incomplete outcome data | Low | N/A |
| Selective reporting | Low | ||
| Other sources of bias | Low | ||
| Yelowlees et al. (2020) | Incomplete outcome data | High | N/A |
| Selective reporting | Low | ||
| Other sources of bias | Low | ||
| Olwill et al. (2020) | Incomplete outcome data | Low | Surveys were based on already identified barriers; restricted to telephone use |
| Selective reporting | Low | ||
| Other sources of bias | High | ||
| Sharma et al. (2020) | Incomplete outcome data | Low | N/A |
| Selective reporting | Low | ||
| Other sources of bias | Low | ||
| Ramtekkar et al. (2020) | Incomplete outcome data | Low | N/A |
| Selective reporting | Low | ||
| Other sources of bias | Low | ||
| Waller et al. (2020) | Incomplete outcome data | Low | Results were based off first 96 h of moving virtual |
| Selective reporting | Low | ||
| Other sources of bias | High |
RESULTS
Barriers to TMH related to provider, patient and institutional factors were divided into four main categories: technical issues; safety, privacy and confidentiality; therapeutic delivery and the patient-provider relationship; and sense of community (Table 2). Corresponding suggestions to barriers as well as benefits to TMH are also discussed (Table 3).
Table 2.
Summary of study characteristics and identified barriers
| Barriers | ||||||
| Patient descriptions | Country of origin | Telepsychiatry platform | Patient factors | Provider factors | Institutional factors | |
| [13▪] | Children and adolescent psychiatric patients | USA | Videoconference platform (specific platform not mentioned) | Obtaining parental consentPrivacy and securitySafety monitoring | Proper training in treatment delivery via telehealthBalance between privacy regulations and meeting patient needs | Size and affiliations of the hospital made the transition more difficult |
| [5▪] | Psychiatric patients | USA | Zoom | Increase in screen and sedentary time (led to reduction in full day programming)Scheduling confusions | Screen-use fatigueStaff burnout | Communication between staffEthical and legal considerations |
| [6▪] | Children and adolescents needing psychiatric, psychological, therapy or autism services | USA | Telephone and Zoom | Internet connectivityLanguage barriers | Decisions about patient priorities | Loss of coordination with school personnelLack of full team-based evaluations |
| [7▪] | Psychiatric patients | USA | Epics MyChat and Zoom | Access to technologyPrivacy and security | Contacting patients under time constraints | Lack of IT support staff |
| [8▪] | AYA patients with problems in mental health, reproductive health, eating disorders and addictions | USA | Zoom | Patient acceptancePrivacy (lack of space at home)Access and understanding of technologyBarriers compounded by lower SES | Provider acceptance and comfortLack of experience for telemedicine in AYA fieldReduced confidence in clinical decision makingEstablish/maintain effective doctor–patient relationships | Lack of real-time availability of mental health professionals (social workers, psychiatrists, dietician) |
| [9▪▪] | Vulnerable populations experiencing emotional disturbances (families with lower SES; families have immigrated); most frequent population was a Latinx population of Mexican origin | USA | Telephone; Various video-conferencing platforms | Lack of access to E-mail, WiFi, smartphones, and/or computersLimited access to telephonePrivacy (lack of space and overcrowded homes)Cultural and language barriersLoss of support group programmingLoss of connection to community | Privacy (shared space with other clinicians)Lack of time for providers (i.e. mother's schooling children)Interruptions from home environments | Need for additional staff to coordinate smooth virtual visits |
| [10▪] | OCD patients | USA | Theranest | Lack of willingness from patientsDifficulty maintaining focus | Confidentiality and patient privacyLack of group sessionsTechnological issuesLoss of personal boundariesSpecific aspects of ERP difficult over telehealth | Loss of interaction with peers and staff |
| [14▪▪] | Psychiatric patients | Ireland | Telephone | N/A | Reduced confidence in clinical decision making (diagnoses, risk assessment, prescriptions)Lack of visual cues from patientsEstablishing patient–clinician relationshipTechnical issuesReduced efficacy for some patient populations (cognitive deficits, hearing deficits, language barriers)Patient confidentiality | N/A |
AYA, adolescent and young adult; ERP, exposure and response prevention; OCD, obsessive compulsive disorder; SES, socioeconomic status.
Table 3.
Benefits and suggestions for improvements
| Benefits to telepsychiatry | Suggestion to overcome barriers | |
| [13▪] | Increase patient's access to medical care | Shadowing telehealth sessions and watching prerecorded sessions for proper training of deliveryOften resorted to telephone care |
| [5▪] | N/A | Program specific training for staffPrior to their first appointment, patients attended a virtual orientation to properly use the platformStaff dedicated to IT problemsUse of a web-based secure collaborative workspace (Microsoft Teams)Staff members encouraged to share self-care tips with one anotherVideoconference ‘lunchroom’ for staff |
| [6▪] | Prevented major disruption to clinical care | N/A |
| [7▪] | Flexible work arrangements | Telephone instead of virtual platformMass E-mail to contact patients |
| [8▪] | Geographic flexibilityAll patients, despite SES, were able to access a device for telemedicineIncreased parental participation | Encouraged use of headphonesUse of Zoom chatMore frequent use of yes/no questions |
| [9▪▪] | More appointment flexibilityAwareness of various technical possibilitiesInsights to family/home life | Continue community feel through more continuous check-in'sConstant presence of IT support staff |
| [10▪] | Geographic flexibilityCost effectiveAbility to assist with at-home exposuresDecrease in cancellationsIncrease in family participation | Patients asked to review and sign informed consent checklist for Telepsychological ServicesSound machines to prevent other peoplein the homes from overhearing appointmentsVirtual support groups after the treatment dayProvision of resources for online support outside of the session |
| [14▪▪] | Flexible work arrangements | N/A |
SES, socioeconomic status.
Barriers regarding technical issues and corresponding suggestions
Some patients may experience lack of access to required technology (e.g. WiFi, Internet, E-mail etc.) and hardware (e.g. webcam, smartphone, computer etc.) to support video-conferencing visits and consultations [5▪–7▪]. Various technological challenges are compounded by low socioeconomic status (SES), thus further intensifying this technology inequity [6▪,8▪,9▪▪]. Patients who lack technological literacy encounter difficulties in both understanding and utilizing relevant technological platforms and devices [8▪].
For providers to be fully prepared for TMH sessions, not only is their professional knowledge required, but hardware and equipment such as room set-up, light and audio must also be satisfactory prior to the treatment session [13▪]. Further, similar to patients, medical providers may encounter challenges regarding technology use and treatment delivery during this period of transition to telehealth [10▪,13▪,14▪▪].
Different technical problems may occur during an online session and impede the progression of a treatment. Hospitals and clinics may face the challenge of lacking sufficient IT support staff readily available to help troubleshoot and assist in a smooth progression of virtual visits and treatment sessions [7▪,9▪▪]. To ensure a good experience during virtual treatment, it is recommended that providers and institutions offer a virtual orientation held by medical staff that provides information on the proper utilization of the technological platform [5▪]. By dedicating a particular staff to help the corresponding patient with IT problems throughout the treatment sessions, it helps minimize the disruption of care for each patient [5▪].
For patients with difficulties in participating in a virtual face-to-face treatment session, telephone calls should be considered as one of the alternative treatment delivery options [7▪]. Although a promising alternative, new barriers to delivery of therapeutic services arise when sessions are conducted via telephone, as will be discussed in later sections [14▪▪].
It is beneficial for healthcare professionals to obtain proper training on telehealth treatment delivery (e.g. shadowing telehealth sessions, watching prerecorded sessions) prior to their formal telehealth sessions. However, the complex, time-consuming training procedures followed by frequent updates and modifications of the protocols and guidelines make the learning and adaptation to this treatment modality much more difficult [13▪].
For hospitals, clinics and other institutions that provide virtual care programs, it is essential for them to ensure IT support groups are constantly present and ready to offer professional help [9▪▪]. Further, it would be beneficial for institutions to incorporate training for TMH delivery into their typical training regimens to be prepared for unforeseen circumstances such as the current pandemic.
Barriers regarding safety, privacy and confidentiality and corresponding suggestions
Concerns regarding safety, privacy and confidentiality are raised among patients, providers and regulatory officials. Some patients are facing the challenge of maintaining quiet and private spaces in the home-setting during treatment sessions. Lack of privacy often affects patients’ ability to talk openly during their session, which undoubtedly impacts the efficacy of treatment [8▪,9▪▪,10▪]. Individuals with low SES who live in overcrowded homes are disproportionately affected by these types of privacy concerns [8▪,9▪▪]. Using telephones instead of video-conference platforms may allow patients to walk to more secluded areas of the home during sessions, as needed [9▪▪]. Patients have also generated concerns about the overall privacy of online treatments, and the security level of different platforms in aspects such as information protection and system encryptions [5▪,7▪,13▪].
Similar to patients, providers face privacy issues when they are working in a shared space with other medical providers [9▪▪]. Providers also have to deal with issues regarding patient's safety monitoring (e.g. risk of suicidality) and local emergency contacts when providing remote therapies or other therapeutic treatments [13▪]. Another challenge for providers is to maintain patients’ confidentiality in telehealth treatments [8▪,10▪,14▪▪]. Complex medical, legal and ethical issues should be taken into consideration when delivering virtual/online treatments [5▪,8▪,14▪▪]. Providers, institutions and regulatory officials must balance privacy regulations and patients/public healthcare demands, by constantly improving the privacy code and available encryptions, while maintaining continual care [13▪].
To minimize members in a communal space overhearing telehealth sessions, patients are encouraged to use headphones instead of speakers when possible and use the chat function built into each platform when desired [8▪,10▪]. If solutions such as headphones are not feasible, healthcare providers are encouraged to ask more yes/no questions (if applicable) to limit the information that can be overheard [8▪]. Protocols should also be established at the beginning of sessions in which the patient and provider mutually agree to solutions if privacy is difficult. For instance, it may be agreed upon that unless otherwise instructed by the patient, if a third-party enters the room during the telehealth session, the session will be paused [10▪]. Sound machines in the patient and providers space may also help limit the chances of the session being overheard [10▪].
Barriers regarding therapeutic delivery and corresponding suggestions
Throughout the transition to telehealth, treatment deviations from the traditional clinical care model were unavoidable, and these deviations impacted both patients and providers’ acceptance and comfort toward remote treatment modality [5▪,8▪,10▪,13▪]. For instance, as TMH has not yet been well integrated into children and pediatric psychiatry, clinicians are lacking experience delivering virtual care to this population, therefore raising concerns regarding parental consent and making it difficult for them to ensure treatment effectiveness and overall quality [8▪]. Insufficiency in the experiences and familiarity regarding remote treatments also results in lower confidence in aspects of clinical decision-making (e.g. diagnosis, risk assessment, prescriptions etc.) in comparison with standard face-to-face treatment [8▪,14▪▪]. Difficulties also arise for patients with cognitive problems, hearing deficits and language barriers, in which a reduction has been seen regarding treatment efficacy via telehealth [14▪▪].
One of the largest concerns over remote treatment delivery is the establishment and maintenance of trustworthy, authentic and effective patient–provider relationships [8▪,14▪▪]. The loss of facial and body cues from patients make it challenging for providers to collect key information and maintain effective communication with their patients [10▪,14▪▪]. Both patients and providers may experience various interruptions and distractions from families and home environments, making it more challenging for them to maintain focus during sessions [9▪▪,10▪]. This issue is further compounded with patients who are younger, or experiencing cognitive or behavioral problems. On-screen distractions are also likely to arise when engaging in therapy via a computer [10▪].
The loss of personal boundaries between providers and patients is also of concern, as patients are unintentionally getting more personal information about the medical providers by being able to view their homes. This leads to difficulties in maintaining provider's professionalism during the session, and has the potential to also impact the patient–provider relationship [10▪].
For both providers and patients, increased screen time are likely to cause screen-use fatigue and the feeling of exhaustion [5▪]. Unreasonable operating or scheduling patterns may elicit confusions among patients and burnouts among medical staff [5▪].
Currently, hospitals and clinics are facing the shortage/absence of real-time availability of mental health professionals (e.g. social workers, psychiatrists, dieticians) [8▪]. Providers need to ensure optimal healthcare service provision while utilizing a limited amount of workforce and resources [6▪]. Thus, it is essential for providers to have the distinct competencies and expertise to coordinate multidisciplinary healthcare in an effective manner, and to be able to make the optimal decisions when deciding patients’ priorities [6▪].
Therapeutic barriers for specific patient populations also arise through the use of TMH. For patients with obsessive-compulsive disorder (OCD), they receive a series of exposures (ranging from easy to difficult) as part of their regular treatments. During the treatment transition period, due to quarantine-related distress, there shows a delay in the practices of those more difficult exposures among patients with OCD, thus impeding their regular treatment [10▪]. Other difficulties are encountered by behavioral therapists in the replication of traditional Exposure and Response Prevention therapy among patients with OCD via telehealth [10▪]. For children and adolescent psychiatric patients, school closure and loss of coordination with school personnel further increase the difficulties of full team-based evaluation [6▪].
Families that are unwilling to use video conferencing services often request telephone care [13▪]. As mentioned previously, delivering services via telephone is a viable second option, especially when privacy, technological or financial barriers prevent the use of video conferencing platforms [6▪,14▪▪]. Providers have found that telephone use is the preferred method for patients of lower SES [6▪]. However, one of the limitations for telephone consultations is that it is difficult to maintain the therapeutic alliance merely by talking over the phone, as it often feels less personal [14▪▪]. In addition, the use of telephone prevents any visual or facial cues, making services such as behavioral therapy particularly difficult [10▪]. Training on how to best deliver specific therapeutic interventions via telehealth and necessary modifications for telephone delivery should be provided for all clinicians. To ensure TMH can continue to be conducted via telephone when necessary, insurance companies should reduce the stringency of policies and extend coverage to telephone visits, at least for the duration of the pandemic.
Barriers regarding a sense of community and corresponding suggestions
Due to the confinement measurements implemented during this pandemic period (e.g. quarantine, physical distancing and social isolation), many patients have felt a loss of community, due to loss of interaction with fellow patients (i.e. in waiting rooms) and clinic staff [9▪▪,10▪]. There is also a decrease in support group programming and group sessions throughout treatment [9▪▪,10▪]. Loss of sense of a community appears to be a more prominent issue among individuals with lower SES [9▪▪]. As sessions via telephone appear to often be more convenient for this population, the delivery of group therapy becomes even more unlikely, further compounding the loss of community. In situations where support groups may be beneficial for the client, providers are encouraged to give recommendations for affordable virtual support group options outside of their session [9▪▪].
Similar challenges are faced by clinicians, as some clinics and hospitals are finding that there is insufficient communication between staff due to a loss of in-person interactions [5▪]. To bridge this gap, clinical teams should conduct more frequent check-in's, offer virtual support groups after the treatment day, and provide resources for local and national support groups they can participate in [9▪▪,10▪]. One clinic found that having a staff member or volunteers dedicated to more continuous check-ins with patients was effective in helping patients feel as though they are still part of a supportive community [9▪▪]. To address the problem of communication among medical providers, the use of web-based secure collaborative workspace (e.g. Microsoft Teams), video conference ‘lunchrooms’, and actively sharing self-care tips with other colleagues should be strongly encouraged during this critical period [5▪].
Benefits of telemental health
Although the transition to TMH has come with complications, there have also been many identified benefits. Compared with traditional face-to-face mental healthcare, remote treatment offers greater flexibility for patients, as well as flexibility in working hours for clinicians [7▪,9▪▪]. Clinicians have reported delivering treatment via telehealth has been more convenient and time-saving in comparison with face-to-face treatment [14▪▪]. As TMH sessions are held remotely, there is also an increase in geographic flexibility. Many patients who either had to travel hours to get to treatment, missed appointments or could not receive treatment all together are now able to easily access services [8▪,10▪]. Clinicians have seen a significant decrease in cancellations since the transition to virtual care, which can likely be attributed to the geographical benefits and convenience from being in the comfort of your own home [10▪].
Therapeutic benefits to telepsychiatry have also been identified. Patients have benefited from an increase in parental participation in sessions, as barriers such as different households, travel or scheduling conflicts are not as prominent. This has been particularly beneficial for young patients with mood disorders and attention deficit hyperactivity disorder [8▪]. In addition, video conferencing has provided a unique opportunity for providers to gain insight to patients living conditions and family dynamics that may not otherwise be possible [9▪▪,10▪]. With regard to mental health challenges such as OCD, TMH has provided the chance for providers to identify and assess in-home exposures, that previously required travelling to the patients home. As well, patients are now able to practice techniques with their providers in the environment where certain exposures actually take place [10▪].
Taken together, the transition to telehealth has made us aware of the various benefits to virtual care that have always been present, but never given serious consideration [9▪▪].
Limitations and future directions
One limitation to the current review is the potential of bias in included studies. All studies were case studies and based on providers subjective experience in delivering TMH services. Moreover, all studies were based on experiences within the first few months of the pandemic. As the COVID-19 situation develops, further barriers and benefits have likely surfaced. With the exception of one study, all studies were based on experiences of providers in the United States. Dissemination of knowledge and experiences from a wider range of countries is critical to gain a more comprehensive understanding of the barriers and benefits to TMH.
As social distancing policies persist, it is critical that mental health providers continue to share their experiences with TMH and suggestions to overcome barriers. Future research should include more objective measures, such as retrospective studies and randomized control trials, to further determine barriers and benefits to TMH and how delivery can be optimized for different patient populations.
CONCLUSION
The rapid transition from face-to-face interventions to telehealth platforms has revolutionized the way mental healthcare is delivered around the world. It is important to keep in mind that the suggestions made in this review are not ‘one size fits all.’ Many solutions that work for some patient populations may not benefit others. For example, solutions that may improve therapeutic delivery for some may not be feasible for those of lower SES [9▪▪]. As well, some barriers, such as technical barriers, may be more complicated for larger hospitals and institutions, as opposed to smaller clinics [13▪]. Nevertheless, the transition to TMH has revealed many benefits to this form of mental healthcare delivery, and even once face-to-face interactions can resume, mental health providers should consider maintaining the option of virtual care for patients.
Acknowledgements
A.S., N.M. and Y.Z. all played an equal role in the writing, analysis and synthesis of this review. J.D.R. and R.S.M. contributed significantly to the writing, and synthesis of this review. Hartej Gill (HBSc) and Leanna M.W. Lui (HBSc) contributed significantly to the revision of this work and to the final article proofreading, edits and approval for submission.
Financial support and sponsorship
None.
Conflicts of interest
Dr. Roger McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation; speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Novo Nordisk, Kris, Eisai, Intra-Cellular, Abbvie. Dr. Roger McIntyre is a CEO of Champignon. All other authors have no conflicts of interest to declare.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Whaibeh E, Mahmoud H, Naal H. Telemental health in the context of a pandemic: the COVID-19 experience. Curr Treat Options Psychiatry 2020; 7:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Carlo F, Sociali A, Picutti E, et al. Telepsychiatry and other cutting edge technologies in Covid-19 pandemic: bridging the distance in mental health assistance. Int J Clin Pract 2021; 75:e13716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020; 277:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McIntyre RS, Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry 2020; 19:250–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5▪.Hom MA, Weiss RB, Millman ZB, et al. Development of a virtual partial hospital program for an acute psychiatric population: lessons learned and future directions for telepsychotherapy. J Psychother Integr 2020; 30:366–382. [Google Scholar]; A study providing detailed information of a virtual partial hospital program as well as the acceptability, feasibility and lessons learned based on this experience.
- 6▪.Ramtekkar U, Bridge J, Thomas G, et al. Pediatric telebehavioral health: a transformational shift in care delivery in the era of COVID-19. JMIR Ment Health 2020; 7:e20157. [DOI] [PMC free article] [PubMed] [Google Scholar]; A study describing experiences of utilizing telebehavioral health among pediatric patients with psychological problems during this transition period.
- 7▪.Yellowlees P, Nakagawa K, Pakyurek M, et al. Rapid conversion of an outpatient psychiatric clinic to a 100% virtual telepsychiatry clinic in response to COVID-19. Psychiatr Serv 2020; 71:749–752. [DOI] [PubMed] [Google Scholar]; A study describing the detailed processes, barriers and lessons learned during a rapid conversion from in person to virtual telepsychiatry clinic.
- 8▪.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health 2020; 67:164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]; A study presenting observations, challenges and corresponding solutions during a rapid implementation of adolescent and young adult telemedicine.
- 9▪▪.Falicov C, Niño A, D’Urso S. Expanding possibilities: flexibility and solidarity with under-resourced immigrant families during the COVID-19 pandemic. Fam Process 2020; 59:865–882. [DOI] [PMC free article] [PubMed] [Google Scholar]; An article discussing new challenges encountered by under-resourced immigrant families and mental health therapists during the coronavirus disease 2019 crisis, providing solutions and visualizing new possibilities in mental health support contain familial elements.
- 10▪.Sequeira A, Alozie A, Fasteau M, et al. Transitioning to virtual programming amidst COVID-19 outbreak. Couns Psychol Q 2020; 1–16. [Google Scholar]; A research article presenting effective strategies, benefits, barriers and future directions based on a rapid mental healthcare clinical transition.
- 11.Hoffman DA. Increasing access to care: telehealth during COVID-19. J Law Biosci 2020; 7:lsaa043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8:336–341. [DOI] [PubMed] [Google Scholar]
- 13▪.Sharma A, Sasser T, Schoenfelder Gonzalez E, et al. Implementation of home-based telemental health in a large child psychiatry department during the COVID-19 crisis. J Child Adolesc Psychopharmacol 2020; 30:404–413. [DOI] [PubMed] [Google Scholar]; A study presenting different issues and challenges encountered during the implementation of a home-based telemental health program among young patients with psychiatric care demands.
- 14▪▪.Olwill C, Mc Nally D, Douglas L. Psychiatrist experience of remote consultations by telephone in an outpatient psychiatric department during the COVID-19 pandemic. Ir J Psychol Med 2020; 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]; A comprehensive study discussing identified challenges, benefits and requirements for conducting successful telephone psychiatric consultations based on the experience of a group of Irish psychiatrists.


