Abstract
Background
Takotsubo cardiomyopathy (TCM) can clinically present as an acute coronary syndrome; however, the former has regional wall motion abnormalities that extend beyond a single coronary vascular territory without any plaque rupture. Takotsubo cardiomyopathy classically involves apical ballooning of left ventricle (LV). It is uncommon for TCM to present as cardiopulmonary arrest (CPA) along with third-degree atrioventricular (AV) block.
Case summary
A 63-year-old female, underwent a ventricular fibrillation (VF) CPA. She was defibrillated three times and return of spontaneous circulation (ROSC) was achieved after 37 min. Her post-ROSC electrocardiogram showed non-specific ST-segment changes and T-wave inversions and soon progressed to third-degree AV block. Patient had a transvenous pacemaker placed to pace her heart. Echocardiogram showed an LV ejection fraction of 15–20% with akinesis of the apex and anteroseptum. An echocardiogram repeated 4 days after the cardiopulmonary arrests showed an ejection fraction of 60–65% with hypokinesis of mid anterior and antero-apical hypokinesis. However, the patient still continued to require a pacemaker and hence eventually received a dual-chamber pacemaker/implantable cardioverter-defibrillator for her AV block and ventricular arrhythmia.
Discussion
Most commonly TCM presents with chest pain and symptoms of acute myocardial infarction. We present a very rare presentation of TCM associated with VF and CPA along with third-degree AV block. There have handful of case reports documenting TCM causing CPA in some patients and other case reports showing TCM causing high degree AV block. In our patient, TCM was associated with both VF and CPA along with third-degree AV block.
Keywords: Takotsubo cardiomyopathy, Stress-induced cardiomyopathy, Case report, Cardiac arrest, Ventricular fibrillation, Atrioventricular block
For the podcast associated with this article, please visit https://academic.oup.com/ehjcr/pages/podcast
Learning points
It is very rare for stress induced cardiomyopathy to cause ventricular fibrillation cardiac arrest.
In addition, stress induced cardiomyopathy can lead to a complete heart block, which can persist even when patients takotsubo cardiomyopathy improves.
Introduction
Takotsubo cardiomyopathy (TCM) also known as stress-induced cardiomyopathy, or broken heart syndrome, is characterized by transient systolic dysfunction of the apical and/or mid-segments of the heart.1–3 It is typically caused by psychological stress likely due to a catecholamine surge.4 Takotsubo cardiomyopathy obtains its name from a Japanese word for ‘fishing pot for trapping octopus’, which resembles the appearance of the left ventricle (LV).1,4 On a pathological study, TCM has focal myocytolysis, diffuse subendocardial haemorrhages with inflammatory infiltrates contraction band formations and myocardial necrosis.1,3 Experiments performed in rats have shown the development of subendocardial haemorrhages and myocardial necrosis in response to emotional and physical stress.3 Takotsubo cardiomyopathy is unique since apical wall of LV is affected, and its base is spared.1 The apex of the LV has restricted coronary perfusion and is more sensitive to adenylate stimulation due to increased receptor density.1
The definitive aetiology of TCM is not clear, but usually emotional or physical stress precedes TCM.4 There is some association between TCM and mental illness, beta-2-adrenergic agonist use for chronic obstructive pulmonary disease, tobacco, and marijuana use.3 TCM classically involves apical ballooning of LV; however, its less common variants involves mid, or basal segments of LV.5 Takotsubo cardiomyopathy is usually considered to have a relatively good prognosis and rarely causes sudden death, congestive heart failure, or fatal arrhythmias.4 Takotsubo cardiomyopathy can clinically present similar to acute coronary syndrome; however, the former has regional wall motion abnormalities that extend beyond a single coronary vascular territory without any plaque rupture.5,6 In most cases, LV ejection fraction recovers within several days.6 However, residual myocardial scar can lead to arrhythmia.3 It is very uncommon for TCM to present as cardiopulmonary arrest along with third-degree atrioventricular (AV) block.
Timeline
| Day 0 0559 | Patient brought to Emergency Department via Emergency Medical Service with cardiopulmonary arrest |
| Day 0 0851 | Underwent emergent left and right heart catheterization |
| Day 0 0915 | Temporary venous pacemaker placed |
| Day 0 1810 | Echocardiogram performed—left ventricular ejection fraction of 15–20% |
| Day 4 1000 | Patient extubated to 4 L nasal cannula |
| Day 4 2005 | Repeat echocardiogram performed—left ventricular ejection fraction of 60–65%. |
| Day 7 1759 | Dual-chamber implantable cardio defibrillator implanted |
| Day 11 1620 | Patient discharged to sub-acute rehab facility |
Case presentation
We present the case of a 63-year-old female, with a past medical history of hypertension, diabetes, diverticulitis, and chronic low back pain. She did not have any significant cardiac history. She has had a hysterectomy, and multiple orthopaedic surgeries in the past. She takes lisinopril, trazodone, amlodipine, metformin, sertraline, cyclobenzaprine, and morphine at home. She is an active half a pack a day cigarette smoker, but no alcohol or illicit drug use.
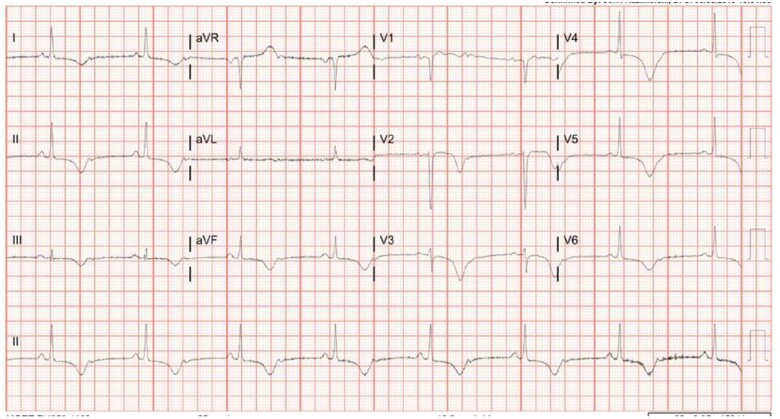
She was found unresponsive at home and did not have a pulse and cardiopulmonary resuscitation was started. Emergency medical services arrived at the scene and she was found to have ventricular fibrillation (VF) on the monitor. She was defibrillated three times and received multiple rounds of epinephrine and sodium bicarbonate. Her total time from cardiopulmonary arrest (CPA) to return of spontaneous circulation (ROSC) was 37 min. After ROSC was achieved, electrocardiogram (ECG) showed non-specific ST-segment changes and T-wave inversions and soon progressed into high grade and third-degree AV block (Figures 1 and 2). Initial troponin I was negative. A bedside echocardiogram was performed by a cardiologist, showing an ejection fraction of 25% with akinesis of the apex and anteroseptum.
Figure 1.
Electrocardiogram showing diffuse T-wave inversions.
Figure 2.
Electrocardiogram showing third-degree atrioventricular block.
On presentation, the patient had a troponin I level of <0.015 ng/mL, lactic acidaemia of 10 mmol/L, potassium of 2.5 mmol/L, elevated creatinine of 1.4 mg/dL. Computed tomography angiogram of the chest was done to rule out pulmonary embolism or aortic dissection as the cause of the CPA, which was negative for any acute process; however, it did show calcification of left anterior descending and left circumflex arteries. She was taken for a right and left heart catheterization the same day which did not show any significant coronary occlusion (Figure 3, Videos 1 and 2). Left ventriculogram showed ballooning of the left ventricle (Figure 4, Video 3).
Figure 3.
Coronary angiogram.
Figure 4.
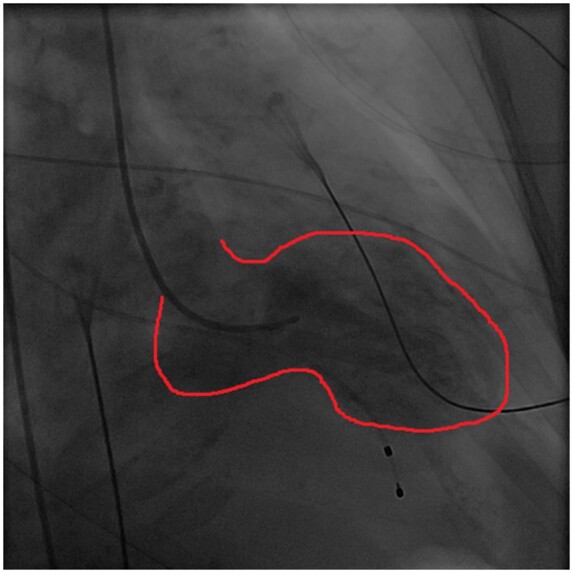
Left ventriculogram, portraying hypokinesis (outlined with red).
A formal transthoracic echocardiogram performed hours after presentation showed an ejection fraction of 15–20% and severe hypokinesis of anterior, apical, anteroseptal, and lateral wall of the heart, resembling TCM (Supplementary material online, Video S1). An echocardiogram repeated 4 days after the cardiopulmonary arrests showed an ejection fraction of 60–65% with hypokinesis of mid anterior and antero-apical hypokinesis and absence of any other wall motion abnormalities compared to the previous echocardiogram.
The patient had a pulmonary artery catheter and transvenous pacemaker placed for closer monitoring of cardiac haemodynamic state and to pace her heart, respectively. The pulmonary artery catheterization revealed right atrial pressure of 11 mmHg, right ventricular systolic pressure of 39 mmHg, pulmonary artery pressure of 46/22 with a mean of 31 mmHg, pulmonary capillary wedge mean pressure of 20 mmHg, cardiac output of 5.27 L/min, and cardiac index of 2.9 L/min/m2. The patient was pacemaker dependent during her hospitalization, despite of improvement in her TCM per repeat echocardiogram. Hence, she eventually received a dual-chamber pacemaker/implantable cardioverter-defibrillator for her AV block and as primary prevention for her ventricular arrhythmia. The patient was intubated during CPA. She had a thorough neurological examination off sedation, and she was following commands and moving all extremities. She was eventually extubated and had a good neurological recovery. Subsequently, she was discharged home without any significant neurological deficits. In addition to her previous home medications, she was started on carvedilol, aspirin, and atorvastatin upon discharge. The patient followed up in an outpatient setting and continued to have a stable ejection fraction of 60–65%; in addition, she was pacemaker dependent without any ventricular arrhythmia events.
Discussion
Takotsubo cardiomyopathy has been associated with an increase in plasma catecholamines, like epinephrine, norepinephrine, and dopamine.7,8 As per the Mayo criteria for cardiomyopathy all four of the following criteria should be present. Criterion 1: Transient hypokinesis, akinesis, or dyskinesis of left ventricular segments and may or may not involve apical wall. Criterion 2: Lack of obstructive coronary disease or acute plaque rupture on angiogram. Criterion 3: New ECG changes either ST-segment elevation and/or T-wave inversions. Criterion 4: Absence of myocarditis or pheochromocytoma.7 Our patient met the Mayo diagnostic criteria for TCM. She had transient akinesis of left ventricular segments, non-specific ST changes, and T-wave inversion, no significant coronary artery disease, and no signs or symptoms suggestive of either myocarditis or pheochromocytoma.
Hospital mortality from TCM varies between 1.1 and 2.5%, with sudden cardiac death being a major cause.5,9 In a study by Zalewska-Adamiec et al.,10 they observed that 89% of TCM patients were women. Takotsubo cardiomyopathy patients have a statistically significant lower likelihood of having diabetes, hyperlipidaemia, renal disorders, compared to patients with acute coronary syndromes.10 Conversely, TCM patients have a statistically increased likelihood of having chronic obstructive pulmonary disease and thyroid disturbances.10 Another study by Cacciotti et al. found hypothyroidism in 29.3% of TCM patients.10 In a case series of 101 patients, ST-elevation was present in 55% of the patients with TCM and T-wave inversion in about 33% of the patients.10 Moreover, 44% of TCM patients had no atherosclerotic disease, while the remaining 56% of patients had insignificant disease.10 However, arrhythmias including atrial fibrillation, AV block, and asystole are very rare.11
Most commonly TCM presents with chest pain and symptoms of acute myocardial infarction. We present a very rare presentation of TCM associated with VF and CPA along with third-degree AV block. There have been handful of case reports documenting TCM causing CPA in some patients and other case reports showing TCM causing high degree AV block. In this case presentation, we present an extremely rare case of TCM with associated VF and CPA followed by third-degree AV block, in a patient without any significant cardiac history.
Lead author biography

Dr Akarsh Parekh is a native of Columbus, Ohio. He attended The Ohio State University for his undergraduate college and St. George's University School of Medicine for his medical school. He is an American Board of Internal Medicine certified physician who is currently undergoing training at a Michigan State University affiliated cardiology fellowship program.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing these cases and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidelines.
Conflict of interest: None declared.
Funding: None declared.
Supplementary Material
References
- 1. Harika R, Bermas K, Hughes C, Al-Khafaji A, Iyer M, Wallace DJ.. Cardiac arrest after liver transplantation in a patient with takotsubo cardiomyopathy. Br J Anaesth 2014;112:594–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sosnowska-Pasiarska B, Bąkowski D, Woronowicz-Chróściel A, Wożakowska-Kapłon B.. Sudden cardiac arrest in takotsubo cardiomyopathy – a case study. Adv Intervent Cardiol 2014;10:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Del Buono MG, O'Quinn MP, Garcia P, Gerszten E, Roberts C, Moeller FG. et al. Cardiac arrest due to ventricular fibrillation in a 23-year-old woman with broken heart syndrome. Cardiovasc Pathol 2017;30:78–81. [DOI] [PubMed] [Google Scholar]
- 4. Kim SR, Nakashima K, Nishiuchi S, Imoto S, Nakajima T, Ando K. et al. A case of takotsubo cardiomyopathy with ventricular fibrillation after gastroenterological endoscopy. Clin J Gastroenterol 2011;4:73–78. [DOI] [PubMed] [Google Scholar]
- 5. Singh K, Parsaik AK, Zeitz CJ.. Takotsubo cardiomyopathy mid ventricle variant and cardiac arrest: chicken or the egg? Am J Emerg Med 2013;31:890–8e1. [DOI] [PubMed] [Google Scholar]
- 6. Jesel L, Berthon C, Messas N, Lim HS, Girardey M, Marzak H. et al. Ventricular arrhythmias and sudden cardiac arrest in Takotsubo cardiomyopathy: incidence, predictive factors, and clinical implications. Heart Rhythm 2018;15:1171–1178. [DOI] [PubMed] [Google Scholar]
- 7. Facciorusso A, Amico C, Vigna C, Santoro T, Potenza D, Massaro R. et al. Cardiac arrest caused by Barlow's syndrome or by stress cardiomyopathy? Int J Cardiol 2010;140:e16–e18. [DOI] [PubMed] [Google Scholar]
- 8. Yaghoubi AR, Ansarin K, Hashemzadeh S, Azhough R, Faraji S, Bozorgi F.. Takotsubo cardiomyopathy induced by emotional stress leading to severe mitral regurgitation, cardiogenic shock and cardiopulmonary arrest. Int J Cardiol 2009;135:e85–e86. [DOI] [PubMed] [Google Scholar]
- 9. Freitas HFG, Renault R, Ribeiro ES, Andrade FM, Brito FS Jr, Velloso LG.. Sudden cardiac arrest due to puerperal transient left ventricular apical ballooning syndrome. Int J Cardiol 2011;149:e12–e13. [DOI] [PubMed] [Google Scholar]
- 10. Zalewska-Adamiec M, Bachorzewska-Gajewska H, Tomaszuk-Kazberuk A, Nowak K, Drozdowski P, Bychowski J. et al. Takotsubo cardiomyopathy: serious early complications and two-year mortality – a 101 case study. Netherlands Heart J 2016;24:511–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Can MG, Özer A, İyigün M, Gökay BV, Emiroğlu R.. Takotsubo cardiomyopathy resulting in cardiac arrest in a patient undergoing liver transplantation. Transplant Proc 2017;49:2392–2394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.