ABSTRACT
Objectives
The purpose of this case series was to describe the effects of a biopsychosocial approach that embeds pain neuroscience education (PNE) within physical therapy for improving foot and ankle function, pain, and psychosocial factors in patients with chronic plantar fasciitis.
Methods
Seven female patients (mean [SD] age = 49.0 [11.4] years) receiving physical therapy for chronic plantar fasciitis were enrolled. Along with formal physical therapy, patients received six 15-minute PNE sessions. Knowledge of pain neuroscience was assessed before and after PNE with the Revised Neurophysiology of Pain Questionnaire. Patients completed questionnaires for foot and ankle function (Activities of Daily Living subscale of the Foot and Ankle Ability Measure), pain intensity (Numeric Rating Scale), pain catastrophizing (Pain Catastrophizing Scale), and fear of movement (Tampa Scale for Kinesiophobia) at baseline (before treatment) and 6 and 12 weeks. Local and remote pain sensitivity was assessed using a pressure algometer at baseline and 6 weeks.
Results
Patients attended a mean (range) of 8.7 (7 to 12) physical therapy sessions over a mean (range) of 46.7 (42 to 56) days. After PNE, six (86%) patients demonstrated increased knowledge of pain neuroscience. At 12 weeks, six (86%) patients met or exceeded minimally clinically important difference (MCID) for foot and ankle function and pain. Five (71%) patients met or exceeded MCID for pain catastrophizing and fear of movement. Local pain sensitivity was reduced in six (86%) patients.
Conclusions
Physical therapy integrating PNE is potentially beneficial for patients with chronic plantar fasciitis. Future studies should examine the efficacy of PNE in randomized trials with larger representative samples.
KEYWORDS: Chronic pain, musculoskeletal pain, pain management, pain neuroscience education, physical therapy modalities, plantar fasciitis
Background
Plantar fasciitis, or more broadly plantar heel pain, is a common cause of foot pain leading patients to seek medical care. The prevalence of plantar fasciitis varies across patient samples (i.e., runners, older adults, military), with estimates suggesting plantar fasciitis affects nearly 1% of the general population [1]. Over 1 million patient visits are attributed to plantar fasciitis [2]. The costs of treating plantar fasciitis are estimated to be over 280 USD million per year [3]. Clinical symptoms of plantar fasciitis range in severity from mild tenderness around the heel and bottom of the foot to debilitating pain requiring assistive devices such as crutches [4]. Currently, there are a multitude of conservative treatments for plantar fasciitis including medication, splints, manual therapy, exercise, and orthotic devices [1,5]. The success rate of these treatments for reducing pain and improving function is variable [6,7], with approximately 10% of patients reporting persistent symptoms.
Psychosocial factors are important correlates of clinical outcomes in patients with plantar fasciitis [8–12]. Specifically, pain catastrophizing and fear of movement are two psychosocial factors that can influence how patients respond to injury or treatment. In a cross-sectional study, Cotchett et al. [8] found pain catastrophizing and fear of movement were significantly associated with foot function and pain in multivariable models. After accounting for age, sex, and body mass index (BMI), Cotchett et al. [8] found pain catastrophizing explained an additional 39% of the variability in foot function (total model r square = 43%), while fear of movement explained an additional 21% of variability in foot function (total model r square = 26%) [8]. These preliminary findings suggest pain catastrophizing and fear of movement substantially improve models that include other known predictors and may be important modifiable factors to target in this population.
A biopsychosocial approach to pain management combining physical (i.e., manual therapy, exercise) and psychosocial strategies may be optimal for patients with chronic plantar fasciitis. Pain neuroscience education (PNE) is a strategy that has been used in physical therapy to address pain catastrophizing and fear of movement [13–15]. PNE is a cognitive-based strategy that aims to reconceptualize a patient’s understanding of pain and reduce the threat that pain is a marker of tissue damage [13]. PNE involves education sessions that describe various aspects of the neurobiology and neurophysiology of pain and pain processing within the nervous system. The knowledge gained from PNE can reduce pain catastrophizing and fear [16–18] and decrease pain sensitivity [16,19]. Enhanced pain sensitivity may be an indicator of a centrally sensitized state and contribute to the maintenance of chronic pain [20]. Several studies have shown beneficial therapeutic effects following PNE for patients with low back pain and fibromyalgia [21–23]. Currently, there are no studies describing the effects of PNE within physical therapy management for patients with chronic plantar fasciitis.
The purpose of this prospective case series was to describe the credibility, acceptability, and preliminary effects of physical therapy management that embeds PNE for improving foot and ankle function, pain, and psychosocial outcomes in patients with chronic plantar fasciitis. The results of this study could inform the potential clinical utility of a biopsychosocial approach to chronic pain management for plantar fasciitis.
Methods
Study design
This study was a prospective case series of consecutive patients with chronic plantar fasciitis presenting to a single outpatient physical therapy clinic at Vanderbilt University Medical Center. Ethical approval was obtained by the Institutional Review Board of Vanderbilt University Medical Center.
Participants
Patients referred to physical therapy for the management of chronic unilateral or bilateral plantar fasciitis at Vanderbilt University Medical Center from August 2019 to March 2020 were screened for eligibility. Our target recruitment and retention plan was to enroll 20 patients over a 6-month period and complete the 3-month follow-up in at least 90% of patients. To be considered for enrollment, patients must have met the following inclusion criteria: 1.) English speaking; 2.) between the ages of 18 and 65 years, 3.) had a referring medical diagnosis of plantar fasciitis by a physician, and 4.) had a duration of pain or symptoms for 3 months or longer. At the initial evaluation, physical therapists ruled out other diagnoses and confirmed plantar fasciitis through the patient history and physical examination.
Patients were excluded from enrollment if they met any of the following criteria: 1.) had current trauma or surgery in the affected foot or ankle; 2.) were diagnosed with a cognitive impairment; 3.) had a history of neurological condition such as Parkinson disease, multiple sclerosis, amyotrophic lateral sclerosis; 4.) had symptoms attributable to Complex Regional Pain Syndrome, 5) were receiving care under a worker’s compensation claim, or 6.) were unable to follow-up for scheduled physical therapy visits.
Procedures
After obtaining written informed consent, enrolled patients completed an intake questionnaire for sociodemographic (age, sex, race, ethnicity, education level, marital status, working status) and health-related information (smoking status, affected foot, pain duration, opioid use, expectations for physical therapy). Expectations for physical therapy were assessed using 4 questions assessing overall expectations for complete relief of pain, moderate relief of pain, more physical activity, and prevention of future disability [24]. Patients rated each question on an 11-point numeric scale from low [1] to high [10] expectation. Patients also completed questionnaires for knowledge of pain neuroscience [25], foot and ankle function [26], pain intensity [27], pain catastrophizing [28], and fear of movement [29]. Pain sensitivity assessment using a pressure algometer was assessed by the evaluating physical therapist. After the initial evaluation, patients received six sessions of structured PNE in addition to physical therapy. The duration, frequency, and content of physical therapy was informed by published clinical guidelines for plantar fasciitis [30]. The patient’s height and weight (for BMI), comorbidities (based on the Functional Comorbidity Index [31]), number of physical therapy visits, and total duration of care were extracted from the electronic health record. Follow-up assessments for patient-reported outcomes and psychosocial factors were conducted at 6 and 12 weeks after enrollment. Pressure pain sensitivity was reassessed at 6 weeks only as patients were not available for in-clinic assessments at 12 weeks. Patients also completed an assessment form for assessing credibility and acceptability of their treatment. All data were entered and managed using Research Electronic Data Capture (REDCap) hosted at Vanderbilt University Medical Center [32]. REDCap is a secure, web-based application designed to support data capture for research studies.
Physical therapy with pain neuroscience education
PNE is a cognitive-based educational strategy aimed at reducing pain and improving function through understanding of the biological processes underlying pain [13]. PNE incorporates metaphors, plain language, examples, and pictures to assist in patient learning. PNE was delivered one-on-one by a PNE-trained physical therapist over six treatment sessions. As part of the delivery of PNE, patients were provided with a copy of the Why Do I Hurt?® Workbook (Orthopedic Physical Therapy Products, Minneapolis, MN). The therapist and patient used the workbook content as the basis for education and discussion at each weekly session. Example topics included examining the patient’s pain journey, the body’s alarm system and what contributes to heightened responses, the role of the brain, and strategies to turn down the alarm system. Each physical therapy session lasted 30 to 45 minutes, with approximately 15 minutes devoted to PNE. The frequency and duration of the PNE component of treatment was pragmatically chosen based on feasibility to complete the workbook topics within the clinical visit and time constraints of the outpatient clinic. The patient was given time within the session to complete workbook questions and discuss these with the therapist. Patients were encouraged to apply what they learned at home independently; however, this was not formally tracked. To assess whether PNE influenced the patient’s understanding of pain neuroscience, the Revised Neurophysiology of Pain Questionnaire (Revised NPQ) was completed before and after completion of PNE. The Revised NPQ examines how patients conceptualize the mechanisms of pain. Patients respond to each item with ‘true,’ ‘false,’ or ‘undecided.’ A total percentage score is obtained based on correct responses. The Revised NPQ has been shown to be reliable and to have good test–retest reliability [25].
In addition to PNE, patients received physical therapy informed by evidence-based guidelines for plantar fasciitis from the Academy of Orthopedic Physical Therapy [30]. Physical therapy interventions included therapeutic exercise (stretching/strengthening) and manual therapy (soft tissue and joint mobilizations). Three licensed physical therapists (K.M, E.P., B.C.) delivered the intervention. Physical therapist’s years of clinical experience ranged from 3 to 18 years. None of the physical therapists received formal PNE training within their entry-level clinical degree program. Two physical therapists underwent postgraduate PNE training through coursework and/or residency education. One physical therapist held specialist certification in orthopedics through the American Board of Physical Therapist Specialties. Prior to the start of the study, each therapist underwent two 2-hour training sessions to review the study protocol and PNE delivery. During training sessions, each physical therapist reviewed workbook content, practiced delivery of PNE, and were provided feedback based on mock case scenarios. To ensure adherence to PNE delivery, each therapist completed a checklist at each visit to document that PNE sessions were conducted.
Treatment credibility and acceptability
Patients completed an assessment form for determining credibility and acceptability of their treatment [33,34]. Patients were asked to rate how helpful they felt PNE was to their overall recovery and how likely they would be to recommend PNE to a friend with chronic pain. These two items were scored on an 11-point scale, with 0 indicating ‘not at all helpful/likely’ and 10 indicating ‘extremely helpful/likely.’ We considered scores of 8 or greater as indicating a high level of helpfulness or likelihood to recommend. Patients also reported their level of expectation fulfillment following treatment as ‘yes,’ ‘partially,’ or ‘no.’ Treatment satisfaction was assessed on a 6-point scale ranging from ‘very dissatisfied’ to ‘very satisfied.’ Open-ended feedback was asked regarding what the patient felt was the most important thing they learned or changed because of PNE.
Patient-reported outcomes
Foot and ankle function and pain intensity were assessed with the Activities of Daily Living subscale of the Foot and Ankle Ability Measure (FAAM-ADL) and Numeric Rating Scale (NRS), respectively. These were completed at baseline (prior to treatment) and 6 and 12 weeks.
Foot and ankle function
The FAAM-ADL is a 21-item measure of foot and ankle function involving a range of daily activities [26]. Patients rated each FAAM-ADL item on a 5-point scale, with 0 representing ‘unable to do’ and 4 representing ‘no difficulty.’ Scores on the FAAM-ADL were computed as a percentage between 0 and 100, where 0 indicates an inability to perform daily activities and 100 indicates full function. Scores of approximately 50 or lower indicate at least moderate difficulty in function. The FAAM-ADL subscale has been shown to be a reliable and valid measure for those with foot and ankle disorders [26]. The minimum clinically important difference (MCID) for the FAAM-ADL subscale is 8 points [26].
Pain intensity
The NRS is single-item measure for assessing pain intensity. Patients rated their foot pain, on average, in the past week using a scale from 0 meaning ‘no pain’ to 10 meaning ‘pain as bad as can imagine.’ NRS scores of 4 or higher have been used as a cutoff for moderate levels of pain. The NRS for pain intensity has demonstrated good internal consistency and test-reliability among patients with chronic pain [27,35]. The MCID for the 11-point NRS is 2 points [36,37].
Psychosocial measures
Pain catastrophizing and fear of movement were assessed with the Pain Catastrophizing Scale (PCS) and Tampa Scale for Kinesiophobia (TSK), respectively. These were completed at baseline and 6 and 12 weeks.
Pain catastrophizing
The PCS is a 13-item questionnaire that was used to examine pain catastrophizing [28]. Patients rated each PCS item to the degree they have catastrophic thoughts or beliefs on a 5-point scale, where 0 indicates ‘not at all’ and 4 indicated ‘all the time.’ Scores on the PCS range between 0 and 52, where higher scores represent higher levels of pain catastrophizing. PCS scores of 20 or higher have been suggested as a cutoff for moderate levels of pain catastrophizing [38]. The PCS has shown good reliability, internal consistency, construct validity, and concurrent validity [28,39]. The MCID for the PCS has been reported as a 45% change in score [40].
Fear of movement
The TSK is a 13-item questionnaire that was used to examine fear of movement. Patients scored each TSK item to the degree they felt fearful or concerned about certain situations on a scale from 1 to 4, where 1 indicated ‘strongly disagree’ and 4 indicated ‘strongly agree.’ Scores on the TSK range between 13 and 52, where higher scores represented a greater fear of movement. TSK scores of 37 or higher have been suggested as a cutoff for moderate levels of fear of movement [38]. The TSK has been found to have good internal consistency and test–retest reliability [29,41]. The MCID for the TSK is 4 points [42].
Pain sensitivity
Pressure pain thresholds were assessed as a measure of pain sensitivity using a hand-held pressure algometer (Wagner Instruments, Greenwich, CT) with a 1-cm diameter tip. For testing pressure pain thresholds, a pressure stimulus was applied to the affected plantar fascia (calcaneal attachment) and bilateral upper trapezius (midpoint of muscle belly) at a rate of 1 kg/s. For each stimulus, participants were instructed to report the moment when the pressure sensation first became painful. The amount of pressure (in kg/cm2) was recorded. A total of three measurements were obtained at each site. An average of measurements was computed for the affected plantar fascia (local pain site) and bilateral upper trapezius (remote anatomical site) [43]. The test–retest reliability of pressure pain thresholds has been established in previous studies [44–47]. A pressure pain threshold change of 1.1 to 1.6 kg/cm2 (112 to 154 kilopascals) at the calcaneal region and 1.2 kg/cm2 (113 kilopascals) at the upper trapezius has been reported as indicating true change beyond measurement error [45,46]. Pressure pain thresholds were assessed at baseline and 6 weeks.
Data analysis
Descriptive data including means, standard deviation (SD), and proportions were computed for sociodemographics, clinical, and psychosocial variables. Clinically meaningful findings were based on the number of patients meeting or exceeding MCID values. Exploration of associations was performed for a 6-week change in patient-reported outcomes, knowledge of pain neuroscience, psychosocial measures, and pain sensitivity and 12-week change in patient-reported outcomes and psychosocial measures with a correlogram from the corrplot package [48] in R statistical software [49]. Associations at p-value of 0.10 or lower were depicted as potentially meaningful relationships.
Results
Participants
Thirty-seven consecutive patients were identified for potential eligibility. Of these, 20 patients did not meet eligibility criteria, six patients were not able to be screened for inclusion, and three patients declined participation because of lack of interest. The most common reasons for ineligibility were a condition other than plantar fasciitis (i.e., lateral ankle pain, Achilles tendinopathy), pain not being chronic, or concurrent trauma to the lower extremity.
Eight patients consented to be part of the study; however, one patient withdrew from physical therapy after the initial evaluation and was not enrolled in the case series. The mean (SD) age of the seven enrolled patients was 49.0 (11.4) years (Table 1). All patients were female, educated at the college level, and currently working. Four (57%) patients had bilateral symptoms. At initial evaluation, patient expectations were rated highest for physical therapy resulting in more physical activity (mean [SD] = 8.4 [1.3]) and lowest for physical therapy resulting in complete relief of foot pain (mean [SD] = 5.7 [2.9]). At evaluation and follow-up time points, all patients reported not taking opioid medication for pain.
Table 1.
Baseline patient characteristics
| Characteristics | Mean (SD) or N (%) | Min – Max |
|---|---|---|
| Sociodemographic | ||
| Age, in years | 49.0 (11.4) | 29–63 |
| Sex, N (%) female | 7 (100) | |
| Race, N (%) White | 4 [57] | |
| Ethnicity, N (%) Not Hispanic or Latino | 7 (100) | |
| Education, N (%) some college or more | 7 (100) | |
| Marital status, N (%) married | 4 [57] | |
| Working status, N (%) working | 7 (100) | |
| Health-related | ||
| Smoking status, N (%) smoking | 0 (0) | |
| Body mass index, in kg/m2 | 36.1 (10.2) | 26.1–55.8 |
| Functional Comorbidity Index | 1.6 (1.1) | 0–3 |
| Clinical | ||
| Affected foot | ||
| N (%) Right | 1 [14] | |
| N (%) Left | 2 [29] | |
| N (%) Bilateral | 4 [57] | |
| Pain duration, in months | 14.0 (9.5) | 4–30 |
| Opioid use, N (%) yes | 0 (0) | |
| Expectations for physical therapy | ||
| Complete relief of foot pain, 1–10 scale | 5.7 (2.9) | 1–10 |
| Moderate relief of foot pain, 1–10 scale | 7.1 (2.4) | 3–10 |
| More physically active, 1–10 scale | 8.4 (1.3) | 7–10 |
| Prevent future disability, 1–10 scale | 7.9 (1.9) | 5–10 |
Physical therapy with pain neuroscience education
Patients attended a mean (SD) of 8.7 (1.8) physical therapy sessions (range = 7 to 12 sessions) over a mean (SD) of 46.7 (5.5) days (range = 42 to 56 days). Documented physical therapy interventions included foot and ankle stretching, soft tissue (i.e., plantar fascia) and joint (i.e., subtalar joint) manual therapy, intrinsic foot and lower extremity strengthening, and proprioceptive and balance training. No thermal or electrical modalities were used. All PNE sessions were delivered weekly as planned and documented by the treating physical therapist. Most revised NPQ scores showed an increase in knowledge of pain neuroscience after PNE (Table 2). Five (71%) patients scored higher after PNE, 1 (14%) patient’s score stayed the same, and 1 (14%) patient had a lower score.
Table 2.
Pre-treatment and post-treatment knowledge of pain neuroscience, treatment credibility, and acceptability
| Knowledge of Pain Neuroscience* |
Helpfulness of PNE | Likelihood to recommend PNE |
Expectation fulfillment |
Satisfaction | ||
|---|---|---|---|---|---|---|
| Pre-Treatment | Post-Treatment | |||||
| Patient 1 | 30.8 | 61.5 | 8 | 10 | Yes | Very satisfied |
| Patient 2 | 69.2 | 69.2 | 6 | 6 | Partially | Satisfied |
| Patient 3 | 38.5 | 69.2 | 10 | 10 | Yes | Very satisfied |
| Patient 4 | 30.8 | 53.8 | 9 | 9 | Yes | Very satisfied |
| Patient 5 | 53.8 | 38.5 | 8 | 8 | Yes | Satisfied |
| Patient 6 | 53.8 | 84.6 | 6 | 6 | Yes | Satisfied |
| Patient 7 | 7.7 | 46.2 | 9 | 9 | Partially | Slightly satisfied |
| Mean (SD) | 40.7 (20.2) | 60.4 (15.6) | 8.0 (1.5) | 8.3 (1.7) | - | - |
Abbreviations: PNE = Pain Neuroscience Education.
*Knowledge of pain neuroscience measured with Revised Neurophysiology of Pain Questionnaire.
Treatment credibility and acceptability
Table 2 depicts the scores reported by patients for treatment credibility and acceptability. Five (71%) patients reported a score of 8 or higher for helpfulness of PNE and likelihood of recommending PNE to others. Five (71%) patients stated their expectations were fulfilled and the remaining two (29%) patients said their expectations were partially fulfilled. Six (86%) patients stated they were very satisfied or satisfied with their overall results following treatment. Regarding the most important thing learned or changed because of PNE, patients expressed the importance of understanding pain neurophysiology (‘Need to remember that pain can be due to overexcited nervous system [Patient 6],’ ‘Pain doesn’t always mean stop movement [Patient 3]’) and the need to target pain (‘I have to break the pain cycle [Patient 2],’ ‘My body can be trained to reduce the pain [Patient 5]’).
Treatment effects on patient-reported outcomes
Individual and mean (SD) scores for foot and ankle function (FAAM-ADL) and pain intensity (NRS) are presented in Table 3. At baseline, 3 (43%) patients had moderate difficulty in function based on FAAM-ADL scores of approximately 50 or lower. All patients reported increases on the FAAM-ADL subscale from baseline to follow-up at 6 and 12 weeks, indicating an improvement in foot and ankle function over time. Six (86%) patients met or exceeded MCID for the FAAM-ADL at both follow-up time points.
Table 3.
Baseline, 6-week, and 12-week foot and ankle function, pain intensity, pain catastrophizing, and fear of movement
| Baseline | 6-week | 12-week | |
|---|---|---|---|
| Foot and Ankle Function (FAAM-ADL) | |||
| Patient 1 | 60.7 | 95.2* | 100.0* |
| Patient 2 | 47.6 | 78.6* | 72.6* |
| Patient 3 | 67.9 | 97.6* | 92.9* |
| Patient 4 | 44.0 | 88.1* | 97.6* |
| Patient 5 | 73.8 | 88.1* | 97.6* |
| Patient 6 | 53.8 | 84.5* | 89.3* |
| Patient 7 | 72.4 | 80.0 | 76.3 |
| Mean (SD) | 60.0 (11.9) | 87.4 (7.1) | 89.5 (10.9) |
| Pain Intensity (NRS) | |||
| Patient 1 | 8 | 0* | 0* |
| Patient 2 | 6 | 3* | 3* |
| Patient 3 | 4 | 1* | 1* |
| Patient 4 | 9 | 3* | 2* |
| Patient 5 | 6 | 5 | 5 |
| Patient 6 | 7 | 4* | 3* |
| Patient 7 | 4 | 2* | 2* |
| Mean (SD) | 6.3 (1.9) | 2.6 (1.7) | 2.3 (1.6) |
| Pain Catastrophizing (PCS) | |||
| Patient 1 | 15 | 3* | 0* |
| Patient 2 | 11 | 4* | 8 |
| Patient 3 | 32 | 24 | 12* |
| Patient 4 | 32 | 5* | 0* |
| Patient 5 | 6 | 6 | 1* |
| Patient 6 | 11 | 1* | 0* |
| Patient 7 | 6 | 6 | 5 |
| Mean (SD) | 16.1 (11.3) | 7.0 (7.7) | 3.7 (4.8) |
| Fear of Movement (TSK) | |||
| Patient 1 | 32 | 16* | 14* |
| Patient 2 | 22 | 22 | 26 |
| Patient 3 | 37 | 22* | 25* |
| Patient 4 | 33 | 28* | 23* |
| Patient 5 | 21 | 13* | 20 |
| Patient 6 | 31 | 20* | 18* |
| Patient 7 | 33 | 30 | 28* |
| Mean (SD) | 29.9 (6.0) | 21.6 (6.1) | 22.0 (4.9) |
Abbreviations: FAAM-ADL = Activities of Daily Living subscale of the Foot and Ankle Ability Measure. NRS = Numeric Rating Scale, PCS = Pain Catastrophizing Scale, TSK = Fear Tampa Scale for Kinesiophobia.
*Indicates change from baseline to each follow-up time point that meets or exceeds minimal clinically important difference (MCID) for FAAM-ADL (MCID = 8 points), NRS (MCID = 2 points), PCS (MCID = 45% change) and TSK (MCID = 4 points).
At baseline, all patients had moderate or higher levels of pain based on an NRS score of 4 or higher. All patients reported a decrease in NRS scores from baseline to follow-up at 6 and 12 weeks, indicating a reduction in pain over time. Six (86%) patients met or exceeded MCID for the NRS at both follow-up time points.
Treatment effects on psychosocial measures
Individual and mean (SD) scores for pain catastrophizing (PCS) and fear of movement (TSK) are presented in Table 3. At baseline, two (29%) patients had moderate levels of pain catastrophizing based on a PCS score of 20 or higher. Six (86%) patients reported decreases on the PCS from baseline to 6 weeks and all patients reported decreases from baseline to 12 weeks, indicating a reduction in pain catastrophizing over time. Four (57%) patients met or exceeded MCID for the PCS at 6 weeks and five (71%) patients met or exceeded MCID at 12 weeks.
At baseline, one (14%) had a moderate level of fear of movement based on a TSK score of 37 or higher. Six (86%) patients reported decreases on the TSK from baseline to follow-up at 6 and 12 weeks, indicating a reduction in fear of movement. One (14%) patient’s TSK scores stayed the same from baseline to 6 weeks and increased at 12 weeks. Five (71%) patients met or exceeded MCID for the TSK at both follow-up time points.
Treatment effects on pain sensitivity
Individual and mean (SD) scores for pressure pain thresholds at the affected foot and bilateral trapezius are presented in Table 4. Pressure pain thresholds of the affected foot increased from baseline to 6 weeks in 6 (86%) patients, indicating reduced local pain sensitivity. This change exceeded measurement error in 4 of the 6 patients. Only 3 (43%) patients demonstrated increased pressure pain threshold at the bilateral trapezius, with 1 patient’s score exceeding measurement error. No reduction in mean remote pain sensitivity was noted from baseline to 6 weeks.
Table 4.
Baseline and 6-week pain sensitivity
| Pressure Pain Threshold (Affected Foot) |
Pressure Pain Threshold (Bilateral Trapezius) |
|||
|---|---|---|---|---|
| Baseline | 6-week | Baseline | 6-week | |
| Patient 1 | 4.0 | 6.3 | 1.5 | 2.4 |
| Patient 2 | 1.8 | 3.9 | 2.9 | 2.0 |
| Patient 3 | 5.4 | 6.5 | 5.1 | 4.5 |
| Patient 4 | 4.3 | 8.3 | 1.6 | 3.0 |
| Patient 5 | 6.3 | 5.3 | 3.1 | 2.1 |
| Patient 6 | 4.5 | 5.1 | 3.9 | 2.2 |
| Patient 7 | 8.8 | 9.5 | 3.4 | 3.9 |
| Mean (SD) | 5.0 (2.2) | 6.4 (1.9) | 3.1 (1.3) | 2.9 (1.0) |
Pressure pain thresholds are in kg/cm2.
Exploratory associations between 6 and 12-week change in measures
Associations between 6 and 12-week change in measures are depicted in Figures 1 and 2. Potentially meaningful associations were noted between 6-week change in foot and ankle function and pain intensity with 6-week change in pain catastrophizing and local pain sensitivity. Six-week change in pain intensity was also associated with 6-week change in remote pain sensitivity.
Figure 1.
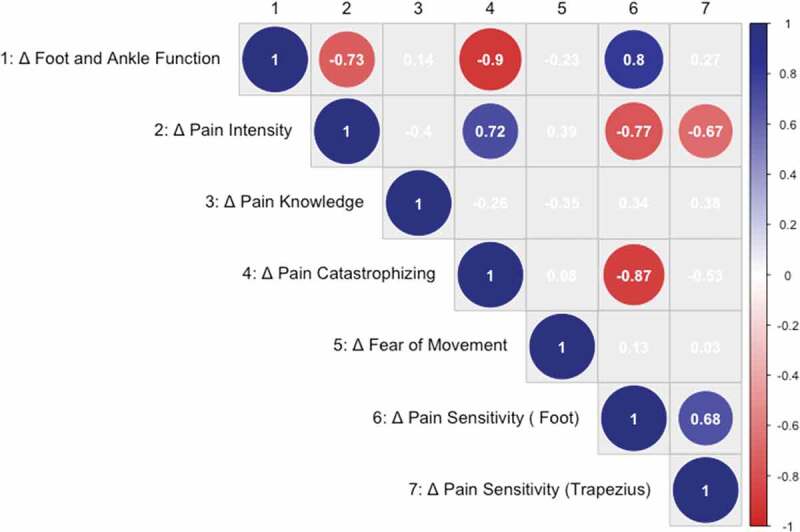
Correlogram depicting associations (p < 0.10) between change in patient-reported outcomes, knowledge of pain neuroscience, psychosocial measures, and pain sensitivity from baseline to 6 weeks. Values are correlation coefficients
Figure 2.
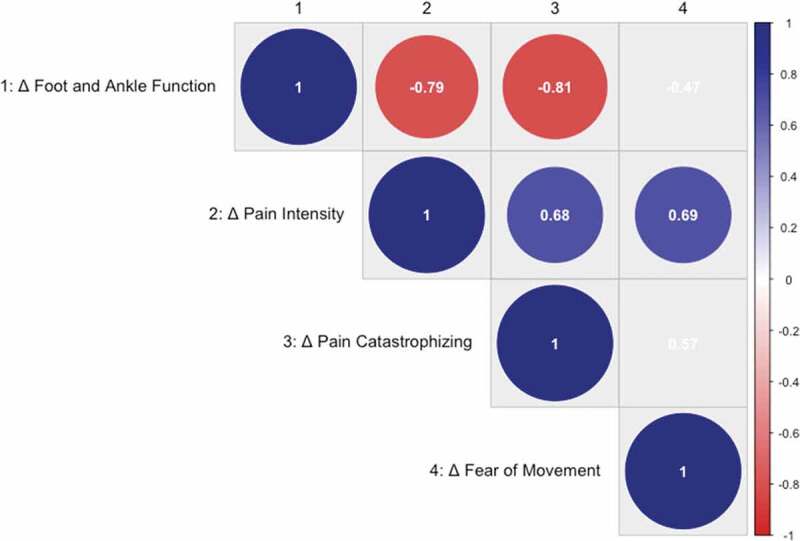
Correlogram depicting associations (p < 0.10) between change in patient-reported outcomes and psychosocial measures from baseline to 12 weeks. Values are correlation coefficients
Twelve-week change in foot and ankle function and pain intensity was associated with 12-week change in pain catastrophizing, while 12-week change in pain intensity was also associated with 12-week change in fear of movement.
Discussion
In this case series, we have described the credibility, acceptability, and preliminary effects of a biopsychosocial approach that embeds PNE into physical therapy for patients with chronic plantar fasciitis. Patients reported the PNE component of our treatment was helpful and they would recommend it to other patients with chronic pain. Most patients reported clinically meaningful improvements at 6 and 12 weeks in foot and ankle function, pain, pain catastrophizing, and fear of movement. Additionally, most patients demonstrated reduced local pain sensitivity at 6 weeks. Our descriptive case series suggests that the integration of PNE within physical therapy may be beneficial to patients with this chronic pain condition.
PNE focuses on content related to the neurobiology and neurophysiology of pain and pain processing within the nervous system. There is empirical support that this specific form of education is efficacious in improving pain knowledge and catastrophizing and reducing disability when combined with other pain management strategies [13,50]. We found PNE within physical therapy to be credible and acceptable to patients. Additionally, our assessment of pain knowledge showed most patients were able to understand and retain PNE concepts. This is in line with the findings of Gallagher et al. [18] who found an improvement in knowledge of pain as well as a reduction in catastrophic thoughts with the use of a metaphor and stories book. In contrast, other studies combining intensive in-person education with a workbook only noted improvements in pain catastrophizing [22]. In our case series, patients reported a mean improvement of approximately 20% on the Revised NPQ. Prior studies of PNE have shown pain knowledge improvements of similar magnitude (i.e., 27%) in a variety of participant groups [51]. Importantly, not all patients in the current case series improved their pain knowledge and a few patients had low post-treatment scores. We did not observe a consistent pattern or association linking improvements in pain knowledge with clinical outcome improvement. We do note, however, that the 2 patients who had the lowest post-treatment pain knowledge scores (patients 5 and 7) were the only patients that did not exceed MCID in both clinical outcome measures. Further investigation is needed to establish whether pain knowledge is a potential mediating factor of the effects of PNE and patient-reported outcomes in this population.
Embedding PNE within physical therapy was feasible. Each PNE session was approximately 15 minutes, which could fit within clinical session templates of busy outpatient settings. Similarly, Louw et al. [51] recently demonstrated the immediate benefits of a brief 15-minute PNE session in patients with recent onset low back pain. To facilitate learning and to enhance standardization of PNE, we used a low-cost workbook. The use of the workbook also enhanced feasibility due to the patient-friendly curriculum and layout, which facilitated meaningful discussions between patient and clinician. Our study showed it was possible to implement PNE by clinicians who had no formal entry-level PNE training within their clinical degree programs and with varying levels of post-graduate PNE coursework and experience (e.g., ranging from no prior PNE experience to some PNE training within physical therapy residency). All of the study physical therapists completed two sessions of PNE training, which represents a minimal burden for training in a psychosocial-based strategy. The workbook may be useful for clinicians who lack extensive training in PNE and allow this potentially beneficial psychosocial treatment strategy to be widely implemented.
Nearly all our patients demonstrated clinically meaningful change in function and pain intensity after treatment. Specifically, patients exhibited a 29.5 point mean improvement in FAAM-ADL scores and a 4 point mean reduction in NRS ratings at 12 weeks. This is a larger magnitude of effect following physical therapy than was observed by McClinton and colleagues [52] among 25 patients with chronic (e.g., duration >7.2 months) plantar fasciitis. The relatively larger outcome effect seen in the current study could relate to differences in the enrolled cohorts, outcome time points, or content and duration of physical therapy. For example, patients in the prior study by McClinton et al. [52] received 6 physical therapy sessions without PNE over 4 weeks and were reassessed at 6 months, while patients in the current case series received 7 to 12 sessions including PNE over 6 to 8 weeks and reassessed at 3 months.
We also observed similar improvement in pain catastrophizing, fear of movement, and local pain sensitivity, which suggests that our biopsychosocial approach may have had a meaningful impact on our theoretical treatment targets. While exploratory, we also noted potentially meaningful associations between changes in these variables and our outcome change in function and pain at 6 and 12 weeks. These results, however, require further evaluation and confirmation in studies with larger sample sizes. Prior studies in patients with musculoskeletal pain have shown improvements following PNE for pain catastrophizing, fear of movement, and pain sensitivity [13]. PNE emphasizes the reconceptualization of pain. Specifically, patients learn that pain can occur due to sensitivity of the nervous system as opposed to tissue damage. This enhanced understanding of pain can address unhelpful thoughts related to pain, which can prompt patients to overcome fear of moving or participating in activities due to the presence of pain [13,53]. Interestingly, one patient showed worsening scores from 6 to 12 weeks in pain catastrophizing (patient 2) and three patients showed worsening scores from 6 to 12 weeks in fear of movement (patients 2, 3, and 5). It may be the case that in some patients, PNE may need to be augmented with other cognitive-behavioral strategies within physical therapy or reviewed and applied over a longer period of time.
Importantly, we paired PNE with guideline-informed physical therapy, which includes manual therapy and therapeutic exercise. Manual therapy is an evidence-based intervention for this patient population [54]. Through PNE, patients understand how pain can be modulated through nervous system processes. This understanding is important for educating patients on how interventions like manual therapy elicit a therapeutic effect. For example, manual therapy, including soft tissue and joint-based techniques, can influence pain modulation through peripheral and central nervous system mechanisms [55,56]. Using PNE language, patients can be offered explanations on how manual therapy can be useful for reducing pain, altering pain sensitivity, and improving outcomes [57].
Limitations
This case series is a small descriptive study. We did not meet our initial targeted recruitment of 20 patients within 6 months due to lower than anticipated volume at our clinic. We ultimately halted our extended recruitment due to the onset of the COVID-19 pandemic. The non-experimental design limits conclusions regarding the efficacy of embedding PNE within physical therapy for plantar fasciitis. Randomized controlled trials are needed to determine whether there is an additive value of incorporating PNE within the plan of care. We depict preliminary associations between change in outcome measures with potential pain-mediating factors. We did not explore additional associations with other factors such as expectations or satisfaction. Caution should be used in interpreting our reported associations as larger sample sizes are required for estimating relationships with greater accuracy and precision. We recruited consecutive patients attending physical therapy; however, our sample was restricted in demographics to female patients. Higher prevalence of plantar fasciitis has been reported among females [1], yet our intention was not to enroll a subset based on sex. Thus, our description of PNE effects lacks generalizability to males. We did not intentionally target PNE to patients with high levels of pain catastrophizing or fear of movement. Despite this, we observed clinically meaningful changes in PCS and TSK scores in this sample. Future work should target PNE to patients at higher psychosocial risk. We did not report longer term outcome scores or track additional non-opioid medication use. Additional studies should aim to establish the effects of PNE beyond the intermediate time frame and consider whether this intervention can influence both opioid and non-opioid pain medication use.
Conclusion
In summary, embedding PNE within physical therapy for patients with chronic plantar fasciitis is a promising and feasible biopsychosocial approach to pain management. We found that over a short time frame, patients demonstrated clinically meaningful improvement in foot and ankle function, pain, and psychosocial factors. This prospective case series provides useful data for informing larger prospective trials.
Biographies
Katherine Mills, PT, DPT, MMHC is a staff physical therapist at Vanderbilt University Medical Center. She specializes in the physical therapy management of patients after trauma and lower extremity limb loss. Dr. Mills obtained her Doctor of Physical Therapy degree from Mayo Clinic and Master of Management in Healthcare from Vanderbilt University.
Emily Preston, PT, MPT graduated from East Tennessee University with as Master's in Physical Therapy degree. She works as a staff physical therapist in the orthopaedics department at Vanderbilt University Medical Center. She is actively engaged in clinical research, primarily in the area of rehabilitation after ACL reconstruction.
Breanna Choffin, PT, DPT, OCS, CMT is a staff physical therapist at Vanderbilt University Medical Center. She is a graduate of St. Ambrose University DPT and residency programs. She is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Haley Brochu, MSA, ATC is a graduate of Mercyhurst University in Erie, PA where she earned her Bachelor's of Science in Athletic Training. She provides patient care at Vanderbilt University Medical Center. She is an Epic certified Clinical Content Builder supporting rehabilitation services.
Eden Schafer, MPH is a Research Coordinator in the Department of Orthopaedic Surgery at Vanderbilt University Medical Center. She is a graduate of the University of Michigan School of Public Health. She has been working in research at Vanderbilt for 10 years.
Payton Robinette, MA is a Research Coordinator in the Department of Orthopaedic Surgery at Vanderbilt University Medical Center. She holds a degree in English and a Master's degree in Medicine, Health, and Society from Vanderbilt University. She plans on attending medical school next year.
Emma Sterling, BE is a Medical Student at George Washington University School of Medicine and Health Sciences. She previously worked as a Research Analyst in the Department of Orthopaedic Surgery at Vanderbilt University Medical Center. She graduated with a degree in Biomedical Engineering from Vanderbilt University.
Rogelio Coronado, PT, PhD is a Research Assistant Professor in the Department of Orthopaedic Surgery and Department of Physical Medicine and Rehabilitation at Vanderbilt University Medical Center. He is core faculty for the Vanderbilt Center for Musculoskeletal Research. Dr. Coronado received his doctoral degree from the University of Florida and physical therapy degree from Texas Tech University Health Sciences Center.
Funding Statement
This work was supported by the National Center for Advancing Translational Sciences [CTSA Award No. UL1 TR002243]; Tennessee Physical Therapy Association. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Nahin RL. Prevalence and pharmaceutical treatment of plantar fasciitis in United States adults. J Pain. 2018;19(8):885–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25(5):303–310. [DOI] [PubMed] [Google Scholar]
- [3].Tong KB, Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthop (Belle Mead NJ). 2010;39(5):227–231. [PubMed] [Google Scholar]
- [4].Irving DB, Cook JL, Young MA, et al. Impact of chronic plantar heel pain on health-related quality of life. J Am Podiatr Med Assoc. 2008;98(4):283–289. [DOI] [PubMed] [Google Scholar]
- [5].Klein SE, Dale AM, Hayes MH, et al. Clinical presentation and self-reported patterns of pain and function in patients with plantar heel pain. Foot Ankle Int. 2012;33(9):693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wolgin M, Cook C, Graham C, et al. Conservative treatment of plantar heel pain: long-term follow-up. Foot Ankle Int. 1994;15(3):97–102. [DOI] [PubMed] [Google Scholar]
- [7].Young CC, Rutherford DS, Niedfeldt MW. Treatment of plantar fasciitis. Am Fam Physician. 2001;63(3):467–74, 77–8. [PubMed] [Google Scholar]
- [8].Cotchett M, Lennecke A, Medica VG, et al. The association between pain catastrophising and kinesiophobia with pain and function in people with plantar heel pain. Foot (Edinb). 2017;32:8–14. [DOI] [PubMed] [Google Scholar]
- [9].Cotchett MP, Whittaker G, Erbas B. Psychological variables associated with foot function and foot pain in patients with plantar heel pain. Clin Rheumatol. 2015;34(5):957–964. [DOI] [PubMed] [Google Scholar]
- [10].Cotchett M, Munteanu SE, Landorf KB. Depression, Anxiety, and Stress in people with and without plantar heel pain. Foot Ankle Int. 2016;37(8):816–821. [DOI] [PubMed] [Google Scholar]
- [11].Drake C, Mallows A, Littlewood C. Psychosocial variables and presence, severity and prognosis of plantar heel pain: A systematic review of cross-sectional and prognostic associations. Musculoskeletal Care. 2018. DOI: 10.1002/msc.1246 [DOI] [PubMed] [Google Scholar]
- [12].Lentz TA, Sutton Z, Greenberg S, et al. Pain-related fear contributes to self-reported disability in patients with foot and ankle pathology. Arch Phys Med Rehabil. 2010;91(4):557–561. [DOI] [PubMed] [Google Scholar]
- [13].Louw A, Zimney K, Puentedura EJ, et al. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. 2016;32(5):332–355. [DOI] [PubMed] [Google Scholar]
- [14].Louw A, Diener I, Butler DS, et al. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehabil. 2011;92(12):2041–2056. [DOI] [PubMed] [Google Scholar]
- [15].Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain: systematic review and meta-analysis. Manual Ther. 2011;16(6):544–549. [DOI] [PubMed] [Google Scholar]
- [16].Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004;8(1):39–45. [DOI] [PubMed] [Google Scholar]
- [17].Meeus M, Nijs J, Van Oosterwijck J, et al. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: a double-blind randomized controlled trial. Arch Phys Med Rehabil. 2010;91(8):1153–1159. [DOI] [PubMed] [Google Scholar]
- [18].Gallagher L, McAuley J, Moseley GL. A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. Clin J Pain. 2013;29(1):20–25. [DOI] [PubMed] [Google Scholar]
- [19].Van Oosterwijck J, Meeus M, Paul L, et al. Pain physiology education improves health status and endogenous pain inhibition in fibromyalgia: a double-blind randomized controlled trial. Clin J Pain. 2013;29(10):873–882. [DOI] [PubMed] [Google Scholar]
- [20].Fernandez-Lao C, Galiano-Castillo N, Cantarero-Villanueva I, et al. Analysis of pressure pain hypersensitivity, ultrasound image, and quality of life in patients with chronic plantar pain: a preliminary study. Pain Med. 2016;17(8):1530–1541. [DOI] [PubMed] [Google Scholar]
- [21].Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297–302. [DOI] [PubMed] [Google Scholar]
- [22].Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–330. [DOI] [PubMed] [Google Scholar]
- [23].Beltran-Alacreu H, Lopez-de-Uralde-Villanueva I, Fernandez-Carnero J, et al. Manual therapy, therapeutic patient education, and therapeutic exercise, an effective multimodal treatment of nonspecific chronic neck pain: a randomized controlled trial. Am J Phys Med Rehabil. 2015;94(10 Suppl 1):887–897. [DOI] [PubMed] [Google Scholar]
- [24].Bishop MD, Mintken PE, Bialosky JE, et al. Patient expectations of benefit from interventions for neck pain and resulting influence on outcomes. J Orthop Sports Phys Ther. 2013;43(7):457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Catley MJ, O’Connell NE, Moseley GL. How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. J Pain. 2013;14(8):818–827. [DOI] [PubMed] [Google Scholar]
- [26].Martin RL, Irrgang JJ, Burdett RG, et al. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26(11):968–983. [DOI] [PubMed] [Google Scholar]
- [27].Jensen MP, Turner JA, Romano JM, et al. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83(2):157–162. [DOI] [PubMed] [Google Scholar]
- [28].Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7(4):524–532. [Google Scholar]
- [29].Roelofs J, Goubert L, Peters ML, et al. The Tampa Scale for Kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur J Pain. 2004;8(5):495–502. [DOI] [PubMed] [Google Scholar]
- [30].Martin RL, Davenport TE, Reischl SF, et al. Heel pain-plantar fasciitis: revision 2014. J Orthop Sports Phys Ther. 2014;44(11):A1–33. [DOI] [PubMed] [Google Scholar]
- [31].Groll DL, To T, Bombardier C, et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58(6):595–602. [DOI] [PubMed] [Google Scholar]
- [32].Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Archer KR, Devin CJ, Vanston SW, et al. Cognitive-behavioral-based physical therapy for patients with chronic pain undergoing lumbar spine surgery: a randomized controlled trial. J Pain. 2016;17(1):76–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ardern CL, Peterson G, Ludvigsson ML, et al. Satisfaction with the outcome of physical therapist-prescribed exercise in chronic whiplash-associated disorders: secondary analysis of a randomized clinical trial. J Orthop Sports Phys Ther. 2016;46(8):640–649. [DOI] [PubMed] [Google Scholar]
- [35].Herr KA, Spratt K, Mobily PR, et al. Pain intensity assessment in older adults: use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin J Pain. 2004;20(4):207–219. [DOI] [PubMed] [Google Scholar]
- [36].Salaffi F, Stancati A, Silvestri CA, et al. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8(4):283–291. [DOI] [PubMed] [Google Scholar]
- [37].Farrar JT, Young JP Jr., LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. [DOI] [PubMed] [Google Scholar]
- [38].Van Wyngaarden JJ, Noehren B, Archer KR. Assessing psychosocial profile in the physical therapy setting. J Appl Biobehav Res. 2019. DOI: 10.1111/jabr.12165 [DOI] [Google Scholar]
- [39].Osman A, Barrios FX, Gutierrez PM, et al. The pain catastrophizing scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23(4):351–365. [DOI] [PubMed] [Google Scholar]
- [40].Scott W, Wideman TH, Sullivan MJ. Clinically meaningful scores on pain catastrophizing before and after multidisciplinary rehabilitation: a prospective study of individuals with subacute pain after whiplash injury. Clin J Pain. 2014;30(3):183–190. [DOI] [PubMed] [Google Scholar]
- [41].French DJ, France CR, Vigneau F, et al. Fear of movement/(re)injury in chronic pain: a psychometric assessment of the original English version of the Tampa scale for kinesiophobia (TSK). Pain. 2007;127(1–2):42–51. [DOI] [PubMed] [Google Scholar]
- [42].Woby SR, Roach NK, Urmston M, et al. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117(1–2):137–144. [DOI] [PubMed] [Google Scholar]
- [43].Walton DM, Levesque L, Payne M, et al. Clinical pressure pain threshold testing in neck pain: comparing protocols, responsiveness, and association with psychological variables. Phys Ther. 2014;94(6):827–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Chesterton LS, Sim J, Wright CC, et al. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain. 2007;23(9):760–766. [DOI] [PubMed] [Google Scholar]
- [45].Saban B, Masharawi Y. Pain threshold tests in patients with heel pain syndrome. Foot Ankle Int. 2016;37(7):730–736. [DOI] [PubMed] [Google Scholar]
- [46].Walton DM, Macdermid JC, Nielson W, et al. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41(9):644–650. [DOI] [PubMed] [Google Scholar]
- [47].Persson AL, Brogardh C, Sjolund BH. Tender or not tender: test-retest repeatability of pressure pain thresholds in the trapezius and deltoid muscles of healthy women. J Rehabil Med. 2004;36(1):17–27. [DOI] [PubMed] [Google Scholar]
- [48].Wei T, Simko V.. R package “corrplot”: visualization of a correlation matrix (version 0.84). 2017. [cited 2020 Jul 16]. Available from: https.//github.com/taiyn/corrplot
- [49].R Core Team . R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. ISBN 3-9000051-07-0. [cited 2020 Jul 16]. http://www.R-project.org/. [Google Scholar]
- [50].Geneen LJ, Martin DJ, Adams N, et al. Effects of education to facilitate knowledge about chronic pain for adults: a systematic review with meta-analysis. Syst Rev. 2015;4:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Louw A, Farrell K, Choffin B, et al. Immediate effect of pain neuroscience education for recent onset low back pain: an exploratory single arm trial. J Man Manip Ther. 2019;27(5):267–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].McClinton SM, Cleland JA, Flynn TW. Predictors of response to physical therapy intervention for plantar heel pain. Foot Ankle Int. 2015;36(4):408–416. [DOI] [PubMed] [Google Scholar]
- [53].Louw A, Puentedura EJ, Nijs J. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017. DOI: 10.1080/10669817.2017.1323699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Fraser JJ, Corbett R, Donner C, et al. Does manual therapy improve pain and function in patients with plantar fasciitis? A systematic review. J Man Manip Ther. 2018;26(2):55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Gay CW, Alappattu MJ, Coronado RA, et al. Effect of a single session of muscle-biased therapy on pain sensitivity: a systematic review and meta-analysis of randomized controlled trials. J Pain Res. 2013;6:7–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Voogt L, de Vries J, Meeus M, et al. Analgesic effects of manual therapy in patients with musculoskeletal pain: a systematic review. Manual Ther. 2015;20(2):250–256. [DOI] [PubMed] [Google Scholar]
- [57].Puentedura EJ, Flynn T. Combining manual therapy with pain neuroscience education in the treatment of chronic low back pain: A narrative review of the literature. Physiother Theory Pract. 2016;32(5):408–414. [DOI] [PubMed] [Google Scholar]


