Abstract
Background:
The early repolarization pattern (ERP) has recently been associated with cardiac events such as ventricular arrhythmias and sudden cardiac death. However, estimates of the prevalence of ERP vary widely, especially between the general population and physically active individuals. We performed this systematic review and meta-analysis to quantitatively evaluate the worldwide prevalence of ERP in the general population and physically active individuals.
Methods:
We thoroughly searched the PubMed, EMBASE, Web of science, the Cochrane Library, and Scopus databases for relevant studies published until December 20, 2020. Studies in which prevalence was presented or could be estimated from eligible data were included. The pooled prevalence was analyzed using a random-effect model.
Results:
Finally, we included 29 studies (182,135 subjects) in the general population and 14 studies (8087 subjects) in the physically active individuals. The worldwide pooled prevalence of ERP in the general population was 11.6% (95% confidence interval [CI]: 10.0%–13.3%). The incidence of ERP was 17.0% and 6.2% in men and women, respectively. The prevalence was 20.9% in blacks, 13.4% in Asians, and 10.1% in Caucasians. Additionally, the prevalence of ERP in physically active individuals was 33.9% (95% CI: 25.3%–42.6%).
Conclusion:
A significant difference in the worldwide prevalence of ERP is revealed in this study. The ERP is highly prevalent in men, blacks, and physically active individuals.
Keywords: early repolarization pattern, meta-analysis, prevalence
1. Introduction
Early repolarization pattern (ERP), which has been first described in 1936 by Shipley and Hallaran,[1] is generally defined as J-point elevation with QRS notching or slurring in the terminal part of the QRS complex detected by the standard 12-lead electrocardiogram (ECG).[2,3] ERP was once considered as a normal variant of ECG and even a sign of good health.[2] However, in recent years there is a growing recognition that early repolarization is associated with adverse outcomes. It has been reported that ERP increases the risk of idiopathic ventricular fibrillation, lone atrial fibrillation, and other arrhythmia events.[4–10] Furthermore, ERP has recently been reported to be associated with significant increased risk for sudden cardiac arrest and future arrhythmic death, which raises clinical and medicolegal concerns among cardiologists.[11–13]
Previous studies have indicated that ERP shows sex- and ethnicity-related penetrance. It is well known that its prevalence seems to be higher in men and blacks.[1,14–17] Because of different region and population, the prevalence of ERP is highly variable due to heterogeneity of each study.[18–20] In addition, previous studies have also investigated the difference in incidence of ERP between physically active individuals and the general population.[21,22] Several studies have reported that ERP is more commonly seen in physically active individuals.[1,21–23]
Up to now, although the prevalence of ERP has been reported in several regions and countries, no systematic evaluation has been done to report the specific worldwide prevalence of ERP. Therefore, we conducted this systematic review and meta-analysis to identify the worldwide prevalence of ERP in the general population and in physically active individuals.
2. Methods
2.1. Search strategy and selection criteria
Under the guidance of the preferred reporting items for systematic reviews and meta-analyses statement (PRISMA), we independently examined related English articles published up to December 20, 2020 by searching the PubMed, EMBASE, Web of science, the Cochrane Library, and Scopus databases. The search strategies were constructed by combining key words and related database-specific subject terms to search appropriate articles. The eligible words including “early repolarization pattern,” “ERP,” “early repolarization,” “J-wave,” “Osborn wave,” “prevalence,” and “incidence” were used. In addition, we hand-searched all the reference lists of the included articles to identify all relevant studies.
The titles and abstracts of the retrieved articles were independently examined by 3 review authors (H-YJ, NH, and RL), and any articles that were obviously irrelevant were excluded. Then the full texts of the remaining studies were reviewed and screened using the eligibility criteria. The inclusion criteria and exclusion criteria of study were as follows: studies were used that contained a clear definition of ERP proposed by Macfarlane et al[3] and Haissaguerre et al.[5] Prevalence of ERP was reported using either clinical ECG data or a follow-up experiment in the crowd or in the certain studying cohort. If not, sufficient data must be available to calculate the prevalence exactly. Studies that discussed prospective relationships between ERP prevalence and age, sex, occupation, ethnicity, or other clinical characteristics were included. The characteristics of the sample must be demonstrated thoroughly and exactly, articles that contained insufficient statistics would be excluded. Apparently healthy individuals and asymptomatic outpatients were employed and individuals who had any evidence of structural heart diseases were excluded from this meta-analysis. Physically active individuals include athletes and military officers.
2.2. Data extraction and quality assessment
From the articles taken into inclusion, useful information was independently extracted by 3 investigators (H-YJ, NH, and RL). Any disagreements were resolved by discussion with other investigators. The extracted data were as follows: first author's name, year, and country of publication, sample size, study design, definition of ERP, study population, average age, percentage of men, ethnicity, the ERP incidence, the percentage of men and women in ERP subjects.
Study quality was judged based on the Newcastle–Ottawa quality assessment scale (NOS) by 2 independent reviewers (H-YJ and X-QQ) using the following factors: study design, inclusion criteria, sample capacity, the sex ratio, and clear diagnostic criteria.
2.3. Ethics
In this study, ethical approval was not necessary because the included data were based on previous published articles, and no original clinical data were collected or utilized.
2.4. Statistical analysis
A random-effect model developed by DerSimonian and Laird was applied to estimate pooled prevalence and 95% confidence interval (CI) because we found that significant heterogeneity was present between studies after using the heterogeneity test. The heterogeneity among studies was quantified using the Cochran’ Q test, and the magnitude of heterogeneity was assessed using the I2 statistic. An I2 > 75% indicated high statistical heterogeneity.[11] Sensitivity analysis was performed by omitting 1 specific study at a time to examine whether the pooled prevalence could have been influenced by any included studies. Finally, the subgroup analysis was performed based on sexes (men vs women), ethnicities, and geographical regions.
Forest plots consisting of the point estimations of prevalence and their 95% CI for all included studies were constructed and statistical significance was defined as a P value <.05. We performed all analyses by using Stata version 16.0 (StataCorp, College Station, TX).
3. Results
3.1. Study selection
Results on literature search and literature selection for the calculation of prevalence were presented in detail (see Figure S1, Supplemental Digital Content, Supplemental Content, which illustrates the information flow of the search and selection of studies). We identified 723 papers with the initial search strategy. Additionally, 15 articles were retrieved from reference lists of included studies. Of the 738 unique articles, 534 studies were discarded after reading the title and abstract. Of the 204 studies selected for full-text review, 151 studies were excluded due to inadequate information and 10 studies were discarded for unclear ERP definition. Thus, the remaining 43 studies (29 studies that reported prevalence in general population and 14 studies that reported prevalence in physically active individuals) with 190,222 subjects were included in this meta-analysis.
3.2. Study characteristics
The characteristics of the 29 included studies involving a total general population of 182,135 subjects are shown in Table 1. Of the 29 studies,[5,8,15,16,19–21,24–45] 14 studies (48.3%) reported the prevalence in the Europe, including 3 in France,[5,30,38] 3 in Germany,[19,31,43] 3 in Finland,[21,24,40] 2 in the UK,[36,41] 2 in Italy,[27,39] and 1 in Spain.[33] Six studies reported the prevalence in the Asia, including 3 in China[32,35,44] and 1 each in Japan,[8] Korea,[15] and Thailand.[34] Eight studies reported the prevalence in the United States[16,20,25,28,37,40,42,45] and 1 each study reported the prevalence in Madagascar,[27] Egypt,[29] and Latin America.[26] The worldwide prevalence map of ERP by region was shown in Fig. 1.
Table 1.
Characteristics of the included studies to calculate total prevalence in the general population.
| Study | Year | Total | Mean age | Population | Ethnicity | Region | Men% | ERP% | ERP of men (%) | ERP of women (%) |
| Holkeri[24] | 2020 | 6631 | 50.1 ± 13.9 | Participants of the Mini-Finland Health Survey | Caucasian | Finland | 44.5 | 12.0 | 14.6 | 9.8 |
| Leiderman[25] | 2020 | 17,901 | 53.0 ± 13.0 | Participants at Montefiore Medical center (n = 6616) | AA | US | 38.6 | 6.8 | 7.1 | 4.6 |
| Participants at Montefiore Medical center (n = 9590) | Caucasian | 4.9 | ||||||||
| Others | NA | 4.5 | ||||||||
| Matta[26] | 2019 | 5398 | 35.0–74.0 | A general population from four mid-sized cities of Latin America | NA | Latin America | 41.3 | 7.3 | 9.2 | 5.9 |
| Creta[27] | 2019 | 616 | 7.5 ± 2.7 | Black African children from north-west Madagascar (300) | African | Madagascar | 47.4 | 23.3 | 25.1 | 21.7 |
| Caucasian ethnicity individuals (316) | Caucasian | Italy | 17.1 | 17.0 | 18.0 | |||||
| Trenkwalder[19] | 2019 | 13,878 | Mean: 54.6 | A population-based cohort located in the Rhein-Main region | Caucasian | Germany | 48.9 | 5.0 | 6.6 | 3.5 |
| Hasegawa[8] | 2019 | 395 | <60.0 | 395 healthy controls | Asian | Japan | NA | 10.0 | NA | NA |
| Movahed[28] | 2019 | 636 | 6.0–75.0 | Participants from the Anthony Bates Foundation | NA | US | NA | 13.5 | NA | NA |
| Abdellah[29] | 2018 | 1850 | NA | Consecutive subjects who attended the outpatient clinic of cardiology and internal medicine at SCUH, Ismailia, Egypt | African | Egypt | NA | 6.7 | NA | NA |
| Kelly[20] | 2018 | 4978 | ERP (−):46.2–65.0ERP (+): 43.2–62.7 | Black in the Jackson Heart Study cohort | AA | US | 35.8 | 28.3 | 50.2 | 16.1 |
| Rohel[30] | 2017 | 306 | 25.87 ± 3.3 | Female flight staff employed in French civilian or military sectors | Caucasian | France | 0 | 9.2 | NA | 9.2 |
| Trenkwalder[31] | 2017 | 1630 | 51.3 ± 13.5 | Population-based Study of Health in Pomerania (SHIP-1) | Caucasian | Germany | 47.1 | 4.8 | 5.1 | 4.5 |
| Sun[32] | 2017 | 10899 | Mean: 53.6 | The general rural Chinese population of Liaoning Province | Asian | China | 45.3 | 1.3 | 2.6 | 0.2 |
| Cho[15] | 2017 | 26345 | 48 ± 10.2 | The general ambulatory Korean population from the Health Promotion Center of Asan Medical Center | Asian | Korea | 60.6 | 11.2 | 15.3 | 4.8 |
| Rodríguez-Capitán[33] | 2017 | 13,179 | Mean: 40 | A large cohort of working adults aged 16–74 years in 5 cities in different regions of Spain | Caucasian | Spain | 73.4 | 2.4 | 3.1 | 0.4 |
| Makarawate[34] | 2015 | 282 | 20.0−45.0 | Healthy young northeastern Thai men at check-up clinics | Asian | Thailand | 100.0 | 10.3 | 10.3 | NA |
| Chen [35] | 2014 | 2247 | 56.0 ± 15.0 | Adult who received an ECG during a physical checkup or in the outpatient clinics | Asian | China | 47.9 | 24.2 | NA | NA |
| Macfarlane[36] | 2013 | 1496 | ≥18 .0 | Healthy individuals in the authors’ lab in UK | Caucasian | UK | 57.4 | 29.3 | 35.0 | 21.5 |
| Walsh[37] | 2013 | 5069 | 18.0−30.0 | Participants (40% black) from the CARDIA cohort (n = 2028) | AA | US | 45.5 | 30.5 | 36.6 | 3.5 |
| Participants (60% white) from the CARDIA cohort (n = 3041) | Caucasian | 10.6 | ||||||||
| Rollin[38] | 2012 | 1161 | 49.8 ± 8.6 | In middle-aged individuals living in the southwestern France | Caucasian | France | 51.6 | 13.7 | 21.0 | 5.9 |
| Lanza[39] | 2012 | 4176 | ERP (+): 38.3 ± 17.9ERP (−): 52.3 ± 17.8 | At Cardiology Service and the Center of pre-hospital evaluation of University Hospital in Italy (without structural heart disease) | Caucasian | Italy | 45.0 | 2.0 | 3.7 | 0.6 |
| Noseworthy[40] | 2011 | 9444 | 18.0−80.0 | Framingham Heart Study (n = 3955) | Caucasian | US | 45.0 | 4.5 | 7.6 | 2.0 |
| Health 2000 Study (n = 5489) in Finland | Caucasian | Finland | ||||||||
| Reinhard[41] | 2011 | 1877 | 18.0−60.0 | 1877 individuals from 505 white nuclear families | Caucasian | UK | 50.2 | 7.7 | 11.7 | 3.7 |
| Uberoi[42] | 2011 | 29281 | Male: 55.0 ± 14.0Female: 56.0 ± 17.0 | From the VA Palo Alto Health Care System (n = 3875) | AA | US | 87.2 | 6.0 | 2.5 | 0.6 |
| From the VA Palo Alto Health Care System (n = 25,406) | Caucasian | 1.7 | ||||||||
| Tikkanen[21] | 2011 | 10,864 | 30.0−59.0 | Middle-aged from 35 different geographical areas of Finland | Caucasian | Finland | 52.0 | 5.3 | 6.7 | 3.8 |
| Sinner[43] | 2010 | 6213 | 52.0 ± 10.1 | In the region of Augsburg, Southern Germany | Caucasian | Germany | 48.8 | 13.1 | 14.5 | 11.7 |
| Haissaguerre[5] | 2008 | 412 | 36.0 ± 12.0 | Control group comprised 412 subjects without heart disease | Caucasian | France | 65.5 | 5.1 | NA | NA |
| Kui[44] | 2008 | 1817 | 46.0 ± 15.0 | Healthy Chinese from April 2006 to July 2006 | Asian | China | 62.2 | 4.6 | 6.8 | 0.9 |
| Klatsky[45] | 2003 | 2081 | 24.0−62.0 | Individuals undergoing health examinations (n = 759) | AA | US | 55.7 | 45.8 | 50.0 | 9.5 |
| Individuals undergoing health examinations (n = 204) | Asian | 35.8 | ||||||||
| Individuals undergoing health examinations (n = 1,298) | Caucasian | 19.2 | ||||||||
| Surawicz[16] | 2002 | 1073 | 5.0−96.0 | Digitally stored ECGs, interpreted as normal, at St. Vincent Hospital, Indianapolis | Caucasian | US | 49.3 | 31.5 | 53.3 | 10.3 |
Figure 1.
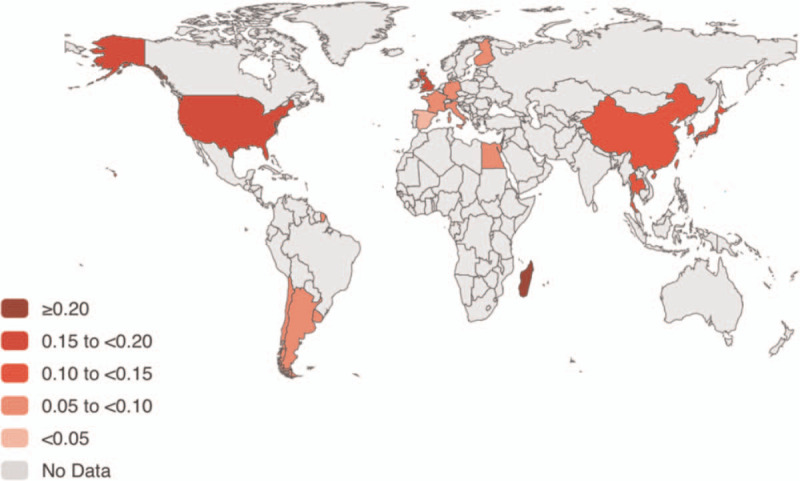
World prevalence map of ERP in the general population. ERP = early repolarization pattern.
Twenty-four studies[15,16,19–21,24–27,30–34,36–45] have discussed sex differences in the incidence of ERP. Additionally, the main characteristics of the 14 articles[22,46–58] included physically active individuals were summarized in Table 2. The NOS quality assessment results were reported (see Table S1, Supplemental Digital Content, Supplemental Content, which illustrates the risk of bias of included studies).
Table 2.
Characteristics of physically active individuals.
| Study | Year | Total | Mean age | Population | ERP% |
| Reinhard[22] | 2019 | 623 | 21.0 ± 5.0 | Elite athletes who were examined in the outpatient clinic of the Department of Prevention and Sports Medicine, Technical University Munich, Germany. | 17.3 |
| Miragoli[46] | 2019 | 414 | 13.6 ± 1.8 | Non-professional healthy adolescent athletes | 22.2 |
| Roche[47] | 2018 | 2508 | 24.0 ± 5.0 | Recruits of the French Foreign Legion who were healthy and physically active men | 19.5 |
| Malhotra[48] | 2015 | 66 | NA | Actively training Indian athletes training for competitive sports in one of the premier training institutes of Indian Armed Forces between July 2012 and August 2012 | 42.4 |
| Kiss[49] | 2015 | 227 | 27.2 ± 8.7 | Asymptomatic elite, non-elite and master athletes in Hungarian | 64.3 |
| Brosnan[50] | 2015 | 726 | 16.0−40.0 | Non-Caucasian Australian male athletes (173) Caucasian male athletes (553) | 36.8 |
| Serra-Grima[51] | 2015 | 299 | ERP (+): 20.5 ± 6.4ERP (−): 20.1 ± 6.4 | White elite athletes recruited between 1960 and 1999 | 31.4 |
| Vinsonneau[52] | 2015 | 250 | 22.9 ± 0.5 | Healthy military officers aged over 17 years, Caucasians and practicing at least two hours of sport per week | 19.2 |
| Aagaard [53] | 2014 | 151 | 50.0 ± 5.0 | Physically active middle-age males who had registered for first-time participation in the 2010 cross-country race and lived in the Greater Stockholm area | 44.4 |
| Vinsonneau[54] | 2013 | 746 | 29.0 ± 10.3 | Caucasian military officers incorporated or engaged in French Navy units in Brittany from November 2010 to November 2011 | 13.8 |
| Noseworthy[55] | 2011 | 879 | 18.4 ± 0.8 | Student athletes ≥18 years old who were official participants in competitive inter-collegiate athletics between 2006 and 2010 | 25.1 |
| Junttila[56] | 2011 | 503 | 17.0−24.0 | Athletes at the University of Miami in 2000 | 29.8 |
| Ouali[57] | 2011 | 540 | 18.3 ± 2.4 | Athletes in the Central Sports Medicine Centre of El Menzah in Tunisia, 100% white Arabs | 22.0 |
| Bianco[58] | 2001 | 155 | 30.9 ± 10.1 | Top-ranking male Caucasian athletes | 89.7 |
3.3. Prevalence of ERP and subgroup analyses
According to the 29 studies reported prevalence in general population, the worldwide pooled prevalence of ERP was 11.6% (95% CI: 10.0%–13.3%, Fig. 2) irrespective of age, sex, race, region, and country. There was a significant heterogeneity among these 29 studies (Cochran Q statistic's P < .001; I2 = 99.7%) and the sensitivity analysis was shown (see Figure S2, Supplemental Digital Content, Supplemental Content).
Figure 2.
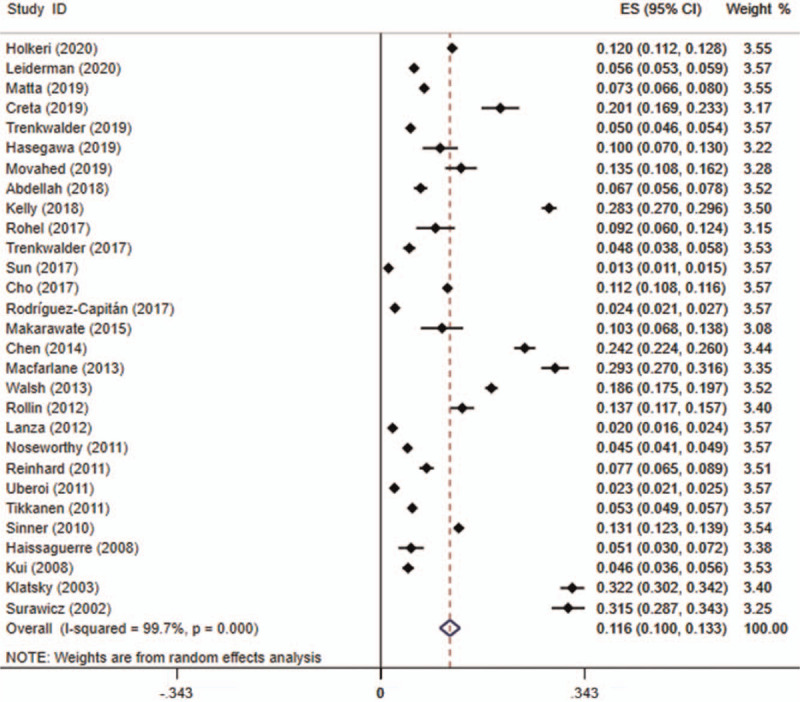
Forest plot of the prevalence of ERP in the general population. ERP = early repolarization pattern.
Twenty-four articles have studied the sex differences of the prevalence of ERP. The pooled prevalence of ERP in men was 17.0% (95% CI: 14.3%–19.6%, see Figure S3, Supplemental Digital Content, Supplemental Content) while that in the women was 6.2% (95% CI: 5.1%–7.3%, see Figure S4, Supplemental Digital Content, Supplemental Content).
The prevalence of ERP in different races was also reported in the included studies. The results of racial prevalence of ERP were presented in Figures S5–S7, Supplemental Digital Content. The prevalence of ERP was 20.9% (95% CI: 13.1%–28.8%, see Figure S5, Supplemental Digital Content, Supplemental Content) in blacks, which was twice higher than the worldwide prevalence in the general population. And the incidence was 13.4% (95% CI: 7.9%–18.8%, see Figure S6, Supplemental Digital Content, Supplemental Content) in Asians and 10.1% (95% CI: 8.5%–11.7%, see Figure S7, Supplemental Digital Content, Supplemental Content) in Caucasians.
For the physically active individuals, including athletes and military officers, the mean prevalence of ERP was 33.9% (95% CI: 25.3%–42.6%, Fig. 3). The heterogeneity among these studies was statistically significant (Cochran Q statistic's P < .001; I2 = 98.8%). The sensitivity analysis was conducted (see Figure S8, Supplemental Digital Content, Supplemental Content), which didn’t indicate obvious influence of each study on the overall result.
Figure 3.
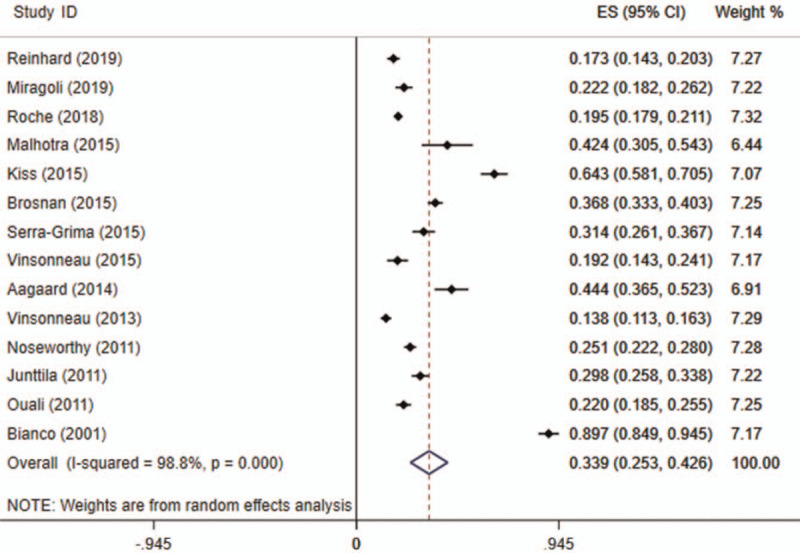
Forest plot of the prevalence of ERP in the physically active individuals. ERP = early repolarization pattern.
4. Discussion
The elevation of the J point ≥0.1 mV in at least 2 leads in the inferior (II, III, aVF) and/or lateral leads (I, aVL, V4–V6) is the main characteristic of ERP. Although ERP has been generally considered benign for decades, recent studies have indicated that ERP portends an increased risk of lone atrial fibrillation, idiopathic ventricular fibrillation, and sudden death without structural heart disease.[5–8] The present study is the first systematic review and meta-analysis to evaluate the worldwide prevalence of ERP among different sexes, ethnicities, regions, countries, and populations. The prevalence of ERP around the world in the general population is about 11.6%. There is a trend toward a higher frequency in blacks, men, and physically active individuals.
In this study, the incidence of ERP is 17.0% and 6.2% in men and women with 176,595 subjects included. The outcome is in keeping with Ezaki study, which has already reported sex differences in the incidence of various types of ventricular arrhythmias.[17] It has been known for years that the J point or ST onset is higher in men in all precordial leads.[4,17] This phenomenon might result from the effect of the male hormone testosterone.[17,59,60] On the other hand, the trans-membrane voltage gradient of action potential is triggered by transient outward potassium current (Ito)-activity in phase 1 and 2.[53] This gradient is the physiological basis of slur or notching of the ECG for ERP.[61] In normal subjects with different sex, there is always a small degree of heterogeneity in this voltage gradient.[17] In summary, the effect of sex hormones and the heterogeneity in voltage gradient have been considered to be the physiological basis for sex differences in ERP.
According to our pooled analyzed prevalence, ERP is approximately twice as common in blacks as in Caucasians, which is similar to previous studies.[20,27,62] Olson et al reported that 24.4% of blacks versus 7.9% of whites had J-point elevation based on Atherosclerosis Risk in Communities (ARIC) study.[20,62] Considering correlation between ECG variations and body composition proposed in previous studies,[63,64] differences in body build, composition, and nutrition might in part explain the clinical differences in prevalence among races.[28]
The present study shows that ERP is more prevalent in physically active individuals (33.9%), which is in accordance with Tikkanen study.[21] According to Tikkanen research, the prevalence of ERP was 43.5% among the Finnish athletes and 30.0% among the US athletes.[21] Vinsonneau study also showed that ERP was more common in population that takes exercise regularly.[54] Vagotonia is often observed in physically active individuals and may increase regional electrophysiological differences and repolarization dispersion in the myocardium, which might explain the development of J-point elevation in athletes.[53,65,66]
However, our study has the following limitations: the subjects in our study are mostly from Europe, Asia, and US. There are only 2 studies from Africa and 1 study from Latin America. Another limitation of this study is the imbalance of the sex ratio (100,467 men, 76,128 women), which may cause bias. The heterogeneity in the overall and subgroup analyses is also a limitation of this study. Heterogeneities in each analysis are high, likely because of differences in methodology, population, ethnicity, and geographic region.
5. Conclusions
In conclusion, according to our study the worldwide prevalence of ERP in the physically active individuals is much higher (around 33.9%) than in subjects from the general population (around 11.6%). The prevalence of ERP in men and blacks is higher as compared with others in the general population. These above-mentioned results might indicate that clinical screening and further examination of ERP in potential population need to be considered.
Acknowledgments
The authors thank all participants who contribute to this meta-analysis.
Author contributions
Hong-Yan Ji and Xiao-Qing Quan contributed to the conception and design of this study. Hong-Yan Ji, Nan Hu and Rui Liu were involved in the selection of the included studies. Hong-Yan Ji, Nan Hu, Rui Liu, Hai-Rong Zhou, Wei-Liang Gao and Xiao-Qing Quan were involved in the acquisition and interpretation of the data. The manuscript was written and reviewed by Hong-Yan Ji, Nan Hu, Rui Liu, Hai-Rong Zhou, Wei-Liang Gao and Xiao-Qing Quan. All authors read and approved the final manuscript.
Conceptualization: Nan Hu.
Writing – original draft: Hong-Yan Ji, Nan Hu, Rui Liu, Hai-Rong Zhou, Wei-Liang Gao, Xiao-Qing Quan.
Writing – review & editing: Xiao-Qing Quan.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, ECG = electrocardiogram, ERP = early repolarization pattern, NOS = Newcastle–Ottawa quality assessment scale, PRISMA = preferred reporting items for systematic reviews and meta-analyses statement.
How to cite this article: Ji HY, Hu N, Liu R, Zhou HR, Gao WL, Quan XQ. Worldwide prevalence of early repolarization pattern in general population and physically active individuals: a meta-analysis. Medicine. 2021;100:22(e25978).
This work is supported by the Shenzhen Key Medical Discipline Construction Fund (SZXK063) and National Natural Science Foundation of China (81400255).
The authors declare that they have no competing interests.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplemental digital content is available for this article.
AA = African American, CARDIA = coronary artery risk development in young adults, NA = not available.
ERP = early repolarization pattern.
References
- [1].Rezus C, Floria M, Moga VD, et al. Early repolarization syndrome: electrocardiographic signs and clinical implications. Ann Noninvasive Electrocardiol 2014;19:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Wu SH, Lin XX, Cheng YJ, Qiang CC, Zhang J. Early repolarization pattern and risk for arrhythmia death: a meta-analysis. J Am Coll Cardiol 2013;61:645–50. [DOI] [PubMed] [Google Scholar]
- [3].Macfarlane PW, Antzelevitch C, Haissaguerre M, et al. The early repolarization pattern: a consensus paper. J Am Coll Cardiol 2015;66:470–7. [DOI] [PubMed] [Google Scholar]
- [4].Antzelevitch C, Antzelevitch C, Yan GX. J wave syndromes. Heart Rhythm 2010;7:549–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Haissaguerre M, Derval N, Sacher F, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med 2008;358:2016–23. [DOI] [PubMed] [Google Scholar]
- [6].Tikkanen JT, Anttonen O, Junttila MJ, et al. Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med 2009;361:2529–37. [DOI] [PubMed] [Google Scholar]
- [7].Rosso R, Kogan E, Belhassen B, et al. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects: incidence and clinical significance. J Am Coll Cardiol 2008;52:1231–8. [DOI] [PubMed] [Google Scholar]
- [8].Hasegawa Y, Watanabe H, Ikami Y, et al. Early repolarization and risk of lone atrial fibrillation. J Cardiovasc Electrophysiol 2019;30:565–8. [DOI] [PubMed] [Google Scholar]
- [9].Rao LY, Mao Y, Huang K, Li YS, Shu YW. Relationship between atrial tissue remodeling and ECG features in atrial fibrillation. Curr Med Sci 2019;39:541–5. [DOI] [PubMed] [Google Scholar]
- [10].Wang XT, Zhao G, Tu L, et al. Continuous positive airway pressure effectively alleviates arrhythmias in patients with obstructive sleep apnea: possible relationship with counteracting oxidative stress. Curr Med Sci 2019;39:52–8. [DOI] [PubMed] [Google Scholar]
- [11].Cheng YJ, Lin XX, Ji CC, et al. Role of early repolarization pattern in increasing risk of death. J Am Heart Assoc 2016;5:e003375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kim SH, Kim DY, Kim H-J, et al. Early repolarization with horizontal ST segment may be associated with aborted sudden cardiac arrest: a retrospective case control study. BMC Cardiovasc Disord 2012;12:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hu J, Tang B, Wang J, et al. Familial atrial enlargement, conduction disorder and symmetric cardiac hypertrophy are early signs of PRKAG2 R302Q. Curr Med Sci 2020;40:486–92. [DOI] [PubMed] [Google Scholar]
- [14].Reddy VK, Gapstur SM, Prineas R, Colangelo LA, Ouyang P, Kadish AH. Ethnic differences in ST height in the multiethnic study of atherosclerosis. Ann Noninvasive Electrocardiol 2008;13:341–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Cho MS, Kwon CH, Nam GB, et al. Characteristics of early repolarization parameters and prognostic implications in the general ambulatory Korean population. Int J Cardiol 2017;227:571–6. [DOI] [PubMed] [Google Scholar]
- [16].Surawicz B, Parikh SR. Prevalence of male and female patterns of early ventricular repolarization in the normal ECG of males and females from childhood to old age. J Am Coll Cardiol 2002;40:1870–6. [DOI] [PubMed] [Google Scholar]
- [17].Ezaki K, Nakagawa M, Taniguchi Y, et al. Gender differences in the ST segment: effect of androgen-deprivation therapy and possible role of testosterone. Circ J 2010;74:2448–54. [DOI] [PubMed] [Google Scholar]
- [18].Maury P, Rollin A. Prevalence of early repolarisation/J wave patterns in the normal population. J Electrocardiol 2013;46:411–6. [DOI] [PubMed] [Google Scholar]
- [19].Trenkwalder T, Rubsamen N, Schmitt VH, et al. Left ventricular geometry and function in early repolarization: results from the population-based Gutenberg Health Study. Clin Res Cardiol 2019;108:1107–16. [DOI] [PubMed] [Google Scholar]
- [20].Kelly JP, Greiner M, Soliman EZ, et al. Relation of early repolarization (j point elevation) to mortality in blacks (from the Jackson Heart Study). Am J Cardiol 2018;122:340–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Tikkanen JT, Junttila MJ, Anttonen O, et al. Early repolarization: electrocardiographic phenotypes associated with favorable long-term outcome. Circulation 2011;123:2666–73. [DOI] [PubMed] [Google Scholar]
- [22].Reinhard W, Trenkwalder T, Haller B, et al. The early repolarization pattern: echocardiographic characteristics in elite athletes. Ann Noninvasive Electrocardiol 2019;24:e12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Quattrini FM, Pelliccia A, Assorgi R, et al. Benign clinical significance of J-wave pattern (early repolarization) in highly trained athletes. Heart Rhythm 2014;11:1974–82. [DOI] [PubMed] [Google Scholar]
- [24].Holkeri A, Eranti A, Haukilahti MAE, et al. Impact of age and sex on the long-term prognosis associated with early repolarization in the general population. Heart Rhythm 2020;17:621–8. [DOI] [PubMed] [Google Scholar]
- [25].Leiderman E, Kargoli F, Shulman E, et al. Early repolarization pattern in an ethnically diverse population: increased risk in Hispanics. Pacing Clin Electrophysiol 2020;43:30–6. [DOI] [PubMed] [Google Scholar]
- [26].Matta MG, Gulayin PE, Garcia-Zamora S, et al. Epidemiology of early repolarization pattern in an adult general population. Acta Cardiol 2019;75:713–23. [DOI] [PubMed] [Google Scholar]
- [27].Creta A, Arigliani M, di Gioia G, et al. Impact of ethnicity on the prevalence of early repolarization pattern in children: comparison between caucasian and african populations. Pediatr Cardiol 2019;40:1553–8. [DOI] [PubMed] [Google Scholar]
- [28].Movahed MR, Sattur S, Bates S. Higher prevalence of abnormal electrocardigrams (ECG) in African Americans undergoing screening ECG and echocardiography. Crit Pathw Cardiol 2019;18:86–8. [DOI] [PubMed] [Google Scholar]
- [29].Abdellah AT, El Wazir M, Kamal H, Hegazy H. Prevalence of early repolarization pattern and its association with sudden cardiac death and arrhythmia over one-year follow-up in an Egyptian cohort. Egypt Heart J 2018;70:315–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rohel G, Perrier E, Delluc A, et al. Progression of early repolarization patterns at a four year follow-up in a female flight crew population: implications for aviation medicine. Ann Noninvasive Electrocardiol 2017;22:e12451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Trenkwalder T, King R, Kaess BM, et al. Ventricular and supraventricular ectopy in subjects with early repolarization. Am J Cardiol 2017;120:92–7. [DOI] [PubMed] [Google Scholar]
- [32].Sun GZ, Ye N, Chen YT, Zhou Y, Li Z, Sun YX. Early repolarization pattern in the general population: prevalence and associated factors. Int J Cardiol 2017;230:614–8. [DOI] [PubMed] [Google Scholar]
- [33].Rodriguez-Capitan J, Fernandez-Meseguer A, Garcia-Pinilla JM, et al. Frequency of different electrocardiographic abnormalities in a large cohort of Spanish workers. Europace 2017;19:1855–63. [DOI] [PubMed] [Google Scholar]
- [34].Makarawate P, Chaosuwannakit N, Ruamcharoen Y, et al. Prevalence and associated factors of early repolarization pattern in healthy young northeastern Thai men: a correlation study with Brugada electrocardiography. J Arrhythm 2015;31:215–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Chen YC, Huang JH, Lin YK, Hsieh MH, Chen YJ. Gender modulates the aging effects on different patterns of early repolarization. Heart Vessels 2014;29:249–55. [DOI] [PubMed] [Google Scholar]
- [36].Macfarlane PW, Clark EN, Heng JS. J wave patterns--morphology, prevalence and nomenclature. J Electrocardiol 2013;46:505–9. [DOI] [PubMed] [Google Scholar]
- [37].Walsh JA, 3rd, Ilkhanoff L, Soliman EZ, et al. Natural history of the early repolarization pattern in a biracial cohort: CARDIA (Coronary Artery Risk Development in Young Adults) Study. J Am Coll Cardiol 2013;61:863–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Rollin A, Maury P, Bongard V, et al. Prevalence, prognosis, and identification of the malignant form of early repolarization pattern in a population-based study. Am J Cardiol 2012;110:1302–8. [DOI] [PubMed] [Google Scholar]
- [39].Lanza GA, Mollo R, Cosenza A, et al. Prevalence and clinical correlates of early repolarization and J wave in a large cohort of subjects without overt heart disease. J Electrocardiol 2012;45:404–10. [DOI] [PubMed] [Google Scholar]
- [40].Noseworthy PA, Tikkanen JT, Porthan K, et al. The early repolarization pattern in the general population: clinical correlates and heritability. J Am Coll Cardiol 2011;57:2284–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Reinhard W, Kaess BM, Debiec R, et al. Heritability of early repolarization: a population-based study. Circ Cardiovasc Genet 2011;4:134–8. [DOI] [PubMed] [Google Scholar]
- [42].Uberoi A, Jain NA, Perez M, et al. Early repolarization in an ambulatory clinical population. Circulation 2011;124:2208–14. [DOI] [PubMed] [Google Scholar]
- [43].Sinner MF, Reinhard W, Muller M, et al. Association of early repolarization pattern on ECG with risk of cardiac and all-cause mortality: a population-based prospective cohort study (MONICA/KORA). PLoS Med 2010;7:e1000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kui C, Congxin H, Xi W, et al. Characteristic of the prevalence of J wave in apparently healthy Chinese adults. Arch Med Res 2008;39:232–5. [DOI] [PubMed] [Google Scholar]
- [45].Klatsky AL, Oehm R, Cooper RA, Udaltsova N, Armstrong MA. The early repolarization normal variant electrocardiogram: correlates and consequences. Am J Med 2003;115:171–7. [DOI] [PubMed] [Google Scholar]
- [46].Miragoli M, Goldoni M, Demola P, et al. Left ventricular geometry correlates with early repolarization pattern in adolescent athletes. Scand J Med Sci Sports 2019;29:1727–35. [DOI] [PubMed] [Google Scholar]
- [47].Roche NC, Massoure PL, Deharo JC, et al. Seven years follow-up of early repolarisation patterns in French elite special forces. Ann Noninvasive Electrocardiol 2018;23:e12560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Malhotra VK, Singh N, Bishnoi RS, et al. The prevalence of abnormal ECG in trained sportsmen. Med J Armed Forces India 2015;71:324–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Kiss O, Sydo N, Vargha P, et al. Prevalence of physiological and pathological electrocardiographic findings in Hungarian athletes. Acta Physiol Hung 2015;102:228–37. [DOI] [PubMed] [Google Scholar]
- [50].Brosnan MJ, Kumar S, LaGerche A, et al. Early repolarization patterns associated with increased arrhythmic risk are common in young non-Caucasian Australian males and not influenced by athletic status. Heart Rhythm 2015;12:1576–83. [DOI] [PubMed] [Google Scholar]
- [51].Serra-Grima R, Donate M, Alvarez-Garcia J, et al. Long-term follow-up of early repolarization pattern in elite athletes. Am J Med 2015;128:192.e1–9. [DOI] [PubMed] [Google Scholar]
- [52].Vinsonneau U, Pangnarind-Heinz V, Paleiron N, et al. Evolution of early repolarization patterns after 5 years in a military population at low cardiovascular risk and practical implications in military medical expertise. Ann Noninvasive Electrocardiol 2015;20:420–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Aagaard P, Braunschweig F, Wecke L, et al. Early repolarization in middle-age runners: cardiovascular characteristics. Med Sci Sports Exerc 2014;46:1285–92. [DOI] [PubMed] [Google Scholar]
- [54].Vinsonneau U, Pinon B, Paleiron N, et al. Prevalence of early repolarization patterns in a French military population at low cardiovascular risk: implications for preventive medicine. Ann Noninvasive Electrocardiol 2013;18:436–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Noseworthy PA, Weiner R, Kim J, et al. Early repolarization pattern in competitive athletes: clinical correlates and the effects of exercise training. Circ Arrhythm Electrophysiol 2011;4:432–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Junttila MJ, Sager SJ, Freiser M, McGonagle S, Castellanos A, Myerburg RJ. Inferolateral early repolarization in athletes. J Interv Card Electrophysiol 2011;31:33–8. [DOI] [PubMed] [Google Scholar]
- [57].Ouali S, Ben Salem H, Hammas S, et al. Prevalence of Brugada-type ECG pattern and early ventricular repolarization pattern in Tunisian athletes. Open Access J Sports Med 2011;2:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Bianco M, Bria S, Gianfelici A, Sanna N, Palmieri V, Zeppilli P. Does early repolarization in the athlete have analogies with the Brugada syndrome? Eur Heart J 2001;22:504–10. [DOI] [PubMed] [Google Scholar]
- [59].Bidoggia H, Maciel JP, Capalozza N, et al. Sex differences on the electrocardiographic pattern of cardiac repolarization: possible role of testosterone. Am Heart J 2000;140:678–83. [DOI] [PubMed] [Google Scholar]
- [60].Bidoggia H, Maciel JP, Capalozza N, et al. Sex-dependent electrocardiographic pattern of cardiac repolarization. Am Heart J 2000;140:430–6. [DOI] [PubMed] [Google Scholar]
- [61].Yan GX, Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation 1996;93:372–9. [DOI] [PubMed] [Google Scholar]
- [62].Olson KA, Viera AJ, Soliman EZ, Crow RS, Rosamond WD. Long-term prognosis associated with J-point elevation in a large middle-aged biracial cohort: the ARIC study. Eur Heart J 2011;32:3098–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Pipberger HV, Goldman MJ, Littmann D, Murphy GP, Cosma J, Snyder JR. Correlations of the orthogonal electrocardiogram and vectorcardiogram with consitutional variables in 518 normal men. Circulation 1967;35:536–51. [DOI] [PubMed] [Google Scholar]
- [64].Kilty SE, Lepeschkin E. Effect of body build on the qrs voltage of the electrocardiogram in normal men: its significance in the diagnosis of left ventricular hypertrophy. Circulation 1965;31:77–84. [DOI] [PubMed] [Google Scholar]
- [65].Barbosa EC, Bomfim Ade S, Benchimol-Barbosa PR, Ginefra P. Ionic mechanisms and vectorial model of early repolarization pattern in the surface electrocardiogram of the athlete. Ann Noninvasive Electrocardiol 2008;13:301–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Cuspidi C, Tadic M. Left atrial function in elite athletes: a meta-analysis of two-dimensional speckle tracking echocardiographic studies. Clin Cardiol 2019;42:579–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


