Abstract
Objectives
To assess the association between soft-shell headgear (HG) use and sports-related concussion (SRC). Secondary objectives were to assess the association between HG and superficial head injury and investigate potential increase in injury risk among HG users.
Design
A systematic search in Ovid MEDLINE, Cochrane Library, Scopus, PsycINFO and SPORTDiscus was conducted in April 2020. Inclusion criteria were youth <18, English language, in vivo studies published after 1980 that evaluated SRC and other injury incidence in HG users compared with non-users.
Outcome measures
Incidence rates of SRC, superficial head injury or other injuries.
Results
Eight studies were eligible. The majority (n=5) reported no difference in the rate of SRC among HG users versus non-users. One rugby study identified significantly lower risk of SRC for non-HG users (risk ratio (RR) 0.63; 95% CI 0.41 to 0.98) compared with HG users, whereas a cross-sectional survey of soccer players indicated higher risk of SRC for non-HG users (RR 2.65; 95% CI 1.23 to 3.12) compared with HG users. Three of the four studies investigating superficial head injury found no significant differences with HG use, though the soccer survey reported reduced risk among HG users (RR 1.86; 95% CI 0.09 to 0.11). Increased incidence of injuries to all body regions for rugby HG users was reported in two studies with adjusted RRs of 1.16 (95% CI 1.04 to 1.29) and 1.23 (95% CI 1.00 to 1.50).
Conclusions
HG use was not associated with reduced rates of SRC or superficial head injury in youth soccer and rugby. The possibility of increased injury risk to all body regions for rugby HG users was raised. The need for research specific to youth and female athletes was highlighted.
PROSPERO registration number
CRD42018115310.
Keywords: neurological injury, sports medicine, trauma management, preventive medicine
Strengths and limitations of this study.
This systematic review provides the first comprehensive examination of the limited available evidence for the use of soft-shell padded headgear for sports related concussion prevention in youth athletes.
The review included only five studies that specifically pertained to youth cohorts. Many studies combined adult and youth participants, potentially confounding findings regarding risk taking behaviour with headgear which may differ across age.
The literature search revealed few articles. Included studies generally lacked robust evidence and did not assess the intervention of headgear as the primary outcome. As such, the conclusions should be interpreted with caution.
This review provides an up to date evidence base for community decision making on club headgear mandates and an indication of where data is currently lacking on the topic, specifically in youth and female athletes.
Introduction
Traumatic brain injury (TBI) is a leading cause of disability and death, contributing to a growing worldwide disease burden.1 Global estimates indicate that TBI affects 60 million individuals per year.2 Collision sports are recognised as a significant contributor, with exponential increases in hospital admissions for children and adolescents sustaining TBI since the early 2000s.3 The majority of these are classified as mild TBI, or sports-related concussion (SRC), with one study indicating that SRC emergency department visits have increased by more than 85% in 8–13 years and by more than 200% in 14–19 years.4 Increased public awareness around SRC and higher numbers of youth participation in collision sport are likely contributing to these increases.5
In most cases of youth SRC, symptoms resolve within 4 weeks,6 though some players have protracted recovery with cognitive, behavioural and emotional difficulties that interfere with school attendance, academic endeavours, sporting performance, social life and family relationships for months and sometimes years.7 Playing technique (eg, teaching skills that reduce exposure to head impacts), rule changes (eg, limiting tackling and contact) and the use of protective equipment (eg, hard shell helmets, padded headgear (HG) and mouthguards) are variably implemented as brain injury prevention initiatives in collision sports such as football, rugby and soccer.8 Helmet subtypes include those with a hard-outer shell used in the National Football League in the USA, and soft-shell padded HG, that either fully covers the head (eg, rugby scrum cap) or resembles a headband (eg, soccer HG) with an opening at the top. HG is most commonly used in rugby, with inconsistent uptake in Australian football and soccer,9 although with varying policy guidelines across community clubs. Within the sporting community it is a widely held belief that such HG protects against injury9 and SRC,10 leading some youth Australian football, soccer and rugby clubs to mandate its use.10 11
Previous reviews have evaluated HG effectiveness across a diverse range of HG models and sports (eg, skiing, American football, hockey, etc). Findings indicate evidence for hard-shell helmets in the prevention of severe TBI,12 though findings for SRC prevention with HG are equivocal at best.8 A systematic review by Emery et al found inconsistent evidence for the use of HG in rugby, and more consistent evidence that HG may play a role in soccer SRC prevention.13 The evidence, however, was scarce and largely drawn from cross-sectional, rather than randomised controlled trial (RCT) methods. The most commonly accepted opinion is that HG provides limited or no protection against SRC,14 although, this may be due to a lack of evidence, rather than a lack of effect.15 As such, debate continues with regard to HG for SRC prevention,8 12 and whether there is any evidence to support the notion of potential risk (ie, risk compensation behaviour). The risk compensation hypothesis posits that players may be at greater risk of sustaining injuries due to increased tackling using the head and increases in aggressive play because they assume greater safety when wearing HG.16 17 Importantly, to date, no reviews have focused exclusively on youth populations. Youth may be more vulnerable to risk compensation than adults,18 as the cognitive processes associated with risk taking in the developing brain are immature.19
The primary objective of this study was to assess the in vivo evidence for the intervention of HG for SRC in youth collision sports. Secondary objectives were to assess HG for prevention for superficial head injury (injuries superficial to the skull) and investigate potential indicators of risk compensation behaviour by assessing the association between HG and rates of injury to all body regions.
Methods
The review was conducted in accordance the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.20 See online supplemental file for search strategy.
bmjopen-2020-044320supp001.pdf (11.3KB, pdf)
Patient and public involvement
Over many years, the study investigators have worked clinically in treating patients with SRC, ranging from initial presentation to the Emergency Department, through to specialist treatment clinics providing interventions for those with prolonged symptoms. Whether children should wear HG to play team sports was a frequent question posed by parents, players and sporting club staff.
Data sources
A systematic search was conducted in April 2020 using databases; Ovid MEDLINE, Cochrane Library, Scopus, PsycINFO and SPORTDiscus.
Study selection
Studies were included when the population of interest were athletes under aged 18 years who participated in a collision team sports study assessing the intervention of HG in comparison to no-HG on the primary (SRC) and secondary outcomes (head injury superficial to the skull and/or injuries to other body regions). Included studies were limited to those using quantitative methods to report SRC, head injury and other injury rates (eg, cross sectional survey, prospective cohort injury surveillance, RCTs). Studies were excluded when they did not report data on incidence of SRC, head injury superficial to the skull and/or injuries to other body regions in HG and no-HG groups, were not published in English language, or were published prior to 1980, laboratory based, conducted in adult only cohorts, conducted in individual and/or non-contact sports or only included participants wearing hard-shell helmets. Authors Archbold et al 21 were contacted and agreed to provide additional unpublished data on the rates of SRC sustained by HG users and non-users.
Two review authors (JMK and JN) independently screened manuscripts on title and abstract, selecting agreed citations in full text using the predetermined eligibility criteria. The reviewers then independently screened the selected manuscripts in full text. Disagreements were adjudicated by a senior member of the team.
Data extraction
Data on study design, sporting code, sample size, cohort characteristics, methods, outcomes and covariates predicted to alter injury risk, and main findings were extracted from each study. Description of study participants, injury definitions and the denominators used to compute injury incidence were extracted in as much detail as each study provided. Incidence rate ratios (IRR), relative risk and risk ratios with 95% CI were extracted (if reported) from each study. Where these were not available, relative risk and 95% CIs were calculated using the incidence data available. Due to the expected heterogeneity in reported statistical methods and study design, a meta-analysis was not planned.
Quality and level of evidence assessment
Two reviewers (JMK and JN) independently assessed the quality of non-randomised studies using the nine-item Newcastle-Ottawa Scale (NOS) for Cohort Studies.22 The NOS assesses three domains and assigns up to a maximum of nine points for: (1) selection of cohorts (four points); (2) comparability of cohorts (two points); and (3) outcomes (three points). On this scale, scores between 7 and 9 were considered good quality, and scores 1–6 were considered low quality. The quality of RCTs were assessed using the 11-item Physiotherapy Evidence Database (PEDro) scale.23 On this scale, scores between 9 and 11 were considered excellent quality; 6–8, good quality; 4–5, fair quality and <4, poor quality.24 Reviewers also assessed levels of evidence using the Oxford Centre for Evidence-Based Medicine (OCEBM) guidelines.25 The OCEBM levels range from level 1, representing systematic reviews, level 2 representing randomised trials, level 3 denoting non-randomised controlled cohort/follow-up, level 4 denoting case series, to level 5, denoting mechanistic reasoning. All included studies were assigned a number indicating the level of evidence and quality.
Results
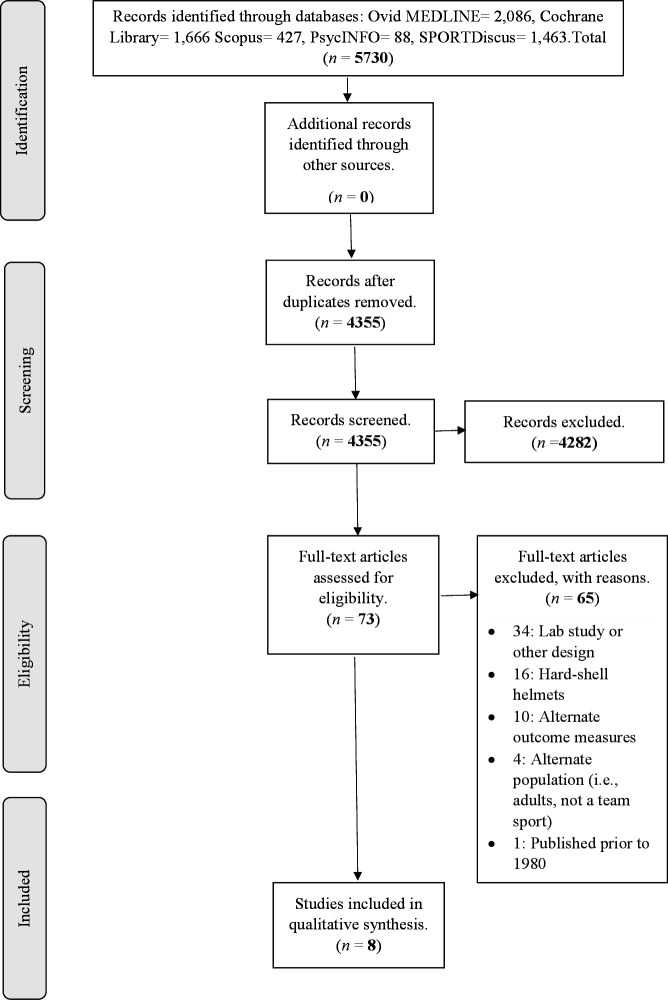
Of the 4355 citations that remained after duplicates were removed, 73 were screened in full text for eligibility and of these, 65 were excluded (figure 1). The most common reasons for exclusion were if studies were laboratory-based or used hard-shell helmets. Studies were also excluded based on outcome measures and alternate populations. After screening, eight studies were included for qualitative analysis and none were excluded based on quality analysis.
Figure 1.
The figure depicts a PRISMA flow chart showing systematic exclusion of articles at each stage of the review. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study characteristics
All studies were published between 2001 and 2019 and study designs included prospective cohort injury surveillance (n=4), RCT (n=2), pilot RCT (n=1) and cross sectional (n=1). There were six rugby and two soccer cohorts, with a total of 12 064 participants. Three studies included female athletes, who represented 2038 (17%) of the total included participants. Of the eight included studies, five were exclusive to youth, and others comprised mixed adult/youth cohorts who ranged in age from 13 to 45 years. Studies examined the effect of HG on rates of SRC (n=6), injuries to other body regions (n=5), head injury superficial to the skull (n=4) and frequency of impacts sustained to the head (n=1). Three studies examined a combination of these outcomes, as they associated the use of soft-shell HG with SRC, superficial head injury and injuries to other body regions. Injury data was typically collected for games and training sessions, with the exception of three studies that included injuries sustained in games only. Study characteristics are summarised in table 1.
Table 1.
Methodological details of studies
| Study | Study design | Sport/ country |
Randomisation of HG use, compliance and wearing rates | Exposure quantification | Level, sex and age: M (SD) | Outcomes | Operational definition of outcomes | Data collection method | Variables adjusted for in analysis |
| McIntosh and McCrory34 | Pilot RCT | Rugby/ Australia |
Random number approach to select 9 HG teams, & 7 non-HG teams. Compliance data NA. |
Player game hours | School competition, males U15s. |
Concussion and head impacts. | Concussion verified by a medical practitioner and classified as a traumatic event that resulted in the player missing a game or training time. | Club personnel completed standardised reporting forms and researchers reviewed video footage. | NA |
| Marshall, et al 30 | Prospective cohort injury surveillance | Rugby/ New Zealand |
Players were asked weekly whether they used protective gear. HG was worn for 14% of player weeks. | Player weeks | Community and school competition, 240 males and 87 females U17 to U22 and 23 and over. | Concussion, head injury and injury for all body regions combined. | Any event that resulted in an injury requiring medical attention or causing a player to miss at least one game or practice. | Researchers completed weekly follow-up interviews with players over the phone. | Protective equipment, level of competition, playing position, playing out of usual position, injury history, frequency of in-season injury, body somatype, fitness level, health status, anger, anxiety, negative affect, task orientation in sport, and perceived importance of injury to team performance. |
| Delaney, et al 39 | Cross sectional study | Soccer/ Canada | Players were retrospectively asked if they wore HG and how often 18.7% of players reportedly used HG (73.1% female). All HG users wore HG for games, while 69.2% wore HG for practices. |
No. of players | Community competition, U13–U18, 180 males and 98 females. | Concussion and head injury. | Concussion symptoms listed were consistent with the Concussion in Sports Group (CISG) statement.59 Head injury defined as abrasions lacerations or contusions. | Players completed retrospective online survey | HG and mouthguard use, sex, age, concussion history, level of experience, and considering oneself as a ‘header’. |
| McIntosh, et al 32 | Cluster RCT | Rugby/ Australia |
HG assigned to rugby teams within a club/ school and level yearly. 45.7% standard HG and 10.8% modified HG compliance. | Player game hours | Community and school competition, U13, U15, U18 and U20 males | Concussion, head injury and injury for all body regions combined. | Concussion in accordance with CISG.60 Injury required on field treatment, a player being removed from the game, or a player missing the next game. | Trained data collectors recorded data on standardised reporting form | Standard HG, modified HG, no HG & competition level. |
| Hollis et al 33 | Prospective cohort injury surveillance | Rugby/ Australia |
Reports on baseline questionnaire outlined 671 players ‘always’ 145 ‘often’, 227 ‘sometimes’ 207 ‘rarely’ and 985 ‘never’ used HG. |
Player game hours | Community competition males 19–45 years. and school competition males aged 15–18 years. 22.7 (5.5) | Concussion | Any event where a player left the field due to dizziness, confusion, loss of coordination, and/or loss of consciousness; and stoppage of play was required, or they received medical attention because of a blow to the head. | Trained data collectors, coaches, club doctors and physical therapists recorded data on standardised reporting forms. | HG and mouthguard use, age, height, weight, impulsivity, time spent training, experience, player position, concussion history, competition level. |
| Chalmers et al 29 | Prospective cohort injury surveillance | Rugby/ New Zealand |
Not reported | Player game hours | Community competition, males aged 13 & above | Injury for all body regions combined. | Any event that resulted in an injury requiring medical attention or causing a player to miss at least one scheduled game or team practice. | Researchers completed weekly follow-up interviews with players over the phone. | Protective equipment. age, ethnicity, experience, lifestyle factors, injury history, player position, training, time of season, foul play, warm ups, weather conditions, ground conditions. |
| Archbold et al 21 | Prospective cohort injury surveillance | Rugby/ Ireland |
46.8% of players reported using HG in a baseline demographic questionnaire prior to the season. | Player game hours | School competition, Males, 16.8 (0.8) | Concussion, head injury and injuries for all body regions combined. | Any injury that prevents a player from taking full part in all training and match play or activities planned for that day for a period of greater than 24 hours from midnight at the end of the day the injury was sustained. | Trained data collectors recorded data using online database. | HG, mouthguard and shoulder pad use, age, weight, height, playing position, injury history, strength profile and experience. |
| McGuine et al 31 | Cluster RCT | Soccer/ USA | Stratified Randomisation using school enrolment size as stratification variable. If a team participated in both years assignment remained the same |
Player game hours | School competition, 1853 females and 913 males, 15.6 (1.2) | Concussion and injuries for all body regions combined, excluding concussion. | Concussion recorded in accordance with National Athletic Trainers Assocation position statement.61 Other injury determined by onset, mechanism, characteristics and physical examination. | Athletic trainers recorded in an online database. | HG use, school, sex, age, year cohort, Sports Concussion Assessment Tool 3 baseline symptom severity and concussion history. |
HG, headgear; NA, not available; RCT, randomised controlled trial.
Quality and levels of evidence results
Interrater agreement for quality analysis between the two reviewers (JMK and JN) assessing the eight included manuscripts was 94.44%. The results for quality assessment and levels of evidence for cohort studies can be seen in table 2. Selection bias was considered low in all studies. Only one study was not awarded full points in this domain, as Delaney et al. 26 did not ascertain the exact number of exposures to SRC reliably due to using self-report, as opposed to direct observation or secure record. For comparability of cohorts, all studies controlled for age, sex and injury history, with only one study not controlling for additional factors. Delaney et al 26 did not account for factors such as player position and player experience that may, in addition to HG use, modify injury rates.27
Table 2.
Results for NOS scale risk of bias assessment and Level of Evidence (OCEBM)
| Study | Selection | Comparability | Outcome | NOS score | OCEBM | ||||||
| A | B | C | D | E | F | G | H | I | |||
| McIntosh and McCrory34 | * | * | * | * | * | * | * | * | * | 9 | 3 |
| Marshall et al 30 | * | * | * | * | * | * | * | * | 8 | 3 | |
| Delaney et al 39 | * | * | * | * | * | * | 6 | 3 | |||
| Hollis et al 33 | * | * | * | * | * | * | * | * | * | 9 | 3 |
| Chalmers et al 29 | * | * | * | * | * | * | * | * | 8 | 3 | |
| Archbold et al 21 | * | * | * | * | * | * | * | * | * | 9 | 3 |
*Criteria met.
A, representativeness of the exposed cohort; B, selection of the non- exposed cohort; C, ascertainment of exposure; D, outcome of interest was not present at start of study; E, study controls for age, sex, injury history; F, study controls for additional factors; G, assessment of outcome; H, follow-up up long enough; I, adequacy of follow-up of cohorts; NOS, Newcastle-Ottawa Scale; OCEBM, Oxford Centre for Evidence-Based Medicine.
For the final domain, three studies did not assess SRC and injury outcomes using an independent observer. The findings of Delaney et al 26 were deemed to have the highest risk of bias due to a cross-sectional survey design with the survey accessible online to players (aged 12–17 years) who could reaccess it multiple times to update SRC symptoms. In addition, the injury definition used did not relate to time lost from participation in sport and/or medical-attention received for injury, the most common definition28 used in all other studies. Two other studies were considered to be subject to the inherent biases associated with self-report data collection, due to a prospective design where researchers completed weekly, postgame follow-up interviews with players over the phone.29 30 These self-reported methods contrasted those used where direct SRC and injury observation was completed by trained data collectors, athletic trainers and medical professionals.
Both RCTs31 32 were assessed as good quality, the OCEBM levels of evidence were scored as two (table 3). On the PEDro scale, they both recieved scores of eight with only three criteria not met (5–7). These criteria related to the blinding of participants, therapists and assessors. It was deemed unfeasible to expect blinding in these studies due to the fact that the intervention (HG use) was directly observable.
Table 3.
Randomisedstudy quality (PEDro scale) and level of evidence (OCEBM)
| Study | Score | OCEBM | |||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |||
| McIntosh et al 32 | * | * | * | * | * | * | * | * | 8 | 2 | |||
| McGuine et al 31 | * | * | * | * | * | * | * | * | 8 | 2 | |||
OCEBM, Oxford Centre for Evidence-Based Medicine; PEDro, Physiotherapy Evidence Database.
Overall, methodology across studies tended to lack scientific rigour in one or more aspects, and incidence of injury was made difficult to interpret due to different methods of reporting injuries (eg, per player, per player weeks, per player hours). The most common convention was for authors to report injuries per player 1000 player games. The two studies who did not conform to this, were subject to retrospective self-report bias. For instance, Marshall et al.,30 obtained injury data from players at weekly intervals and therefore reported by ‘player week’, and Delaney et al.,26 reported injuries ‘per player’, likely because players reported SRC at a single survey time point. These studies likely reported injuries in this way because they did not capture players’ true exposure to injury, and therefore could not report per hour.
Few studies prospectively recorded HG wearing rates throughout the season. Indeed, many studies relied on a questionnaire administered at a single time point asking players whether they used HG. In the Hollis et al. 33 study the authors used a Likert scale (eg, never, rarely, sometimes) to ascertain HG useage rates, and reported that players who ‘always’ wore HG were significant less likely to sustain SRC than those who ‘rarely’ wore HG. First, this is not an accurate reflection of HG use, as players may have decided to use or not use HG depending on how they felt on match day, and second, the rates of SRC among those who ‘always’ wore HG, compared with those who ‘never’ wore HG, were in fact very similar (see table 4 for details).
Table 4.
Outcome data for concussion, head injury and injuries to other body regions stratified by HG versus no-HG
| Study | N | No-HG exposures | HG exposures | No-HG SRC |
HG SRC |
No-HG superficial head injury | HG superficial head injury | No-HG all body regions combined | HG all body regions combined |
| McIntosh and McCrory34 | 294 | 357 player game hours | 1179 player game hours | n=2 *Relative Risk=0.94 95% CI (0.19 to 4.52) |
n=7 | n=7 *Relative risk= 1.54 90% CI (0.63 to 3.75) |
n=15 | – | – |
| Marshall et al 200530 | 304 | 4656 player weeks | 752 player weeks | Not reported | Rate ratio=1.13 95% CI (0.40–3.16) |
Not reported | Rate ratio=0.59, 95% CI (0.19 to 1.85) |
Not reported | Rate ratio= 0.96, 95% CI (0.75 to 1.23) |
| Delaney et al 39 | 278 | n=216 players | n=52 players | n=114 relative risk=2.65, 95% CI (1.23 to 3.12) |
n=14 | n=151 relative risk=1.86, 96% CI (1.49 to 3.45) |
n=15 | – | – |
| Hollis et al 33 | 3207 | n=985 players |
n=671 players | 7.48 per 1000 player hours. *Relative Risk=0.68 95% CI (0.24 to 1.93) |
7.39 per 1000 player hours. | – | – | – | – |
| McIntosh et al 32 | 3686 | 1493 player game hours | Standard HG 1,128 player game hours | n=90 | n=85 with standard HG. Incidence Rate ratio=1.13, 95% CI (0.86 to 1.49) |
n=106 | n=100 with standard HG. Incidence Rate ratio=1.14, 95% CI (0.84 to 1.54) |
n=799 | n=828 with standard HG. Incidence Rate ratio= 1.16, 95% CI (1.04 to 1.29) |
| Modified HG 1474 player game hours |
See above row for control group | n=19 with Modified HG. Incidence Rate ratio=1.06, 95% CI (0.70 to 1.60) |
See above row for control group | n=22 with modified HG. Incidence Rate ratio=1.03 95% CI (0.67 to 1.58) |
See above row for control group | n=175 with modified HG. Incidence Rate ratio=1.05 95% CI (0.78 to 1.41) |
|||
| Chalmers et al 29 | 704 | 4223 player game hours | 1807 player game hours |
– | – | – | – | n=4419 injuries. Incidence rate ratio:1.00 | n=1844 injuries. incidence rate ratio: 1.26 95% CI (1.00 to 1.50) |
| Archbold et al 21 | 811 | n=553 players | n=258 players | n=42 *relative risk=0.63, 95% CI (0.41 to 0.98) |
n=31 | log rank=0.327; df=1; p=0.567) | Not reported | n=549 *relative risk=0.99 95% CI (0.99 to 1.00) |
n=258 |
| McGuine et al 31 | 3050 | n=1545 players | n=1505 players |
n=68 | n=62 risk ratio=0.98, 95% CI (0.62 to 1.56) |
– | – | Not reported | Risk ratio= 0.91, 95% CI (0.64 to 1.29) |
*Denotes crude relative risk as calculated by authorsof the review to facilitate consistency of interpretation. - Denotes missingdata as outcome not analysed in the study.
HG, headgear; SRC, sports related concussion.
The RCTs (of which there were only 2) were the only studies that reliably recorded HG use. Without accurate data on whether players consistently wore HG, the results are prone to bias and confounding as player propensity to risk taking may have been inconsistent across games. In addition, HG uptake was generally low across observational studies, and compliance poor in RCTs, rendering many studies statistically underpowered to assess for difference in outcomes among HG users and non-users. As data reporting methodologies differed across studies, the data presented should be interpreted with caution, especially when comparing results that were obtained across varying contexts with inconsistent definitions of SRC and injury.
HG use and SRC
Outcomes for SRC, superficial head injury, head impacts, and injuries to other body regions stratified by HG use versus no-HG use (No-HG) are listed in table 4. There were seven studies included that analysed SRC. Of these, five (one in soccer and four in rugby) found no differences in rates of SRC with or without HG (see table 4).21 30–32 34 Contrasting findings were seen in two other studies; a prospective cohort study in rugby showed that non-HG users were at significantly lower risk of SRC (risk ratio (RR 0.63; 95% CI 0.41 to 0.98) than HG users, and a cross-sectional survey of soccer players outlined higher risk of SRC for non-HG users (RR 2.65; 95% CI 1.23 to 3.12) compared with HG users.
HG use and superficial head injury
There were four included studies that investigated the association of HG use and superficial head injury. Two assessed rugby cohorts and found no statistically significant difference in rates of sustaining superficial head injury between HG users and non-users.21 34 In the soccer survey study, non-HG users were reported to have higher adjusted risk of superficial head injury (RR=1.86; 96% CI: 0.09 to 0.11) compared with HG users.26 Among the four studies reporting superficial head injury, one reported frequency and type of head impacts using game video analysis. That study found no statistically significant association among HG users (RR: 1.54; 95% CI 0.63 to 3.75) compared with non-HG users.34
HG and injuries to all body regions
There were five included studies that reported on injuries to all body regions. Four of these conducted the analyses with SRC and all body injuries combined as a composite outcome variable.21 29 30 32 Reporting this composite outcome were two studies conducted in rugby with no differences observed in injury rates among HG users vs non-users.21 30 In contrast, Chalmers et al 29 and McIntosh et al 32 reported increases in injury rates to all body regions in rugby players wearing standard HG, adjusted RR: 1.23 (95% CI 1.00 to 1.50) and adjusted RR: 1.16 (95% CI 1.04 to 1.29), respectively. The McIntosh et al 32 study also investigated injury rates to all body regions for players who wore ‘modified HG’. The use of this HG was not associated with increased injury risk, adjusted IRR: 1.05 (95% CI 0.78 to 1.41), although the group accounted for only 11% of exposures to SRC due to poor compliance. The remaining RCT study by McGuine et al 31 reported the outcome of injury to other body regions (excluding SRC) and found no difference in rates for soccer HG users and non-users with adjusted RR=0.91 (95% CI 0.64 to 1.29).
Discussion
The association of HG with SRC, superficial head injury and other injuries
The findings from this review do not support the use of the current, commercially available HG to prevent SRC in youth soccer or rugby. The majority of in vivo evidence is consistent with laboratory research showing that HG does not mitigate the forces associated with head impacts.35–37 Though some protection may be offered against superficial head injury, as purported by Delaney et al 26 and prior studies where HG has been shown to protect against soft tissue injuries sustained to areas of the head covered by padding.38 Importantly, there may also be potential for increased risk of sustaining all types of injuries. Two studies reported 23%29 and 16%32 increases in all types of injury risk for rugby players who wore commercially available HG, and indeed, results from one prospective cohort injury surveillance study indicated higher risk of SRC among players who wore HG.21 Raised by these findings, is the possibility that risk compensation is a phenomena occurring in rugby, but not soccer, as increased injuries were not observed among soccer HG users in a RCT. Soccer is unique in that SRC and other types of injury are sustained when players purposefully use their head to progress the ball,9 when players knock heads39 or when falling over during a tackle.40 In contrast, the majority of SRC and other injuries in rugby are sustained in player to player collisions during full body tackling.40 41 These fundamental differences may render rugby HG users more vulnerable to risk compensation behaviours because injury mechanisms overtly differ and their style of play allows for the head to be used as a tackle weapon.
Given that perceptions about HG and associated behavioural changes may differ across the lifespan, it is unclear whether injury risk associated with HG use differs between adult and youth populations. A commonly held belief reported by youth rugby players is that HG makes them feel safer in contact situations and allows them to play ‘harder’.16 42 A study on HG perceptions among adult and youth rugby players indicated that these beliefs differed with age, as youth tended towards greater acceptance and beliefs in the utility of HG.43Adult HG users may be protected against risk compensation as they are less prone to misguided beliefs about HG.
The studies included in the review span almost two decades raising the possibility that changes in HG technology might influence outcomes. No chronological trends were apparent in the analysis and industry experts are of the opinion that the commercially available HG has not advanced considerably since the 1990s.37 Confounding a summative interpretation was the heterogeneity found in definitions of injury. One study referred to superficial head injury as the ear and scalp only,30 while others included the face21 26 or excluded the face from the definition.32 Some studies defined an injury as occurring only if a player was observed to miss time from play,21 32 33 or received attention from a medic or athletic trainer,31 33 34 while others used retrospective player self-report.26 29 30 Retrospective self-reported methods are not consistent with standards which suggest prospective recording by health professionals is superior to retrospective interview.28 The differences in methodology were prominent in the heterogeneity of outcomes with far higher proportion of SRC recorded when self-reported compared with studies that used direct observation.26 31
Directions for future research
A key finding of this review is that standardised definitions and reliable recording of HG use are vital to ensure the translation of findings to clinicians and the community. It is recommended that injury definitions are guided by the most recently published consensus statements, and that definitions rely on a number of factors to describe severity. It is recommended that an SRC be defined as a ‘TBI induced by biomechanical forces’ with physical, behavioural, cognitive and somatic clinical features documented with each SRC event.6 A superficial head injury should be defined as any injury to the head that is superficial to the skull (including contusions, abrasions and lacerations).26 To capture the full spectrum of SRC and other injuries and facilitate comparison with past results, it is recommended that researchers record all injuries using a combination of ‘broad’ definitions (eg, injury recorded if it causes a player pain or discomfort) and ‘narrow definitions’ (eg, injury recorded if player misses a game).44 As an example, an injury anywhere on the body should be initially documented by body region (eg, lower leg, arm, head) and pathology (bruise, open wound, fracture) if it causes a player pain. Additional information on whether that injury resulted in time lost from play, missed games, required medical attention or resulted in hospital transfer should be collected as surrogates for severity.45 Data collection conducted by a medical professional diagnosing SRC and reliably classifying players as HG users and non-HG users would be optimal, however, we acknowledge this is not possible in most youth community sports. As an alternative, live observation by trained data collectors that are athletic trainers or work in health-related fields has shown promise.28 Video analysis may also have a role in augmenting findings. This could allow researchers to examine the number of head impacts sustained by each player, observe whether the player was wearing HG at the time of impact, and code the behaviours of HG wearers.
Under-representation of female athletes in the included studies was frequently observed. Compared with male athletes, females have been reported to have higher rates of SRC46–50 report more SRC symptoms,51 52 demonstrate worse cognitive impairment following SRC,50 51 and may take longer to recover.52 53 In addition, it has been suggested that females are at higher risk of the effects of subconcussive impacts due to differences in neck strength and body composition.54 Given the exponential increase in female participation in these sports,55–57 further evaluation of injury risk and prevention in this cohort is crucial to future research.
Ultimately, injury surveillance systems specific to youth have not yet been developed, as they largely exist at the elite level and require significant financial and operational resources to conduct.28 Nonetheless, identifying constraints is an important step for researchers conducting future studies to address this important issue. Existing constraints are the potential ethical dilemmas regarding HG being implemented in an RCT because of the lack of evidence that supports its protective benefit versus potential harm. Other barriers include difficulty truly randomising HG (ie, allocation often occurs based on entire teams and is stratified by gender) and poor compliance. For instance, only 11% of exposure hours were attributable to those in the modified HG arm of the McIntosh et al.32 RCT due to very low compliance. A HG RCT conducted in Australian football that was screened for inclusion also revealed that SRC and injury outcomes could not be assessed due to very low compliance in HG use.58 Low compliance was less problematic in the included soccer RCT with 99.5% of those allocated to the HG arm consistently wearing it,31 raising the question of what encourages compliance in these types studies. As seen in McGuine’s (2019) study, players chose their preferred HG model from a range of provided options that met specific testing standards. This potentially contributed to higher compliance because the players had greater involvement and autonomy. It may also be that soccer HG is less intrusive because it covers less of the head and may not induce as much discomfort via increased heat and perspiration.
Strengths and limitations
The primary strength of this review is that it provides a picture of where data is currently lacking, highlights significant evidence gaps particularly in youth and female athletes, and outlines a framework for researchers to further explore this important topic. The review included only five studies that specifically pertained to youth cohorts. Many studies combined adult and youth participants, potentially confounding findings in outcomes due to the higher level of experience, training and increased maturity in risk-taking decision making among adults.19 Without robust data, it was difficult to draw definitive conclusions about the role of HG in sports injury prevention. An important methodological issue was that reporting of results across studies was inconsistent. Reporting of homogeneous outcomes and 95% CIs was not possible in all cases as data was not available, although attempts were made to reanalyse available data to provide consistency.
Conclusion
Extending on the most recent Concussion in Sports Group consensus,6 this review indicates a lack of scientifically rigorous research that clearly outlines the benefit or harm of wearing HG in youth collision sports. Future research should include a representative population and focus on including female participants across a range of sporting codes that use HG. Standardisation of the definitions and measurement of outcome variables are indicated for comparability across studies.
Supplementary Material
Footnotes
Twitter: @Biswadev_M
Contributors: CW was the chief investigator. CW, BM and JMK were involved in the planning, design and registration of the study protocol. JMK conducted the systematic search. JMK and JN screened studies for eligibility. JMK extracted data from studies and wrote the first draft of the manuscript. All authors made revisions and approved the final manuscript.
Funding: This work was supported by the Equity Trustees Walter Cottman Charitable Trust (COTT2017M002) and the Australian Football League (no grant number provided from this organisation).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
References
- 1. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators . Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2019;18:56–87. 10.1016/S1474-4422(18)30415-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dewan MC, Rattani A, Gupta S, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg 2018;130:1080–97. 10.3171/2017.10.JNS17352 [DOI] [PubMed] [Google Scholar]
- 3. Haring RS, Canner JK, Asemota AO, et al. Trends in incidence and severity of sports-related traumatic brain injury (TBI) in the emergency department, 2006-2011. Brain Inj 2015;29:989–92. 10.3109/02699052.2015.1033014 [DOI] [PubMed] [Google Scholar]
- 4. Bakhos LL, Lockhart GR, Myers R, et al. Emergency department visits for concussion in young child athletes. Pediatrics 2010;126:e550–6. 10.1542/peds.2009-3101 [DOI] [PubMed] [Google Scholar]
- 5. Karlin AM. Concussion in the pediatric and adolescent population: "different population, different concerns". Pm R 2011;3:S369–79. 10.1016/j.pmrj.2011.07.015 [DOI] [PubMed] [Google Scholar]
- 6. McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med 2017;51:838–47. 10.1136/bjsports-2017-097699 [DOI] [PubMed] [Google Scholar]
- 7. Beauchamp MH, Aglipay M, Yeates KO, et al. Predictors of neuropsychological outcome after pediatric concussion. Neuropsychology 2018;32:495–508. 10.1037/neu0000419 [DOI] [PubMed] [Google Scholar]
- 8. Bonfield CM, Shin SS, Kanter AS. Helmets, head injury and concussion in sport. Phys Sportsmed 2015;43:236–46. 10.1080/00913847.2015.1039922 [DOI] [PubMed] [Google Scholar]
- 9. Hrysmallis. C. Protective headgear for rugby, Australian rules football and soccer. Sports Injuries, 2015. [Google Scholar]
- 10. Pettersen JA. Does rugby headgear prevent concussion? attitudes of Canadian players and coaches. Br J Sports Med 2002;36:19–22. 10.1136/bjsm.36.1.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Broglio SP, Ju Y-Y, Broglio MD, et al. The efficacy of soccer headgear. J Athl Train 2003;38:220. [PMC free article] [PubMed] [Google Scholar]
- 12. Sone JY, Kondziolka D, Huang JH, et al. Helmet efficacy against concussion and traumatic brain injury: a review. J Neurosurg 2017;126:768–81. 10.3171/2016.2.JNS151972 [DOI] [PubMed] [Google Scholar]
- 13. Emery CA, Black AM, Kolstad A, et al. What strategies can be used to effectively reduce the risk of concussion in sport? A systematic review. Br J Sports Med 2017;51:978–84. 10.1136/bjsports-2016-097452 [DOI] [PubMed] [Google Scholar]
- 14. Rivara FP, Tennyson R, Mills B, et al. Consensus statement on sports-related concussions in youth sports using a modified Delphi approach. JAMA Pediatr 2020;174:79–85. 10.1001/jamapediatrics.2019.4006 [DOI] [PubMed] [Google Scholar]
- 15. Gardner AJ, Quarrie KL, Iverson GL. The epidemiology of sport-related concussion: what the rehabilitation clinician needs to know. J Orthop Sports Phys Ther 2019;49:768–78. 10.2519/jospt.2019.9105 [DOI] [PubMed] [Google Scholar]
- 16. Finch CF, McIntosh AS, McCrory P. What do under 15 year old schoolboy rugby union players think about protective headgear? Br J Sports Med 2001;35:89–94. 10.1136/bjsm.35.2.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Menger R, Menger A, Nanda A. Rugby headgear and concussion prevention: misconceptions could increase aggressive play. Neurosurg Focus 2016;40:E12. 10.3171/2016.1.FOCUS15615 [DOI] [PubMed] [Google Scholar]
- 18. Hagel B, Meeuwisse W. Risk compensation: a “side effect” of sport injury prevention? LWW 2004;14:193–6. 10.1097/00042752-200407000-00001 [DOI] [PubMed] [Google Scholar]
- 19. Steinberg L. Risk taking in adolescence: new perspectives from brain and behavioral science. Curr Dir Psychol Sci 2007;16:55–9. [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 21. Archbold HAP, Rankin AT, Webb M, et al. RISUS study: rugby injury surveillance in ulster schools. Br J Sports Med 2017;51:600–6. 10.1136/bjsports-2015-095491 [DOI] [PubMed] [Google Scholar]
- 22. Wells G, Shea B, O'Connell D. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute, 2009. [Google Scholar]
- 23. Moseley AM, Herbert RD, Sherrington C, et al. Evidence for physiotherapy practice: a survey of the physiotherapy evidence database (PEDro). Aust J Physiother 2002;48:43–9. 10.1016/S0004-9514(14)60281-6 [DOI] [PubMed] [Google Scholar]
- 24. Teasell R, Marshall S, Cullen N. Evidence-Based review of moderate to severe acquired brain injury. Toronto, ON: Ontario Neurotrauma Foundation, 2005. [Google Scholar]
- 25. Howick J, Chalmers I, Glasziou P. The 2011 Oxford CEBM evidence levels of evidence (introductory document). Oxford Center for Evidence Based Medicine, 2011. [Google Scholar]
- 26. Delaney JS, Al-Kashmiri A, Drummond R, et al. The effect of protective headgear on head injuries and concussions in adolescent football (soccer) players. Br J Sports Med 2008;42:110–5. 10.1136/bjsm.2007.037689 [DOI] [PubMed] [Google Scholar]
- 27. McIntosh AS. Risk compensation, motivation, injuries, and biomechanics in competitive sport. Br J Sports Med 2005;39:2–3. 10.1136/bjsm.2004.016188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ekegren CL, Gabbe BJ, Finch CF. Sports injury surveillance systems: a review of methods and data quality. Sports Med 2016;46:49–65. 10.1007/s40279-015-0410-z [DOI] [PubMed] [Google Scholar]
- 29. Chalmers DJ, Samaranayaka A, Gulliver P, et al. Risk factors for injury in rugby Union football in New Zealand: a cohort study. Br J Sports Med 2012;46:95–102. 10.1136/bjsports-2011-090272 [DOI] [PubMed] [Google Scholar]
- 30. Marshall SW, Loomis DP, Waller AE. Evaluation of protective equipment for prevention of injuries in rugby Union. Int J Epidemiol 2004;34:113–8. 10.1093/ije/dyh346 [DOI] [PubMed] [Google Scholar]
- 31. McGuine T, Post E, Pfaller AY, et al. Does soccer headgear reduce the incidence of sport-related concussion? a cluster, randomised controlled trial of adolescent athletes. Br J Sports Med 2020;54:408–13. 10.1136/bjsports-2018-100238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McIntosh AS, McCrory P, Finch CF, et al. Does padded headgear prevent head injury in rugby Union football? Med Sci Sports Exerc 2009;41:306–13. 10.1249/MSS.0b013e3181864bee [DOI] [PubMed] [Google Scholar]
- 33. Hollis SJ, Stevenson MR, McIntosh AS, et al. Incidence, risk, and protective factors of mild traumatic brain injury in a cohort of Australian nonprofessional male rugby players. Am J Sports Med 2009;37:2328–33. 10.1177/0363546509341032 [DOI] [PubMed] [Google Scholar]
- 34. McIntosh AS, McCrory P. Effectiveness of headgear in a pilot study of under 15 rugby Union football. Br J Sports Med 2001;35:167–9. 10.1136/bjsm.35.3.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hassan MHA, Taha Z, Hasanuddin I. Mechanics of soccer heading and protective headgear. Springer, 2018. [Google Scholar]
- 36. McIntosh AS, McCrory P. Impact energy attenuation performance of football headgear. Br J Sports Med 2000;34:337–41. 10.1136/bjsm.34.5.337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Patton DA, McIntosh AS. Considerations for the performance requirements and technical specifications of soft-shell padded headgear. Proceedings of the institution of mechanical Engineers, part P. Journal of sports engineering and technology 2016;230:29–42. [Google Scholar]
- 38. Jones SJ, Lyons RA, Evans R, et al. Effectiveness of rugby headgear in preventing soft tissue injuries to the head: a case-control and video cohort study. Br J Sports Med 2004;38:159–62. 10.1136/bjsm.2002.002584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Delaney JS, Al-Kashmiri A, Drummond R, et al. The effect of protective headgear on head injuries and concussions in adolescent football (soccer) players. Br J Sports Med 2008;42:110–5. discussion 15. 10.1136/bjsm.2007.037689 [DOI] [PubMed] [Google Scholar]
- 40. O’Rourke KP, Quinn F, Mun S, et al. A comparison of paediatric soccer, gaelic football and rugby injuries presenting to an emergency department in Ireland. Injury 2007;38:104–11. 10.1016/j.injury.2006.06.010 [DOI] [PubMed] [Google Scholar]
- 41. Hendricks S, O'Connor S, Lambert M, et al. Video analysis of concussion injury mechanism in under-18 rugby. BMJ Open Sport Exerc Med 2016;2:e000053. 10.1136/bmjsem-2015-000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. White PE, Newton JD, Makdissi M, et al. Knowledge about sports-related concussion: is the message getting through to coaches and trainers? Br J Sports Med 2014;48:119–24. 10.1136/bjsports-2013-092785 [DOI] [PubMed] [Google Scholar]
- 43. Barnes A, Rumbold JL, Olusoga P. Attitudes towards protective headgear in UK rugby union players. BMJ Open Sport Exerc Med 2017;3:e000255. 10.1136/bmjsem-2017-000255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lathlean TJH, Gastin PB, Newstead SV, et al. The incidence, prevalence, severity, mechanism and body region of injury in elite junior Australian football players: a prospective cohort study over one season. J Sci Med Sport 2018;21:1013–8. 10.1016/j.jsams.2018.03.002 [DOI] [PubMed] [Google Scholar]
- 45. Braham R, Finch CF, McCrory P. The incidence of head/neck/orofacial injuries in non-elite Australian football. J Sci Med Sport 2004;7:451–3. 10.1016/S1440-2440(04)80263-9 [DOI] [PubMed] [Google Scholar]
- 46. Gessel LM, Fields SK, Collins CL, et al. Concussions among United States high school and collegiate athletes. J Athl Train 2007;42:495. [PMC free article] [PubMed] [Google Scholar]
- 47. Dick RW. Is there a gender difference in concussion incidence and outcomes? Br J Sports Med 2009;43:i46–50. 10.1136/bjsm.2009.058172 [DOI] [PubMed] [Google Scholar]
- 48. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train 2007;42:311. [PMC free article] [PubMed] [Google Scholar]
- 49. Lincoln AE, Caswell SV, Almquist JL, et al. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med 2011;39:958–63. 10.1177/0363546510392326 [DOI] [PubMed] [Google Scholar]
- 50. Covassin T, Schatz P, Swanik CB. Sex differences in neuropsychological function and post-concussion symptoms of concussed collegiate athletes. Neurosurgery 2007;61:345–51. 10.1227/01.NEU.0000279972.95060.CB [DOI] [PubMed] [Google Scholar]
- 51. Broshek DK, Kaushik T, Freeman JR, et al. Sex differences in outcome following sports-related concussion. J Neurosurg 2005;102:856–63. 10.3171/jns.2005.102.5.0856 [DOI] [PubMed] [Google Scholar]
- 52. Zuckerman SL, Apple RP, Odom MJ, et al. Effect of sex on symptoms and return to baseline in sport-related concussion. J Neurosurg Pediatr 2014;13:72–81. 10.3171/2013.9.PEDS13257 [DOI] [PubMed] [Google Scholar]
- 53. Varriano B, Tomlinson G, Tarazi A, et al. Age, gender and mechanism of injury interactions in post-concussion syndrome. Can J Neurol Sci 2018;45:636–42. 10.1017/cjn.2018.322 [DOI] [PubMed] [Google Scholar]
- 54. Kontos AP, Dolese A, Elbin RJ, et al. Relationship of soccer heading to computerized neurocognitive performance and symptoms among female and male youth soccer players. Brain Inj 2011;25:1234–41. 10.3109/02699052.2011.608209 [DOI] [PubMed] [Google Scholar]
- 55. Cooky C, Messner MA, Hextrum RH. Women play sport, but not on TV: a longitudinal study of televised news media. Communication & Sport 2013;1:203–30. [Google Scholar]
- 56. Jacobs B, Sellars N. The evolution of women’s rugby. In: Routledge Handbook of the Business of Women’s Sport, 2019. [Google Scholar]
- 57. Dick R, Putukian M, Agel J. Descriptive epidemiology of collegiate women’s soccer injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2002–2003. J Athl Train 2007;42:278. [PMC free article] [PubMed] [Google Scholar]
- 58. Braham RA, Finch CF. Do community football players wear allocated protective equipment? descriptive results from a randomised controlled trial. J Sci Med Sport 2004;7:216–20. 10.1016/S1440-2440(04)80011-2 [DOI] [PubMed] [Google Scholar]
- 59. McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport--the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Pm R 2013;5:255–79. 10.1016/j.pmrj.2013.02.012 [DOI] [PubMed] [Google Scholar]
- 60. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport – the 3rd International Conference on concussion in sport held in Zurich, November 2008. South African Journal of Sports Medicine 2009;21. 10.17159/2078-516X/2009/v21i2a296 [DOI] [PubMed] [Google Scholar]
- 61. Broglio SP, Cantu RC, Gioia GA, et al. National athletic trainers' association position statement: management of sport concussion. J Athl Train 2014;49:245–65. 10.4085/1062-6050-49.1.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-044320supp001.pdf (11.3KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.