Abstract
Purpose of review
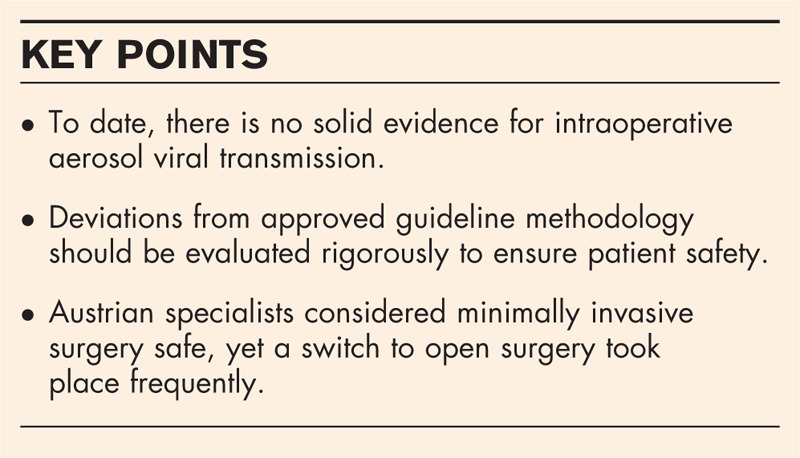
The purpose of this review is to evaluate the risk of intraoperative aerosol viral transmission and the impact of updated COVID-19 guidelines on minimally invasive surgery (MIS) in Austria.
Recent findings
The current literature does not support the risk of intraoperative viral transmission nor does it suggest a harm of minimally invasive procedures in the context of the COVID-19 pandemic. However, medical societies mostly adopted a precautionary approach with a focus on protective measures. Austrian surgeons considered MIS safe during the pandemic and Austria managed to keep the initial outbreak in control. Yet, MIS programs were still affected due to the postponements of elective procedures and switches to other methods by some surgeons.
Summary
The postponement and cancellation of MIS caused complexities in health-care delivery in Austria, whilst the evidence to substantiate this precautionary approach is missing. It must be noted, both the guidelines and our review are limited by the scarcity of evidence. In further consequence, regional factors should be considered while taking precautions. Specific studies on the severe acute respiratory syndrome coronavirus type 2 transmission risk during MIS are urgently needed.
Keywords: Austria, COVID-19, intraoperative viral transmission, minimally invasive surgery, surgical smoke
INTRODUCTION
The COVID-19 outbreak drastically changed healthcare delivery worldwide. Prioritization and reduction of surgical activity were necessary to shift resources to the urgent care of severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) patients. However, this transformation also had an impact on the use of minimally invasive surgery (MIS), which originated from concerns of increased risk of SARS-CoV-2 transmission via pneumoperitoneum for operating theater staff [1]. Surgical smoke and aerosol were already regarded as biohazards before the pandemic [2,3]. The reason for the emerging concern about COVID-19 transmission through MIS stems from the proven presence of several other pathogens in surgical smoke, such as the Human Papilloma Virus (HPV) [4], Hepatitis B Virus (HBV) [5]. Furthermore, a recent study by Wang et al.[6] demonstrated that SARS-CoV-2 can spread via aerosol, similarly to SARS-CoV-1 [7], MERS-CoV [8], H1N1 [9].
Current evidence does suggest the presence of SARS-CoV-2 in various tissues such as gastrointestinal mucosa [10]. Nevertheless, there exists no solid evidence for intraoperative SARS-CoV-2 transmission yet. But due to the uncertainty arising from weak data and lack of experience, many medical societies embraced the precautionary approach, including the European Association of Urology (EAU) [11▪▪], American College of Surgeons (ACS) [12▪], and Royal College of Surgeons [13▪] that recommended rather avoiding laparoscopic or robotic surgery right at the beginning of the pandemic. In contrast, the joint statement of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and European Association for Endoscopic Surgery and other Interventional Techniques (EAES) [14▪] emphasize the proven benefits of MIS and state that there is no evidence for aerosolization of COVID-19 specifically in MIS procedures [4]. All guidelines cite the work of Zheng et al.[15▪▪], which suggests operational adjustments to minimize the exposure, preoperative testing, along with some organizational measures.
Governmental public health measures successfully curbed the transmission of the novel coronavirus in Austria [16▪]. As of March 24, 2021, Austria had 520.050 cases of COVID-19 with 9.121 fatalities [17]. The case fatality rate (CFR) is below the European and the world average [18], thanks to the healthcare system in which virtually all individuals receive publicly funded care [19].
Our aim was to evaluate the risk of intraoperative aerosol viral transmission and to determine the adherence of Austrian surgeons to updated COVID-19 guidelines and the impact of COVID-19 on surgical activity in Austria.
Box 1.
no caption available
EVIDENCE ACQUISITION
We conducted a nonsystematic search in September 2020 using MEDLINE/PubMed database with a focus on articles published to evaluate the risk of intraoperative aerosol viral transmission and COVID-19 guideline recommendations for MIS. We used the following string terms in combination or isolation: ‘COVID-19’, ‘surgical smoke’, ‘aerosol’, ‘surgery’, ’virus’, ‘viral’, ‘guidelines’. Based on eligibility, we selected articles published in the English language and extracted additional relevant publications from authors’ bibliography. Furthermore, to analyze the COVID-19's effect on MIS in Austria, a 15-item, cross-sectional web-based survey was constructed in English using Google Forms. Its structure is based on the Checklist for Reporting Results of Internet E-Surveys [20]. The survey was sent to operators in Austria on April 13, 2020 via E-Mail. Specialists from the fields of general surgery, gynecology, and urology were included. The course of the COVID-19 outbreak in Austria was also summarized.
EVIDENCE SYNTHESIS
Guidelines
The EAU [11▪▪] graded the urologic interventions according to their priority in the context of the COVID-19 pandemic (in 4 grades) and recommends postponement for lower grade operations. According to the EAU, prioritization of the operations should base on the local situation, because the health system capacities and the severity of the pandemic may differ between countries/cities. They suggested that laparoscopic or robotic surgery should only be performed, when it is a necessity, because the released surgical smoke may contain viral particles. The ACS [12▪] also took a similar pathway. They recommended against laparoscopy because of the higher aerosolization and increased droplet transmission hazard [2,3]. In the UK, the main surgical associations released the joint guideline ‘Intercollegiate General Surgery Guidance on COVID-19’ [13▪]. Although they initially suggested avoiding laparoscopy completely on March 25, 2020, after a week they modified this suggestion into considering laparoscopy only when the clinical benefit to the specific patient markedly exceeded the risk of potential viral transmission in that situation. As of July 11, 2020, the joint guideline recommended using laparoscopy, whereas highlighting the importance of precautionary measures [13▪].
However, not all medical associations adopted a precautionary approach in the earlier phases of the pandemic. The SAGES and the EAES released a joint recommendation [14▪] on March 30, 2020, which stated that there is no evidence for aerosolization of COVID-19 specifically in MIS procedures. They emphasized the proven benefits of MIS such as reduced length of stay and fewer complications, whereas recommending the use of devices to filter released CO2 for aerosolized particles during laparoscopy. As of August 8, 2020, this joint statement of SAGES und EAES was subject to change and update [14▪]. Similarly, the Joint Statement on Minimally Invasive Gynecologic Surgery During the COVID-19 Pandemic [21] recommended laparoscopy, but they described a detailed surgical approach with several precautions in laparoscopic procedures. This joint statement was also updated several times, but as of July 20, 2020, no essential change has been made.
Although most guidelines mentioned that circumstances might differ among regions/countries, none of them provided a detailed approach that described how the geographic nature of the pandemic should influence the clinical decision-making process.
Intraoperative viral transmission risk
Currently, there is no evidence on the specific subject of ‘SARS-CoV-2 transmission during MIS’. WHO mentioned contact, droplet, airborne, fomite, fecal-oral, bloodborne, mother-to-child, and animal-to-human transmission in a scientific brief, yet the intraoperative transmission risk was not mentioned [22]. In Basel, a clinical trial [23] is registered with the primary objective to investigate the contamination of surgical smoke and aerosols with SARS-COV-2 virus particles during laparoscopic and open abdominal emergency procedures.
Several reports suggest the presence of viruses in the surgical smoke, such as HBV [5], HPV [24], or human immunodeficiency virus (HIV) [25], but the infectivity of these pathogens remains unclear [26].
HPV is the only virus, of which an infection via surgical smoke is suspected [2]. Gloster Jr. et al.[27] reported a higher prevalence of nasopharyngeal warts in laser surgeons, whereas acknowledging the limitations of their study; such as potential selection bias among the surgeons that responded to the survey, recall bias, or opinion bias by the surgeons. On the other hand, a recent review of Fox-Lewis et al. claims the current recommended precautions to be effective, while also suggesting treating surgical smoke as potentially infectious and underlining the importance of the preventive measures [28].
There are no studies reporting an HBV or HIV transmission via surgical smoke. Likewise, no studies are reporting the transmission of any other coronavirus via surgical smoke either.
COVID-19 pandemic in Austria
The first COVID-19 cases in Austria were reported on February 25, 2020 [29]. After the World Health organization characterized COVID-19 as pandemic on March 11, 2020 [30], the Austrian Federal government imposed several restrictions on social life on 16th March 2020 [29]. With the fast reaction of the authorities and the compliance of the citizens, Austria managed to keep the COVID-19 casualties at a relatively low level. As of March 24, 2021, there were 520.050 cases and 9.151 fatalities in Austria [17]. The CFR and mortality of COVID-19 in Austria are clearly below the EU average [18], which is shown in Fig. 1.
FIGURE 1.

Comparison of Case Fatality Rates in Austria, Germany, European Union, United Kingdom, and the United States. Comparison of Mortality Rates in Austria, Germany, European Union, United Kingdom, and the United States.
Due to the principle of statutory health insurance, 99% of the Austrian population is insured [31]. SARS-CoV-2 testing and treatment were conducted without additional costs for the patients [32]. The bed or ventilator capacities in COVID-19 stations were not in shortage. During the pandemic, there were some critics [33,34] about the scope of testing, since the ‘share of COVID-19 tests that are positive’ hit 20% mark on multiple days by the end of March 2020 in Austria [18]. Austria then managed to reduce this number, which has been between 2 and 6% in the past 60 days with a declining trend. As of March 24, 2021, the COVID-19 situation in Austria is far from over, especially 33.521 active cases and the increasing new infections are considered [17].
Survey
Our survey was submitted to participants on April 13, 2020 and was completed by 84 specialists. Table 1 displays the characteristics of the respondents. Apart from few exceptions, the study participants were urologists, who work in Austria. In total, 26% of participants are faculty doctors and 93% are working in the public sector. By the time of the survey, 72% of the responders were treating COVID-19 patients in their hospital, whereas only 68% of participants were conducting preoperative screening for SARS-CoV-2.
Table 1.
Characteristics of survey respondents (n = 84).
| Position, n (%) | |
| Faculty | 22 (26%) |
| Resident | 62 (74%) |
| Hospital n (%) | |
| Private | 6 (7%) |
| Public | 78 (93%) |
| Treating COVID-19 patients in hospital, n (%) | |
| No | 23 (27%) |
| Yes | 61 (73%) |
| Systematic screening for COVID-19 prior to surgery, n (%) | |
| No | 26 (31%) |
| Yes | 58 (69%) |
Overall, 98% of the respondents stated that COVID-19 affected their surgical program (Fig. 2). In total, 90% of the respondents believe that MIS is a safe option during the pandemic (Fig. 2), although 22% were operating only urgent cases and 74% were operating nonelective and urgent cases (Fig. 2). Minimally invasive operations were postponed by 47% of the surgeons, 15% switched to open surgery and around 12% decided to treat the patients with nonsurgical options (Fig. 2).
FIGURE 2.

Survey results.
In total, 47% of the respondents stated that the COVID-19 pandemic did not change their surgery program (Fig. 2) and 33% of the respondents choose to work without any additional protective measures during the outbreak (Fig. 2). The additional protective measures used by participants were lowest possible intra-abdominal pressure (29%), lowest possible settings for electrosurgical devices (20%), ultrafiltration systems (26%), personal protection devices (54%), and negative pressure rooms (11%) (Fig. 2).
Austria does not have specific guidelines on the subject of ‘MIS during the COVID-19 pandemic’. In total, 64% of Austrian doctors were following standard surgical smoke guidelines before the pandemic (Fig. 2). The EAU Guidelines are followed by 60% of Austrian operators, thus it is the leading recommendation on the subject in Austria (Fig. 2).
DISCUSSION
The present empirical data on the intraoperative aerosol viral transmission is quite poor. The scarcity of information might be due to the complexity of evidence acquisition on the subject. There is not enough data even on the HIV transmission risk during MIS, although AIDS has been a major threat to human health in the last 40 years [35]. Multiple experts underline the weak availability of data for intraoperative transmission risk and emphasize the benefits of MIS for patients [36,37]. However, they also highlight the value of precautionary measures.
The purpose of medical guidelines is to support doctors in light of the latest scientific data. As mentioned above, several leading medical societies released guidelines on MIS during the COVID-19 pandemic. Yet, there is no broad consensus on the recommendations because SARS-CoV-2 is a novel virus, and the pathogen transmission during MIS is not a subject with comprehensive data on it. Many guidelines have adopted a precautionary approach, emphasizing the severity of the pandemic. However, due to various regional factors, the protection strategies cannot be incorporated in the same manner across different countries. Especially when the relatively stable situation of the COVID-19 outbreak in Austria is considered, the lacking compliance of Austrian doctors to the guidelines becomes more understandable. Our critical view is, it is best to stick to the standards until we have clear data, as hasty alterations may pose a serious risk for the patients.
Our survey findings illustrate COVID-19's remarkable effect on minimally invasive operations in Austria, as well as the differences between recommendations and practitioners’ choices. EAU has the most followed guideline in Austria, which suggests the postponement of MIS procedures according to their prioritizations. In contrast, 90% of Austrian doctors think that MIS is a safe option during the COVID-19 pandemic, whereby 47% did not change their MIS programs.
Guideline development is a scientific gradual process of evaluating the best current evidence. The unexpected breakout of the COVID-19 pandemic made a systematic development impossible. There was no time for a comprehensive benefit-risk analysis, wherefore guidelines had to be updated several times.
CONCLUSION
As things stand, the COVID-19 pandemic is far from over in the world, and in Austria. Precautionary measures in our social lives and healthcare seem mandatory. However, the extent of this precautionary approach in medical guidelines must be carefully evaluated, since it affects healthcare delivery directly. In our opinion, the recommendations of medical societies were given too hastily, given the fact that pathogen transmission during MIS is a disputed subject. It must also be noted; no guideline has provided a methodology that describes how the regional severity of the pandemic should affect clinical decision making.
The next obstacle for the Austrian and global medical professionals is to find a way to optimize surgical operations during COVID-19 times. Concrete studies on the SARS-CoV-2 transmission risk during MIS are needed. Austrian medical chambers must assess the risk of minimally invasive procedures during the COVID-19 pandemic so that the interventions can continue with the maximum benefit for all parties.
Acknowledgements
None.
Conceptualization: S.F.S., M.R., B.P., D.H.M., O.Y.; Methodology: S.F.S., M.R., B.P., D.H.M., O.Y; Formal analysis and investigation: B.P., D.H.M., O.Y.; Writing – original draft preparation: O.Y.; Writing – review and editing: M.R., B.P., D.H.M.; Supervision: S.F.S., M.R.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Mowbray N, Ansell J, Warren N, et al. Is surgical smoke harmful to theater staff? a systematic review. Surg Endosc 2013; 27:3100–3107. [DOI] [PubMed] [Google Scholar]
- 2.Barrett WL, Garber SM. Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc 2003; 17:979–987. [DOI] [PubMed] [Google Scholar]
- 3.Alp E, Bijl D, Bleichrodt RP, et al. Surgical smoke and infection control. J Hosp Infect 2006; 62:1–512. [DOI] [PubMed] [Google Scholar]
- 4.Zhou Q, Hu X, Zhou J, et al. Human papillomavirus DNA in surgical smoke during cervical loop electrosurgical excision procedures and its impact on the surgeon. Cancer Manag Res 2019; 11:3643–3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwak HD, Kim S-H, Seo YS, Song K-J. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occupational and environmental medicine 2016; 73:857–863. [DOI] [PubMed] [Google Scholar]
- 6.Wang J, Du G. COVID-19 may transmit through aerosol. Ir J Med Sci 2020; 189:1143–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu ITS, Li Y, Wong TW, et al. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med 2004; 350:1731–1739. [DOI] [PubMed] [Google Scholar]
- 8.Adhikari U, Chabrelie A, Weir M, et al. A case study evaluating the risk of infection from Middle Eastern Respiratory Syndrome Coronavirus (MERS-CoV) in a Hospital Setting Through Bioaerosols. Risk Anal 2019; 39:2608–2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang H, Li X, Ma R, et al. Airborne spread and infection of a novel swine-origin influenza A (H1N1) virus. Virol J 2013; 10:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao F, Tang M, Zheng X, et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 2020; 158:1831–1833. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11▪▪. EAU-Guidelines-Office-Rapid-Reaction-Group-An-organisation-wide-collaborative-effort-to-adapt-the-EAU-guidelines-recommendations-to-the-COVID-19-era; 2020. [Internet]. [cited August 4, 2020]. Available from: https://uroweb.org/guideline/covid-19-recommendations/. [Google Scholar]; EAU recommendations to COVID-19 pandemic, including surgical procedures and risk stratification.
- 12▪. COVID-19: Considerations for Optimum Surgeon Protection Before, During, and After Operation; 2020 [cited July 20, 2020] Available from: URL: https://www.facs.org/covid-19/clinical-guidance/surgeon-protection. [Google Scholar]; FACS recommendations to COVID-19 pandemic, including surgical procedures and risk stratification
- 13▪. Intercollegiate General Surgery Guidance on COVID-19 UPDATE | RCSEd [Internet]; 2020. [cited July 20, 2020]. Available from URL: https://www.rcsed.ac.uk/newspublic-affairs/news/2020/march/intercollegiate-general-surgery-guidance-oncovid-19-update. [Google Scholar]; RCSE recommendations to COVID-19, including surgical procedure.
- 14▪. SAGES and EAES Recommendations Regarding Surgical Response to COVID19 Crisis - SAGES [Internet]; 2020. [cited August 4, 2020]. Available from URL: https://www.sages.org/recommendations-surgical-response-covid-19/. [Google Scholar]; SAGES/EAES recommendation to COVID-19 pandemic, including surgical procedure and risk stratification.
- 15▪▪.Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg 2020; 272:e5–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article is one of the first publications to discuss the issue of intraoperative aerosol viral transmission with a short review on the evidence and lessons learned from the initial experience in China and Italy. Especially, protective measures are presented in detail.
- 16▪.Moshammer H, Poteser M, Lemmerer K, et al. Time course of COVID-19 cases in Austria. Int J Environ Res Public Health 2020; 17:3270. [DOI] [PMC free article] [PubMed] [Google Scholar]; An analysis on the early course of the pandemic in Austria.
- 17. Neuartiges Coronavirus (2019-nCov); 2021 [cited March 24, 2021] Available from: URL: https://www.sozialministerium.at/Informationen-zum-Coronavirus/Neuartiges-Coronavirus-(2019-nCov).html. [Google Scholar]
- 18.Max Roser, Hannah Ritchie, Esteban Ortiz-Ospina, Hasell Joe. (2020) - ‘Coronavirus Pandemic (COVID-19)’. Published online at OurWorldInData.org. Available from URL: ’https://ourworldindata.org/coronavirus’ [Online Resource]. [Google Scholar]
- 19.Bachner F, Bobek J, Habimana K, et al. Austria: Health System Review. Health Syst Transit 2018; 20:1–254. [PubMed] [Google Scholar]
- 20.Eysenbach G. Improving the quality of web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004; 6: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004; 6:e34. 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Transmission of SARS-CoV-2: implications for infection prevention precautions; 2020 [cited August 4, 2020] Available from: URL: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions. [Google Scholar]
- 23. University Hospital, Basel, Switzerland. Is SARS-CoV-2 Contaminating Surgical Aerosols From Laparoscopy and Open Abdominal Surgery?: NCT04444687, 052020; 2020 [cited August 4, 2020] Available from: URL: https://clinicaltrials.gov/ct2/show/NCT04444687. [Google Scholar]
- 24.Garden JM, Kerry O’Banion M, Bakus AD, Olson C. Viral disease transmitted by laser-generated plume (aerosol). Arch Dermatol 2002; 138:1303–1307. [DOI] [PubMed] [Google Scholar]
- 25.Baggish MS, Polesz BJ, Joret D, et al. Presence of human immunodeficiency virus DNA in laser smoke. Lasers Surg Med 1991; 11:197–203. [DOI] [PubMed] [Google Scholar]
- 26.Vourtzoumis P, Alkhamesi N, Elnahas A, et al. Operating during COVID-19: Is there a risk of viral transmission from surgical smoke during surgery? Can J Surg 2020; 63: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gloster HMJ, Roenigk RK. Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J Am Acad Dermatol 1995; 32:436–441. [DOI] [PubMed] [Google Scholar]
- 28.Fox-Lewis A, Allum C, Vokes D, Roberts S. Human papillomavirus and surgical smoke: a systematic review. Occup Environ Med 2020; 77:809–817. [DOI] [PubMed] [Google Scholar]
- 29. Chronologisch sortierte News - Archiv; 2020 [cited July 20, 2020] Available from: URL: https://www.aekwien.at/coronavirus-news-archiv. [Google Scholar]
- 30. Coronavirus Disease (COVID-19) - events as they happen; 2020 [cited July 20, 2020] Available from: URL: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. [Google Scholar]
- 31. Gesundheitssystem - Krankenversorgung | Gesundheitsportal; 2020 [cited July 20, 2020] Available from: URL: https://www.gesundheit.gv.at/gesundheitsleistungen/gesundheitswesen/gesundheitssystem. [Google Scholar]
- 32. FAQ: Testungen und Quarantäne; 2020 [cited July 20, 2020] Available from: URL: https://www.sozialministerium.at/Informationen-zum-Coronavirus/Coronavirus---Haeufig-gestellte-Fragen/FAQ--Testungen-und-Quarantaene.html. [Google Scholar]
- 33. Wird in Österreich zu wenig getestet? Wiener Zeitung 2020 Mar 18 [cited July 20, 2020] Available from. URL: https://www.wienerzeitung.at/nachrichten/politik/oesterreich/2054733-Wird-in-Oesterreich-zu-wenig-getestet.html. [Google Scholar]
- 34. Hohe Dunkelziffer: Warum Wien so wenig Corona-Tests macht; 2020 [cited July 20, 2020] Available from: URL: https://www.kleinezeitung.at/international/corona/5786200/. [Google Scholar]
- 35.Eisinger RW, Fauci AS. Ending the HIV/AIDS pandemic1. Emerging Infect Dis 2018; 24:413–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Francis N, Dort J, Cho E, et al. SAGES and EAES recommendations for minimallyly invasive surgery during COVID-19 pandemic. Surg Endosc 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morris SN, Fader AN, Milad MP, Dionisi HJ. Understanding the ‘Scope’ of the problem: why laparoscopy is considered safe during the COVID-19 pandemic. J Minim Invasive Gynecol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]


