ABSTRACT
Background
Patients with myofascial pain syndrome of the neck and upper back have active trigger points and may present with pain and decreased function. Dry needling (DN) and trigger point manual therapy (TMPT) techniques are often used to manage MPS.
Objective
To compare DN and TPMT for reducing pain on the Visual Analog Scale (VAS) and Pressure Pain Threshold (PPT) scores and improving function on the Neck Disability Index (NDI) in patients with neck and upper back MPS.
Methods
PubMed, PEDro, and CINAHL were searched for randomized controlled trials within the last 10 years comparing a group receiving DN and the other receiving TPMT. Studies were assessed using PEDro scale and Cochrane risk-of-bias tool to assess methodological quality. Meta-analyses were performed using random-effect model. Standardized mean differences (Cohen’s d) and confidence intervals were calculated to compare DN to TPMT for effects on VAS, PPT, and NDI.
Results
Six randomized controlled trials with 241 participants total were included in this systematic review. The effect size of difference between DN and TPMT was non-significant for VAS [d = 0.41 (−0.18, 0.99)], for PPT [d = 0.64 (−0.19, 1.47)], and for NDI [d = −0.66 (−1.33, 0.02)].
Conclusions
Both DN and TPMT improve pain and function in the short to medium term. Neither is more superior than the other.
KEYWORDS: Myofascial pain syndrome, dry needling, trigger point, manual therapy
Introduction
Myofascial pain syndrome is characterized by the presence of active myofascial trigger points, which are knots in skeletal muscle that are tender upon palpation[1]. Risk factors for the development of myofascial pain syndrome in the neck and shoulder include overuse and prolonged awkward postures [2,3]. Commonly affected muscles in patients with neck and shoulder myofascial pain syndrome include the upper trapezius, levator scapulae and infraspinatus [4,5]. Upon physical examination, patients with active myofascial trigger points may present with local pain, referred pain, reproduction of pain with compression on the muscle, and an elicited local twitch response with snapping palpation[1]. In addition to pain, patients with active myofascial trigger points may also have decreased range of motion, muscle weakness, muscle tightness, and an overall decrease in function [1,6]. A variety of interventions have been developed to address the above issues by relieving myofascial trigger points[1].
Trigger point manual therapy (TPMT) and dry needling (DN) are commonly used interventions for the management of myofascial trigger points and myofascial pain syndrome [7,8]. TPMT is the conservative first line of treatment and is proposed to work by reducing the overlap between actin and myosin by stretching the muscle[1]. Ischemic compression, pressure release, manual pressure, strain counter-strain, and trigger point compression are types of TPMT compression techniques that provide trigger point pain relief [9–11]. DN involves insertion of a fine needle without medication into the skin, subcutaneous tissues, and muscle to mechanically disrupt myofascial trigger points by eliciting local twitch responses[1]. The most common method of DN is called the ‘fast in, fast out’ technique[12]. This technique involves inserting a needle into the myofascial trigger point until the first local twitch response is produced; then the needle is moved up and down in a straight plane to get additional local twitch responses[12].
There are several systematic reviews and meta-analyses examining the effect of DN or ischemic compression for reducing pain and improving function for both neck and shoulder myofascial pain syndrome [6,13]. Some of these studies also investigate the effect of delivering these interventions across various time intervals [14,15]. Callejas-Marcos et al.[13], in their systematic review, concluded that DN reduces neck pain, but could not determine the effectiveness of DN compared to other interventions. Liu et al.[14], reported a decrease in pain in neck and shoulder myofascial pain syndrome after DN over the short term (immediately to 3 days) and medium term (nine-28 days). Ong and Claydon [15] found that DN decreased pain at three and 6 month follow ups. Cagnie et al.[6], found moderate evidence with ischemic compression and strong evidence with DN for pain reduction in patients with myofascial trigger points. However, there was weak evidence for the ability of either intervention to change function[6]. There are currently no systematic reviews and meta-analyses comparing the effectiveness of DN to TPMT techniques for reducing pain and improving function in patients with neck or shoulder myofascial pain syndrome. This systematic review compared the effectiveness of both DN and TPMT in reducing pain and improving function in patients with neck and shoulder MPS.
Methods
Study registration
This systematic review protocol was registered with PROSPERO 2019 (registration number: CRD42019124076) and is performed in line with the PRISMA declaration guidelines.
Data sources and searches
In June 2019, searches were performed in the electronic databases PubMed, PEDro, and CINAHL. The search strategy was based on combinations of MeSH terms and free-text terms detailed in Table 1. The exact searches performed for each database are detailed in Appendix S1. For PubMed and CINAHL filters were applied for clinical trials, English articles, human studies/adults (18+), and studies published within the last 10 years. For PEDro, filters were applied for English articles and studies published within the last 10 years.
Table 1.
Search terms
| ‘Myofascial pain’ OR ‘trigger point’ |
|---|
| AND |
| ‘Ischemic compression’ OR ‘manual therapy’ |
| AND |
| ‘Dry needling’ |
| AND |
| ‘Neck pain’ OR ‘shoulder pain’ OR ‘upper back pain’ OR ‘upper trapezius’ |
The population of interest was patients with myofascial pain or trigger points of the neck, shoulders, upper back, and upper trapezius in order to focus on a body region with commonly affected muscles.
Study selection
Randomized controlled trials within the last 10 years comparing DN to TPMT in adults with neck, shoulder, and/or upper back pain were eligible for inclusion.
Studies included in the review:
Chosen studies met the following criteria: TPMT that provided at least three repetitions of compression or compression for at least 60 seconds until resistance was felt and the patient experienced relief of the trigger point. TPMT techniques included pressure release, ischemic compression, strain counter-strain, manual pressure, and trigger point compression. DN involved performing between 30 seconds to 2 minutes of needle insertion into the trigger point until a local twitch response was produced.
Non-randomized controlled trials and animal studies were excluded. Also excluded were studies with patients that experienced macro trauma or post-operative pain in the neck, shoulder, and upper back to decrease the likelihood of confounding co-morbidities. Specific diagnoses that were excluded were fractures of the neck and upper back region, radiculopathy, neurological lesions, and degenerative diseases, such as osteoarthritis, degenerative joint disease, and degenerative disc disease. Articles that did not explicitly include groups receiving DN and TPMT for comparison were also excluded.
Two reviewers independently performed an initial screen of the titles and abstracts of the records found based on the inclusion and exclusion criteria. In the case of disagreement, a third reviewer screened the title and abstract of the study to reach a consensus. For the studies that met title/abstract screen, full text articles were attained and independently screened. Full text articles that were excluded are detailed in Appendix S2. In the case of disagreement, a third reviewer would have been used to resolve discrepancies regarding eligibility.
Quality assessment
Two independent, blinded reviewers used the PEDro scale, a valid and reliable measure of methodological quality, to assess the quality of the articles [16,17]. The PEDro scale consists of eleven items, 10 of which focus on external validity. Answers to each of the 10 items were ‘yes’ (one point) and ‘no’ (zero points), giving a possible maximum score of ten. Scores were compared item-by-item and disagreements were settled with a third blinded reviewer. Scores above nine, between six to eight, between four to five, and below four are considered to be excellent, good, fair, and poor quality, respectively [18,19].
Two independent reviewers used the Cochrane risk-of-bias tool to assess bias in selection, performance, detection, attrition, reporting, and other bias[20]. A third blinded reviewer settled disagreements.
Data extraction
The following items were systematically extracted from every study included in this systematic review: author, study demographics, DN and TPMT intervention and protocol, outcome parameters, namely, visual analog scale (VAS), numeric rating scale (NRS), pressure pain threshold (PPT), and neck disability index (NDI), and main results. Although the initial plan was to assess both short and long-term effects, there were insufficient studies examining long-term effects. Therefore, to maintain consistency between studies, data were only extracted in the short to medium term period of 1 week to 28 days with one to two sessions of treatment per week. The data were compared afterward to ensure that it was accurately extracted from each study.
Data synthesis and analysis
Meta-analyses were performed when outcome measure data on pain (VAS, NRS and PPT) and function (NDI) were available from a minimum of three clinical trials which reported similar outcome measures, similar data collection methods, and utilized similar timeframes for assessment of outcome measures, i.e. short to medium term. To produce the best possible synthesis, only studies with fair to high quality on the PEDro scale and low-risk scores on the Cochrane risk-of-bias tool were included in the meta-analyses. Data for the meta-analyses were analyzed by using Neyeloff Microsoft Excel spreadsheet. The random effect model was used to account for variability between studies. The effect size used to measure the standardized mean difference, i.e. Cohen’s d and confidence intervals were calculated for each study included in the analysis using the following formula:
d = (xexperimental post – xcontrol post)/SDpooled
where for the outcome measures of VAS, PPT, or NDI scores, xexperimental post is the post-treatment mean for the DN group, xcontrol post is the post-treatment mean for the TPMT group, and SDpooled is the square root of the average of the post-treatment standard deviations. 95% confidence intervals were calculated using the following formula:
95% CI = d ± 1.96 x SEd
where SEd = √[(nexperimental + ncontrol)/(nexperimental x ncontrol)] + [d2/2(nexperimental+ ncontrol)]. nexperimental is the number of subjects in the DN group, ncontrol is the number of subjects in the TPMT group, and d is the effect size. Effect sizes of 0.2, 0.5, or 0.8 are interpreted as small, medium, or large effects, respectively [21,22]. Statistical heterogeneity was quantified using the I2 test. A threshold of 50% was used to define high heterogeneity[23].
Results
Study selection
The search resulted in a total of 56 studies. After removal of duplicates, screening for the titles and abstracts, and screening the full-text articles, six relevant randomized controlled trials remained. An overview of the study selection is presented in Figure 1.
Figure 1.
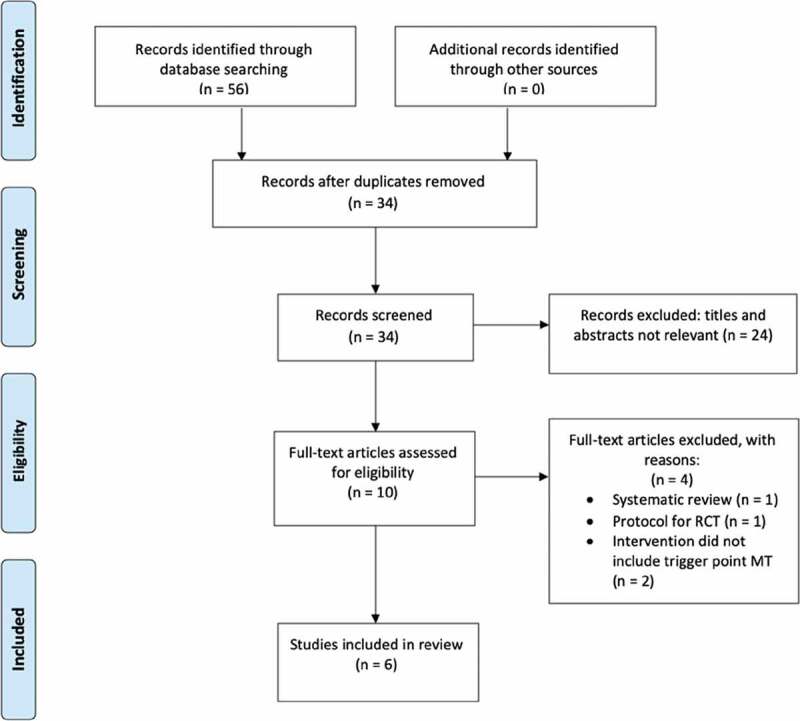
Flow chart of study selection
Assessment of methodological quality
Criteria assessment using the PEDro scale of the six studies included in this systematic review are presented in Table 2. Four of the articles included in this systematic review are of good quality and two of the articles are of fair quality [18,19]. A limitation of methodological quality of all the studies was the lack of clarity regarding blinding of the patients and the therapists. The mean PEDro score of the included studies was 6.17.
Table 2.
Methodological assessment of randomized controlled trials included in the systematic review using the PEDro scale and Cochrane risk-of-bias tool
| PEDro Criterion | Llamas-Ramos et al. 2014 | Sobhani et al. 2014 |
Campa-Moran et al. 2015 |
Segura-Orti et. al 2016 |
De Meulemeester et al. 2017 |
Ziaeifar et al. 2017 |
|---|---|---|---|---|---|---|
| Eligibility criteria specified | Y | N | Y | N | Y | Y |
| Random allocation | Y | Y | Y | Y | Y | Y |
| Concealed allocation | Y | N | N | Y | Y | N |
| Baseline comparability | Y | Y | Y | Y | Y | Y |
| Blinding of subjects | N | N | N | N | N | N |
| Blinding of therapists | N | N | N | N | N | N |
| Blinding of assessors | Y | Y | Y | Y | Y | N |
| Adequate follow-up | Y | N | Y | N | Y | N |
| Intention to treat | Y | N | Y | N | N | N |
| Between-group comparison | Y | Y | Y | Y | Y | Y |
| Point estimates and variability | Y | Y | Y | Y | Y | Y |
| Total Score | 8/10 | 5/10 | 7/10 | 6/10 | 7/10 | 4/10 |
| Cochrane risk-of-bias | Llamas-Ramos et al. 2014 |
Sobhani et al. 2014 |
Campa-Moran et al. 2015 |
Segura-Orti et. al 2016 |
De Meulemeester et al. 2017 |
Ziaeifar et al. 2017 |
| Selection bias Random sequence generation |
Low | Low | Low | Low | Low | Low |
| Selection bias Allocation concealment |
Low | Unclear | Unclear | Low | Low | High |
| Reporting bias Selective reporting |
Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Other bias Other sources of bias |
Low | Low | Low | Low | Low | Low |
| Performance bias Blinding (participants and personnel) |
Low | Unclear | Unclear | Low | Low | Unclear |
| Detection bias Blinding (outcome assessment) |
Low | Low | Low | Low | Low | High |
| Attrition bias Incomplete outcome data |
Low | Low | Low | Low | Low | Low |
| Overall RoB | Some concerns * | Some concerns* | Some concerns* | Some concerns* | Some concerns | High risk |
Y = Yes, N = No, RoB = risk of bias, *required a 3rd reviewer
Risk-of-bias (RoB) using the Cochrane risk-of-bias tool of the six studies are also presented in Table 2. Based on the assessment, there are some concerns regarding performance bias due to the lack of clarity about blinding of participants/personnel in the studies and selective reporting of positive changes postDN and TPMT treatment.
Study characteristics
Table 3 reports study demographics, intervention protocol, outcome measures, follow-up time points, and results of all individual studies included in this review. All six studies evaluated the effects of DN to different TPMT techniques, which included pressure release, ischemic compression, strain counter-strain, manual pressure, and trigger point compression [24–29]. All six studies performed DN until a local twitch response was produced [24–29]. The studies by Sobhani et al.[27], Campa-Moran et al.[28], and Segura-Orti et al.[29], included shoulder ROM exercises and passive stretching after needling. Both DN and TPMT interventions in all studies were done on the upper trapezius muscle, with Campa-Moran et al. [28] and Segura-Orti et al. [29] additionally performing the intervention on the levator scapulae muscle. Follow-up periods across all six studies assessed the effects of DN and TPMT on pain (NRS, VAS, and PPT) and function (NDI) in the short to medium term [24–29].
Table 3.
Characteristics of the studies included in this review
| Study | Number of participants DN/TPMT |
DN M/F TPMT M/F |
DN mean age (SD) TPMT mean age (SD) |
Intervention frequency | DN protocol | Performed after DN | TPMT type + protocol | Time point + Outcome measures |
Results |
|---|---|---|---|---|---|---|---|---|---|
| Llamas-Ramos et al. 2014 | 47/47 | 17/30 15/32 |
31 (3) 31 (2) |
1x/wk for 2 wks | UT Duration: until LTR then 25–30 s |
None | Pressure release 3 reps Stretching of taut band: 1 rep Passive stretching of UT Duration: 45 s |
Baseline and after 2 wk: NRS PPT |
NRS: ↓ in DN and TPMT groups* PPT: DN group >↑ in than TPMT group |
|
Sobhani et al. 2014 |
13/13 | Not reported | 34.6 (10.5) 35.9 (11.4) |
5x/10 days | UT and LS Duration: 20 min |
Passive stretching bilaterally to UT and LS | IC on UT and LS Duration: 4 min AP mob of the upper c/s Duration: 4 min C/s lateral glide mob, and neural t/s mob |
Baseline and after 10 days: VAS NDI |
VAS: ↓ for DN and TPMT groups* NDI: ↓ for DN and TPMT groups* |
|
Campa-Moran et al. 2015 |
12/12 | 3/9 2/10 |
53.9 (12.7) 45.8 (15.4) |
2 treatment sessions w/48 hrs between each session | UT and LS: Duration: until LTR; ~2 min/myofascial trigger point |
Passive stretching to UT and LS Duration: 20 s |
IC on UT and LT Duration: 90 s DSTM on UT: Duration: 2 min |
Baseline and after 2 sessions: NDI PPT VAS |
VAS: ↓ in DN and IC groups* PPT: ↑ in DN and IC groups* NDI: ↓statistically significant decrease for DN group |
|
Segura-Orti et al. 2016 |
12/10 | 4/8 3/7 |
30.0 (9.5) 34.1 (11.5) |
DN: 1x/wk for 3 wks SCS: 2x/wk |
UT Duration: until LTR |
Active shoulder abduction and shoulder shrugging for 8 reps Passive UT stretch |
SCS on UT Duration: 90 s |
Baseline and after 3 wk: VAS PPT NDI |
VAS: ↓ in DN and SCS groups* PPT: ↑ in DN and SCS groups NDI: ↓ in DN and SCS groups* |
|
De Meulemeester et al. 2017 |
20/22 | 0/20 0/22 |
36.1 (10.7) 40.5 (8.3) |
1x/wk for 4 wks | 4 most painful myofascial trigger points Duration: until LTR |
None | MP on 4 most painful myofascial trigger points Duration: 60 s |
Baseline, after 1 wk, and after 4 wk: PPT Baseline and after 4 wk: NDI |
NRS: ↓ in DN and MP groups* PPT: ↑ in DN and MP groups* NDI: ↓ in DN and MP groups* |
|
Ziaeifar et al. 2017 |
17/16 | Not reported | 30.06 (9.87) 26.5 (8.57) |
3x/wk for 1 wk | UT Duration: until LTR |
None | TrPC on UT. Duration: 90 s |
Baseline and after 1 wk: VAS PPT |
VAS: ↓ in both DN and TPMT groups, significant between group differences PPT: ↑ in both DN and TPMT groups* |
M = male, F = female, DN = dry needling, LTR = local twitch response, TPMT = manual therapy, IC = ischemic compression, SCS = strain counter-strain, MP = manual pressure, TrPC = trigger point compression, DSTM = dynamic soft tissue mobilization, UT = upper trapezius, LS = levator scapulae, VAS = visual analog scale, NRS = numeric rating scale, PPT = pressure pain threshold, NDI = neck disability index, wk = week, hrs = hours, min = minutes, s = seconds, reps = repetitions, * = no significant differences between groups
Individual studies
Table 3 describes the results of all the individual studies. All studies demonstrated a decrease in NRS, VAS, and NDI scores and an increase in PPT in both DN and TPMT groups from baseline to the corresponding follow-up time, which ranged from 1 week to 28 days across studies. Decrease in NRS and VAS scores represented a reduction in myofascial trigger point pain, decrease in NDI scores represented a reduction in self-rated disability, and an increase in PPT represented a reduction in tenderness, which allowed for increased pressure (force) to be tolerated before pain was perceived [30–32].
The effects on NRS, VAS, NDI, and PPT from the majority of the studies were due to significant time effects rather than significant time by group interactions. Additionally, there were no significant differences between DN and TPMT groups for a majority of the outcome measures evaluated across the studies. Three different outcome measures demonstrated a significant difference between DN and TPMT treatment groups [25,26]. Llamas-Ramos et al. [26] demonstrated a significant between-group difference for an increase in PPT favoring the DN group after 2 weeks of treatment. Campa-Moran et al. [28] demonstrated significant between-group differences for a decrease in NDI scores favoring the DN group after two treatment sessions (p = 0.032). Lastly, Ziaeifar et al. [25] demonstrated that there were significant between-group differences (p = 0.01) in VAS scores after 1 week of treatment.
Meta-analysis: dry needling compared to manual therapy: VAS
Three studies compared DN to TPMT for effects on VAS scores shown in Figure 2(a). The meta-analysis revealed no statistically significant differences between the groups (d = 0.41, 95%CI: −0.18 to 0.99, I2 = 34.8%) [27–29].
Figure 2.
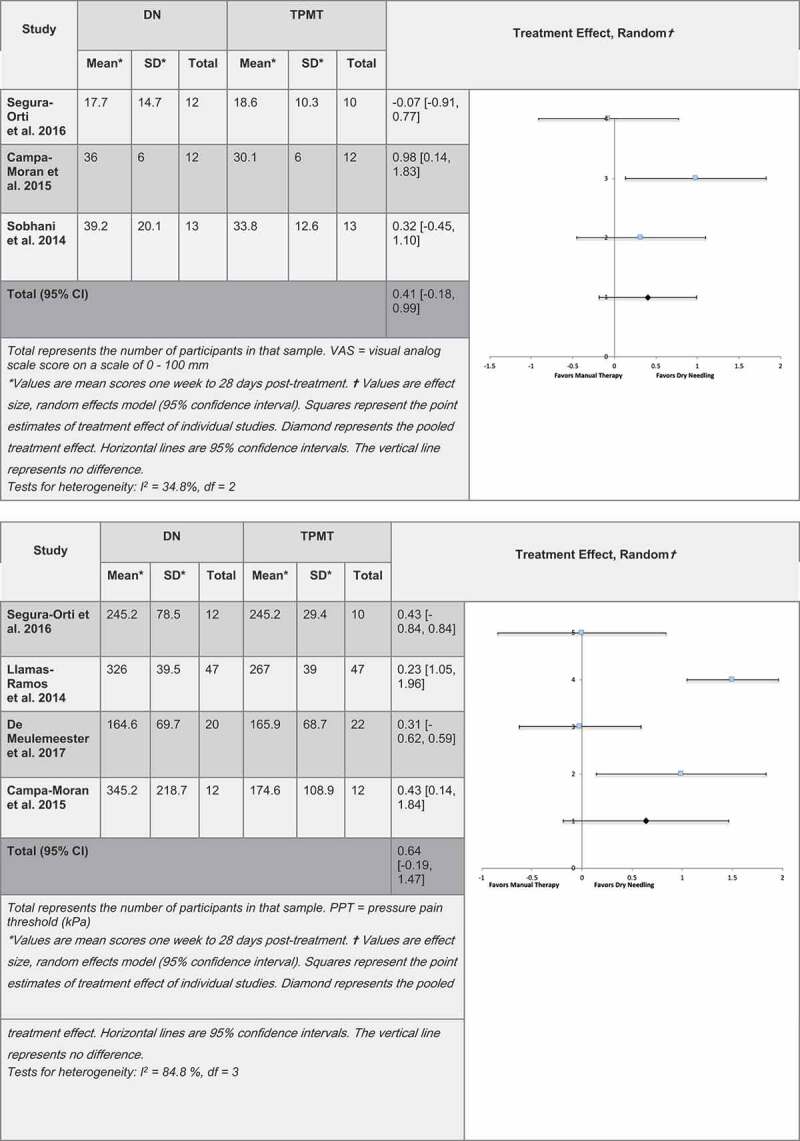
(a). Forest plot for dry needling compared to manual therapy for effects on VAS. (b). Forest plot for dry needling compared to manual therapy for effects on PPT
Meta-analysis: dry needling compared to manual therapy: PPT
Four studies compared DN to TPMT for effects on PPT, as shown in Figure 2(b). The meta-analysis revealed no statistically significant differences between the two groups (d = 0.64, 95% CI: −0.19 to 1.47, I2 = 84.8%) [24,26,28,29].
Figure 2.
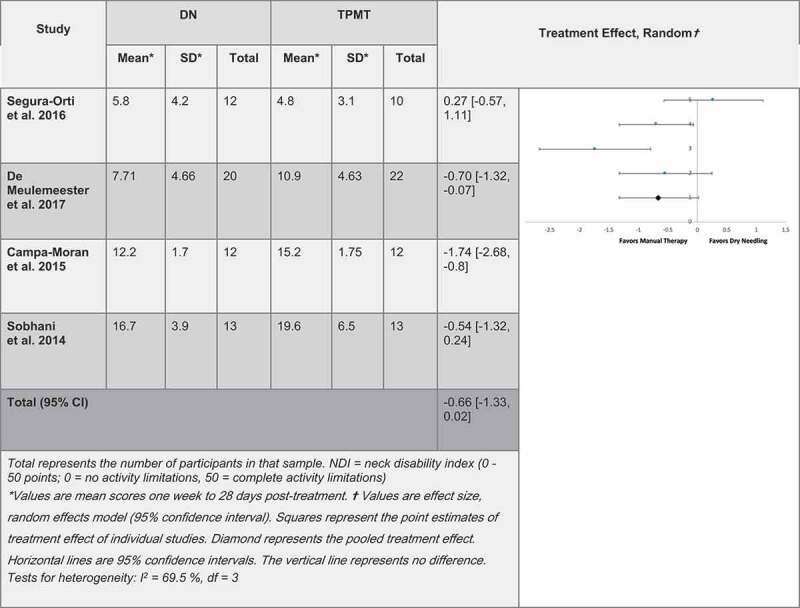
(c). Forest plot for dry needling compared to manual therapy for effects on NDI
Meta-analysis: dry needling compared to manual therapy: NDI
Four studies compared DN to TPMT for effects on NDI, as shown in Figure 2(c). The meta-analysis revealed no statistically significant differences between the two groups (d = −0.66, 95% CI: −1.33 to 0.02, I2 = 69.5%) [24,27–29].
Meta-analysis: dry needling compared to manual therapy: NRS
A meta-analysis comparing DN to TPMT for its effects on NRS was not performed due to limited data.
Discussion
The goal of this systematic review was to compare the efficacy of DN to TPMT on reducing myofascial trigger points in patients with myofascial pain syndrome of the upper back. Pain (VAS and NRS), PPT, and function (NDI) were used as outcome parameters to evaluate and compare the effectiveness of the two interventions. Although at initial registration the aim was to assess both short and long-term effects of the interventions, evidence for long-term effects were insufficient leading to the deviation from protocol and synthesis of only short and medium-term effects. A decision was made a priori to focus on trigger points in the neck and shoulder region because the diagnostic process was consistent across studies. This improved the homogeneity of included participants and allowed for a more consistent picture of the effectiveness of interventions. Studies published over the past 10 years were utilized in this review so as to only account for the most recent information in the field, which could be a strength or a limitation of the study. DN compared to TPMT was selected because prior systematic reviews had found that each of the interventions were more effective than a sham/control for the patient population of interest, but research had not been done comparing one to the other. NRS, VAS, PPT, and NDI were chosen as the relevant outcome measures to understand how the interventions affected pain and function.
None of the included studies detailed the potential adverse events of the use of either intervention. Research should be done to evaluate any adverse effects between DN and TPMT in order to effectively weigh out the benefits versus risks with the use of these interventions to treat chronic myofascial pain syndrome. Participants may have been put through unnecessary pain and stress due to a lack of clarity regarding appropriate vigor of intervention protocols.
There are some threats to internal validity of the studies included in this systematic review that should be considered when drawing conclusions. Of the studies included in the systematic review, four lacked clarity regarding blinding of participants and assessors, which increased the studies’ risk-of-bias [26–29]. Another challenge to internal validity was the use of samples of convenience, increasing the likelihood that the study population may not have been representative of the population. The results were also likely affected by maturation since none of the studies compared either intervention to time alone. This meant that the effect of time itself was not accounted for in causing a significant change in the outcome measures.
The conclusions from the study were also limited by differences in dosage of DN and TPMT, such as intervention frequency, adjunct interventions performed after DN and TPMT, number of repetitions of TPMT, and vigor of TPMT treatment. Intervention frequencies ranged from two treatment sessions total to once a week for 4 weeks [24,28]. There was no research that provided evidence regarding optimal treatment frequencies of the two interventions. In order to decrease heterogeneity, a meta-analysis was performed examining the effectiveness of the interventions in the short to medium term, since only two studies had data for medium or long term follow ups. Thus, the findings of the meta-analyses may not indicate the effectiveness of either intervention for longer time frames and may have missed significant differences that are only evident after time.
While it is unknown as to why passive stretching was included as an adjunct to DN in three of the six studies rather than as part of the TPMT protocol, the assumption was that this decision may be related to the hypothesized mechanism of efficacy that Simons and Travel [1] described regarding reducing the overlap of actin and myosin filaments of the muscles with myofascial trigger points [27–29]. Segura-Orti et al. [29] included shoulder AROM exercises[29]. Therefore, it is possible that the passive stretching and AROM exercises could have contributed to the overall treatment effect. The majority of studies maintained TPMT compression for one repetition, but one study performed it for three repetitions[26]. Llamas-Ramos et al. [26] performed the intervention shy of pain, two studies performed the intervention until the onset of pain [24,28], and the vigor of TPMT of the remaining three studies are unknown [25,27,29].
Strengths of internal validity included the consistency of randomization of participants into the different groups and the standardization of duration of both DN and TPMT protocols. Based on the current but limited research, both DN and TPMT had similar positive effects on pain and function in the short to medium term, giving clinicians more tools to address chronic myofascial pain syndromes. These findings may also help resolve disputes between clinicians who strongly favor one intervention over the other.
Suggestions for future research should evaluate the effects of DN and TPMT against sham interventions on improving pain and function in different body regions. Further clarification of optimal dosages of DN and TPMT are needed in order to facilitate a better interpretation of results across multiple studies. Higher quality randomized controlled trials are also needed in order to produce more conclusive evidence of the effects of both interventions. Lastly, the generalizability of this systematic review is limited by the specificity of diagnosis and the body region included in this study. This systematic review does not give insight into the effectiveness of DN versus TPMT in other body regions or for other diagnoses. Since macro trauma and post-operative pain was excluded, the effectiveness of either intervention to decrease acute pain following trauma is unknown.
Conclusions
This study was consistent with existing research that demonstrated the effectiveness of DN and TPMT in improving pain and function in the short to medium term for patients with myofascial pain syndrome in the neck and upper back. Neither intervention appeared to be superior than the other. The effectiveness of both interventions allows clinicians and patients to have more choices in their treatment plan.
Supplementary Material
Acknowledgments
Michela Biale, DPT, Ada Kan, DPT, Joanna Lee, DPT, Jenny Li, DPT, Darby Nordin, DPT.
Biographies
Jennalyn Lew earned her Bachelor of Science in Molecular, Cell, and Developmental Biology from the University of California, Santa Cruz. She received her Doctor of Physical Therapy degree at Samuel Merritt University and will go on to pursue her interests in orthopedic rehabilitation and manual therapy.
Jennifer Kim received a bachelor’s degree in Integrative Biology from University of California, Berkeley and received her Doctor of Physical Therapy degree at Samuel Merritt University.
Preeti Nair earned her Bachelor of Physiotherapy at Pune University in India. She then earned a PhD in Rehabilitation Sciences at the University of Florida, with a research focus on Biomechanics and Neurophysiology of walking in individuals with neurological impairment. She is currently an Associate Professor in the Department of Physical Therapy at Samuel Merritt University.
Supplemental Material
Supplemental data for this article can be accessed here.
Disclosure statement
The authors report no conflict of interest.
Financial disclosure
We affirm that we have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript.
Key points
Findings: Both DN and TPMT improves pain and function for individuals with neck and/or upper back myofascial pain syndrome in the short to medium term. Neither is more effective than the other.
Implications: Clinicians and patients have the ability to choose between DN or TPMT for treatment of neck and/or upper back myofascial pain syndrome for reducing pain and improving function in the short to medium term.
Caution: The findings of this systematic review cannot be generalized to individuals with myofascial pain syndrome of other regions nor does it assess whether pain and function can be improved in the long term.
References
- [1].Simons DG, Travell JG, Simons LS.. Travell & Simons’ myofascial pain and dysfunction: the trigger point manual. 2nd ed. Baltimore: Williams & Wilkins; 1999. [Google Scholar]
- [2].Duyur CB, Altuntas V, Genc H, et al. Disability and related factors in patients with chronic cervical myofascial pain. Clin Rheumatol. 2009;28(6):647–654. [DOI] [PubMed] [Google Scholar]
- [3].van der Windt DA, Thomas E, Pope DP, et al. Occupational risk factors for shoulder pain: a systematic review. Occup Environ Med. 2000;57(7):433–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bron C, Dommerholt J, Stegenga B, et al. High prevalence of shoulder girdle muscles with myofascial trigger points in patients with shoulder pain. BMC Musculoskelet Disord. 2011;12(139). DOI: 10.1186/1471-2474-12-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Cerezo-Tellez E, Torres-Lacomba M, Mayoral-Del Moral O, et al. Prevalence of myofascial pain syndrome in chronic non-specific neck pain: A population-based cross-sectional descriptive study. Pain Med. 2016;17(12):2369–2377. [DOI] [PubMed] [Google Scholar]
- [6].Cagnie B, Castelein B, Pollie F, et al. Evidence for the use of ischemic compression and dry needling in the management of trigger points of the upper trapezius in patients with neck pain: a systematic review. Am J Phys Med Rehabil. 2015;94(7):573–583. [DOI] [PubMed] [Google Scholar]
- [7].Tough EA, White AR, Cummings TM, et al. Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomised controlled trials. Eur J Pain. 2009;13(1):3–10. [DOI] [PubMed] [Google Scholar]
- [8].Cummings M, Baldry P. Regional myofascial pain: diagnosis and management. Best Pract Res Clin Rheumatol. 2007;21(2):367–387. [DOI] [PubMed] [Google Scholar]
- [9].Travell JG, Simons DG. Myofascial pain and dysfunction: the trigger point manual. Baltimore: Williams & Wilkins; 1983. [Google Scholar]
- [10].Lewit K. Manipulative therapy in rehabilitation of the locomotor system. 3rd ed. Oxford: Butterworth Heinemann; 1999. [Google Scholar]
- [11].Jones L. Strain and counterstrain. Indianapolis: American Academy of Osteopathy; 1981. [Google Scholar]
- [12].Hong C. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil. 1994;73(4):256–263. [DOI] [PubMed] [Google Scholar]
- [13].Callejas-Marcos I, Torrijos-Bravo A, Torres-Chica B, et al. Efficacy of dry needling in neck pain compared with other physiotherapy techniques: A systematic review. Rehabilitacion (Madr). 2019;53(3):189–197. [DOI] [PubMed] [Google Scholar]
- [14].Liu L, Huang QM, Liu QG, et al. Effectiveness of dry needling for myofascial trigger points associated with neck and shoulder pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;96(5):944–955. [DOI] [PubMed] [Google Scholar]
- [15].Ong J, Claydon LS. The effect of dry needling for myofascial trigger points in the neck and shoulders: a systematic review and meta-analysis. J Bodyw Mov Ther. 2014;18(3):390–398. [DOI] [PubMed] [Google Scholar]
- [16].de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–133. [DOI] [PubMed] [Google Scholar]
- [17].Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- [18].Maher CG. A systematic review of workplace interventions to prevent low back pain. Aust J Physiother. 2000;46(4):259–269. [DOI] [PubMed] [Google Scholar]
- [19].Foley NC, Teasell RW, Bhogal SK, et al. Stroke rehabilitation evidence-based review: methodology. Top Stroke Rehabil. 2003;10(1):1–7. [PubMed] [Google Scholar]
- [20].Higgins JP, Altman DG, Gotzche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928-d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Neyeloff JL, Fuchs SC, Moreira LB. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes. 2012;5(52). DOI: 10.1186/1756-0500-5-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ. 2012;4(3):279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- [24].De Meulemeester KE, Castelein B, Coppieters I, et al. Comparing trigger point dry needling and manual pressure technique for the management of myofascial neck/shoulder pain: a randomized clinical trial. J Manipulative Physiol Ther. 2017;40(1):11–20. [DOI] [PubMed] [Google Scholar]
- [25].Ziaeifar M, Arab AM, Karimi N, et al. The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J Bodyw Mov Ther. 2014;18(2):298–305. [DOI] [PubMed] [Google Scholar]
- [26].Llamas-Ramos R, Pecos-Martin D, Gallego-Izquierdo T, et al. Comparison of the short-term outcomes between trigger point dry needling and trigger point manual therapy for the management of chronic mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44(11):852–861. [DOI] [PubMed] [Google Scholar]
- [27].Sobhani V, Shamsoddini A, Khatibi-Aghda A, et al. Effectiveness of dry needling, manual therapy, and Kinesio Taping® for patients with chronic myofascial neck pain: a single-blind clinical trial. Trauma Mon. 2017;22(6). DOI: 10.5812/traumamon.39261 [DOI] [Google Scholar]
- [28].Campa-Moran I, Rey-Gudin E, Fernandez-Carnero J, et al. Comparison of dry needling versus orthopedic manual therapy in patients with myofascial chronic neck pain: a single-blind, randomized pilot study. Pain Res Treat. 2015;327307. DOI: 10.1155/2015/327307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Segura-Orti E, Prades-Vergara S, Manzaneda-Pina L, et al. Trigger point dry needling versus strain-counterstrain technique for upper trapezius myofascial trigger points: a randomised controlled trial. Acupunct Med. 2016;34(3):171–177. [DOI] [PubMed] [Google Scholar]
- [30].Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–1093. [DOI] [PubMed] [Google Scholar]
- [31].Young IA, Dunning J, Butts R, et al. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother Theory Pract. 2019;35(12):1328–1335. [DOI] [PubMed] [Google Scholar]
- [32].Maquet D, Croisier JL, Demoulin C, et al. Pressure pain thresholds of tender point sites in patients with fibromyalgia and in healthy controls. Eur J Pain. 2004;8(2):111–117. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


