Abstract
Analysis of health care workers’ stress levels during the COVID-19 virus pandemic, and whether there is a relationship between health care workers’ stress levels and mental health in the context of coping with stress. One hundred and seventy professionally active health care workers took part in the study: doctors (n=41), nurses (n=114) and paramedics (n = 15). On average, study subjects were 37 years old and had 14 years of work experience. The following were used in this questionnaire-based study: General Health Questionnaire (GHQ–28), Perceived Stress Scale (PSS-10), Mini-COPE – Coping Inventory. The research group experienced high levels of stress. Nurses experienced the most acute stress. Increasing stress levels are accompanied by an intensification of psychopathological symptoms (insomnia and depression). Older individuals and those with more years worked at work experienced less psychopathological symptoms. Non-adaptive stress coping methods (e.g. use of psychoactive substances) resulted in deteriorating mental health within the research group. Habitual use of non-adaptive strategies may bring relief in the short term in the form of reduced negative consequences of stress transactions and facilitate mobilisation or just sufficient performance at work. However, in the longer term, it may lead to deteriorating health. The obtained data shows that positive reinterpretation, age and length of work track record constitute protective factors against deteriorating health.
Keywords: COVID-19, Health care professional, Stress
Introduction
The COVID-19 outbreak is a singular and unprecedented event for many health care workers. On the 3rd of March 2020, at a COVID-19 press conference, the Director-General of the World Health Organisation (WHO) in his general remarks said that COVID-19 causes a more severe disease than seasonal influenza.1 Prior studies suggest a relation between virus epidemics and mental health problems currently seen in many populations. Poland’s COVID-19 patient 0 was diagnosed on March 4th, individuals arriving from abroad began spreading infections, horizontal transmission set in and on the 20th of May we had 20 thousand cases. A number of restrictions were imposed: social distancing rules, border closures, movement restrictions. These also resulted in emotional and social needs not being satisfied to the same degree as before. The risk of mental illnesses associated with anxiety and grief brought on by the outbreak of the epidemic is perhaps not emphasised sufficiently; it may affect more people than the infectious disease itself. Mohamed F. Jalloh, MPH, et al. assessed the relation between the proximity of the 2015 EVD outbreak in Sierra Leone and occurrences of mental health problems. Their findings, published in the May 2018 edition of BMJ Global Health,2 have shown that the EVD infection constitutes a threat and is significantly associated with a higher risk of anxiety and depression as well as post-traumatic stress disorder (PTSD).
From a psychological perspective, finding oneself in a pandemic associated with the spread of the COVID-19 virus may be treated as an occurrence of a critical life event.3,4 Such events lead to a new, different life situation and initiate an adaptation process. The change in life conditions affects the whole population; however, it can be assumed that for health care workers (doctors, nurses, paramedics), people diagnosed with the virus and people quarantined due to the possibility of coming into contact with the virus, and people who lost colleagues and friends, the stress is more acute.
The transactional model of psychological stress developed by Lazarus and Folkman (1984)5 is a useful concept for understanding the psychological situation and processes occurring during the struggle with this critical life event. According to Schwarzer and Schulz (2003), it can be assumed that stress transaction is a dynamic process in which successive phases can be identified, including causal determinants, stressor (event) characteristics, intermediary coping processes, effects (direct and distant) and resources and deficits modifying the stress transaction.6 Looked upon from such a perspective, stress is an active process, spread over time. From the research perspective, the features of a stressor, coping processes and the effects of a stress transaction are of key importance to this paper.
Uncertainty of COVID-19 not only threatens people’s physical health, but also affects mental health, especially in terms of emotions and cognition. According to the Behavioural Immune System (BIS) theory,7 people are likely to develop negative emotions (e.g. aversion, anxiety)8 and negative cognitive assessment9 for coping with a crisis situation. Stress as a biological response for the situation—disease spreading, social distancing, etc. —has a negative effect on emotions and develops negative thinking and subjective evaluation of the situation as loss, harm, and the threat of valuable parts of life.10 Long-term negative emotions, when one is unable to isolate themselves from the threat due to one’s work commitments, may reduce the immune function and destroy the balance of their normal physiological mechanisms.11 Therefore, it is essential to understand the potential psychological changes caused by COVID-19.
Coping is defined as the entirety of actions undertaken in a given stress situation. Due to the fact that many stress situations are spread over time, attention is drawn to the dynamic nature of this process, which manifests itself in the variability of the used coping strategies. Lazarus and Folkman’s (1984) classic approach distinguishes two ways of coping: problem-focused and emotion-focused.5 Various coping strategies are employed to achieve these objectives.12 Carver et al. (1989) suggested a classification of coping strategies by identifying 15 actions and behaviours used by people to cope with stress. These are active coping, planning, seeking social support for instrumental problems, seeking social support for emotional problems, suppression of competing activities, turning to religion, positive reinterpretation and growth, mental disengagement, acceptance, focus on/venting emotion, denial, behavioural disengagement, use of psychoactive substances and sense of humour.13 The set of coping strategies put forward by Carver et al. is quite extensive and there are attempts by researchers to reduce it. Wong, Reker and Peacock (2006) indicate a possibility of reducing the number of strategies to three groups: problem-focused coping (e.g. active coping, planning), emotion-focused coping (e.g. positive reinterpretation, acceptance, sense of humour) and dysfunctional coping (e.g. engagement in other actives, denial, venting, use of psychoactive substances).14
The last stage of stress transaction entails identifying its consequences. In this phase, the individual appraises the attempts to cope with stress made to date. Time may be taken into account when analysing the effects of the employed coping strategies. These are then grouped into immediate and long term. Direct consequences include quality of dealing with confrontations, aroused emotional states and physiological changes.15,16 Within the scope of this paper, direct consequences shall be taken to mean changes in the state of mental health.
The following research problems have been formulated in this paper: (1) what is the health care workers’ stress level during the COVID-19 virus pandemic, (2) is there a relationship between health care workers’ stress levels and mental health during the COVID-19 pandemic, and (3) is that relationship mediated by coping strategies?
Material and Methods
Persons working within the healthcare system took part in this study: doctors, nurses and paramedics. The study was performed between 28 April 2020 and 21 September 2020, during the COVID-19 pandemic among medical personnel not in contact with patients infected with the virus. The study was anonymous, voluntary and consensual. The project was approved by the K. Marcinkowski Medical University in Poznań bioethics committee.
One hundred and seventy professionally active health care workers took part in the study: doctors (n=41; 24.1%), nurses (n=114; 67.1%) and paramedics (n= 15; 8.8%). Women constituted the majority of the sample, 142 (83.5%). On average, study subjects were 37 years old (SD=12.23) and had 14years (SD=12.32) of work experience. Subjects executing various medical careers were of a similar age: nurses (M=37; SD=12; min=22; max=68), doctors (M=40; SD=10; min=25; max=65), paramedics (M=33; SD=10; min=24; max=62) (F=1.759(2, 167); p=0.175). There were also no significant differences in job seniority: nurses (M=15; SD=13; min=1; max=41), doctors (M=15; SD=10; min=1; max=40), paramedics (M=11; SD=10; min=1; max=43) (F=0.467(2, 167); p=0.628).
The study was questionnaire-based. Participants completed a set of questionnaires which included the following tools: General Health Questionnaire (GHQ–28),17 Perceived Stress Scale (PSS-10)18 and Mini-COPE – Coping Inventory.13,19 Basic descriptive statistics and reliability coefficients are shown in Tables 1, 2, 3, and 4.
Table 1.
Descriptive statistics for stress level and state of mental health variables
| Variable | Min | Max | M | SD | α-Cronbach | Z Kolmogorov–Smirnov test | |
|---|---|---|---|---|---|---|---|
| Z | p | ||||||
| Stress | 0.00 | 36.00 | 19.72 | 6.97 | 0.87 | 0.068 | 0.052 |
| Stress – helplessness | 0.00 | 20.00 | 11.82 | 4.47 | 0.90 | 0.082 | 0.007 |
| Stress – effectiveness | 0.00 | 12.00 | 6.06 | 2.83 | 0.65 | 0.088 | 0.003 |
| Mental health | 0.00 | 28.00 | 6.32 | 6.32 | 0.92 | 0.159 | <0.001 |
| Somatic symptoms | 0.00 | 7.00 | 2.04 | 2.00 | 0.78 | 0.216 | <0.001 |
| Anxiety | 0.00 | 7.00 | 2.42 | 2.53 | 0.88 | 0.225 | <0.001 |
| Social dysfunction | 0.00 | 7.00 | 1.21 | 1.82 | 0.82 | 0.312 | <0.001 |
| Depression | 0.00 | 8.00 | 0.86 | 1.54 | 0.81 | 0.324 | <0.001 |
Source: in-house materials
Table 2.
Descriptive statistics for problem-focused coping variable
| Variable | Min | Max | M | SD | α-Cronbach | Z Kolmogorov–Smirnov test | |
|---|---|---|---|---|---|---|---|
| Z | p | ||||||
| Problem-focused coping | 0.00 | 18.00 | 12.71 | 3.36 | 0.79 | 0.105 | <0.001 |
| Active coping# | 0.00 | 6.00 | 4.48 | 1.40 | 0.56** | 0.171 | <0.001 |
| Planning# | 0.00 | 6.00 | 4.43 | 1.29 | 0.46** | 0.176 | <0.001 |
| Seeking social support for instrumental reasons# | 0.00 | 6.00 | 3.79 | 1.47 | 0.48** | 0.185 | <0.001 |
Source: authors' work
#As the individual subscales are made up of two test items, the Tau b Kendall correlation coefficient was calculated to determine reliability
Table 3.
Descriptive statistics for emotion-focused coping variable
| Variable | Min | Max | M | SD | α-Cronbach | Z Kolmogorov–Smirnov test | |
|---|---|---|---|---|---|---|---|
| Z | p | ||||||
| Emotion-focused coping | 0.00 | 29.00 | 15.85 | 4.54 | 0.70 | 0.079 | .011 |
| Positive reinterpretation# | 0.00 | 6.00 | 3.82 | 1.45 | 0.53** | 0.226 | <0.001 |
| Acceptance# | 0.00 | 7.00 | 4.08 | 1.25 | 0.37** | 0.244 | <0.001 |
| Sense of humour# | 0.00 | 6.00 | 1.92 | 1.28 | 0.29** | 0.182 | <0.001 |
| Turning to religion# | 0.00 | 6.00 | 2.18 | 2.05 | 0.68** | 0.186 | <0.001 |
| Seeking social support for emotional reasons# | 0.00 | 6.00 | 3.85 | 1.59 | 0.57** | 0.203 | <0.001 |
Source: authors' work
#As the individual subscales are made up of two test items, the Tau b Kendall correlation coefficient was calculated to determine reliability
* p < 0.05; ** p < 0.01
Table 4.
Descriptive statistics for dysfunctional coping variable
| Variable | Min | Max | M | SD | α-Cronbach | Z Kolmogorov–Smirnov test | |
|---|---|---|---|---|---|---|---|
| Z | p | ||||||
| Dysfunctional coping | 0.00 | 33.00 | 13.67 | 5.40 | 0.75 | 0.075 | .022 |
| Engagement in other actives# | 0.00 | 6.00 | 3.65 | 1.62 | 0.47** | 0.132 | <0.001 |
| Denial# | 0.00 | 6.00 | 1.49 | 1.49 | 0.43** | 0.199 | <0.001 |
| Venting# | 0.00 | 6.00 | 2.95 | 1.23 | -0.41 | 0.206 | <0.001 |
| Use of psychoactive substances# | 0.00 | 6.00 | 1.17 | 1.55 | 0.67** | 0.321 | <0.001 |
| Behavioural disengagement# | 0.00 | 6.00 | 1.40 | 1.35 | 0.40** | 0.185 | <0.001 |
| Blame# | 0.00 | 6.00 | 3.01 | 1.55 | 0.44** | 0.143 | <0.001 |
Source: authors' work
#As the individual subscales are made up of two test items, the Tau b Kendall correlation coefficient was calculated to determine reliability
*p < 0.05; **p < 0.01
The Goldberg’s General Health Questionnaire (GHQ-28) was used to perform the Mental Health Assessment.17 The questionnaire comprises 28 questions, which relate to ailments experienced by the subject over the previous weeks. It is used to assess the general state of mental health. In addition, there are 4 subscales (7 items each) to determine the intensity of somatic symptoms, anxiety and insomnia, social dysfunction and depression. Questions include “Have you recently been feeling perfectly well and in good health? Have you recently lost much sleep over worry? Have you recently been managing to keep yourself busy and occupied? Have you recently felt constantly under strain? Have you recently felt that life is entirely hopeless?”
Cohen’s Perceived Stress Scale (PSS-10) was used to estimate the stress level.18 This method makes it possible to determine the level of perceived stress 1 month prior to the test. It consists of ten test items: for example, “In the last month, how often have you felt that you were unable to control the important things in your life?, In the last month, how often have you felt nervous and ‘stressed’?, In the last month, how often have you felt difficulties were piling up so high that you could not overcome them?” which can be assigned to two subscales, which are used to measure feelings of helplessness and self-efficacy.18
The Mini-COPE – Coping Inventory was used to determine stress coping strategies.13,18 The inventory consists of 28 statements allowing to measure 14 strategies of coping with a distressed situation. These are active coping, planning, positive reinterpretation, acceptance, sense of humour, turning to religion, seeking social support for emotional reasons, seeking social support for instrumental reasons, engagement in other actives, denial, venting, use of psychoactive substances, behavioural disengagement and self-blame. The analyses excluded those strategies where the correlation between test items was less than 0.5 (see Tables 2, 3, 4).
Due to the large number of coping strategies, results of works by Coolidge, Segal, Hook and Stewart (2000) were used for general analyses, where three primary coping strategies are identified: problem-focused, emotion-focused and dysfunctional.20r
The obtained data was analysed in four steps. First, stress level and mental health were compared to existing standards. Correlation coefficients between stress levels and mental health were then calculated. As the distribution of the relevant variables differed from the normal distribution, the ρ-Spearman correlation coefficient was calculated. In the next step, a regression equation was formulated and solved, in which mental health was placed on the side of the dependent variable and stress levels, problem-focused coping, emotion-focused coping and dysfunctional coping were treated as independent variables. The fourth step tests the hypothesis about the mediating role of coping in the relationship between stress levels and mental health. A mediation analysis proposed by Preacher and Hayes (2008) was carried out using a resampling procedure, with five thousand repetitions.20
Results
The mean values of stress levels for the whole health care workers group participating in the study are in the high results range (they correspond to sten score 8 according to the standards developed for the PSS-10 questionnaire by Juczyński and Ogińska-Bulik1 (Table 1)). Nurses experienced the most acute stress (M=24.28; SD=4.69; min=0; max=36—value corresponding to sten score 8). This is a higher stress level than that experienced by doctors (M=22.02; SD=4.24; min=4; max=36—value corresponding to sten score 7) and paramedics (M=22.67; SD=3.88; min=6; max=36—value corresponding to sten score 8) (F=4.071(2, 167); p=0.019). The post hoc test results (Tukey’s HSD test) showed that nurses experienced the stress level which was significantly higher than those observed in doctors and paramedics. The latter two groups experienced similar levels of stress.
Mean mental health values were M=6.32; SD=6.32; min=0; max=28, which corresponds to sten score 8 (Table 1). There were no differences in the state of mental health between nurses (M=6.69; SD=6.26; min=0; max=27—value corresponding to sten score 8), doctors (M=5.56; SD=5.74; min=0; max=22—value corresponding to sten score 8) and paramedics (M=5.6; SD=8.30; min=0; max=28—value corresponding to 8 sten score) (F=0.588(2, 167); p=0.556).
The obtained correlation coefficient values show that increasing stress levels are accompanied by an intensification of psychopathological symptoms. Stress levels were positively related to both the general mental health index (ρ=0.70**) and its components. Correlation coefficients were between (ρ=0.50**) for somatic symptoms and (ρ=0.70**) for anxiety and insomnia (Table 5).
Table 5.
Correlation coefficients between stress level and state of mental health
| Mental health | Somatic symptoms | Anxiety | Social dysfunction | Depression | |
|---|---|---|---|---|---|
| Stress | 0.70** | 0.50** | 0.70** | 0.51** | 0.56** |
| Stress – helplessness | 0.67** | 0.50** | 0.69** | 0.45** | 0.52** |
| Stress – effectiveness | 0.42** | 0.26** | 0.45** | 0.33** | 0.33** |
| Age | −0.34** | −0.24** | −0.37** | −0.21** | −0.30** |
| Length of track record at work | −0.31** | −0.21** | −0.34** | −0.18* | −0.29** |
Source: in-house materials
*p < 0.05; **p < 0.01
The state of mental health also depended on the age of the subjects (ρ=−0.34**) and their track record (length) at work (ρ=−0.31**). Older individuals and those with more years worked (above 14 years) experienced less psychopathological symptoms.
Analysing the relationship between coping and mental health, it was found that the use of problem-focused and emotion-focused strategies is in most cases not related to mental health. A relationship was identified only between positive reinterpretation and overall state of mental health (ρ=0.17*) and severity of anxiety and insomnia (ρ=0.17*). Persons using this coping strategy exhibited a lower intensity of symptoms.
It turned out that use of dysfunctional coping strategies is more important for mental health. People using them have lower mental health indicators (ρ=0.43**). For given aspects of health, the correlation coefficient ranged from ρ=0.36** for social dysfunction symptoms to ρ=0.43** for depression symptoms (Table 6).
Table 6.
Correlation coefficients between coping strategies and state of mental health
| Mental health | Somatic symptoms | Anxiety | Social dysfunction | Depression | |
|---|---|---|---|---|---|
| Problem-focused coping | −0.06 | −0.01 | −0.05 | −0.05 | −0.02 |
| Active coping | −0.14 | −0.05 | −0.15 | −0.15 | −0.08 |
| Emotion-focused coping | −0.11 | −0.01 | −0.11 | −0.056 | −0.14 |
| Positive reinterpretation | −0.15* | 0.01 | −0.17* | −0.070 | −0.14 |
| Turning to religion | −0.08 | −0.10 | −0.06 | −0.002 | −0.13 |
| Seeking social support for emotional reasons | −0.08 | −0.04 | −0.07 | −0.003 | −0.06 |
| Dysfunctional coping | 0.46** | 0.38** | 0.41** | 0.36** | 0.43** |
| Use of psychoactive substances | 0.25** | 0.25** | 0.22** | 0.16* | 0.22** |
Source: in-house materials
* p < 0.05; ** p < 0.01
In formulating the regression equation, mental health was assumed to be the dependent variable and stress levels, problem-focused coping, emotion-focused coping and dysfunctional coping were treated as independent variables. Solving the linear regression equation (stepwise method) showed that the factors determining the level of mental health are high stress (β=0.55; p<0.001) and the use of dysfunctional coping strategies (β=0.24; p<0.001). This set of variables explained the level of mental health in 48% (Table 7).
Table 7.
Mental health predictors, stepwise method regression analysis results
| Mental health | |||
|---|---|---|---|
| Predictor | β | t | p |
| Stress level | 0.55 | 8.77 | <0.001 |
| Dysfunctional coping | 0.24 | 3.75 | <0.001 |
| R2 = 0.47, F = 76.894** | |||
| Doctors | |||
| Stress level | 0.58 | 6.72 | <0.001 |
| R2 = 0.53, F = 45.199*** | |||
| Nurses | |||
| Stress level | 0.46 | 6.23 | <0.001 |
| Dysfunctional coping | 0.36 | 4.77 | <0.001 |
| R2 = 0.46, F = 49.654** | |||
| Paramedics | |||
| Stress level | 0.80 | 6.22 | <0.001 |
| Problem-focused coping | −0.38 | −2.98 | <0.001 |
| R2 = 0.77, F = 24.530** | |||
** p < 05
The same equation was applied to groups of doctors, nurses and paramedics and it appeared that the mental health levels in these groups were determined by different predictors. In doctors, the stress level (β=0.58) turned out to be significant and this predictor explained around 53% of the variance in mental health. In nurses, these were the stress level (β=0.46) and dysfunctional coping (β=0.36); these predictors explained around 47% of the variance in mental health. In paramedics, these were the stress level (β=0.80) and problem-focused coping (β=−0.38) and these predictors explained around 77% of the variance in mental health (Table 7).
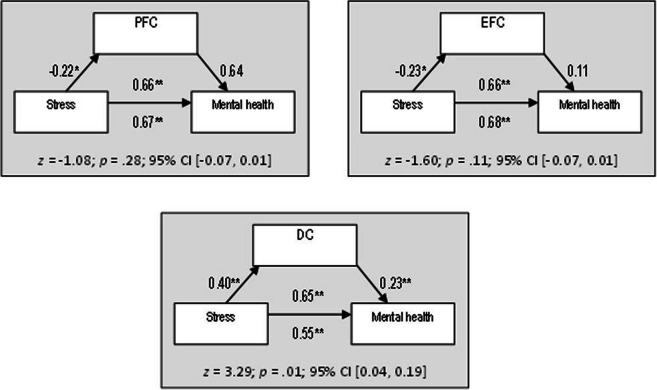
The analysis of simple mediation showed that only dysfunctional coping is a mediator of mental health – stress relationship. This means that people with high stress levels are more likely to have mental disorders as a result of using dysfunctional coping strategies. The observed mediation is of a partial nature, which means that other factors also take part in the relationship in question (Fig. 1). Problem-focused coping and emotion-focused coping did not mediate the relationship.
Figure 1.
Mediating role of coping in a stress—mental health relationship. *p< .01, ** p < 05. PFC problem-focused coping, EFC emotion-focused coping, DC dysfunctional coping
Discussion
Many studies in Poland21 and across the world indicate that work in health care and medical professions (e.g. doctors, nurses, paramedics) is stressogenic.22–25 The results we obtained reflect such data.
The time of the study suggests that in light of a global health crisis, psychosocial occupational stress risk factors, such as the following, may have had a particular impact on the deterioration of mental health: (1) work-related duties, associated with the uncertainty that accompanied the pandemic; (2) the pace and volume of work, in terms of workload in situations where other team members are in quarantine; and (3) work environment and equipment, associated with insufficient availability of personal protective equipment and difficult physical working conditions, e.g. the necessity of using personal protective equipment.
Consequently, the stress resulting from the need to work in an epidemiological emergency has worsened mental health and triggered non-adaptive coping strategies. Habitual use of non-adaptive strategies may bring relief in the short term in the form of reduced negative consequences of stress transactions and facilitate mobilisation or just sufficient performance at work. However, in the longer term, it may lead to deteriorating health. In a crisis situation, a number of personal resources are depleted26; for this reason, an individual may be less likely to use coping strategies that require additional cognitive or emotional resources.
Implications for Behavioral Health
The obtained data shows that age and length of work track record constitute protective factors against deteriorating health. It is likely that older healthcare workers have more life experience in the form of both professional procedural skills and autobiographical memories related to coping with new or uncertain situations. For example, a review of studies on disasters27 has shown that middle-aged adults are more affected by disasters than older people. Younger people, due to their life obligations (e.g. financial burden or family commitments), have less resources at their disposal than older people, who in the face of a crisis can cope better with the demands of unexpected and dangerous situations.28
The study carried out is not error-free. Its first limitation is analysis of general and not occupational stress (or other work-related psychological attributes), which does not allow one to arrive at fully conclusive results on the occupational aspects of medical workers during the COVID-19 pandemic. Another limitation is testing a group identified in the study as medical workers, although we are aware that doctors, paramedics or nurses varies have different duties. The strength of the study lies in capturing the mental functioning of the subjects during the actual pandemic. This data is all the more valuable because it provides information on how people, who work in healthcare, cope in a crisis situation and what the costs are. In further research on this issue, we suggest a more numerous group, which will enable justified inter-group comparisons and longitudinal studies that will capture the dynamics of the observed stress transaction.
Declarations
Conflict of Interest
The authors declare no competing interests.
Ethics Approval and Consent to Participate
All the procedures performed in the current study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Bioethical Commission at Poznan University of Medical Science (reference number 475/20). Written informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO Director-General's opening remarks at the media briefing on COVID-19 - 3 March 2020. World Health Organization (WHO) website. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-3-march-2020. Published March, 2020. Accessed March 20, 2020.
- 2.Jalloh MF, Li W, Bunnell RE et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018. [DOI] [PMC free article] [PubMed]
- 3.Filipp SH. Kritische Lebensereignisse. München: Urban & Schwarzenberg; 2006. [Google Scholar]
- 4.Ziarko M. Zmaganie się ze stresem choroby przewlekłej. Wydawnictwo Naukowe Wydziału Nauk Społecznych UAM: Poznań; 2014. [Google Scholar]
- 5.Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- 6.Schwarzer R, Schulz U. Stressful life events. In: A. M. Nezu, C. M. Nezu, P. A. Geller (Ed.), Handbook of psychology. Volume 9 Health Psychology. (pp. 27-50). Hoboken, New Jersey: John Wiley & Sons, Inc. 2003.
- 7.John ATJ, Natalie JS, Michael AM. The behavioral immune system and social conservatism: A meta-analysis. Evolution and Human Behavior. 2013;34:99–108. doi: 10.1016/j.evolhumbehav.2012.10.003. [DOI] [Google Scholar]
- 8.Mortensen CR, Becker DV, Ackerman JM, et al. Infection breeds reticence: The effects of disease salience on self-perceptions of personality and behavioral avoidance tendencies. Psychological Science. 2010;21:440–447. doi: 10.1177/0956797610361706. [DOI] [PubMed] [Google Scholar]
- 9.Ackerman JM, Becker DV, Mortensen CR, et al. A pox on the mind: Disjunction of attention and memory in the processing of physical disfigurement. Journal of experimental social psychology. 2009;45. [DOI] [PMC free article] [PubMed]
- 10.Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry: Interpersonal and Biological Processes. 2002;65:240–260. doi: 10.1521/psyc.65.3.240.20169. [DOI] [PubMed] [Google Scholar]
- 11.Kiecolt-Glaser JK, McGuire L, Robles TF, et al. Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- 12.Heszen I. Psychologia stresu. Warsaw: Wydawnictwo Naukowe PWN; 2013.
- 13.Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 14.Wong PTP, Reker GT, Peacock EJ. A resource-congruence model of coping and the development of the coping schemas inventory. In: Wong PTP, Wong LCJ, editors. Handbook of Multicultural Perspectives on Stress and Coping. New York: Springer Science Business Media; 2006. [Google Scholar]
- 15.Heszen-Niejodek I. Teoria stresu psychologicznego i radzenia sobie. In: J. Strelau (Ed.), Psychologia. Podręcznik akademicki. Jednostka w społeczeństwie i elementy psychologii stosowanej Gdańsk: Gdańskie Wydawnictwo Psychologiczne; 2000, pp. 465 – 492.
- 16.Ogińska-Bulik N, Juczyński Z. Osobowość stres a zdrowie. Difin: Warsaw; 2008. [Google Scholar]
- 17.Makowska Z, Merecz D. Polska adaptacja kwestionariuszy ogólnego stanu zdrowia Davida Goldberga: GHQ-12 i GHQ-28. In: B. Dudek, (Ed.), Ocena zdrowia psychicznego na podstawie badań kwestionariuszami Davida Goldberga. Podręcznik dla użytkowników kwestionariuszy GHQ-12 GHQ-28 Łódź: Instytut Medycyny Pracy; 2001, pp. 191-264.
- 18.Juczyński Z, Ogińska-Bulik N. Narzędzia pomiaru stresu i radzenia sobie ze stresem. Pracownia Testów Psychologicznych: Warsaw; 2009. [Google Scholar]
- 19.Coolidge FL, Segal DL, Hook JN, et al. Personality disorders and coping among anxious older adults. Journal of Anxiety Disorders. 2000;14:157–172. doi: 10.1016/S0887-6185(99)00046-8. [DOI] [PubMed] [Google Scholar]
- 20.Preacher KJ, Hayes AF. Asymptotic and resamplic strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;30:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- 21.Plopa M, Makarowski R. Kwestionariusz Poczucia stresu. Warszawa: Vizja Press IT; 2010. [Google Scholar]
- 22.Figley CR. Treating compassion fatigue. Brunner-Routledge: New York, NY; 2002. [Google Scholar]
- 23.Smith A, Johal S, Wadsworth E, et al. The scale of occupational stress: The Bristol stress and health at work study. Health & Safety Executive research report no. CRR265. Sudbury: HSEBooks; 2000. [Google Scholar]
- 24.Suzuki S, Ohida T, Kaneita Y, et al. Mental health status, shift work, and occupational accidents among hospital nurses in Japan. Journal of Occupational Health. 2004;46:448–454. doi: 10.1539/joh.46.448. [DOI] [PubMed] [Google Scholar]
- 25.Westphal RJ. Secondary trauma among medical professionals. In: Ch. R. Figley (Ed.), Encyclopedia of trauma: an interdisciplinary guide London SAGE Publications; 2012;594-597.
- 26.Fullerton CS, Ursano RJ, Psychological and Psychopathological Consequences of Disasters West Sussex: John Wiley & Sons Ltd. 2002;13-36.
- 27.Norris FH, Friedman MJ, Watson PJ, et al. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- 28.McFarlane AC. Psychiatric Morbidity Following Disasters: Epidemiology, Risk and Protective Factors. In: JJ. López-Ibor, G. Christodoulou, M. Maj, et al. (Eds.), Disasters and mental health West Sussex: John Wiley & Sons Ltd. 2002;37-63.